Abstract
African Animal Trypanosomiasis (AAT) is transmitted by the tsetse fly which carries pathogenic trypanosomes in its saliva, thus causing debilitating infection to livestock health. As the disease advances, a multistage progression process is observed based on the progressive clinical signs displayed in the host’s body. Investigation of genes expressed with regular monotonic patterns (known as Monotonically Expressed Genes (MEGs)) and of their master regulators can provide important clue for the understanding of the molecular mechanisms underlying the AAT disease. For this purpose, we analysed MEGs for three tissues (liver, spleen and lymph node) of two cattle breeds, namely trypanosusceptible Boran and trypanotolerant N’Dama. Our analysis revealed cattle breed-specific master regulators which are highly related to distinguish the genetic programs in both cattle breeds. Especially the master regulators MYC and DBP found in this study, seem to influence the immune responses strongly, thereby susceptibility and trypanotolerance of Boran and N’Dama respectively. Furthermore, our pathway analysis also bolsters the crucial roles of these master regulators. Taken together, our findings provide novel insights into breed-specific master regulators which orchestrate the regulatory cascades influencing the level of trypanotolerance in cattle breeds and thus could be promising drug targets for future therapeutic interventions.
Keywords: animal african trypanosomiasis, master regulators, over-represented pathways, DBP, MYC
1. Introduction
African Animal Trypanosomiasis (AAT), also known as ’nagana’, is a parasitic disease of animals caused by the flagellated protozoan species of Trypanosoma which is transmitted primarily through the bite of infected tsetse flies [1]. This neglected disease is a threat to animal and human health, especially in sub-Saharan African countries [2,3,4]. It affects millions of livestock annually, leading to major economic loss of billions of US dollars every year and substantial decrease in agricultural productivity in Africa [5,6].
Trypanosoma congolense, Trypanosoma vivax, and Trypanosoma brucei are the major causes of infection in livestock [7]. Trypanotolerance refers to the capability of the animal to control parasitaemia and anaemia and to remain productive despite the infection of the parasite [8,9,10]. It has become an important trait in the recent decade and this trait is widely found in some Bos taurus cattle breeds including N’Dama and West African shorthorn breeds [9,11,12,13]. Although the aforementioned cattle breeds remain productive during the course of the disease, they are not desirable for farming due to their smaller size and lower draft power. On the other hand, Zebu (Bos indicus) cattle are not particularly resistant to trypanosomiasis, unlike the native Bos taurus cattle. Farmers depend on the Zebu cattle breeds like Boran as they are more suitable for agricultural purposes due to their high draught power and agricultural productivity. However, susceptibility of these breeds to trypanosomiasis poses heavy economic constraints to the farmers [9,10,14,15,16,17,18,19].
Until now, several studies have been performed in cattle by analysing genotype or gene expression data in order to understand the molecular mechanism underlying the genetic resistance to African trypanosomiasis [20,21,22,23,24,25]. Hanotte et al. [25] identified quantitative trait loci (QTL) controlling trypanotolerance in a cross of tolerant West African N’Dama and susceptible East African Boran cattle. Moreover, Mekonnen et al. [20] surveyed the genome of the cattle breed Sheko to study the genotype-phentotype associations and identified genomic regions associated with trypanosomiasis. On the other hand, O’Gorman et al. [22] identified temporal changes in peripheral blood mononuclear cell (PBMC) gene expression in trypanotolerant N’Dama and trypanosusceptible Boran, by studying transcriptomic profiles during the disease progression. To this end, Noyes et al. [26] performed gene expression analysis and identified several candidate genes in pathways which responded to trypanosome infection in Boran and N’Dama.
Recently, by analysing the gene expression data set generated by Noyes et al. [26], we have deciphered the cattle breed-specific partner choice of transcription factors (TFs) during the disease progression [27]. For this purpose, we mainly considered the Monotonically Expressed Genes (MEGs) to capture the multistage progression process of the AAT disease in liver, spleen and lymph node tissues. Importantly, we highlighted the pivotal relevance of the preferential partner choice of the TF albumin D-site-Binding Protein (DBP) in these tissues.
It has been widely shown that the transcriptional regulation of DBP controls the circadian output/behaviour not only in the suprachiasmatic nucleus SCN [28], but also in the peripheral tissues [29,30]. Taking this aspect into account, we addressed the association of DBP with circadian transcriptional regulation of tissue-specific processes in mammalian species, in the context of AAT. Especially our findings implicating the functional relationship of circadian control with the immune system are well substantiated by Solis et al. [31], Barik et al. [32] and Scheiermann et al. [33]. In reference to the study by Frank Hawking [34], in which he experimentally established the link between circadian rhythm and T. congolense infection in the blood of laboratory rodents, our findings also support the important role of the circadian rhythm in the AAT disease.
Exploring tissue-specific regulatory mechanisms is of utmost importance, especially in tissues such as liver, spleen and lymph nodes, which are likely the primary sites where anaemia occurs as extra-vascular haemolysis [13,35,36]. Therefore, similar to our previous studies [37,38], taking advantage of the systems biology approaches, we attempted in this study to gain novel insights by unravelling the tissue- and breed-specific master regulators and over-represented signalling pathways that responded to trypanosome infection in Boran and N’Dama. Surprisingly, our results show DBP as a master regulator for liver tissue of N’Dama, emphasizing the role of the circadian rhythm in the hepatic metabolism and in the immune responses after trypanosome infection in this resistant breed. Altogether, our results highlight a striking feature of the circadian clock in trypanotolerance, especially in the regulatory role of DBP in the immunity of trypanotolerant cattle, which confirms our previous finding about the relevance of the clock-controlled gene DBP to AAT.
Master Regulators as Drug Targets
Recently omics technologies and computational approaches have become intriguing tools and approaches for drug discovery, making use of gene expression data. Exploiting the systems biology approaches in several studies [39,40,41,42], master regulators have been reported as potential therapeutic targets. By definition, master regulators are molecules that are located at the top of the hierarchy involved in the transcriptomic regulation, where the nodes tend to converge after certain upstream steps [43]. In biological processes, master regulators specifically regulate the expression of downstream genes either directly or through cascades thereby leading to altered phenotypes. In cellular context, dendritic cells involved in antigen-specific responses are regarded as the master regulators which serve as a major link between the innate and the adaptive immune system [44]. A recent study from Vargas et al on Alzheimer’s disease has proposed several therapeutic molecular targets for drug development based on master regulator analysis [45]. Similar analyses revealed potential drug targets experimentally for anaplastic thyroid carcinoma in which few transcription factors were proposed as master regulators [46]. Few aforementioned examples demonstrate that transcription regulatory networks and master regulators could be promising drug candidates analysed for investigating complex diseases (including Alzheimer’s disease and cancer) as they could be crucial drivers of the molecular mechanism of disease processes.
2. Materials and Methods
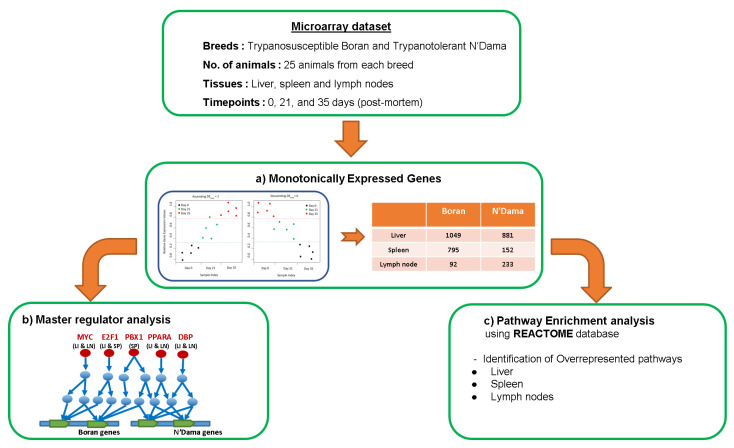
In this section, we provided an outline of the data set and the methods we used in this study. Figure 1 depicts the workflow of this study.
Figure 1.
Flowchart of the analysis. (a) Monotonically Expressed Genes (MEGs) obtained from the analysis of microarray data set comprising gene expression profiles of two cattle breeds: trypanosusceptible Boran and trypanotolerant N’Dama (Boran Asc - MEGs expressed in the ascending pattern for Boran, Boran Des - MEGs expressed in the descending pattern for Boran, N’Dama Asc - MEGs expressed in the ascending pattern for N’Dama and N’Dama Des - MEGs expressed in the descending pattern for N’Dama; (b) Master regulator analysis (Red circles and texts in red represent the exemplarily selected master regulators from this study; LI, SP & LN stand for liver, spleen and lymph node tissues); (c) Pathway enrichment analysis performed using Reactome database.
2.1. Gene Sets
In order to identify master regulators and over-represented pathways related to the genetic programs underlying AAT, we analysed six gene sets that exhibit regular monotonic expression patterns in liver-, spleen-, and lymph node tissues of the two cattle breeds, namely trypanosusceptible Boran and trypanotolerant N’Dama, after being infected with Trypanosoma congolense. For this purpose, we took the gene sets from our previous study [27] in which we identified the genes based on the publicly available continuous transcription profiling time-series microarray data set (http://www.ebi.uk/arrayexpress/, accession no.E-MEXP-1778) [26]. In this study, we will mainly focus on the analysis of the gene sets. A brief summary about the microarray data set and the number of monotonically expressed genes (MEGs) is given below.
2.2. Microarray Data Set
In this section, we recapitulate the experimental procedure performed by Noyes et al. [26]. They performed a microarray experiment based on the cattle breeds Boran and N’Dama as per the following: In the animal experiment, 25 healthy trypanosomiasis-free animals from each breed (trypanosusceptible Boran and trypanotolerant N’Dama) were infected with Trypanosoma congolense IL1180 clone. To ensure the health of trypanosomiasis-free animals before experimental infection, the cattle were selected from herds in a tsetse fly-free and trypanosomiasis-free zone of the ILRI Kapiti Plains ranch and assessed negative for tick-borne parasites before transferring them to the ILRI research facility at Kabete. All procedures for handling the animals were performed according to the International Livestock Research Institute (ILRI) ethical review process. Liver, spleen and lymph node tissues were harvested from the cattle on day 0, day 21 and day 35. For control experiments, five animals from each breed were killed before infection and the gene expression readings were recorded for day 0. Tissue harvest was performed after infection. After infection of the cattle, the tissues were collected on day 21 and day 35 post-mortem. Additionally, needle biopsy method was applied only for the liver tissue sampling on day 0 (before infection), day 12, day 15, day 18, day 26, day 29, day 32 after infection. For each condition, extraction of RNA from tissues was done and hybridisation were performed on individual arrays.
2.3. Monotonically Expressed Genes
In our recent study [27], we identified the MEGs for each tissue of both cattle breeds by applying the monotonic feature selector (MFSelector) approach [47] to the microarray data set. The lists of MEGs for each tissue are provided in the Supplementary File S1 and the numbers of MEGs are given in Table 1.
Table 1.
Number of MEGs in ascending and descending order for liver-, spleen- and lymph node tissues for the cattle breeds Boran and N’Dama.
| Boran | N’Dama | |||
|---|---|---|---|---|
| Ascending | Descending | Ascending | Descending | |
| Liver | 741 | 308 | 757 | 124 |
| Spleen | 669 | 126 | 13 | 139 |
| Lymph node | 87 | 5 | 119 | 114 |
2.4. Finding Master Regulators and Over-Represented Pathways
Similar to our previous studies [20,37,38], we applied well established systems biology approaches using the geneXplain platform [48] in order to identify master regulators and over-represented pathways.
For this purpose, we first run the “upstream analysis” workflow developed by [49] with the maximum radius of 10 steps upstream using the Reactome database [50]. The “upstream analysis” algorithm constructs a global signal transduction network and then identifies the master regulators based on the convergence points of these networks. In general, master regulators are located at the top of a regulatory hierarchy and control the downstream genes without their regulatory influence in signalling pathways [51].
Afterwards, we identified the over-represented pathways in order to unravel the functional properties of the MEGs. The knowledge about the over-represented pathways from Reactome database [50] provides mechanistic insight into the MEGs and helps to decipher novel biological functions underlying the AAT disease mechanisms.
3. Results
Mainly focusing on the regular monotonic changes of gene expression profiles in liver-, spleen-, and lymph node tissues during the AAT disease progression, we analyzed in this study for each tissue the related MEG set and identified master regulators as well as over-represented pathways.
3.1. Master Regulator Analysis
The “upstream analysis” workflow [48] has been employed using the MEG sets of the tissues in order to computationally identify a variety of master regulators. As a result, we obtained altogether 10 unique master regulators for both breeds across all tissues as shown in Table 2. Remarkably, the vast majority of the master regulators are highly distinct between trypanosusceptible Boran and trypanotolerant N’Dama breeds, only PBX1 is found common for the spleen tissue of both breeds.
Table 2.
Master regulators of the breeds Boran and N’Dama.
| Boran | N’Dama | |
|---|---|---|
| Liver | MYC, E2F1, PPARG | DBP, PBX1, HOXA4, PPARA |
| Spleen | PITX2, E2F1, PBX1 | PBX1 |
| Lymph node | MYC, pSTAT1, PBX1 | DBP, PPARA |
3.1.1. Master Regulators in Liver
Using the “upstream analysis" workflow, we identified three master regulators (MYC, E2F1, PPARG) for the liver tissue of Boran and four master regulators (DBP, PBX1, HOXA4, PPARA) for N’Dama.
MYC is a member of the basic helix-loop-helix (bHLH) transcription factor family. It regulates a wide range of biological processes including metabolism, apoptosis, cell cycle, cell growth, angiogenesis or reprogramming in several tissues [52,53]. Importantly, MYC is highly pleiotropic [54] indicating that its deregulation is in close connection with all hematological malignancies, especially anaemia [55,56] which is a prominent feature of the AAT disease and also with drug resistance [56,57,58,59]. Furthermore, it has been reported as regulator of large networks of genes and has been associated with several cancer types, and is thus serving as a potential drug target [52,60,61,62]. Furthermore, it has been reported in the host-parasite interaction, improving the survival rate of parasites in surpassing immune surveillance mechanisms [63,64]. With regard to the parasite’s survival, MYC could be playing pivotal roles in induction and manipulation of host cell’s immunity in Animal African Trypanosomiasis as well. The master regulator E2F1 found for Boran liver, plays a critical role in bile acid synthesis as per a study performed in mouse model [65]. E2F1 inhibits the clearance of circulating cholesterol by regulating the expression of PCSK9 [66], which might be related to the parasite’s critical need of cholesterol-related metabolism from Boran’s body, implicating the progressive conditions of hypocholesteraemia and hypolipidaemia after infection [67]. Peroxisome proliferator-activated receptor gamma (PPARG), found as the third master regulator for Boran liver, belongs to the nuclear hormone receptor super family [68,69]. In liver, induction of PPARG overexpression as a result of pathophysiological stress, has led to lipid accumulation. Interestingly, blocking of PPARG gene expression has reduced the accumulation of lipids and the expression of inflammatory genes [70,71]. Therefore, PPARG is strongly associated not only with the lipid metabolism but also with inflammatory processes [72]. This suggests the role of PPARG in the induction of lipid metabolism by T. congolense to utilise a high amount of energy from Boran, resulting in weight loss and loss of body conditions in the cattle during the AAT disease.
Albumin D site-binding protein (DBP), found for the liver tissue of N’Dama, is a liver-enriched transcription factor [73] and plays important roles in circadian rhythm in the mammals [30,74]. Specifically, it influences the circadian transcriptional regulation of several liver-specific genes namely P450 genes such as Cyp2a4 and Cyp2a5 [75,76]. Belonging to the PAR bZIP basic leucine zipper family, DBP accumulates following a stringent circadian rhythm in liver cells [30]. The circadian control of the liver gene CYP7 encoding the cholesterol 7-hydroxylase enzyme, which catalyses the metabolism of cholesterol to bile acids [29,77,78], establishes the strong indispensable association of the circadian rhythm and DBP in cholesterol homeostasis. Remarkably, the expression of DBP was found upregulated in a tolerant mouse model after T. congolense infection, suggesting the strong link of DBP and trypanotolerance [79]. Our findings are further well-supported by the results in [34], in which he established the association of the circadian rhythm with the infection of T. congolense in rodents. Strikingly, the master regulator PPARA (Peroxisome proliferator-activated receptor ) is a ligand-induced nuclear receptor that is highly expressed in the liver of mammals [80,81]. PPARA is well-known for its transcriptional regulatory role in metabolic and inflammatory pathways, making it a potential therapeutic target [82,83,84]. Particularly, it plays a crucial role in several metabolic processes, including bile and amino acid metabolism, transportation and metabolism of lipids, fatty acid beta-oxidation, ketogenesis and lipogenesis [81,85,86], which could contribute to the protection of the host from worsening conditions of AAT like weight loss and hypolipidemia.
Furthermore, PBX1 (Pre-B-cell leukemia homeobox-1) is necessary for the maintenance of definitive hematopoiesis in the fetal liver, which indicates the host-protective role of PBX1 from anaemia [87] and thus contributing to trypanotolerance of N’Dama. Another master regulator HOXA4 from the homeobox family, is known for its role in hematopoiesis and B-cell progenitor population expansion [88], which implicates its importance in the production and maintenance of blood cells and immune cells, thus helping the cattle to control the major complications of AAT such as anaemia or parasitaemia.
3.1.2. Master Regulators in Spleen
The analysis of MEGs for the spleen tissues of the cattle breeds reveals that PBX1 is a common master regulator between Boran and N’Dama. It is essential for the spleen tissue-specific function of hematopoiesis [89]. Another key regulator, E2F1, found for the spleen tissue of Boran, has been reported as a suppressor of dendritic cell maturation [90], therefore implicating its role as a transcription factor for the immunosuppression in the infected cattle Boran. Macrophages and dendritic cells play a significant role in the innate immune system. In particular, they are involved in the production of interferon (IFN-), which is important for resistance against T. congolense [91]. Inhibition of dendritic cell maturation inhibits IFN- secretion [92], thus resulting in the reduction of the immune response against T. congolense [93]. The regulator E2F1 in Boran spleen may have a leading role in immune depression of Boran, thus contributing to the susceptibility of Boran to AAT.
The remaining master regulator PITX2, found for the Boran spleen tissue, is a member of the bicoid transcription factor family, which is involved in a wide variety of developmental processes [94]. However, the reason for its importance and potential role with respect to host-pathogen interaction is still unclear.
3.1.3. Master Regulators in Lymph Node
Investigation of the MEG sets of lymph node tissue unravelled three master regulators (MYC, pSTAT1, and PBX1) for Boran and two master regulators (DBP and PPARA) for N’Dama. MYC plays an essential role in immune suppression and immune evasion mechanisms in assisting cancer cells to avoid the host’s immunity, as suggested in cancer studies [95,96]. It might play a role in helping the trypanosomes to escape the immune check points in host immune surveillance mechanisms, suggesting a major player in parasitaemia in Boran’s body which is one of the major characteristics of the AAT disease. Strikingly, we identified pSTAT1 (signal transducer and activator of transcription 1) as the second master regulator. The role of STAT1 is strongly associated with the development of Th1 and Th17 responses which are CD4+ T-cell subsets [97,98,99]. This mainly implicates overproduction of pro-inflammatory cytokines (like IL-17) leading to cell death and inflammation, which connects the severity of anaemia in Boran [100,101]. The master regulator PBX1 has been studied in the homeostatic developmental programming of natural killer (NK) cells [102], which contributes to the main symptom of trypanosomiasis-associated acute anaemia as reported by [103].
DBP, identified as the master regulator in the lymph node of N’Dama, is a clock-controlled transcription factor and an important regulatory component of the circadian clock to ensure the 24 hour rhythm in mammalian species [104,105]. Several studies have reported the rhythmic expression of clock genes in cells of the immune system such as macrophages, dendritic cells and B-cells [106,107,108,109,110,111,112,113], representing the function of clock genes in immune responses. CD4+ T helper cells play crucial roles in the stimulation of effective antibody response and efficient isotype switching from IgM to IgG production [114,115,116], the critical features reported in N’Dama for its AAT tolerance [117]. These cells, being the significant regulators of adaptive immunity, harbor a circadian oscillator and generate cytokines such as IL-2, IL-4 and IFN- according to robust rhythms [118], implicating the tight connection of the circadian clock with adaptive immune responses during the AAT disease. Another interesting master regulator found for N’Dama is PPARA which has been reported to be expressed in B- and T-cells of the immune system [119,120]. Importantly, PPARA is known as the crucial regulator of immune responses such as inflammation and cytokine production [121,122,123]. According to its biological function in the immune system, PPARA could be protecting the depletion of the host’s cells from its own immune system during parasitic manipulation of immune responses, possibly controlling anaemia in N’Dama after trypanosome infection.
3.2. Pathway Analyses
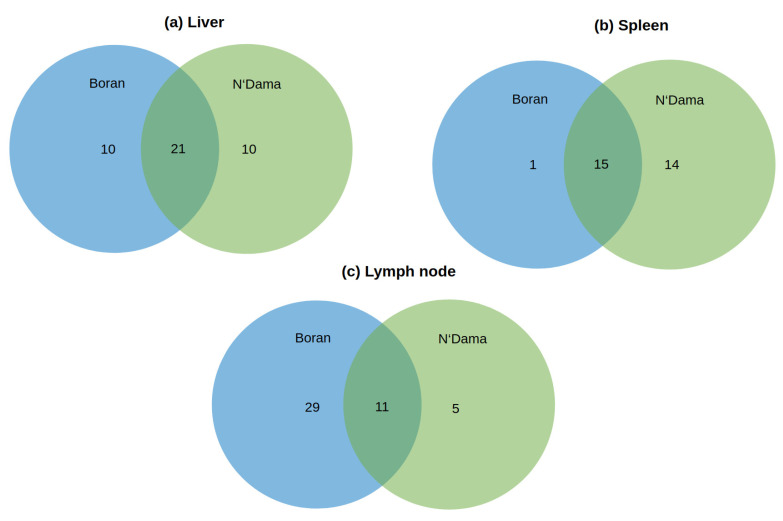
To further decipher the specific biological functions of MEGs regarding AAT disease mechanisms, we investigated the over-represented pathways using the Reactome pathway database [50] for the three tissues of Boran and N’Dama. All the over-represented pathways obtained from the analysis are listed in the Supplementary File S2 and the pathways unique for each tissue of the two breeds are shown in Table 3, Table 4 and Table 5. Mainly focusing on these pathways, we found that several of them are overlapping between the breeds (see Figure 2a–c). Interestingly, Figure 2b shows that there is only one pathway unique for the spleen tissue of Boran. Taking the liver tissue into account (Figure 2a), there are only 10 unique pathways obtained for each breed despite the big overlap. On the other hand, remarkably high numbers of pathways are found for the lymph node tissue of Boran, in comparison to N’Dama (Figure 2c).
Table 3.
Significantly over-represented pathways found for the liver tissue of Boran and N’Dama (p-adjusted ).
| Liver | |||
|---|---|---|---|
| Pathway Name | Hit Names | Adjusted p-Value | |
| Boran | Cellular responses to external stimuli | Arnt, Fos, Hif1a, Hsf1 | 4.64 × 10 |
| Regulation of beta-cell development | Foxo1, Hnf4g, Nkx2.2 | 0.0032 | |
| Regulation of Hypoxia-inducible Factor (HIF) by oxygen | Arnt, Hif1a | 0.0033 | |
| Cellular response to hypoxia | Arnt, Hif1a | 0.0033 | |
| Signaling by TGF-beta Receptor Complex | Myc, Smad3, Smad4 | 0.0036 | |
| Signaling by TGF-beta family members | Myc, Smad3, Smad4 | 0.0063 | |
| Signaling by NOTCH1 | Hif1a, Myc | 0.0105 | |
| Transcriptional activity of SMAD2/SMAD3:SMAD4 heterotrimer | Myc, Smad4 | 0.0147 | |
| Signaling by NOTCH | Hif1a, Myc | 0.0349 | |
| Interleukin-1 family signaling | Nfkb1, Smad3 | 0.0371 | |
| Cellular Senescence | Fos, Jun | 0.0416 | |
| N’Dama | PTEN Regulation | Atf, Jun | 0.0025 |
| Activation of HOX genes during differentiation | Hoxa4, Jun, Meis1 | 0.0036 | |
| Activation of anterior HOX genes in hindbrain development during early embryogenesis | Hoxa4, Jun, Meis1 | 0.0036 | |
| BMAL1:CLOCK, NPAS2 activates circadian gene expression | Dbp, Ppara | 0.0161 | |
| PIP3 activates AKT signaling | Atf, Jun | 0.0229 | |
| Transcriptional regulation of pluripotent stem cells | Pbx1, Pou5f1 | 0.0229 | |
| Intracellular signaling by second messengers | Atf2, Jun | 0.0280 | |
| Transcriptional regulation by RUNX2 | Sox9, Stat1 | 0.0364 | |
| Transcriptional regulation of white adipocyte differentiation | Pparg, Rxra | 0.0424 | |
| Circadian Clock | Dbp, Ppara | 0.0488 | |
Table 4.
Significantly over-represented pathways found for the spleen tissue of Boran and N’Dama (p-adjusted ).
| Spleen | |||
|---|---|---|---|
| Pathway Name | Hit Names | Adjusted p-Value | |
| Boran | POU5F1 (OCT4), SOX2, NANOG activate genes related to proliferation | Pou5f1, Stat3 | 0.0034 |
| N’Dama | Oxidative Stress Induced Senescence | Fos, Jun | 0.0033 |
| BMAL1:CLOCK NPAS2 activates circadian gene expression | Dbp, Ppara | 0.0052 | |
| MAPK6/MAPK4 signaling | Foxo1, Jun | 0.0052 | |
| Signaling by NOTCH3 | Hes1, Pbx1 | 0.0052 | |
| Cellular responses to stress | Fos, Hsf1, Jun | 0.0062 | |
| Fc epsilon receptor (FCERI) signaling | Fos, Jun | 0.0067 | |
| Cellular responses to external stimuli | Fos, Hsf1, Jun | 0.0135 | |
| MAPK family signaling cascades | Foxo1, Jun | 0.0166 | |
| Circadian Clock | Dbp, Ppara | 0.0166 | |
| Signaling by NOTCH | Hes1, Pbx1 | 0.0203 | |
| Generic Transcription Pathway | E2f1, Hes1, Sox9, Stat1, Tead1 | 0.0243 | |
| Cellular Senescence | Fos, Jun | 0.0243 | |
| RNA Polymerase II Transcription | E2f1, Hes1, Sox9, Stat1, Tead1 | 0.0350 | |
| Regulation of lipid metabolism by Peroxisome proliferator-activated receptor alpha (PPARalpha) | PPara, Rxra | 0.0432 | |
Table 5.
Significantly over-represented pathways found for the lymph node tissue of Boran and N’Dama (p-adjusted ).
| Lymph Node | |||
|---|---|---|---|
| Pathway Name | Hit Names | Adjusted p-Value | |
| Boran | MAP kinase activation in TLR cascade | Atf1, Atf2, Fos, Jun, Nfkb1 | 2.37 |
| Interleukin-17 signaling | Atf1, Atf2, Fos, Jun, Nfkb1 | 1.83 × 10 | |
| MAPK targets/ Nuclear events mediated by MAP kinases | Atf1, Atf2, Fos, Jun | 3.66 × 10 | |
| MyD88 cascade initiated on plasma membrane | Atf1, Atf2, Fos, Jun, Nfkb1 | 5.54 × 10 | |
| MyD88 dependent cascade initiated on endosome | Atf1, Atf2, Fos, Jun, Nfkb1 | 7.62 × 10 | |
| MyD88:Mal cascade initiated on plasma membrane | Atf1, Atf2, Fos, Jun, Nfkb1 | 1.03 × 10 | |
| MyD88-independent TLR4 cascade | Atf1, Atf2, Fos, Jun, Nfkb1 | 2.27 × 10 | |
| Toll Like Receptor 3 (TLR3) Cascade | Atf1, Atf2, Fos, Jun, Nfkb1 | 2.88 × 10 | |
| Toll-Like Receptors Cascades | Atf1, Atf2, Fos, Jun, Nfkb1 | 4.39 × 10 | |
| MAPK6/MAPK4 signaling | Foxo1, Jun, Myc | 4.66 × 10 | |
| Innate Immune System | Atf1, Atf2, Fos, Jun, Ltf, Nfkb1 | 9.27 × 10 | |
| Signaling by Interleukins | Atf1, Atf2, Fos, Jun, Nfkb1, Stat1, Stat3 | 0.0010 | |
| PTEN Regulation | Atf2, Jun | 0.0016 | |
| MAPK family signaling cascades | Foxo1, Jun, Myc | 0.0028 | |
| Oxidative Stress Induced Senescence | Fos, Jun | 0.0069 | |
| Cytokine Signaling in Immune system | Atf1, Atf2, Fos, Jun, Nfkb1, Stat1, Stat3 | 0.0081 | |
| Fc epsilon receptor (FCERI) signaling | Fos, Jun | 0.0138 | |
| PIP3 activates AKT signaling | Atf2, Jun | 0.0154 | |
| Transcriptional activity of SMAD2/SMAD3:SMAD4 heterotrimer | Myc, Smad4 | 0.0171 | |
| NGF signalling via TRKA from the plasma membrane | Atf1, Stat3 | 0.0171 | |
| Intracellular signaling by second messengers | Atf2, Jun | 0.0189 | |
| Immune System | Atf1, Atf2, Fos, Jun, Ltf, Nfkb1, Relb, Stat1, Stat3 | 0.0241 | |
| Transcriptional regulation by the AP-2 (TFAP2) family of transcription factors | Mybl2, Myc | 0.0311 | |
| Generic Transcription Pathway | E2f1, Mybl2, Myc, Smad4, Sox9, Stat1 | 0.0338 | |
| Mitotic G2-G2/M phases | Foxm1, Mybl2 | 0.0381 | |
| Mitotic G1-G1/S phases | E2f1, Mybl2 | 0.0381 | |
| Interleukin-1 family signaling | Nfkb1, Stat3 | 0.0430 | |
| Signaling by TGF-beta Receptor Complex | Myc, Smad4 | 0.0456 | |
| Cellular Senescence | Fos, Jun | 0.0482 | |
| N’Dama | POU5F1 (OCT4), SOX2, NANOG activate genes related to proliferation | Pou5f1, Stat3 | 0.0042 |
| BMAL1:CLOCK, NPAS2 activates circadian gene expression | Dbp, Ppara | 0.0078 | |
| Circadian Clock | Dbp, Ppara | 0.0244 | |
| Factors involved in megakaryocyte development and platelet production | Irf1, Irf2 | 0.0354 | |
| Interleukin-12 family signaling | Stat1, Stat3 | 0.0375 | |
Figure 2.
Venn diagram of over-represented pathways (p-adjusted ) obtained for liver-, spleen- and lymph node tissues of the two cattle breeds Boran and N’Dama after the infection of Trypanosoma congolense. Pathway enrichment analysis was performed based on the Reactome pathway database [50].
3.2.1. Over-Represented Pathways Found for Liver Tissue
Analysis of over-represented pathways for the liver tissue of Boran and N’Dama uncovered ten pathways unique for each breed (see Table 3 and Figure 2a ).
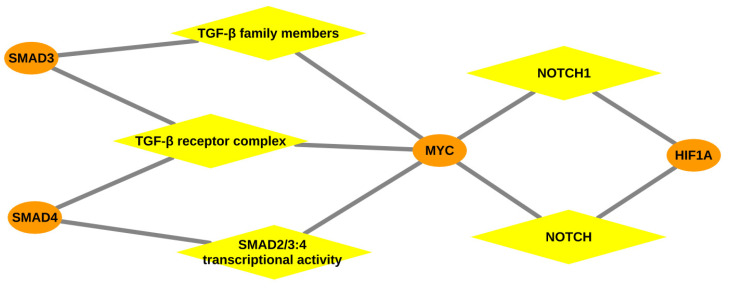
In Table 3, the top three over-represented pathways are associated with low oxygen environment and HIF accumulation due to parasitic infection [124,125] in the liver tissue of the trypanosusceptible breed Boran. Furthermore, the TGF- signaling pathway, which includes the TGF- receptor complex, TGF- family members and SMAD2/SMAD3:SMAD4 heterotrimer (shown in Figure 3), is reported as a critically important pathway for the parasite in mammalian cell invasion and to escape the host’s immune system [126,127]. Especially, this pathway is involved in the suppression of macrophages that are essential players against parasites [128,129], implicating immunosuppression [130,131] during AAT in Boran. Moreover, our findings also lend support to experimental studies on TGF- on other species of Trypanosoma [132,133]. Importantly, the interleukin-1 family signaling pathway found for Boran has been reported in direct association with damaging inflammation [134], which could explain the development of anaemia in Boran.
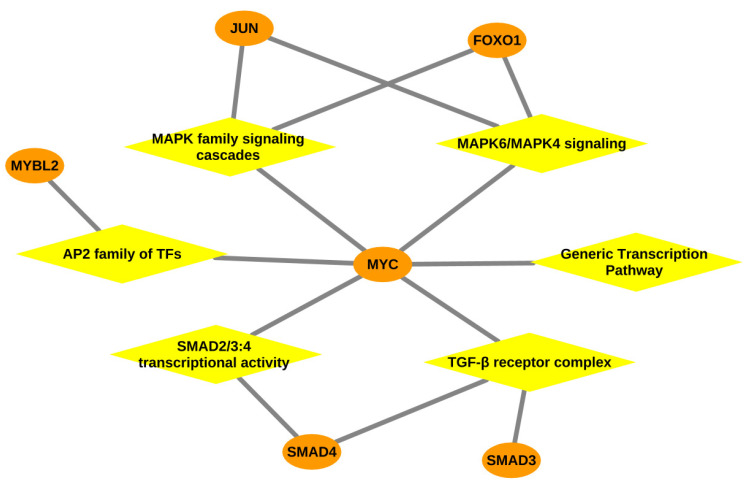
Figure 3.
Gene-pathway network: Network representing the association between the over-represented pathways and transcription factors especially MYC, depicted for the liver tissue of Boran. Orange coloured ellipses in the network represent the transcription factor genes and yellow coloured rhombuses indicate the over-represented pathways. The transcription factors are connected to the pathways, thereby forming a network of interactions between them.
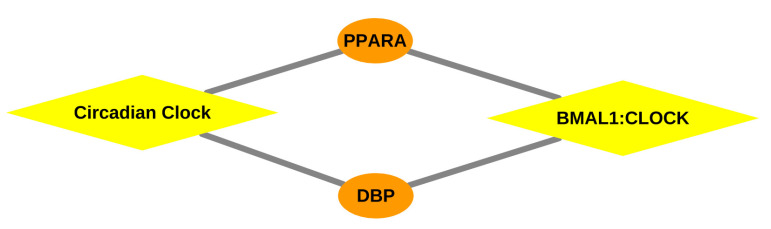
Regarding N’Dama’s liver tissue, the circadian clock and its components are inextricably in association with the transcriptional regulation of liver functions [135,136,137,138], suggesting the integrity of the circadian rhythm in the trypanotolerance mechanisms of N’Dama as shown in Table 3 and Figure 4. This finding is consistent with our previous results [27] and also a recent study by Solis et al. [31]. Intriguingly, the second and third over-represented pathways found for N’Dama are emphasizing the activation of HOX genes, which have been implicated as master regulator genes in the process of haematopoiesis [139]. Haematopoietic cells, derived mainly from fetal liver and bone marrow, are important in self-renewal and long-term supply of blood cells, especially T cells, which play a crucial role in the immune system [139,140,141,142]. These pathways strongly suggest their potential roles in protection of N’Dama from anaemia which is the most prominent feature of AAT disease.
Figure 4.
Gene-pathway network: Network representing the association between the over-represented pathways and transcription factors, especially DBP, depicted for the liver, spleen and lymph node tissue of N’Dama. Orange coloured ellipses in the network represent the transcription factor genes and yellow coloured rhombuses indicate the over-represented pathways. The transcription factors are connected to the pathways, thereby forming a network of interactions between them.
3.2.2. Over-Represented Pathways Found for Spleen Tissue
For the spleen tissue, we identified one unique significantly over-represented pathway for Boran and 14 significantly over-represented pathways for N’Dama (see Table 4 and Figure 2b).
The over-represented pathway found for Boran’s spleen tissue is related to the activation of genes during the proliferation by transcription factors POU5F1, SOX2, and NANOG. This pathway is also associated with the downstream processes related to self-renewal and pleuripotency in embryonic stem cells [143,144] which appears to be the normal function of spleen tissue in mammals.
Circadian clock related pathways in Table 4 can be categorised as the most prominent pathways in the spleen tissue due to the circadian control of splenic macrophages and B-cell development [107,145] (see Figure 4). In particular, these pathways are essential in the context of the trypanotolerance of N’Dama, since circadian regulation of immune responses are controlled at various levels in mammals [31,73]. Fundamentally, as reported in previous studies [22,23,26,146], MAPK family signalling cascades have been demonstrated to play critical roles in immune response through the production of pro-inflammatory cytokines in macrophages, suggesting their role in host defense against T. congolense in N’Dama [22,23,26,146]. Another striking pathway (in Table 4 and Figure 4) is related to the regulation of lipid metabolism by PPARA, which strongly establishes the relationship of spleen tissue with cholesterol metabolism in trypanotolerant N’Dama. Splenomegaly and hypocholesteraemia [67], being clinical signs of AAT, are indications of high workload of the reticuloendothelial system [147,148] for the parasite clearance in the blood. This pathway could be controlling the AAT conditions of splenomegaly and hypocholesteraemia in trypanotolerant N’Dama.
3.2.3. Over-Represented Pathways Found for Lymph Node Tissue
We identified 29 and 5 unique significantly over-represented pathways for lymph node tissue of Boran and N’Dama, respectively(see Table 5 and Figure 2c).
Inspection of Table 5 shows that we obtained a list of immune-related pathways for the lymph node tissue of Boran, suggesting the activation of immune cells in response to trypanosome infection. The toll-like receptor- and MyD88-related signalling pathways, being the major pathways for pathogen recognition in the innate immune system, have been reported as activated after protozoan infection [149]. Furthermore, activation of MAPK family signalling cascades, cytokine signalling, Fc epsilon RI signalling, interleukin-17 (IL-17) and interleukin-1 (IL-1) signalling strongly suggest that the inflammatory responses are following the cytokine production in response to T. congolense infection in Boran, as reported in previous studies [23,26,150]. Conversely, it seems quite possible that few pathways are under the manipulation of the parasite leading to the hyperproduction of proinflammatory cytokines resulting in catastrophic inflammation of host cells in Boran, especially involving MYC (see Figure 5). Particularly CD4+ T cells, which secrete IL-17, are reported in autoimmunity wherein IL-17 development is promoted by cytokines IL-1 and TGF- [151]. The autoimmune phenomena of Boran result in the chronic destruction of own cells mainly leading to severe anaemia. Moreover, the major immune-related MAPK family signalling cascade has been demonstrated as the targeted pathway for manipulation by T. congolense in the host to escape the host immune responses [150].
Figure 5.
Gene-pathway network: Network representing the association between the over-represented pathways and transcription factors especially MYC, depicted for the lymph node tissue of Boran. Orange coloured ellipses in the network represent the transcription factor genes and yellow coloured rhombuses indicate the over-represented pathways. The transcription factors are connected to the pathways, thereby forming a network of interactions between them.
For the lymph node tissue of N’Dama, two circadian clock related pathways have been found over-represented as shown in Table 5 and Figure 4, implicating the functioning of the immune system intimate accordance with the circadian clock as reported in several studies [31,33,152,153]. Important functional aspects of the immune responses such as phagocytosis, antigen presentation and immune regulation are regulated by the circadian clock [107], suggesting the circadian control of immunity against T. congolense infection in trypanotolerant N’Dama. Furthermore, interleukin-12 family signalling harbors IL-12, which is mainly leading to IFN- production which has been reported to be responsible for resistance to trypanosomiasis [154,155]. Remarkably, deletion of IL-12 in T. b. brucei and T. evansi infection models has resulted in the deficient IFN- production required for controlling parasitaemia [154], emphasizing the critical role of interleukin-12 family signalling in establishing resistance to AAT in N’Dama.
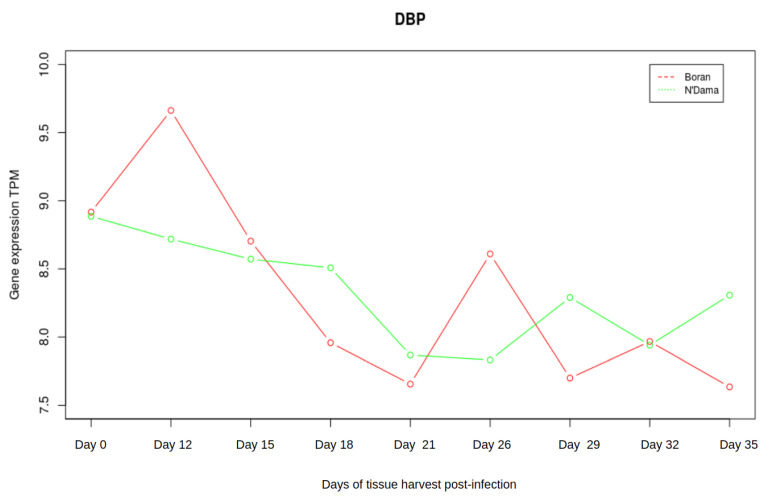
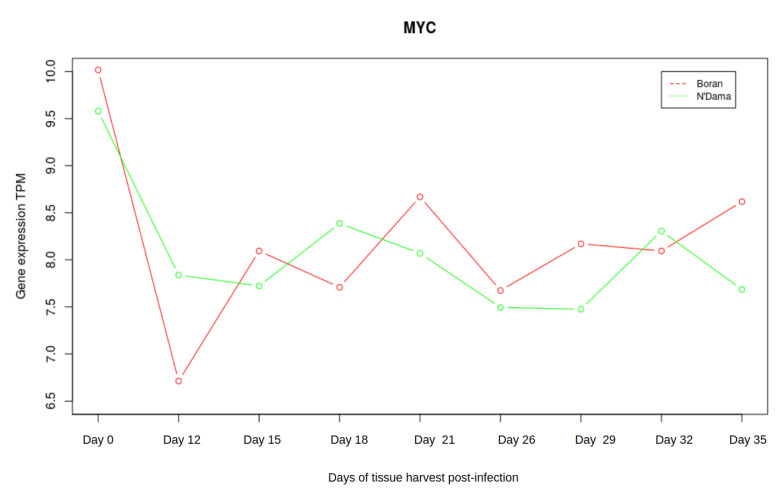
3.3. Analysis of Gene Expression Profiles of DBP and MYC
Taking the liver tissue into account, the microarray data set consisted of gene expression profiles for nine timepoints namely day 0, days 12, 15, 18, 21, 26, 29, 32, and 35. Emphasizing the crucial roles of the two master regulators DBP and MYC, we were interested in additionally investigating the changes in gene expression pattern of DBP and MYC of Boran and N’Dama during the disease progression. Interestingly, we observed slight antagonistic patterns of gene expression at different stages of the AAT disease, although both of these genes are not differentially expressed. The expression of DBP is abruptly declining for Boran from timepoint 2 (see Figure 6). Then, DBP increases its expression slightly and again declines towards the later stages. In contrast, the expression of DBP shows an increasing trend towards the later stages in N’Dama, despite the continuous steady decrease in its expression at earlier timepoints. It might be important to consider the expression of DBP during the later stages of the disease progression. AAT could be exhibiting similar effect in both cattle breeds during the earlier timepoints of infection. On the other hand, the expression of MYC seems quite clear for Boran with increasing tendency at the later timepoints (as shown in Figure 7). Whereas for N’Dama, MYC decreases its expression at several timepoints. These minor changes could be greatly contributing to susceptibility or tolerance mechanisms of both cattle breeds.
Figure 6.
Expression of DBP. The red line in the plot corresponds to Boran whereas the green line corresponds to the breed N’Dama. In the early timepoints, expression of DBP reaches a peak in Boran and then starts to drop down. After the timepoint 5, the curve again increases slightly and at the later stages, it falls down again. On the other hand, the expression of DBP in N’Dama steadily drops until the timepoint 5, then it gradually increases.
Figure 7.
Expression of MYC.The red line in the plot corresponds to Boran whereas the green line corresponds to the breed N’Dama. In the early timepoints, expression of MYC decreases in both Boran and N’Dama. At the later stage, the expression of MYC increases for Boran whereas it decreases for N’Dama.
4. Discussion
African Animal Trypanosomiasis (AAT) is a vector-borne disease spread through the tsetse fly by carrying pathogenic African trypanosomes in its saliva. Clinical signs such as anaemia, hepatomegaly and splenomegaly are displayed in the cattle during the course of the AAT disease, which gradually progresses in multiple steps. Based on its signs, the AAT disease shows a multi-stage progression process in the body of the animal. Previous studies have pointed out that the consideration of monotonic expression patterns of genes (MEGs) could reflect the stage-by-stage progression of the disease [47,156]. Thus, we analysed several MEG sets in this study to identify master regulators which govern the transcriptional machinery of tissue-specific gene expression and thus influencing trypanosusceptibility and trypanotolerance of the breeds Boran and N’Dama, respectively. For this purpose, the consideration of the three tissues, liver, spleen, and lymph nodes are quintessential since they are the primary target sites of trypanosome infection. Inextricably, these tissues play crucial roles in generating host immune responses especially by increasing the number of macrophages, which results in the production of pro-inflammatory cytokines [35,146].
Remarkably, our findings suggest that the master regulators DBP and MYC identified for liver and lymph node tissues, appear to be greatly influencing the genetic programs for trypanosusceptibility and trypanotolerance mechanisms in Boran and N’Dama. Notably, DBP could be supporting the regulation of immune responses [27,31,73,153,157] beccause of its function in the circadian oscillatory mechanism [105] thereby establishing trypanotolerance in N’Dama. On the other hand, MYC has been reported to be responsible for the disruption of the circadian clock in cancer cells [158,159,160], elucidating the possibility of a dysfunctional circadian rhythm in Boran. Furthermore, MYC has gained its importance as it directly programs inflammation and immune suppression [96], which are constantly reported conditions in trypanosome-infected Boran.
Kupffer cells, the largest immune cell population of macrophages resident in the liver tissue, play a critical role in the mononuclear phagocytic system mounting the first line of immune response to foreign antigens [161]. Immune responses in the liver tissue depend on the activation state of macrophages [161,162]. M1 and M2 polarization of macrophages are known as two extremes in which M1 (classically activated) is characterised by expression of high pro-inflammatory cytokines and M2 (alternatively activated) by high anti-inflammatory cytokines [162,163]. Surprisingly, all three master regulators MYC, E2F1 and PPARG identified for the liver tissue of Boran in this study, have been reported as the regulators necessary for M2-like polarization of macrophages [164], which could be an advantage for the trypanosomes to increase their survival inside the host’s body, and thereby contributing to enhanced parasitaemia in Boran.
In order to gain more mechanistic insights and to discover novel biological functions underlying the AAT disease progression of both breeds, the investigation of over-represented pathways based on the MEG sets of tissues is crucial. Based on pathway analysis, we obtained a number of over-represented pathways (see Supplementary File S2), several of which are in agreement with the results of previous studies [23,26,150] and are activated due to trypanosome infection in both breeds. Remarkably, the majority of these pathways were found to be common for both cattle breeds, while few of them are unique and breed-specific which could provide an important clue for distinguishing the biological processes controlling the mechanisms underlying trypanosusceptibility or trypanotolerance of the cattle breeds. Consequently, we focused in this study on outlining the potential roles of breed-specific unique pathways (see Table 3, Table 4 and Table 5) in association with the level of trypanotolerance in the respective cattle breeds. Although we reported the major immune-related pathways in Boran, these pathways could be leading to inflammation due to hyperproduction of pro-inflammatory cytokines in the host cells [165], thereby contributing to susceptibility of this breed. Despite the activation of immune signalling pathways, dysregulation causes the death of infected animals, especially dysregulated cytokine networks and overproduction of inflammatory cytokines (hallmark of African Trypanosomiasis) [146]. Contrarily, circadian clock related pathways (see Figure 4), interleukin-12 family signalling, regulation of lipid metabolism, and MAPK family signalling cascades might be properly regulated in N’Dama, indicating the underlying mechanism for trypanotolerance in N’Dama during the AAT disease. Especially, the pathways related to the circadian clock bolster our previous findings [27] in highlighting the important role of DBP and circadian rhythm in the coordination of the immune responses in trypanotolerant breed N’Dama.
Today it is well-known that the knowledge about master regulators is fundamental since they greatly control the TFs and the related genes [166,167]. Further, it is also pivotal to understand the regulatory network of TFs that cooperatively regulate a large number of genes during a disease process [168]. In our previous study [27], by analysing the promoter regions of the MEGs, we reported the importance of several TFs and their preferential partner choices elucidating their roles during the AAT disease progression. The consideration of TFs and their cooperations only provides the information regarding the first level of the transcriptional regulatory hierarchy [168]. However, for gaining a proper understanding of the disease progress in both breeds, it is still necessary to establish the hierarchy of the transcriptomic regulation in order to identify the master regulators [166,167,168]. Thus, our main objective in this study was to identify the master regulators together with signal transduction pathways associated with the AAT disease as potential drug targets, to complement our previous study [27]. Our current study provides a combined knowledge along with our previous findings. On one hand, it evidently indicates that DBP functions more as a master regulator of the circadian clock in peripheral tissues, supporting the trypanotolerance mechanisms in the cattle breed N’Dama. On the other hand, our analysis remarkably leads to the identification of novel master regulator MYC in association with the trypanosusceptibility mechanism of Boran.
Taken together, the systematic investigation of the upstream master regulators and over-represented pathways governing the regulatory mechanisms of the trypanotolerance level of two cattle breeds could provide novel mechanistic insights into the tissue- and breed-specific genetic programs. In particular, we identified MYC and DBP (as represented in Figure 3, Figure 4 and Figure 5) as potential discriminators between the two cattle breeds, trypanosusceptible Boran and trypanotolerant N’Dama, which are likely to be promising therapeutic targets for future works and for the selective breeding of this trait.
Acknowledgments
We acknowledge support by the German Research Foundation and the Open Access Publication Funds of the Göttingen University. We would like to thank Selina Klees, Faisal Ramzan, Martin Wutke and Felix Heinrich for proofreading the manuscript and providing helpful advices and discussions.
Supplementary Materials
The following are available online at https://www.mdpi.com/1422-0067/22/2/562/s1, File S1: Lists of Monotonically Expressed Genes obtained from the MFSelector approach, File S2: Lists of all over-represented pathways obtained for liver-, spleen- and lymph node tissues of Boran and N’Dama. The common pathways between the breeds are highlighted in red.
Author Contributions
M.G. designed and supervised the research. A.R. participated in the design of the study and conducted computational analyses together with M.G. and performed the literature survey. A.O.S. interpreted the results with A.R. and M.G. A.R. and M.G. wrote the final version of the manuscript. M.G. conceived of and managed the project. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steverding D. Arthropod Borne Diseases. Springer; Berlin/Heidelberg, Germany: 2016. Sleeping Sickness and Nagana Disease Caused by Trypanosoma; p. 277. [Google Scholar]
- 2.Steverding D. The history of African trypanosomiasis. Parasites Vectors. 2008 doi: 10.1186/1756-3305-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hursey B., Slingenbergh J. The tsetse fly and its effects on agriculture in sub-Saharan Africa. World Anim. Rev. 1995;3–4:67–73. [Google Scholar]
- 4.Losos G.J., Ikede B. Review of pathology of diseases in domestic and laboratory animals caused by Trypanosoma congolense, T. vivax, T. brucei, T. rhodesiense and T. gambiense. Vet. Pathol. 1972;9:1–79. doi: 10.1177/030098587200901s01. [DOI] [Google Scholar]
- 5.Giordani F., Morrison L.J., Rowan T.G., De Koning H.P., Barrett M.P. The animal trypanosomiases and their chemotherapy: A review. Parasitology. 2016;143:1862–1889. doi: 10.1017/S0031182016001268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angara T., Ismail A., Ibrahim A. Research Paper Veterinary An Overview on the Economic Impacts of Animal Trypanosomiasis. Global Journal for Research Analysis; Ahmedabad, India: 2014. [Google Scholar]
- 7.Morrison L.J., Vezza L., Rowan T., Hope J.C. Animal African trypanosomiasis: Time to increase focus on clinically relevant parasite and host species. Trends Parasitol. 2016;32:599–607. doi: 10.1016/j.pt.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Naessens J. Bovine trypanotolerance: A natural ability to prevent severe anaemia and haemophagocytic syndrome? Int. J. Parasitol. 2006 doi: 10.1016/j.ijpara.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Murray M., Trail J.C., Davis C.E., Black S.J. Genetic resistance to African trypanosomiasis. J. Infect. Dis. 1984 doi: 10.1093/infdis/149.3.311. [DOI] [PubMed] [Google Scholar]
- 10.Murray M., Morrison W.I., Whitelaw D. Host susceptibility to African trypanosomiasis: Trypanotolerance. Adv. Parasitol. 1982;21:1–68. doi: 10.1016/s0065-308x(08)60274-2. [DOI] [PubMed] [Google Scholar]
- 11.Courtin D., Berthier D., Thevenon S., Dayo G.K., Garcia A., Bucheton B. Host genetics in African trypanosomiasis. Infect. Genet. Evol. 2008 doi: 10.1016/j.meegid.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Starkey P. N’Dama Cattle—A Productive Trypanotolerant Breed. FAO World Anim. Rev. 1984;50:2–15. [Google Scholar]
- 13.Dargie J., Murray P., Murray M., Grimshaw W., McIntyre W. Bovine trypanosomiasis: The red cell kinetics of Ndama and Zebu cattle infected with Trypanosoma congolense. Parasitology. 1979;78:271–286. doi: 10.1017/S0031182000051143. [DOI] [PubMed] [Google Scholar]
- 14.Hassan F.A. The Origins and Development of African Livestock: Archaeology, Genetics, Linguistics and Ethnography. University College London Press, Taylor & Francis Group; Oxford, UK: 2006. Climate and cattle in North Africa: A first approximation; p. 61. [Google Scholar]
- 15.Mattioli R., Wilson R. Trypanosomes, tsetse and trypanotolerance: Coevolution in tropical Africa. Parassitologia. 1996;38:531–535. [PubMed] [Google Scholar]
- 16.Paling R., Moloo S., Scott J., Gettinby G., McOdimba F., Murray M. Susceptibility of N’Dama and Boran cattle to sequential challenges with tsetse-transmitted clones of Trypanosoma congolense. Parasite Immunol. 1991;13:427–445. doi: 10.1111/j.1365-3024.1991.tb00295.x. [DOI] [PubMed] [Google Scholar]
- 17.Murray M., Trail J., d’Ieteren G. Trypanotolerance in cattle and prospects for the control of trypanosomiasis by selective breeding. Rev. Sci. Tech. 1990;9:369–386. doi: 10.20506/rst.9.2.506. [DOI] [PubMed] [Google Scholar]
- 18.Roelants G.E. Natural resistance to African trypanosomiasis. Parasite Immunol. 1986 doi: 10.1111/j.1365-3024.1986.tb00828.x. [DOI] [PubMed] [Google Scholar]
- 19.Epstein H. The Origin of the Domestic Animals of Africa. Africana Publishing Corporation; New York, NY, USA: 1971. [Google Scholar]
- 20.Mekonnen Y.A., Gültas M., Effa K., Hanotte O., Schmitt A.O. Identification of Candidate Signature Genes and Key Regulators Associated With Trypanotolerance in the Sheko Breed. Front. Genet. 2019;10:1095. doi: 10.3389/fgene.2019.01095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim S.J., Ka S., Ha J.W., Kim J., Yoo D., Kim K., Lee H.K., Lim D., Cho S., Hanotte O., et al. Cattle genome-wide analysis reveals genetic signatures in trypanotolerant N’Dama. BMC Genom. 2017;18:371. doi: 10.1186/s12864-017-3742-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Gorman G.M., Park S.D., Hill E.W., Meade K.G., Coussens P.M., Agaba M., Naessens J., Kemp S.J., MacHugh D.E. Transcriptional profiling of cattle infected with Trypanosoma congolense highlights gene expression signatures underlying trypanotolerance and trypanosusceptibility. BMC Genom. 2009;10:207. doi: 10.1186/1471-2164-10-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher P., Hedeler C., Wolstencroft K., Hulme H., Noyes H., Kemp S., Stevens R., Brass A. A systematic strategy for large-scale analysis of genotype–phenotype correlations: Identification of candidate genes involved in African trypanosomiasis. Nucleic Acids Res. 2007;35:5625–5633. doi: 10.1093/nar/gkm623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill E.W., O’Gorman G.M., Agaba M., Gibson J.P., Hanotte O., Kemp S.J., Naessens J., Coussens P.M., MacHugh D.E. Understanding bovine trypanosomiasis and trypanotolerance: The promise of functional genomics. Vet. Immunol. Immunopathol. 2005;105:247–258. doi: 10.1016/j.vetimm.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Hanotte O., Ronin Y., Agaba M., Nilsson P., Gelhaus A., Horstmann R., Sugimoto Y., Kemp S., Gibson J., Korol A., et al. Mapping of quantitative trait loci controlling trypanotolerance in a cross of tolerant West African N’Dama and susceptible East African Boran cattle. Proc. Natl. Acad. Sci. USA. 2003;100:7443–7448. doi: 10.1073/pnas.1232392100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noyes H., Brass A., Obara I., Anderson S., Archibald A.L., Bradley D.G., Fisher P., Freeman A., Gibson J., Gicheru M., et al. Genetic and expression analysis of cattle identifies candidate genes in pathways responding to Trypanosoma congolense infection. Proc. Natl. Acad. Sci. USA. 2011;108:9304–9309. doi: 10.1073/pnas.1013486108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rajavel A., Heinrich F., Schmitt A.O., Gültas M. Identifying Cattle Breed-Specific Partner Choice of Transcription Factors during the African Trypanosomiasis Disease Progression Using Bioinformatics Analysis. Vaccines. 2020;8:246. doi: 10.3390/vaccines8020246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lopez-Molina L., Conquet F., Dubois-Dauphin M., Schibler U. The DBP gene is expressed according to a circadian rhythm in the suprachiasmatic nucleus and influences circadian behavior. EMBO J. 1997;16:6762–6771. doi: 10.1093/emboj/16.22.6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fonjallaz P., Ossipow V., Wanner G., Schibler U. The two PAR leucine zipper proteins, TEF and DBP, display similar circadian and tissue-specific expression, but have different target promoter preferences. EMBO J. 1996;15:351–362. doi: 10.1002/j.1460-2075.1996.tb00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wuarin J., Schibler U. Expression of the liver-enriched transcriptional activator protein DBP follows a stringent circadian rhythm. Cell. 1990;63:1257–1266. doi: 10.1016/0092-8674(90)90421-A. [DOI] [PubMed] [Google Scholar]
- 31.Orozco-Solis R., Aguilar-Arnal L. Circadian Regulation of Immunity Through Epigenetic Mechanisms. Front. Cell. Infect. Microbiol. 2020;10:96. doi: 10.3389/fcimb.2020.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barik S. Molecular Interactions between Pathogens and the Circadian Clock. Int. J. Mol. Sci. 2019;20:5824. doi: 10.3390/ijms20235824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scheiermann C., Kunisaki Y., Frenette P.S. Circadian control of the immune system. Nat. Rev. Immunol. 2013;13:190–198. doi: 10.1038/nri3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hawking F. Circadian rhythms of Trypanosoma congolense in laboratory rodents. Trans. R. Soc. Trop. Med. Hyg. 1978;72:592–595. doi: 10.1016/0035-9203(78)90008-1. [DOI] [PubMed] [Google Scholar]
- 35.Taylor K.A. Immune responses of cattle to African trypanosomes: Protective or pathogenic? Int. J. Parasitol. 1998;28:219–240. doi: 10.1016/S0020-7519(97)00154-9. [DOI] [PubMed] [Google Scholar]
- 36.Andrianarivo A.G., Muiya P., Opollo M., Loganhenfrey L.L. Trypanosoma congolense: Comparative Effects of a Primary Infection on Bone Marrow Progenitor Cells from N’Dama and Boran Cattle. Exp. Parasitol. 1995;80:407–418. doi: 10.1006/expr.1995.1053. [DOI] [PubMed] [Google Scholar]
- 37.Ramzan F., Klees S., Schmitt A.O., Cavero D., Gültas M. Identification of Age-Specific and Common Key Regulatory Mechanisms Governing Eggshell Strength in Chicken Using Random Forests. Genes. 2020;11:464. doi: 10.3390/genes11040464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wlochowitz D., Haubrock M., Arackal J., Bleckmann A., Wolff A., Beißbarth T., Wingender E., Gültas M. Computational identification of key regulators in two different colorectal cancer cell lines. Front. Genet. 2016;7:42. doi: 10.3389/fgene.2016.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hosen M.R., Goody P.R., Zietzer A., Nickenig G., Jansen F. MicroRNAs as master regulators of atherosclerosis: From pathogenesis to novel therapeutic options. Antioxidants Redox Signal. 2020 doi: 10.1089/ars.2020.8107. [DOI] [PubMed] [Google Scholar]
- 40.Cai W., Zhou W., Han Z., Lei J., Zhuang J., Zhu P., Wu X., Yuan W. Master regulator genes and their impact on major diseases. PeerJ. 2020;8:e9952. doi: 10.7717/peerj.9952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ziegler Y., Laws M.J., Guillen V.S., Kim S.H., Dey P., Smith B.P., Gong P., Bindman N., Zhao Y., Carlson K., et al. Suppression of FOXM1 activities and breast cancer growth in vitro and in vivo by a new class of compounds. NPJ Breast Cancer. 2019;5:1–11. doi: 10.1038/s41523-019-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Picaud S., Leonards K., Lambert J.P., Dovey O., Wells C., Fedorov O., Monteiro O., Fujisawa T., Wang C.Y., Lingard H., et al. Promiscuous targeting of bromodomains by bromosporine identifies BET proteins as master regulators of primary transcription response in leukemia. Sci. Adv. 2016;2:e1600760. doi: 10.1126/sciadv.1600760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barillot E., Calzone L., Hupe P., Vert J.P., Zinovyev A. Computational Systems Biology of Cancer. CRC Press; Boca Raton, FL, USA: 2012. [Google Scholar]
- 44.Mellman I. Dendritic cells: Master regulators of the immune response. Cancer Immunol. Res. 2013;1:145–149. doi: 10.1158/2326-6066.CIR-13-0102. [DOI] [PubMed] [Google Scholar]
- 45.Vargas D.M.d., De Bastiani M.A., Zimmer E.R., Klamt F. Alzheimer’s disease master regulators analysis: Search for potential molecular targets and drug repositioning candidates. Alzheimer Res. Ther. 2018;10:59. doi: 10.1186/s13195-018-0394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pan Z., Li L., Fang Q., Qian Y., Zhang Y., Zhu J., Ge M., Huang P. Integrated bioinformatics analysis of master regulators in anaplastic thyroid carcinoma. BioMed Res. Int. 2019;2019 doi: 10.1155/2019/9734576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang H.W., Sun H.J., Chang T.Y., Lo H.H., Cheng W.C., Tseng G.C., Lin C.T., Chang S.J., Pal N.R., Chung I.F. Discovering monotonic stemness marker genes from time-series stem cell microarray data. B Genom. Biomed. Cent. 2015;16:S2. doi: 10.1186/1471-2164-16-S2-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wingender E., Kel A.E. geneXplain — eine integrierte Bioinformatik-Plattform. BIOspektrum. 2012;18:554–556. doi: 10.1007/s12268-012-0228-2. [DOI] [Google Scholar]
- 49.Koschmann J., Bhar A., Stegmaier P., Kel A.E., Wingender E. “Upstream analysis”: An integrated promoter-pathway analysis approach to causal interpretation of microarray data. Microarrays. 2015;4:270–286. doi: 10.3390/microarrays4020270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jassal B., Matthews L., Viteri G., Gong C., Lorente P., Fabregat A., Sidiropoulos K., Cook J., Gillespie M., Haw R., et al. The reactome pathway knowledgebase. Nucleic Acids Res. 2019;48:D498–D503. doi: 10.1093/nar/gkz1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chan S.S.K., Kyba M. What is a master regulator? J. Stem Cell Res. Ther. 2013;3:114. doi: 10.4172/2157-7633.1000e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benetatos L., Benetatou A., Vartholomatos G. Enhancers and MYC interplay in hematopoiesis. J. Mol. Med. 2020 doi: 10.1007/s00109-020-01891-1. [DOI] [PubMed] [Google Scholar]
- 53.Casey S.C., Tong L., Li Y., Do R., Walz S., Fitzgerald K.N., Gouw A.M., Baylot V., Gütgemann I., Eilers M., et al. MYC regulates the antitumor immune response through CD47 and PD-L1. Science. 2016 doi: 10.1126/science.aac9935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Conacci-Sorrell M., McFerrin L., Eisenman R.N. An overview of MYC and its interactome. Cold Spring Harb. Perspect. Med. 2014 doi: 10.1101/cshperspect.a014357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Delgado M.D., León J. Myc roles in hematopoiesis and leukemia. Genes Cancer. 2010;1:605–616. doi: 10.1177/1947601910377495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guo Y., Niu C., Breslin P., Tang M., Zhang S., Wei W., Kini A.R., Paner G.P., Alkan S., Morris S.W., et al. c-Myc–mediated control of cell fate in megakaryocyte-erythrocyte progenitors. Blood, J. Am. Soc. Hematol. 2009;114:2097–2106. doi: 10.1182/blood-2009-01-197947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ohanian M., Rozovski U., Kanagal-Shamanna R., Abruzzo L.V., Loghavi S., Kadia T., Futreal A., Bhalla K., Zuo Z., Huh Y.O., et al. MYC protein expression is an important prognostic factor in acute myeloid leukemia. Leuk. Lymphoma. 2019;60:37–48. doi: 10.1080/10428194.2018.1464158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weng S., Matsuura S., Mowery C.T., Stoner S.A., Lam K., Ran D., Davis A.G., Lo M.C., Zhang D.E. Restoration of MYC-repressed targets mediates the negative effects of GM-CSF on RUNX1-ETO leukemogenicity. Leukemia. 2017;31:159–169. doi: 10.1038/leu.2016.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Matsushita H., Nakajima H., Nakamura Y., Tsukamoto H., Tanaka Y., Jin G., Yabe M., Asai S., Ono R., Nosaka T., et al. C/EBPα and C/EBPϵ induce the monocytic differentiation of myelomonocytic cells with the MLL-chimeric fusion gene. Oncogene. 2008;27:6749–6760. doi: 10.1038/onc.2008.285. [DOI] [PubMed] [Google Scholar]
- 60.Shroff E.H., Eberlin L.S., Dang V.M., Gouw A.M., Gabay M., Adam S.J., Bellovin D.I., Trand P.T., Philbrick W.M., Garcia-Ocana A., et al. MYC oncogene overexpression drives renal cell carcinoma in a mouse model through glutamine metabolism. Proc. Natl. Acad. Sci. USA. 2015 doi: 10.1073/pnas.1507228112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ventura A., Kirsch D.G., McLaughlin M.E., Tuveson D.A., Grimm J., Lintault L., Newman J., Reczek E.E., Weissleder R., Jacks T. Restoration of p53 function leads to tumour regression in vivo. Nature. 2007 doi: 10.1038/nature05541. [DOI] [PubMed] [Google Scholar]
- 62.Hoffman B., Amanullah A., Shafarenko M., Liebermann D.A. The proto-oncogene c-myc in hematopoietic development and leukemogenesis. Oncogene. 2002 doi: 10.1038/sj.onc.1205400. [DOI] [PubMed] [Google Scholar]
- 63.Franco M., Shastri A.J., Boothroyd J.C. Infection by Toxoplasma gondii specifically induces host c-Myc and the genes this pivotal transcription factor regulates. Eukaryot. Cell. 2014;13:483–493. doi: 10.1128/EC.00316-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dessauge F., Hilaly S., Baumgartner M., Blumen B., Werling D., Langsley G. c-Myc activation by Theileria parasites promotes survival of infected B-lymphocytes. Oncogene. 2005;24:1075–1083. doi: 10.1038/sj.onc.1208314. [DOI] [PubMed] [Google Scholar]
- 65.Zhang Y., Xu N., Xu J., Kong B., Copple B., Guo G.L., Wang L. E2F1 is a novel fibrogenic gene that regulates cholestatic liver fibrosis through the Egr-1/SHP/EID1 network. Hepatology. 2014;60:919–930. doi: 10.1002/hep.27121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lai Q., Giralt A., Le May C., Zhang L., Cariou B., Denechaud P.D., Fajas L. E2F1 inhibits circulating cholesterol clearance by regulating Pcsk9 expression in the liver. JCI Insight. 2017;2 doi: 10.1172/jci.insight.89729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Biryomumaisho S., Katunguka-Rwakishaya E., Rubaire-Akiiki C. Serum biochemical changes in experimental Trypanosoma congolense and Trypanosoma brucei infection in Small East Africa goats. Vet. Arh. 2003;73:167–180. [Google Scholar]
- 68.Tyagi S., Gupta P., Saini A.S., Kaushal C., Sharma S. The peroxisome proliferator-activated receptor: A family of nuclear receptors role in various diseases. J. Adv. Pharm. Technol. Res. 2011;2:236. doi: 10.4103/2231-4040.90879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barak Y., Nelson M.C., Ong E.S., Jones Y.Z., Ruiz-Lozano P., Chien K.R., Koder A., Evans R.M. PPARγ is required for placental, cardiac, and adipose tissue development. Mol. Cell. 1999;4:585–595. doi: 10.1016/S1097-2765(00)80209-9. [DOI] [PubMed] [Google Scholar]
- 70.Hasenfuss S.C., Bakiri L., Thomsen M.K., Williams E.G., Auwerx J., Wagner E.F. Regulation of steatohepatitis and PPARγ signaling by distinct AP-1 dimers. Cell Metab. 2014;19:84–95. doi: 10.1016/j.cmet.2013.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yamazaki T., Shiraishi S., Kishimoto K., Miura S., Ezaki O. An increase in liver PPARγ2 is an initial event to induce fatty liver in response to a diet high in butter: PPARγ2 knockdown improves fatty liver induced by high-saturated fat. J. Nutr. Biochem. 2011;22:543–553. doi: 10.1016/j.jnutbio.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 72.Katunguka-Rwakishaya E., Murray M., Holmes P. Pathophysiology of Trypanosoma congolense infection in two breeds of sheep, Scottish blackface and Finn Dorset. Vet. Parasitol. 1997;68:215–225. doi: 10.1016/S0304-4017(96)01075-8. [DOI] [PubMed] [Google Scholar]
- 73.Bozek K., Relógio A., Kielbasa S.M., Heine M., Dame C., Kramer A., Herzel H. Regulation of clock-controlled genes in mammals. PLoS ONE. 2009;4:e4882. doi: 10.1371/journal.pone.0004882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Takahashi J.S. Molecular components of the circadian clock in mammals. Diabetes, Obes. Metab. 2015;17:6–11. doi: 10.1111/dom.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schrem H., Klempnauer J., Borlak J. Liver-enriched transcription factors in liver function and development. Part II: The C/EBPs and D site-binding protein in cell cycle control, carcinogenesis, circadian gene regulation, liver regeneration, apoptosis, and liver-specific gene regulation. Pharmacol. Rev. 2004;56:291–330. doi: 10.1124/pr.56.2.5. [DOI] [PubMed] [Google Scholar]
- 76.Lavery D.J., Lopez-Molina L., Margueron R., Fleury-Olela F., Conquet F., Schibler U., Bonfils C. Circadian expression of the steroid 15 α-hydroxylase (Cyp2a4) and coumarin 7-hydroxylase (Cyp2a5) genes in mouse liver is regulated by the PAR leucine zipper transcription factor DBP. Mol. Cell. Biol. 1999;19:6488–6499. doi: 10.1128/MCB.19.10.6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee Y.H., Alberta J.A., Gonzalez F.J., Waxman D.J. Multiple, functional DBP sites on the promoter of the cholesterol 7 alpha-hydroxylase P450 gene, CYP7. Proposed role in diurnal regulation of liver gene expression. J. Biol. Chem. 1994;269:14681–14689. [PubMed] [Google Scholar]
- 78.Lavery D.J., Schibler U. Circadian transcription of the cholesterol 7 alpha hydroxylase gene may involve the liver-enriched bZIP protein DBP. Genes Dev. 1993;7:1871–1884. doi: 10.1101/gad.7.10.1871. [DOI] [PubMed] [Google Scholar]
- 79.Kierstein S., Noyes H., Naessens J., Nakamura Y., Pritchard C., Gibson J., Kemp S., Brass A. Gene expression profiling in a mouse model for African trypanosomiasis. Genes Immun. 2006;7:667–679. doi: 10.1038/sj.gene.6364345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kersten S., Rakhshandehroo M., Knoch B., Müller M. Peroxisome proliferator-activated receptor alpha target genes. PPAR Res. 2010 doi: 10.1155/2010/612089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mandard S., Müller M., Kersten S. Peroxisome proliferator-activated receptor α target genes. Cell. Mol. Life Sci. CMLS. 2004;61:393–416. doi: 10.1007/s00018-003-3216-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gervois P., Mansouri R.M. PPARα as a therapeutic target in inflammation-associated diseases. Expert Opin. Ther. Targets. 2012;16:1113–1125. doi: 10.1517/14728222.2012.715633. [DOI] [PubMed] [Google Scholar]
- 83.Varga T., Czimmerer Z., Nagy L. PPARs are a unique set of fatty acid regulated transcription factors controlling both lipid metabolism and inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2011 doi: 10.1016/j.bbadis.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aoyama T., Peters J.M., Iritani N., Nakajima T., Furihata K., Hashimoto T., Gonzalez F.J. Altered constitutive expression of fatty acid-metabolizing enzymes in mice lacking the peroxisome proliferator-activated receptor α (PPARα) J. Biol. Chem. 1998 doi: 10.1074/jbc.273.10.5678. [DOI] [PubMed] [Google Scholar]
- 85.Abdelmegeed M.A., Moon K.H., Hardwick J.P., Gonzalez F.J., Song B.J. Role of peroxisome proliferator-activated receptor-α in fasting-mediated oxidative stress. Free. Radic. Biol. Med. 2009 doi: 10.1016/j.freeradbiomed.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Desvergne B., Wahli W. Peroxisome proliferator-activated receptors: Nuclear control of metabolism. Endocr. Rev. 1999;20:649–688. doi: 10.1210/edrv.20.5.0380. [DOI] [PubMed] [Google Scholar]
- 87.Dimartino J.F., Selleri L., Traver D., Firpo M.T., Rhee J., Warnke R., O’Gorman S., Weissman I.L., Cleary M.L. The Hox cofactor and proto-oncogene Pbx1 is required for maintenance of definitive hematopoiesis in the fetal liver. Blood. 2001 doi: 10.1182/blood.V98.3.618. [DOI] [PubMed] [Google Scholar]
- 88.Fournier M., Lebert-Ghali C.E., Krosl G., Bijl J.J. HOXA4 induces expansion of hematopoietic stem cells in vitro and confers enhancement of pro-B-cells in vivo. Stem Cells Dev. 2012;21:133–142. doi: 10.1089/scd.2011.0259. [DOI] [PubMed] [Google Scholar]
- 89.Zewdu R., Risolino M., Barbulescu A., Ramalingam P., Butler J.M., Selleri L. Spleen hypoplasia leads to abnormal stress hematopoiesis in mice with loss of Pbx homeoproteins in splenic mesenchyme. J. Anat. 2016;229:153–169. doi: 10.1111/joa.12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fang F., Wang Y., Li R., Zhao Y., Guo Y., Jiang M., Sun J., Ma Y., Ren Z., Tian Z., et al. Transcription factor E2F1 suppresses dendritic cell maturation. J. Immunol. 2010;184:6084–6091. doi: 10.4049/jimmunol.0902561. [DOI] [PubMed] [Google Scholar]
- 91.Magez S., Radwanska M., Drennan M., Fick L., Baral T.N., Brombacher F., Baetselier P.D. Interferon-γ and nitric oxide in combination with antibodies are key protective host immune factors during Trypanosoma congolense Tc13 infections. J. Infect. Dis. 2006;193:1575–1583. doi: 10.1086/503808. [DOI] [PubMed] [Google Scholar]
- 92.Pan J., Zhang M., Wang J., Wang Q., Xia D., Sun W., Zhang L., Yu H., Liu Y., Cao X. Interferon-γ is an autocrine mediator for dendritic cell maturation. Immunol. Lett. 2004;94:141–151. doi: 10.1016/j.imlet.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 93.Wu H., Liu G., Shi M. Interferon gamma in African trypanosome infections: Friends or foes? Front. Immunol. 2017;8:1105. doi: 10.3389/fimmu.2017.01105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cox C.J., Espinoza H.M., McWilliams B., Chappell K., Morton L., Hjalt T.A., Semina E.V., Amendt B.A. Differential regulation of gene expression by PITX2 isoforms. J. Biol. Chem. 2002;277:25001–25010. doi: 10.1074/jbc.M201737200. [DOI] [PubMed] [Google Scholar]
- 95.Casacuberta-Serra S., Soucek L. Myc and Ras, the Bonnie and Clyde of immune evasion. Transl. Cancer Res. 2018;7:S457. doi: 10.21037/tcr.2018.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kortlever R.M., Sodir N.M., Wilson C.H., Burkhart D.L., Pellegrinet L., Swigart L.B., Littlewood T.D., Evan G.I. Myc cooperates with Ras by programming inflammation and immune suppression. Cell. 2017;171:1301–1315. doi: 10.1016/j.cell.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Villarino A.V., Gallo E., Abbas A.K. STAT1-activating cytokines limit Th17 responses through both T-bet–dependent and–independent mechanisms. J. Immunol. 2010;185:6461–6471. doi: 10.4049/jimmunol.1001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tesmer L.A., Lundy S.K., Sarkar S., Fox D.A. Th17 cells in human disease. Immunol. Rev. 2008;223:87–113. doi: 10.1111/j.1600-065X.2008.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Szabo S.J., Sullivan B.M., Peng S.L., Glimcher L.H. Molecular mechanisms regulating Th1 immune responses. Annu. Rev. Immunol. 2003;21:713–758. doi: 10.1146/annurev.immunol.21.120601.140942. [DOI] [PubMed] [Google Scholar]
- 100.Okwor I., Muleme H., Jia P., Uzonna J.E. Altered proinflammatory cytokine production and enhanced resistance to Trypanosoma congolense infection in lymphotoxin β-deficient mice. J. Infect. Dis. 2009;200:361–369. doi: 10.1086/599792. [DOI] [PubMed] [Google Scholar]
- 101.Shi M., Pan W., Tabel H. Experimental African trypanosomiasis: IFN-γ mediates early mortality. Eur. J. Immunol. 2003;33:108–118. doi: 10.1002/immu.200390013. [DOI] [PubMed] [Google Scholar]
- 102.Zhou Y., Fu B., Xu X., Tong X., Sun R., Tian Z., Wei H. Requirement for PBX1 in developmental programming of natural killer cells. J. Immunol. 2017;198:202–215. [Google Scholar]
- 103.Cnops J., De Trez C., Stijlemans B., Keirsse J., Kauffmann F., Barkhuizen M., Keeton R., Boon L., Brombacher F., Magez S. NK-, NKT-and CD8-Derived IFNγ drives myeloid cell activation and erythrophagocytosis, resulting in trypanosomosis-associated acute anemia. PLoS Pathog. 2015;11:e1004964. doi: 10.1371/journal.ppat.1004964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ueda H.R., Hayashi S., Chen W., Sano M., Machida M., Shigeyoshi Y., Iino M., Hashimoto S. System-level identification of transcriptional circuits underlying mammalian circadian clocks. Nat. Genet. 2005;37:187–192. doi: 10.1038/ng1504. [DOI] [PubMed] [Google Scholar]
- 105.Yamaguchi S., Mitsui S., Yan L., Yagita K., Miyake S., Okamura H. Role of DBP in the circadian oscillatory mechanism. Mol. Cell. Biol. 2000;20:4773–4781. doi: 10.1128/MCB.20.13.4773-4781.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Silver A.C., Arjona A., Hughes M.E., Nitabach M.N., Fikrig E. Circadian expression of clock genes in mouse macrophages, dendritic cells, and B cells. Brain Behav. Immun. 2012;26:407–413. doi: 10.1016/j.bbi.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Keller M., Mazuch J., Abraham U., Eom G.D., Herzog E.D., Volk H.D., Kramer A., Maier B. A circadian clock in macrophages controls inflammatory immune responses. Proc. Natl. Acad. Sci. USA. 2009;106:21407–21412. doi: 10.1073/pnas.0906361106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Archer S.N., Viola A.U., Kyriakopoulou V., von Schantz M., Dijk D.J. Inter-individual differences in habitual sleep timing and entrained phase of endogenous circadian rhythms of BMAL1, PER2 and PER3 mRNA in human leukocytes. Sleep. 2008;31:608–617. doi: 10.1093/sleep/31.5.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hayashi M., Shimba S., Tezuka M. Characterization of the molecular clock in mouse peritoneal macrophages. Biol. Pharm. Bull. 2007;30:621–626. doi: 10.1248/bpb.30.621. [DOI] [PubMed] [Google Scholar]
- 110.Arjona A., Sarkar D.K. The circadian gene mPer2 regulates the daily rhythm of IFN-γ. J. Interferon Cytokine Res. 2006;26:645–649. doi: 10.1089/jir.2006.26.645. [DOI] [PubMed] [Google Scholar]
- 111.Arjona A., Sarkar D.K. Evidence supporting a circadian control of natural killer cell function. Brain, Behav. Immun. 2006;20:469–476. doi: 10.1016/j.bbi.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 112.Arjona A., Sarkar D.K. Circadian oscillations of clock genes, cytolytic factors, and cytokines in rat NK cells. J. Immunol. 2005;174:7618–7624. doi: 10.4049/jimmunol.174.12.7618. [DOI] [PubMed] [Google Scholar]
- 113.Boivin D.B., James F.O., Wu A., Cho-Park P.F., Xiong H., Sun Z.S. Circadian clock genes oscillate in human peripheral blood mononuclear cells. Blood. 2003;102:4143–4145. doi: 10.1182/blood-2003-03-0779. [DOI] [PubMed] [Google Scholar]
- 114.Sha Z., Compans R.W. Induction of CD4+ T-cell-independent immunoglobulin responses by inactivated influenza virus. J. Virol. 2000;74:4999–5005. doi: 10.1128/JVI.74.11.4999-5005.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Oxenius A., Zinkernagel R.M., Hengartner H. Advances in Immunology. Volume 70. Elsevier; Amsterdam, The Netherlands: 1998. CD4+ T-cell induction and effector functions: A comparison of immunity against soluble antigens and viral infections; pp. 313–367. [DOI] [PubMed] [Google Scholar]
- 116.Parker D.C. T cell-dependent B cell activation. Annu. Rev. Immunol. 1993;11:331–360. doi: 10.1146/annurev.iy.11.040193.001555. [DOI] [PubMed] [Google Scholar]
- 117.Taylor K.A., Lutje V., Kennedy D., Authié E., Boulangé A., Logan-Henfrey L., Gichuki B., Gettinby G. Trypanosoma congolense: B-lymphocyte responses differ between trypanotolerant and trypanosusceptible cattle. Exp. Parasitol. 1996;83:106–116. doi: 10.1006/expr.1996.0054. [DOI] [PubMed] [Google Scholar]
- 118.Bollinger T., Leutz A., Leliavski A., Skrum L., Kovac J., Bonacina L., Benedict C., Lange T., Westermann J., Oster H., et al. Circadian clocks in mouse and human CD4+ T cells. PLoS ONE. 2011;6:e29801. doi: 10.1371/journal.pone.0029801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jones D.C., Ding X., Daynes R.A. Nuclear Receptor Peroxisome Proliferator-activated Receptor α (PPARα) Is Expressed in Resting Murine Lymphocytes The Pparα In T and B Lymphocytes Is Both Transactivation and Transrepression Competent. J. Biol. Chem. 2002;277:6838–6845. doi: 10.1074/jbc.M106908200. [DOI] [PubMed] [Google Scholar]
- 120.Cunard R., Ricote M., DiCampli D., Archer D.C., Kahn D.A., Glass C.K., Kelly C.J. Regulation of cytokine expression by ligands of peroxisome proliferator activated receptors. J. Immunol. 2002;168:2795–2802. doi: 10.4049/jimmunol.168.6.2795. [DOI] [PubMed] [Google Scholar]
- 121.Yang Y., Gocke A.R., Lovett-Racke A., Drew P.D., Racke M.K. PPAR alpha regulation of the immune response and autoimmune encephalomyelitis. PPAR Res. 2008;2008 doi: 10.1155/2008/546753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cunard R., DiCampli D., Archer D.C., Stevenson J.L., Ricote M., Glass C.K., Kelly C.J. WY14, 643, a PPARα ligand, has profound effects on immune responses in vivo. J. Immunol. 2002;169:6806–6812. doi: 10.4049/jimmunol.169.12.6806. [DOI] [PubMed] [Google Scholar]
- 123.Delerive P., De Bosscher K., Besnard S., Berghe W.V., Peters J.M., Gonzalez F.J., Fruchart J.C., Tedgui A., Haegeman G., Staels B. Peroxisome proliferator-activated receptor α negatively regulates the vascular inflammatory gene response by negative cross-talk with transcription factors NF-κB and AP-1. J. Biol. Chem. 1999;274:32048–32054. doi: 10.1074/jbc.274.45.32048. [DOI] [PubMed] [Google Scholar]
- 124.Jantsch J., Schödel J. Hypoxia and hypoxia-inducible factors in myeloid cell-driven host defense and tissue homeostasis. Immunobiology. 2015;220:305–314. doi: 10.1016/j.imbio.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 125.Arena E.T., Tinevez J.Y., Nigro G., Sansonetti P.J., Marteyn B.S. The infectious hypoxia: Occurrence and causes during Shigella infection. Microbes Infect. 2017;19:157–165. doi: 10.1016/j.micinf.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 126.Waghabi M.C., Keramidas M., Bailly S., Degrave W., Mendonça-Lima L., Maria de Nazaré C.S., Maria de Nazareth L.M., Paciornik S., Araújo-Jorge T.C., Feige J.J. Uptake of host cell transforming growth factor-β by Trypanosoma cruzi amastigotes in cardiomyocytes: Potential role in parasite cycle completion. Am. J. Pathol. 2005;167:993–1003. doi: 10.1016/S0002-9440(10)61189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gantt K.R., Schultz-Cherry S., Rodriguez N., Jeronimo S.M., Nascimento E.T., Goldman T.L., Recker T.J., Miller M.A., Wilson M.E. Activation of TGF-β by Leishmania chagasi: Importance for parasite survival in macrophages. J. Immunol. 2003;170:2613–2620. doi: 10.4049/jimmunol.170.5.2613. [DOI] [PubMed] [Google Scholar]
- 128.Boutard V., Havouis R., Fouqueray B., Philippe C., Moulinoux J.P., Baud L. Transforming growth factor-beta stimulates arginase activity in macrophages. Implications for the regulation of macrophage cytotoxicity. J. Immunol. 1995;155:2077–2084. [PubMed] [Google Scholar]
- 129.Bogdan C., Nathan C. Modulation of Macrophage Function by Transforming Growth Factor β, Interleukin-4, and Interleukin-10 a. Ann. N. Y. Acad. Sci. 1993;685:713–739. doi: 10.1111/j.1749-6632.1993.tb35934.x. [DOI] [PubMed] [Google Scholar]
- 130.Johnston C.J., Smyth D.J., Dresser D.W., Maizels R.M. TGF-β in tolerance, development and regulation of immunity. Cell. Immunol. 2016;299:14–22. doi: 10.1016/j.cellimm.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hansen G., McIntire J.J., Yeung V.P., Berry G., Thorbecke G.J., Chen L., DeKruyff R.H., Umetsu D.T. CD4+ T helper cells engineered to produce latent TGF-β1 reverse allergen-induced airway hyperreactivity and inflammation. J. Clin. Investig. 2000;105:61–70. doi: 10.1172/JCI7589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ferrão P.M., Nisimura L.M., Moreira O.C., Land M.G., Pereira M.C., de Mendonça-Lima L., Araujo-Jorge T.C., Waghabi M.C., Garzoni L.R. Inhibition of TGF-β pathway reverts extracellular matrix remodeling in T. cruzi-infected cardiac spheroids. Exp. Cell Res. 2018;362:260–267. doi: 10.1016/j.yexcr.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 133.MacLean L., Chisi J.E., Odiit M., Gibson W.C., Ferris V., Picozzi K., Sternberg J.M. Severity of human African trypanosomiasis in East Africa is associated with geographic location, parasite genotype, and host inflammatory cytokine response profile. Infect. Immun. 2004;72:7040–7044. doi: 10.1128/IAI.72.12.7040-7044.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Dinarello C.A. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol. Rev. 2018;281:8–27. doi: 10.1111/imr.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bass J., Takahashi J.S. Circadian integration of metabolism and energetics. Science. 2010;330:1349–1354. doi: 10.1126/science.1195027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wang J., Mauvoisin D., Martin E., Atger F., Galindo A.N., Dayon L., Sizzano F., Palini A., Kussmann M., Waridel P., et al. Nuclear proteomics uncovers diurnal regulatory landscapes in mouse liver. Cell Metab. 2017;25:102–117. doi: 10.1016/j.cmet.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mauvoisin D., Wang J., Jouffe C., Martin E., Atger F., Waridel P., Quadroni M., Gachon F., Naef F. Circadian clock-dependent and-independent rhythmic proteomes implement distinct diurnal functions in mouse liver. Proc. Natl. Acad. Sci. USA. 2014;111:167–172. doi: 10.1073/pnas.1314066111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Panda S., Antoch M.P., Miller B.H., Su A.I., Schook A.B., Straume M., Schultz P.G., Kay S.A., Takahashi J.S., Hogenesch J.B. Coordinated transcription of key pathways in the mouse by the circadian clock. Cell. 2002;109:307–320. doi: 10.1016/S0092-8674(02)00722-5. [DOI] [PubMed] [Google Scholar]
- 139.Taghon T., Thys K., De Smedt M., Weerkamp F., Staal F., Plum J., Leclercq G. Homeobox gene expression profile in human hematopoietic multipotent stem cells and T-cell progenitors: Implications for human T-cell development. Leukemia. 2003;17:1157–1163. doi: 10.1038/sj.leu.2402947. [DOI] [PubMed] [Google Scholar]
- 140.Taghon T., Stolz F., De Smedt M., Cnockaert M., Verhasselt B., Plum J., Leclercq G. HOX-A10 regulates hematopoietic lineage commitment: Evidence for a monocyte-specific transcription factor. Blood, J. Am. Soc. Hematol. 2002;99:1197–1204. doi: 10.1182/blood.V99.4.1197. [DOI] [PubMed] [Google Scholar]
- 141.Res P., Spits H. Seminars in Immunology. Volume 11. Elsevier; Amsterdam, The Netherlands: 1999. Developmental stages in the human thymus; pp. 39–46. [DOI] [PubMed] [Google Scholar]
- 142.Magli M.C., Largman C., Lawrence H.J. Effects of HOX homeobox genes in blood cell differentiation. J. Cell. Physiol. 1997;173:168–177. doi: 10.1002/(SICI)1097-4652(199711)173:2<168::AID-JCP16>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 143.Niwa H. How is pluripotency determined and maintained? Development. 2007;134:635–646. doi: 10.1242/dev.02787. [DOI] [PubMed] [Google Scholar]
- 144.Niwa H., Miyazaki J., Smith A.G. Quantitative expression of Oct-3/4 defines differentiation, dedifferentiation or self-renewal of ES cells. Nat. Genet. 2000;24:372–376. doi: 10.1038/74199. [DOI] [PubMed] [Google Scholar]
- 145.Sun Y., Yang Z., Niu Z., Peng J., Li Q., Xiong W., Langnas A.N., Ma M.Y., Zhao Y. MOP3, a component of the molecular clock, regulates the development of B cells. Immunology. 2006;119:451–460. doi: 10.1111/j.1365-2567.2006.02456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kuriakose S.M., Singh R., Uzonna J.E. Host intracellular signaling events and pro-inflammatory cytokine production in African trypanosomiasis. Front. Immunol. 2016;7:181. doi: 10.3389/fimmu.2016.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Fatouros M., Bourantas K., Bairaktari E., Elisaf M., Tsolas O., Cassioumis D. Role of the spleen in lipid metabolism. Br. J. Surg. 1995;82:1675–1677. doi: 10.1002/bjs.1800821230. [DOI] [PubMed] [Google Scholar]
- 148.Aviram M., Brook J., Tatarsky I., Levy Y., Carter A. Increased low-density lipoprotein levels after splenectomy: A role for the spleen in cholesterol metabolism in myeloproliferative disorders. Am. J. Med Sci. 1986;291:25–28. doi: 10.1097/00000441-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 149.Egan C., Sukhumavasi W., Butcher B., Denkers E. Functional aspects of Toll-like receptor/MyD88 signalling during protozoan infection: Focus on Toxoplasma gondii. Clin. Exp. Immunol. 2009;156:17–24. doi: 10.1111/j.1365-2249.2009.03876.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kuriakose S., Onyilagha C., Singh R., Olayinka-Adefemi F., Jia P., Uzonna J.E. TLR-2-dependent activation of MAPK and STAT proteins regulates proinflammatory cytokine response and immunity to experimental Trypanosoma congolense infection. Front. Immunol. 2019;10:2673. doi: 10.3389/fimmu.2019.02673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sutton C.E., Lalor S.J., Sweeney C.M., Brereton C.F., Lavelle E.C., Mills K.H. Interleukin-1 and IL-23 induce innate IL-17 production from gamma delta T cells, amplifying Th17 responses and autoimmunity. Immunity. 2009;31:331–341. doi: 10.1016/j.immuni.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 152.Scheiermann C., Gibbs J., Ince L., Loudon A. Clocking in to immunity. Nat. Rev. Immunol. 2018;18:423–437. doi: 10.1038/s41577-018-0008-4. [DOI] [PubMed] [Google Scholar]
- 153.Curtis A.M., Bellet M.M., Sassone-Corsi P., O’Neill L.A. Circadian clock proteins and immunity. Immunity. 2014;40:178–186. doi: 10.1016/j.immuni.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 154.Barkhuizen M., Magez S., Atkinson R.A., Brombacher F. Interleukin-12p70-dependent interferon-γ production is crucial for resistance in African trypanosomiasis. J. Infect. Dis. 2007;196:1253–1260. doi: 10.1086/521681. [DOI] [PubMed] [Google Scholar]
- 155.Liu Y., Ragaa E., Li Z., Nuortio L., Mustafa A., Bakhiet M. Interferon-gamma and interleukin-12 genes are preferentially expressed during early experimental African trypanosomiasis and suppressed by denervation of the spleen. Scand. J. Immunol. 1999;50:485–491. doi: 10.1046/j.1365-3083.1999.00639.x. [DOI] [PubMed] [Google Scholar]
- 156.Tian S. Identification of monotonically differentially expressed genes for non-small cell lung cancer. BMC Bioinform. 2019;20:177. doi: 10.1186/s12859-019-2775-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hergenhan S., Holtkamp S., Scheiermann C. Molecular interactions between components of the circadian clock and the immune system. J. Mol. Biol. 2020 doi: 10.1016/j.jmb.2019.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Altman B.J., Hsieh A.L., Sengupta A., Krishnanaiah S.Y., Stine Z.E., Walton Z.E., Gouw A.M., Venkataraman A., Li B., Goraksha-Hicks P., et al. MYC disrupts the circadian clock and metabolism in cancer cells. Cell Metab. 2015;22:1009–1019. doi: 10.1016/j.cmet.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gery S., Koeffler H. The Role of Circadian Regulation in Cancer. Volume 72. Cold Spring Harbor Symposia on Quantitative Biology, Cold Spring Harbor Laboratory Press; Cold Spring Harbor, NY, USA: 2007. pp. 459–464. [DOI] [PubMed] [Google Scholar]
- 160.Masri S., Sassone-Corsi P. The emerging link between cancer, metabolism, and circadian rhythms. Nat. Med. 2018;24:1795. doi: 10.1038/s41591-018-0271-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dixon L.J., Barnes M., Tang H., Pritchard M.T., Nagy L.E. Kupffer cells in the liver. Compr. Physiol. 2013;3:785–797. doi: 10.1002/cphy.c120026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Stout R.D., Suttles J. Functional plasticity of macrophages: Reversible adaptation to changing microenvironments. J. Leukoc. Biol. 2004;76:509–513. doi: 10.1189/jlb.0504272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gordon S., Taylor P.R. Monocyte and macrophage heterogeneity. Nat. Rev. Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 164.Hörhold F., Eisel D., Oswald M., Kolte A., Röll D., Osen W., Eichmüller S.B., König R. Reprogramming of macrophages employing gene regulatory and metabolic network models. PLoS Comput. Biol. 2020;16:e1007657. doi: 10.1371/journal.pcbi.1007657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Uzonna J., Kaushik R., Gordon J., Tabel H. Cytokines and antibody responses during Trypanosoma congolense infections in two inbred mouse strains that differ in resistance. Parasite Immunol. 1999;21:57–71. doi: 10.1046/j.1365-3024.1999.00202.x. [DOI] [PubMed] [Google Scholar]
- 166.Kel A.E. Biological Networks and Pathway Analysis. Springer; Berlin/Heidelberg, Germany: 2017. Search for Master Regulators in Walking Cancer Pathways; pp. 161–191. [DOI] [PubMed] [Google Scholar]
- 167.Kel A.E., Stegmaier P., Valeev T., Koschmann J., Poroikov V., Kel-Margoulis O.V., Wingender E. Multi-omics “upstream analysis” of regulatory genomic regions helps identifying targets against methotrexate resistance of colon cancer. EuPA Open Proteom. 2016;13:1–13. doi: 10.1016/j.euprot.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Sikdar S., Datta S. A novel statistical approach for identification of the master regulator transcription factor. BMC Bioinform. 2017;18:1–11. doi: 10.1186/s12859-017-1499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.