Abstract
In addition to being a marker of cardiovascular (CV) aging, aortic stiffening has been shown to be independently associated with increased CV risk (directly and/or indirectly due to stiffness-gradient attenuation). Arterial stiffness determines the rate at which the pulse pressure wave propagates (i.e., pulse wave velocity, PWV). Thus, propagated PWV (i.e., the distance between pressure-wave recording sites divided by the pulse transit time) was proposed as an arterial stiffness index. Presently, aortic PWV is considered a gold-standard for non-invasive stiffness evaluation. The limitations ascribed to PWV have hampered its use in clinical practice. To overcome the limitations, different approaches and parameters have been proposed (e.g., local PWV obtained by wave separation and pulse wave analysis). In turn, it has been proposed to determine PWV considering blood pressure (BP) levels (β-PWV), so as to evaluate intrinsic arterial stiffness. It is unknown whether the different approaches used to assess PWV or β-PWV are equivalent and there are few data regarding age- and sex-related reference intervals (RIs) for regional and local PWV, β-PWV and PWV ratio. Aims: (1) to evaluate agreement between data from different stiffness indexes, (2) to determine the need for sex-specific RIs, and (3) to define RIs for PWV, β-PWV and PWV ratio in a cohort of healthy children, adolescents and adults. Methods: 3619 subjects (3–90 y) were included, 1289 were healthy and non-exposed to CV risk factors. Carotid-femoral (cfPWV) and carotid-radial (crPWV) PWV were measured (SphygmoCor System (SCOR)) and PWV ratio (cfPWV/crPWV) was quantified. Local aortic PWV was obtained directly from carotid waves (aoPWV-Carotid; SCOR) and indirectly (generalized transfer function use) from radial (aoPWV-Radial; SCOR) and brachial (aoPWV-Brachial; Mobil-O-Graph system (MOG)) recordings. β-PWV was assessed by means of cardio-ankle brachial (CAVI) and BP-corrected CAVI (CAVIo) indexes. Analyses were done before and after adjustment for BP. Data agreement was analyzed (correlation, Bland-Altman). Mean and standard deviation (age- and sex-related) equations were obtained for PWV parameters (regression methods based on fractional polynomials). Results: The methods and parameters used to assess aortic stiffness showed different association levels. Stiffness data were not equivalent but showed systematic and proportional errors. The need for sex-specific RIs depended on the parameter and/or age considered. RIs were defined for all the studied parameters. The study provides the largest data set related to agreement and RIs for stiffness parameters obtained in a single population.
Keywords: adolescents, adults, arterial stiffness, blood pressure, children, pulse wave velocity
1. Introduction
The arterial wall thickens and stiffens with aging. Such aging-related structural and functional changes are not distributed homogeneously but predominate in the aorta and central elastic arteries [1,2]. On the other hand, the mechanisms linking arterial stiffness and vascular disease (e.g., atherosclerotic) are not completely understood, in addition to being a marker of cardiovascular (CV) aging, aortic stiffening has been shown to be independently associated with increased CV risk and morbi-mortality [3]. This accounts for the interest in assessing aortic stiffness in the clinical practice.
Arterial stiffness determines the rate at which the pulse pressure wave propagates, that is, the pulse wave velocity (PWV). Thus, propagated PWV (obtained as the distance traveled by the pulse wave divided by the transit time) was proposed as an arterial stiffness index. Furthermore, up to now, PWV (in particular the carotid-femoral PWV (cfPWV)) is considered a gold standard for non-invasive arterial stiffness evaluation [1,4]. Although PWV is the most validated method to evaluate arterial stiffness in a non-invasive way, the limitations ascribed to PWV have hampered its use in clinical practice, the development in the field and the recognition of PWV as an independent marker of the vascular status [1]. About this, PWV measurement requires some skills, and pulse wave recording is difficult in some patients. On the other hand, PWV is inherently dependent on blood pressure (BP), which, if not considered, would lead to an inaccurate interpretation of PWV data [3,5,6]. To overcome such limitations, different approaches and parameters have been proposed. Then, methods relying on pulse-wave analysis and wave separation analysis (PWA and WSA, respectively) have been developed to non-invasively assess (local) PWV, directly from measured waves (e.g., carotid) or indirectly, from central waves mathematically-derived using general transfer functions (GTF) applied to peripheral waves (e.g., brachial, radial). In turn, the use of cuff-based oscillometric devices that give an estimated (local) PWV based on PWA and/or WSA requires less expertise, makes the process less operator-dependent and enables ambulatory measurements [7]. Finally, the stiffness index β and cardio-ankle vascular index (CAVI) would have the advantage of considering the relationship between stiffness and BP. Hence, they were proposed to evaluate intrinsic wall stiffness [6].
The detrimental impact of arterial stiffness on the CV system would be mediated by a direct effect of the increased stiffness and/or by the attenuation of the center-to-periphery stiffness gradient (e.g., evaluated by the PWV ratio). In this regard, the age-related reduction in the stiffness gradient is associated with adverse clinical outcomes [8]. Then, analyzing the PWV ratio would add to and complement data obtained from PWV.
Currently, different devices, approaches and parameters are used to non-invasively assess arterial stiffness. It is unknown whether the different methods used to quantify PWV provide equivalent information and/or if it is possible to define equations to convert data obtained with a given approach into data corresponding to another one. Additionally, there is little information regarding age and/or sex-related reference intervals (RIs) for regional and local PWV, β-PWV (or CAVI) and PWV ratio obtained at the same time in a large healthy population including children, adolescents and adults.
This work’s aims were: (1) to evaluate agreement between PWV data obtained with different approaches, (2) to determine the need for sex-specific RIs, and (3) to define RIs for PWV, β-PWV and PWV ratio in a cohort of healthy children, adolescents and adults from South America.
2. Materials and Methods
2.1. Study Population
The study was carried out in the context of the Centro Universitario de Investigación, Innovación y Diagnóstico Arterial (CUiiDARTE) project [9,10,11,12,13], a population-based study developed in Uruguay. In this work, we considered data from 3619 subjects included in the CUiiDARTE Database. This includes data on demographic and anthropometric variables, exposure to CV risk factors (CRFs), personal and family history of CV disease and data on structural and functional CV parameters non-invasively obtained, mainly from community-based projects [9,10,11].
To determine RIs (age- and sex-specific normative tables) for arterial stiffness parameters, we selected a healthysub-population that included children, adolescents and adults who did not meet any of the following criteria: (i) history of CV disease (defined as presence of cerebrovascular, coronary heart, valvular or peripheral arterial disease, impaired cardiac ejection fraction and/or left ventricular hypertrophy); (ii) use of BP-, lipid- and/or glucose-lowering drugs; (iii) arterial hypertension (≥18 y: brachial systolic blood pressure (bSBP) ≥ 140 mmHg and/or brachial diastolic blood pressure (bDBP) ≥ 90 mmHg); <18 y: bSBP and bDBP < 95th percentile for sex, age and body height (BH)); (iv) current smoking; (v) diabetes (defined as self-reported and/or fasting plasma glucose ≥ 126 mg/dL (if available)); (vi) dyslipidemia (defined as self-reported, total cholesterol ≥ 240 mg/dL or HDL cholesterol < 40 mg/dL (if available)); (vii) obesity (≥18 y: body mass index (BMI) ≥ 30 kg/m2; <18 y: z-BMI ≥ 2.0). The cut-off values used to define the healthy sub-population were chosen, whenever possible, to be similar to those used to indicate increased risk in clinical guidelines (or risk algorithms) [14,15,16,17], and to enable optimal comparison with data from other groups (e.g., the European Reference Values for Arterial Measurements Collaboration Group) [18,19,20,21]. Additionally, none of the subjects in the RIs group had congenital, chronic or infectious diseases and cardiac rhythm other than sinus rhythm. The resulting sub-population included 1289 individuals. All procedures are in agreement with the Declaration of Helsinki (1975 and reviewed in 1983) and the study protocol was approved by the Institution’s Ethics Committee. In adults, written informed consent was obtained prior to the evaluation. In children and adolescents (<18 y), parents’ written consent and children’s assent were obtained before the study. The procedures followed to obtain data used in this work are described below.
2.2. Anthropometric and Clinical Evaluation
A brief clinical interview, together with the anthropometric evaluation enabled us to assess CRFs exposure, defined according to the criteria (cut-off points) described above. A family history of CV disease was defined by the presence of first-degree (for all the subjects) and/or second-degree (for subjects ≤18 y) relatives with early (<55 y in males; <65 y in females) CV disease (see above). Bodyweight (BW) and BH were measured with the participants wearing light clothing and no shoes. Standing BH was measured using a portable stadiometer and recorded to the nearest 0.1 cm. BW was measured with an electronic scale (841/843, Seca Inc., Hamburg, Germany; model HBF-514C, Omron Inc., Chicago, IL, USA) and recorded to the nearest 0.1 kg. BMI was calculated as BW-to-squared BH ratio. In children and adolescents, z-scores for the BMI were calculated using the World Health Organization software (Anthro-v.3.2.2; Anthro-Plus-v.1.0.4) [9].
2.3. Cardiovascular Evaluation
Participants were asked to avoid exercise, tobacco, alcohol, caffeine and food-intake four hours before the evaluation. All hemodynamic measurements were performed in a temperature-controlled environment (21–23 °C), with the subject in supine position and after resting for at least 10–15 min, which enabled reaching steady hemodynamic conditions. Using a validated oscillometric device (HEM-433INT; Omron Healthcare Inc., Lake Forest, IL, USA), heart rate (HR), bSBP and bDBP were recorded simultaneously and/or immediately before or after each non-invasive tonometric (radial, femoral, carotid) and brachial oscillometry record. Then, brachial pulse pressure (bPP; bPP = bSBP − bDBP) and bMBP (bMBP = bDBP + bPP/3) were obtained.
CV evaluation in the CUiiDARTE project includes assessing: (i) peripheral (brachial, radial, ankle) and central (aortic, carotid) BP levels; central (aortic, carotid) PWA and WSA-derived parameters (e.g., augmentation index, forward and backward pressure components), (ii) carotid, femoral and brachial beat-to-beat diameter waves and intima-media thickness, (iii) brachial artery reactivity (e.g., flow-mediated dilation; low flow-mediated constriction), (iv) carotid, femoral and brachial doppler-derived blood velocity profiles and resistive/pulsatile indexes, (v) ankle-brachial index, (vi) screening for carotid and femoral atherosclerotic plaques presence, (vii) carotid, femoral and brachial local stiffness (e.g., distensibility, elastic modulus), (viii) systemic hemodynamic evaluation (e.g., systemic vascular resistances, cardiac output and index quantified from brachial pulse contour analysis and/or cardiography impedance, (ix) regional stiffness (cfPWV, crPWV) [9,10,11,12,13,22]. In this work, we focused on regional and local PWV data.
2.4. Carotid and Femoral Artery Ultrasound
Left and right common (CCA), internal and external carotid arteries and common femoral (CFA) arteries were examined (B-Mode and Doppler ultrasound, 7–13 MHz, linear transducer, M-Turbo, SonoSite Inc., Bothell, WA, USA) [22]. Transverse and longitudinal arterial views were obtained to assess the presence of atherosclerotic plaques. Near and far walls were analyzed, and images were obtained from anterior, lateral, and posterior angles. An atherosclerotic plaque was defined as: focal wall thickening at least 50% greater than the adjacent segment, focal thickening protruding into the lumen at least 0.5 mm or an intima-media thickness (IMT) ≥ 1.5 mm [23].
2.5. Regional PWV (cfPWV and crPWV) and Pulse Wave Velocity Ratio (PWV Ratio)
Carotid-femoral (aortic; cfPWV) and upper arm (crPWV) regional stiffness were assessed (applanation tonometry, SphygmoCor-CvMS, AtCor-Medical, Sidney, Australia) (Figure 1). PWV values depend on the algorithm used for detecting the so-called “foot of the wave” and on the distance (path-length) considered [24,25,26,27]. In this work, the intersecting tangent algorithm was used to detect the wave-foot [24,25,26,27]. The path length can be the direct distance between the recording sites (e.g., carotid and femoral), or the distance obtained by subtracting the distance between the proximal recording site (e.g., carotid) and the sternal notch from the distance between the sternal notch and the peripheral recording site (e.g., femoral) [24,25,26,27]. Following international recommendations, for cfPWV, we used the direct distance multiplied by 0.8, which enabled us to obtain the real cfPWV. In turn, we considered the subtracted distance for crPWV quantification [24,25,26,27]. cfPWV and crPWV values were obtained from the median of three measurements (random order). PWV Ratio, a marker of center-periphery stiffness gradient was quantified as cfPWV/crPWV [28,29].
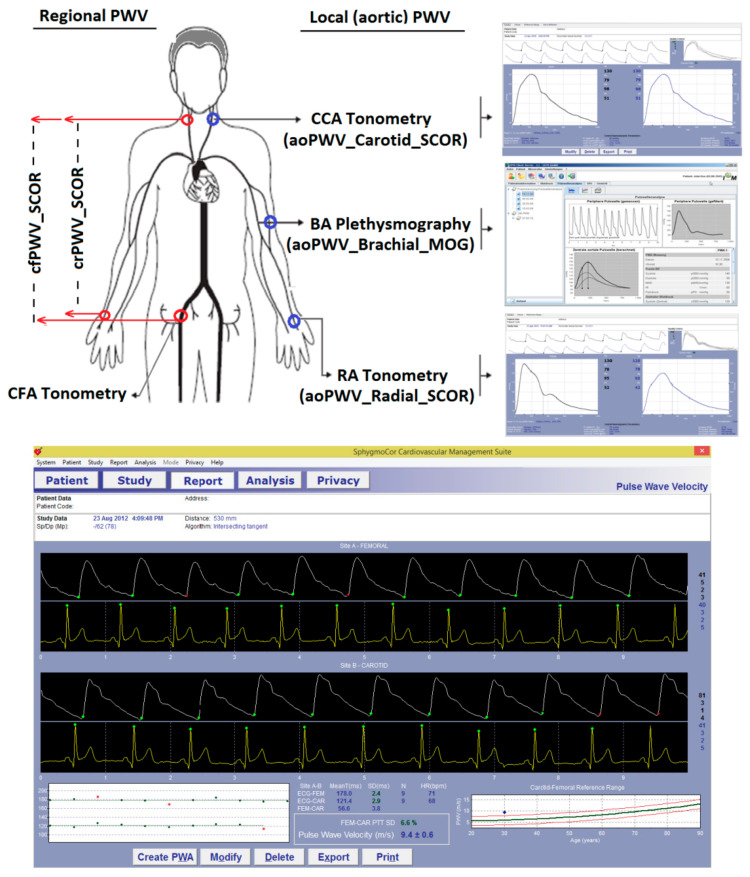
Figure 1.
Top: Diagram showing arterial recording sites and pulse waves, measured or obtained to calculate local PWV. Software screens (SCOR and MOG) for carotid and radial applanation tonometry (SCOR) and for brachial oscillometry/plethysmography (MOG) records are shown. Bottom: software screen during cfPWV assessment showing the peripheral (femoral) and central (carotid) waves records and the resulting cfPWV (9.4 m/s).
2.6. Local PWV: aoPWV_Radial_SCOR, aoPWV_Carotid_SCOR and aoPWV_Brachial_MOG
Central BP levels and waveforms were obtained (random order) using two commercially available devices: SphygmoCor-CvMS (SCOR; v.9, AtCor-Medical, Australia) and Mobil-O-Graph PWA-monitor system (MOG; I.E.M.-GmbH, Stolberg, Germany) (Figure 1). Both devices and systems enable PWA and WSA [12]. A detailed (step-by-step) explanation of the method used for WSA based on recorded (carotid wave, SCOR) and mathematicallyderived aortic wave (SCOR and MOG) was included in a previous work as Supplementary Material [12].
Using SCOR, central BP waves were derived from (i) radial (using a GTF) and (ii) carotid tonometric recordings (Figure 1). Only accurate waveforms on visual inspection and high-quality recordings (in-device quality index > 75%) were considered. Carotid artery pulse waves were assumed to be identical to the aortic ones (due to the proximity of the arterial sites) [12]. Thus, a GTF was not applied to obtain central waves from carotid records. In turn, brachial BP (bBP) levels and waveforms were obtained using the MOG (brachial cuff-based oscillometric/plethismographic device) [12]. The device determined central BP levels and waveforms from peripheral recordings using a validated GTF. Only high-quality records (index equal to 1 or 2) and satisfactory waves (visual inspection) were considered. Both devices (SCOR and MOG) quantify (local) PWV by proprietary algorithms (e.g., based on age, bSBP, pulse wave characteristics, transition time between WSA-derived forward and reflected components of the pulse wave) [30]. Data were named based on the recording site and device used: aoPWV_Radial_SCOR, aoPWV_Carotid_SCOR and aoPWV_Brachial_MOG (Figure 1).
2.7. CAVI and CAVIo Determination
Arterial stiffness (e.g., assessed by PWV) is influenced by BP levels during the examination, which, if not considered, could lead to inaccurate conclusions [5,6,31,32,33]. To overcome the problem of BP dependence, Shirai et al. proposed the use of the cardio-ankle vascular index (CAVI) [6], which “combines” the stiffness index β (commonly used to quantify local arterial stiffness) and the Bramwell–Hill equation, to obtain an index that can be calculated using arterial BP and PWV (unlike β which is calculated from arterial BP and diameter) [5,33]. CAVI was suggested to better reflect structural changes of the arterial wall (with independence of arterial distending BP). However, due to the use of bDBP instead of a fixed reference BP, both the stiffness index and CAVI theoretically have a residual dependence on BP. Additionally, CAVI exhibits BP dependence since it considers an estimated derivative of the pressure-diameter relationship. Recently, a BP-corrected CAVI (CAVIo) was proposed, which is suggested (theoretically) to represent a less BP-dependent stiffness index [5,33]. Although named cardio-ankle, the CAVI formula can equally well be applied to any PWV measurement [31,33]. CAVI or β-cfPWV was previously used in both children and adults [5,32]. In this work, CAVI and CAVIo were calculated as:
| CAVI = (Ln(bSBP/bDBP))*((PWV2*2ρ)/bSBP − bDBP)) | (1) |
| CAVIo = ((PWV2*2ρ)/bDBP) − Ln(bDBP/BPref) | (2) |
where Ln is natural logarithm, bSBP and bDBP are brachial systolic and diastolic BP, BPref is 100 mmHg, PWV is regional (cfPWV, crPWV) or local (aoPWV_Radial_SCOR, aoPWV_Carotid_SCOR, aoPWV_Brachial_MOG) PWV and ρ is blood mass density (assumed 1060 kg/m3) [5,33]. BP, PWV and ρ were entered into equation in Pa, m/s and kg/m3, respectively [5,33].
2.8. Arterial Stiffness Parameters
After completing the calculations, 18 stiffness-related parameters were obtained (Table 1).
Table 1.
PWV-, CAVI- and CAVIo-related parameters.
| PWV-Related Parameter | CAVI-Related Parameter | CAVIo-Related Parameter |
|---|---|---|
| cfPWV_Real_SCOR | CAVI_cfPWV_Real_SCOR | CAVIo_cfPWV_Real_SCOR |
| crPWV_SCOR | CAVI_crPWV_SCOR | CAVIo_crPWV_SCOR |
| aoPWV_Radial_SCOR | CAVI_aoPWV_Radial_SCOR | CAVIo_aoPWV_Radial_SCOR |
| aoPWV_Carotid_SCOR | CAVI_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Carotid_SCOR |
| aoPWV_Brachial_MOG | CAVI_aoPWV_Brachial_MOG | CAVIo_aoPWV_Brachial_MOG |
| PWV Ratio | CAVI_PWV_Ratio | CAVIo_PWV_Ratio |
2.9. Data Analysis
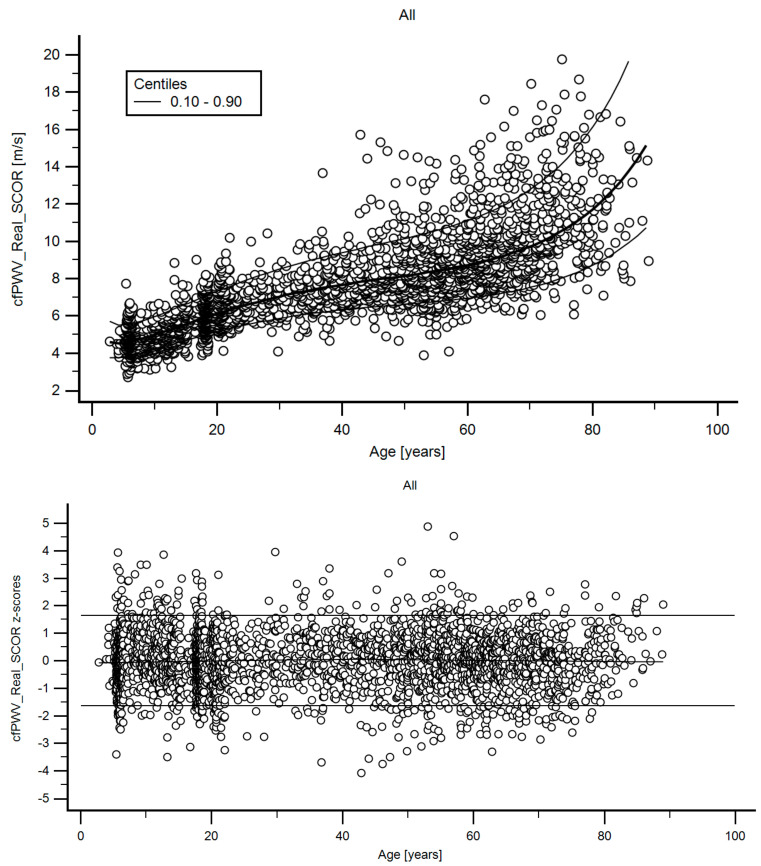
A step-wise analysis was performed. First, we assessed the association between age and arterial stiffness parameters, considering the whole population (n = 3169). Figure 2 shows the age-related profiles obtained for cfPWV. Similar data were obtained for the 18 PWV-related parameters.
Figure 2.
Top: Age-related cfPWV profile (10th, 50th, 90th percentiles). Bottom: z-score diagram used to verify model fit.
Second, considering the inclusion and exclusion criteria, subjects to be included in the RIs group were identified (n = 1289) (Table 2 and Table 3). Additional complimentary data and sex distribution for the entire population (n = 3619), excluded subjects (n = 2330) and for the RIs group (n = 1289) are included in Supplementary Material 1 (Tables S1–S3).
Table 2.
Subjects demographic, anthropometric and clinical characteristics.
| All Subjects (n = 3619) | Reference Intervals Group (n = 1289) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MV | SD | Min. | p25th | p50th | p75th | Max. | Range | MV | SD | Min. | p25th | p50th | p75th | Max. | Range | |
| Age (years) | 33.9 | 24.2 | 2.8 | 11.5 | 23.7 | 56.4 | 89.0 | 86.2 | 20.1 | 16.9 | 2.8 | 6.3 | 17.6 | 21.8 | 84.2 | 81.4 |
| BW (kg) | 61.1 | 25.3 | 12.3 | 45.6 | 63.2 | 78.1 | 150.6 | 138.3 | 47.9 | 22.8 | 12.3 | 22.6 | 52.8 | 65.2 | 105.0 | 92.7 |
| BH (m) | 1.55 | 0.23 | 0.90 | 1.46 | 1.62 | 1.71 | 1.97 | 1.07 | 1.47 | 0.26 | 0.90 | 1.17 | 1.58 | 1.69 | 1.94 | 1.04 |
| BMI (kg/m2) | 24.06 | 6.02 | 11.53 | 19.7 | 23.63 | 27.84 | 71.34 | 59.81 | 20.36 | 4.22 | 11.53 | 16.59 | 20 | 23.56 | 29.95 | 18.42 |
| z-BMI (SD) * | 0.94 | 1.45 | −4.63 | −0.05 | 0.74 | 1.77 | 8.03 | 12.66 | 0.34 | 0.92 | −4.63 | −0.27 | 0.41 | 1 | 1.98 | 6.61 |
| TC (mg/dL) | 200 | 44 | 94 | 170 | 196 | 227 | 379 | 285 | 195 | 26 | 99 | 179 | 198 | 214 | 238 | 139 |
| HDL (mg/dL) | 51 | 15 | 17 | 41 | 49 | 60 | 122 | 105 | 58 | 12 | 41 | 49 | 55 | 64 | 100 | 59 |
| LDL (mg/dL) | 123 | 40 | 28 | 95 | 119 | 146 | 323 | 295 | 118 | 26 | 31 | 101 | 121 | 134 | 180 | 149 |
| TG (mg/dL) | 133 | 86 | 24 | 80 | 111 | 158 | 783 | 759 | 93 | 39 | 24 | 65 | 86 | 113 | 272 | 248 |
| Glic. (mg/dL) | 94 | 19 | 40 | 85 | 92 | 100 | 307 | 267 | 88 | 9 | 40 | 83 | 88 | 93 | 121 | 81 |
| bSBP (mmHg) | 119 | 17 | 64 | 107 | 118 | 129 | 235 | 171 | 112 | 13 | 80 | 101 | 112 | 121 | 171 | 91 |
| bDBP (mmHg) | 69 | 10 | 41 | 61 | 68 | 76 | 129 | 88 | 65 | 8 | 47 | 59 | 63 | 70 | 97 | 51 |
| TC ≥240 mg/dL (%) | 7.20 | 0.00 | ||||||||||||||
| HDL <40 mg/dL (%) | 8.90 | 0.00 | ||||||||||||||
| Glic. ≥126 (%) mg/dL | 0.90 | 0.00 | ||||||||||||||
| Current Smoker (%) | 11.40 | 0.00 | ||||||||||||||
| Hypertension (%) | 26.40 | 0.00 | ||||||||||||||
| Diabetes (%) | 5.70 | 0.00 | ||||||||||||||
| History of CVD (%) | 8.80 | 0.00 | ||||||||||||||
| Obesity (%) | 22.60 | 0.00 | ||||||||||||||
| Family CVD (%) | 13.50 | 7.60 | ||||||||||||||
| Sedentarism (%) | 45.60 | 32.30 | ||||||||||||||
| Anti-hypertensive (%) | 21.70 | 0.00 | ||||||||||||||
| Anti-hyperlip. (%) | 13.50 | 0.00 | ||||||||||||||
| Anti-diabetic (%) | 4.10 | 0.00 | ||||||||||||||
| Atheroma plaques (%) | ||||||||||||||||
| 0 | 64.70 | 88.20 | ||||||||||||||
| 1 | 6.20 | 2.70 | ||||||||||||||
| 2 | 8.10 | 4.20 | ||||||||||||||
| 3 | 6.40 | 1.90 | ||||||||||||||
| 4 | 6.50 | 1.80 | ||||||||||||||
| 5 | 3.20 | 0.60 | ||||||||||||||
| 6 | 3.00 | 0.30 | ||||||||||||||
| 7 | 1.20 | 0.10 | ||||||||||||||
| 8 | 0.70 | 0.10 | ||||||||||||||
MV: mean value. SD: standard deviation. Min. and Max.: minimum and maximum values. p25th, p50th (median) and p75th: 25, 50 and 75 percentiles. BMI: body mass index. bSBP, bDBP: brachial systolic and diastolic blood pressure. CVD: cardiovascular disease. TC: total cholesterol. TG: Triglycerides. Glic: Glycemia. Hyperlip: hyperlipidemic Atheroma plaques refers to plaques in common, internal and external carotid arteries; common femoral arteries (both hemibodies; 8 segments); presented as% of subjects with 0, 1, 2, ...., 8 segments affected. * only for <18 y. BW: body weight. BH: Body height.
Table 3.
Arterial stiffness parameters.
| All Subjects (n = 3619) | Reference Intervals Group (n = 1289) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MV | SD | Min. | p25th | p50th | p75th | Max. | Range | MV | SD | Min. | p25th | p50th | p75th | Max. | Range | |
| cfPWV_Real_SCOR | ||||||||||||||||
| bSBP (mmHg) | 120 | 17 | 63 | 110 | 120 | 130 | 211 | 148 | 114 | 14 | 79 | 103 | 113 | 122 | 167 | 88 |
| bDBP (mmHg) | 69 | 11 | 40 | 60 | 69 | 76 | 127 | 87 | 64 | 9 | 40 | 58 | 63 | 70 | 100 | 60 |
| HR (b.p.m.) | 73 | 15 | 35 | 62 | 71 | 82 | 149 | 114 | 75 | 15 | 40 | 64 | 74 | 85 | 134 | 94 |
| cfPWV_Real_SCOR (m/s) | 7.39 | 2.46 | 2.7 | 5.57 | 7 | 8.72 | 19.75 | 17.06 | 6.23 | 1.63 | 2.7 | 5.04 | 5.98 | 7.13 | 14.59 | 11.89 |
| CAVI_cfPWV_Real_SCOR | 10.06 | 6.6 | 1.61 | 5.73 | 8.3 | 12.32 | 65.22 | 63.62 | 7.34 | 3.56 | 1.61 | 4.97 | 6.57 | 8.84 | 33.43 | 31.82 |
| CAVIo_cfPWV_Real_SCOR | 13.89 | 9.09 | 2.62 | 8.2 | 11.45 | 16.47 | 97.39 | 94.77 | 10.31 | 4.68 | 2.7 | 7.13 | 9.36 | 12.24 | 46.84 | 44.14 |
| crPWV_SCOR | ||||||||||||||||
| bSBP (mmHg) | 120 | 15 | 71 | 110 | 119 | 129 | 195 | 124 | 115 | 13 | 71 | 106 | 114 | 124 | 162 | 91 |
| bDBP (mmHg) | 68 | 10 | 40 | 60 | 68 | 76 | 102 | 62 | 65 | 9 | 43 | 58 | 64 | 70 | 100 | 57 |
| HR (b.p.m.) | 71 | 13 | 35 | 61 | 69 | 79 | 140 | 105 | 72 | 14 | 40 | 62 | 70 | 81 | 131 | 91 |
| crPWV_SCOR (m/s) | 9.3 | 1.97 | 4.4 | 7.8 | 9.2 | 10.7 | 15.7 | 11.3 | 8.76 | 1.76 | 4.4 | 7.5 | 8.5 | 9.9 | 14.9 | 10.5 |
| CAVI_crPWV_SCOR | 15.47 | 5.6 | 3.11 | 11.32 | 15.03 | 19.04 | 47.5 | 44.39 | 14.38 | 5.18 | 4.46 | 10.87 | 13.35 | 17.27 | 47.5 | 43.04 |
| CAVIo_crPWV_SCOR | 21.11 | 7.14 | 3.8 | 15.9 | 20.72 | 25.59 | 63.07 | 59.28 | 19.86 | 6.72 | 6.79 | 15.18 | 18.73 | 23.49 | 63.07 | 56.28 |
| PWV Ratio (cfPWV_Real_SCOR/crPWV_SCOR) | ||||||||||||||||
| PWV_Ratio | 0.78 | 0.19 | 0.35 | 0.65 | 0.74 | 0.87 | 1.86 | 1.51 | 0.72 | 0.15 | 0.35 | 0.62 | 0.71 | 0.8 | 1.49 | 1.14 |
| CAVI_PWV_Ratio | 0.64 | 0.35 | 0.12 | 0.42 | 0.56 | 0.76 | 3.67 | 3.55 | 0.54 | 0.23 | 0.12 | 0.38 | 0.5 | 0.64 | 2.3 | 2.18 |
| CAVIo_PWV_Ratio | 0.65 | 0.34 | 0.13 | 0.43 | 0.57 | 0.76 | 3.87 | 3.74 | 0.55 | 0.23 | 0.13 | 0.39 | 0.52 | 0.65 | 2.36 | 2.23 |
| aoPWV_Radial_SCOR | ||||||||||||||||
| bSBP (mmHg) | 121 | 16 | 77 | 109 | 120 | 130 | 235 | 158 | 114 | 14 | 78 | 105 | 114 | 124 | 160 | 82 |
| bDBP (mmHg) | 69 | 11 | 37 | 61 | 69 | 76 | 130 | 93 | 65 | 9 | 42 | 59 | 64 | 71 | 95 | 53 |
| HR (b.p.m.) | 73 | 14 | 35 | 63 | 71 | 82 | 151 | 116 | 76 | 15 | 38 | 65 | 74 | 85 | 151 | 113 |
| aoPWV_Radial_SCOR (m/s) | 7.24 | 1.25 | 4 | 6.5 | 7.2 | 8 | 14.3 | 10.3 | 6.73 | 1.15 | 4 | 6 | 6.8 | 7.4 | 11.2 | 7.2 |
| CAVI_aoPWV_Radial_SCOR | 9.21 | 2.92 | 3.16 | 7.31 | 8.8 | 10.58 | 33.55 | 30.39 | 8.41 | 2.62 | 3.37 | 6.72 | 8.2 | 9.68 | 21.7 | 18.33 |
| CAVIo_aoPWV_Radial_SCOR | 12.82 | 4.07 | 4.51 | 10.12 | 12.28 | 14.76 | 46.81 | 42.3 | 11.9 | 3.71 | 4.51 | 9.56 | 11.44 | 13.77 | 28.85 | 24.34 |
| aoPWV_Carotid_SCOR | ||||||||||||||||
| bSBP (mmHg) | 121 | 18 | 78 | 109 | 120 | 131 | 239 | 161 | 114 | 15 | 78 | 104 | 114 | 124 | 217 | 139 |
| bDBP (mmHg) | 69 | 11 | 38 | 60 | 68 | 76 | 127 | 89 | 64 | 9 | 38 | 58 | 63 | 70 | 100 | 62 |
| HR (b.p.m.) | 72 | 14 | 32 | 61 | 70 | 80 | 145 | 113 | 75 | 15 | 40 | 64 | 74 | 84 | 145 | 105 |
| aoPWV_Carotid_SCOR (m/s) | 7.01 | 1.02 | 4 | 6.4 | 7 | 7.6 | 13.2 | 9.2 | 6.68 | 0.97 | 4 | 6.2 | 6.6 | 7.2 | 13.2 | 9.2 |
| CAVI_aoPWV_Carotid_SCOR | 8.51 | 2.44 | 2.94 | 6.95 | 8.11 | 9.58 | 29.7 | 26.76 | 8.08 | 2.42 | 2.94 | 6.68 | 7.73 | 8.98 | 28.59 | 25.65 |
| CAVIo_aoPWV_Carotid_SCOR | 11.85 | 3.46 | 3.99 | 9.66 | 11.25 | 13.41 | 40.02 | 36.03 | 11.47 | 3.54 | 3.99 | 9.37 | 10.84 | 12.79 | 39.94 | 35.95 |
| aoPWV_Brachial_MOG | ||||||||||||||||
| bSBP (mmHg) | 117 | 14 | 81 | 107 | 115 | 125 | 199 | 118 | 112 | 12 | 81 | 104 | 111 | 120 | 158 | 77 |
| bDBP (mmHg) | 68 | 11 | 36 | 60 | 67 | 75 | 131 | 95 | 65 | 9 | 39 | 58 | 64 | 70 | 106 | 67 |
| HR (b.p.m.) | 76 | 15 | 33 | 64 | 73 | 86 | 135 | 102 | 79 | 16 | 41 | 67 | 77 | 89 | 135 | 94 |
| aoPWV_Brachial_MOG (m/s) | 5.74 | 2.07 | 3.58 | 4.33 | 4.88 | 6.36 | 15.25 | 11.68 | 4.87 | 1.18 | 3.58 | 4.15 | 4.55 | 5.08 | 12.93 | 9.36 |
| CAVI_aoPWV_Brachial_MOG | 6.26 | 4.55 | 2.84 | 3.58 | 4.21 | 6.7 | 31.45 | 28.62 | 4.55 | 2.46 | 2.84 | 3.4 | 3.83 | 4.55 | 28.09 | 25.25 |
| CAVIo_aoPWV_Brachial_MOG | 8.64 | 5.84 | 3.86 | 5.21 | 6.25 | 9.15 | 46.01 | 42.15 | 6.51 | 3.19 | 3.9 | 4.92 | 5.57 | 6.74 | 38.9 | 35 |
Abbreviations: similar to Table 1. HR: heart rate. Other abbreviations: see the text.
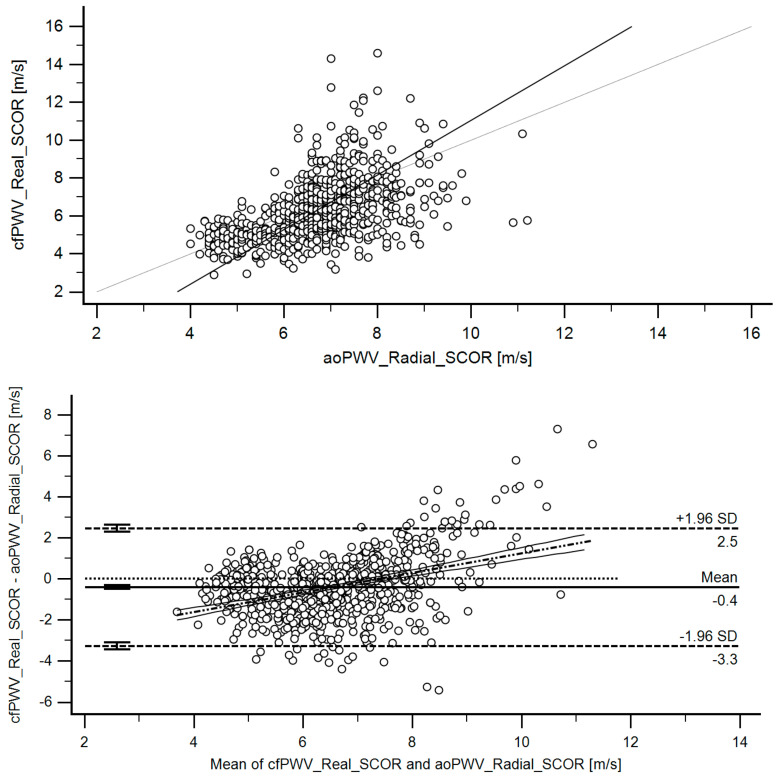
Third, working with the RIs group, we first analyzed the agreement between the methods used to assess aortic stiffness. Concordance correlation coefficients (CCC) (Table 4) and Bland–Altman tests were considered (Table 5). Figure 3 exemplifies CCC analysis and Bland–Altman graph obtained when comparing cfPWV_Real_SCOR and aoPWV_Radial_SCOR. Similar analyses were done for different parameters. The above enabled us to identify that the approaches and parameters considered did not provide similar data; they were not equivalent. Therefore, it was necessary to define the RIs for each parameter.
Table 4.
Concordance correlation coefficients between PWV parameters (Reference Interval Group).
| cfPWV (Variable Y) vs. aoPWV_Radial_SCOR, aoPWV_Carotid_SCOR or aoPWV_Brachial_MOG | |||
| Variable X | aoPWV_Radial_SCOR | aoPWV_Carotid_SCOR | aoPWV_Brachial_MOG |
| CCC | 0.448 | 0.271 | 0.614 |
| 95% C.I. CCC | 0.3963 to 0.4967 | 0.2073 to 0.3319 | 0.5727 to 0.6527 |
| Pearson ρ (precision) | 0.498 | 0.3145 | 0.7336 |
| p-value (Pearson) | <1.0 × 10−14 | <1.0 × 10−14 | <1.0 × 10−14 |
| aoPWV_Radial_SCOR vs. aoPWV_Carotid_SCOR vs. aoPWV_Brachial_MOG | |||
| Variable Y | aoPWV_Radial_SCOR | aoPWV_Radial_SCOR | aoPWV_Carotid_SCOR |
| Variable X | aoPWV_Carotid_SCOR | aoPWV_Brachial_MOG | aoPWV_Brachial_MOG |
| CCC | 0.617 | 0.235 | 0.109 |
| 95% C.I. CCC | 0.5661 to 0.6632 | 0.1851 to 0.2838 | 0.04981 to 0.1668 |
| Pearson ρ (precision) | 0.6425 | 0.4205 | 0.1882 |
| p-value (Pearson) | <1.0 × 10−14 | <1.0 × 10−14 | 0.000257 |
| CAVI_cfPWV (Variable Y) vs. CAVI_aoPWV: Radial_SCOR, Carotid_SCOR or Brachial_MOG | |||
| Variable Y | CAVI_cfPWV_Real_SCOR | CAVI_cfPWV_Real_SCOR | CAVI_cfPWV_Real_SCOR |
| Variable X | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Carotid_SCOR | CAVI_aoPWV_Brachial_MOG |
| CCC | 0.2779 | 0.09839 | 0.553 |
| 95% C.I. CCC | 0.2181 to 0.3355 | 0.02888 to 0.1670 | 0.5073 to 0.5956 |
| Pearson ρ (precision) | 0.3075 | 0.1115 | 0.6704 |
| p-value (Pearson) | <1.0 × 10−14 | 0.0057 | <1.0 × 10−14 |
| CAVI_aoPWV_Radial_SCOR vs. CAVI_aoPWV_Carotid_SCOR vs. CAVI_aoPWV_Brachial_MOG | |||
| Variable Y | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Carotid_SCOR |
| Variable X | CAVIo_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Brachial_MOG | CAVIo_aoPWV_Brachial_MOG |
| CCC | 0.5133 | 0.1439 | 0.03279 |
| 95% C.I. CCC | 0.4538 to 0.5682 | 0.09252 to 0.1944 | −0.03191 to 0.09722 |
| Pearson ρ (precision) | 0.5389 | 0.2545 | 0.05159 |
| p-value (Pearson) | <1.0 × 10−14 | 2.36 × 10−8 | 0.3203 |
| CAVIo_cfPWV (variable Y) vs. CAVIo_aoPWV: Radial_SCOR, Carotid_SCOR or Brachial_MOG | |||
| Variable X | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Brachial_MOG |
| CCC | 0.2294 | 0.08023 | 0.5078 |
| 95% C.I. CCC | 0.1671 to 0.2898 | 0.007051 to 0.1526 | 0.4608 to 0.5518 |
| Pearson ρ (precision) | 0.25 | 0.08661 | 0.6402 |
| p-value (Pearson) | 2.02E−12 | 0.0319 | 1.00 × 10−14 |
| CAVIo_aoPWV_Radial_SCOR vs. CAVIo_aoPWV_Carotid_SCOR vs. CAVIo_aoPWV_Brachial_MOG | |||
| Variable Y | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Carotid_SCOR |
| Variable X | CAVIo_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Brachial_MOG | CAVIo_aoPWV_Brachial_MOG |
| CCC | 0.5623 | 0.08684 | 0.008803 |
| 95% C.I. CCC | 0.5064 to 0.6134 | 0.03752 to 0.1357 | −0.05276 to 0.07029 |
| Pearson ρ (precision) | 0.5864 | 0.1604 | 0.01454 |
| p-value (Pearson) | <1.0 × 10−14 | 4.97 × 10−4 | 7.80 × 10−1 |
CCC: concordance correlation coefficient. C.I.: confidence interval.
Table 5.
Bland–Altman test between arterial stiffness parameters (Reference Interval Group).
| Part 1 | |||||||||
| (1) cfPWV (Method A) vs. aoPWV: Radial_SCOR, Carotid_SCOR or Brachial_MOG | |||||||||
| Method B | aoPWV_Radial_SCOR | aoPWV_Carotid_SCOR | aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error (m/s) | −0.41 | −0.14 | 0.81 | ||||||
| Mean error, 95% CI (m/s) | −0.5123 to −0.3052 | −0.2624 to −0.009219 | 0.7308 to 0.8833 | ||||||
| Mean error, P (H0: Mean = 0) | 2.99 × 10−14 | 3.55 × 10−2 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit (m/s) | −3.2767 | −3.2661 | −1.1438 | ||||||
| Mean error, 95% CI (m/s) | −3.4538 to −3.0996 | −3.4826 to −3.0497 | −1.2742 to −1.0134 | ||||||
| Mean error, Upper limit (m/s) | 2.4592 | 2.9945 | 2.7578 | ||||||
| Mean error, 95% CI (m/s) | 2.2821 to 2.6363 | 2.7781 to 3.2110 | 2.6274 to 2.8882 | ||||||
| Mean error, Regression Eq. | y = −3.5184 + 0.4766x | y =−5.3391 + 0.7875x | y = −0.1298 + 0.1732x | ||||||
| Parameter | |||||||||
| Intercept, Coeff. (m/s) | −3.5184 | −5.3391 | −0.1298 | ||||||
| Intercept, Coeff. 95% CI (m/s) | −4.0397 to −2.9971 | −6.0251 to −4.6530 | −0.4615 to 0.2019 | ||||||
| Intercept, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | 0.4425 | ||||||
| Slope | |||||||||
| Slope, Coeff. (m/s/y) | 0.4766 | 0.7875 | 0.1732 | ||||||
| Slope, Coeff. 95% CI (m/s/y) | 0.3980 to 0.5551 | 0.6850 to 0.8900 | 0.1135 to 0.2330 | ||||||
| Slope, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | 0.000 | ||||||
| (2) aoPWV_Radial_SCOR vs. aoPWV_Carotid_SCOR vs. aoPWV_Brachial_MOG | |||||||||
| Method A | aoPWV_Radial_SCOR | aoPWV_Radial_SCOR | aoPWV_Carotid_SCOR | ||||||
| Method B | aoPWV_Carotid_SCOR | aoPWV_Brachial_MOG | aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error (m/s) | 0.28 | 1.49 | 1.38 | ||||||
| Mean error, 95% CI (m/s) | 0.2122 to 0.3457 | 1.3754 to 1.6096 | 1.2300 to 1.5345 | ||||||
| Mean error, P (H0: Mean = 0) | <1.0 × 10−14 | <1.0 × 10−14 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit (m/s) | −1.3327 | −1.0341 | −1.5492 | ||||||
| Mean error, 95% CI (m/s) | −1.4469 to −1.2185 | −1.2344 to −0.8339 | −1.8097 to −1.2887 | ||||||
| Mean error, Upper limit (m/s) | 1.8907 | 4.0192 | 4.3137 | ||||||
| Mean error, 95% CI (m/s) | 1.7765 to 2.0049 | 3.8189 to 4.2194 | 4.0532 to 4.5742 | ||||||
| Mean error, Regression Eq. | y = 0.2207 + 0.008533x | y = 2.2722−0.1320x | y = 3.3683−0.3309x | ||||||
| Intercept | |||||||||
| Intercept, Coeff. (m/s) | 0.2207 | 2.2722 | 3.3683 | ||||||
| Intercept, Coeff. 95% CI (m/s) | −0.3024 to 0.7437 | 1.5775 to 2.9670 | 2.3609 to 4.3756 | ||||||
| Intercept, Coeff. p-value | 0.4077 | 3.23 × 10−10 | 1.65 × 10−10 | ||||||
| Slope | |||||||||
| Slope, Coeff. (m/s/y) | 0.008533 | −0.132 | −0.3309 | ||||||
| Slope, Coeff. 95% CI (m/s/y) | −0.06737 to 0.08444 | −0.2479 to −0.01605 | −0.4969 to −0.1649 | ||||||
| Slope, Coeff. p-value | 0.8253 | 0.0258 | 0.000 | ||||||
| Part 2 | |||||||||
| (3) CAVI_cfPWV_Real_SCOR (Method A) vs. CAVI_aoPWV: Radial_SCOR, Carotid_SCOR or Brachial_MOG | |||||||||
| Method B | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Carotid_SCOR | CAVI_aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error | −0.89 | −0.12 | 1.81 | ||||||
| Mean error, 95% CI | −1.1609 to −0.6148 | −0.4612 to 0.2183 | 1.6231 to 1.9921 | ||||||
| Mean error, P (H0: Mean = 0) | 3.00 × 10−10 | 4.83 × 10−1 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit | −8.4481 | −8.5235 | −2.9128 | ||||||
| Mean error, 95% CI | −8.9150 to −7.9813 | −9.1045 to −7.9426 | −3.2283 to −2.5973 | ||||||
| Mean error, Upper limit | 6.6724 | 8.2806 | 6.5281 | ||||||
| Mean error, 95% CI | 6.2055 to 7.1392 | 7.6997 to 8.8615 | 6.2126 to 6.8436 | ||||||
| Mean error, Regression Eq. | y = −5.1891 + 0.5399x | y = −6.9488 + 0.8540x | y = 0.5711 + 0.2188x | ||||||
| Intercept | |||||||||
| Intercept, Coeff. | −5.1891 | −6.9488 | 0.5711 | ||||||
| Intercept, Coeff. 95% CI | −6.0114 to −4.3667 | −8.0063 to −5.8912 | 0.1496 to 0.9925 | ||||||
| Intercept, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | 0.008 | ||||||
| Slope | |||||||||
| Slope, Coeff. | 0.5399 | 0.854 | 0.2188 | ||||||
| Slope, Coeff. 95% CI | 0.4418 to 0.6381 | 0.7272 to 0.9809 | 0.1513 to 0.2862 | ||||||
| Slope, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | <0.0001 | ||||||
| (4) CAVI_aoPWV_Radial_SCOR vs. CAVI_aoPWV_Carotid_SCOR vs. CAVI_aoPWV_Brachial_MOG | |||||||||
| Method A | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Radial_SCOR | CAVI_aoPWV_Carotid_SCOR | ||||||
| Method B | CAVI_aoPWV_Carotid_SCOR | CAVI_aoPWV_Brachial_MOG | CAVI_aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error | 0.76 | 3.34 | 3.02 | ||||||
| Mean error, 95% CI | 0.5752 to 0.9524 | 3.0420 to 3.6416 | 2.6246 to 3.4233 | ||||||
| Mean error, P (H0: Mean = 0) | <1.0 × 10−14 | <1.0 × 10−14 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit | −3.7885 | −3.1272 | −4.6633 | ||||||
| Mean error, 95% CI | −4.1111 to −3.4660 | −3.6399 to −2.6145 | −5.3464 to −3.9803 | ||||||
| Mean error, Upper limit | 5.3161 | 9.8107 | 10.7112 | ||||||
| Mean error, 95% CI | 4.9936 to 5.6386 | 9.2980 to 10.3235 | 10.0282 to 11.3943 | ||||||
| Mean error, Regression Eq. | y = 0.8012 − 0.004401x | y = 3.9494 − 0.09117x | y = 4.3010 − 0.1895x | ||||||
| Intercept | |||||||||
| Intercept, Coeff. | 0.8012 | 3.9494 | 4.301 | ||||||
| Intercept, Coeff. 95% CI | 0.02191 to 1.5804 | 2.9684 to 4.9304 | 2.9409 to 5.6611 | ||||||
| Intercept, Coeff. p-value | 0.0439 | 1.87 × 10−14 | 1.36 × 10−9 | ||||||
| Slope | |||||||||
| Slope, Coeff. | −0.004401 | −0.09117 | −0.1895 | ||||||
| Slope, Coeff. 95% CI | −0.09345 to 0.08465 | −0.2313 to 0.04899 | −0.3825 to 0.003503 | ||||||
| Slope, Coeff. p-value | 0.9227 | 0.2018 | 0.054 | ||||||
| Part 3 | |||||||||
| (5) CAVIo_cfPWV_Real_SCOR (Method A) vs. CAVIo_aoPWV: Radial_SCOR, Carotid_SCOR orBrachial_MOG | |||||||||
| Method B | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error | −1.29 | −0.28 | 2.63 | ||||||
| Mean error, 95% CI | −1.6699 to −0.9076 | −0.7459 to 0.1913 | 2.3706 to 2.8798 | ||||||
| Mean error, P (H0: Mean = 0) | 6.03 × 10−11 | 0.2456 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit | −11.8424 | −11.8658 | −3.8891 | ||||||
| Mean error, 95% CI | −12.4942 to −11.1907 | −12.6671 to −11.0646 | −4.3245 to −3.4538 | ||||||
| Mean error, Upper limit | 9.2649 | 11.3112 | 9.1395 | ||||||
| Mean error, 95% CI | 8.6132 to 9.9166 | 10.5100 to 12.1125 | 8.7041 to 9.5748 | ||||||
| Mean error, Regression Eq. | y = −6.5225 + 0.4651x | y = −8.0619 + 0.6887x | y = 0.5729 + 0.2545x | ||||||
| Intercept | |||||||||
| Intercept, Coeff. | −6.5225 | −8.0619 | 0.5729 | ||||||
| Intercept, Coeff. 95% CI | −7.7702 to −5.2748 | −9.6582 to −6.4655 | −0.04940 to 1.1952 | ||||||
| Intercept, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | 0.0711 | ||||||
| Slope | |||||||||
| Slope, Coeff. | 0.4651 | 0.6887 | 0.2545 | ||||||
| Slope, Coeff. 95% CI | 0.3591 to 0.5712 | 0.5528 to 0.8246 | 0.1836 to 0.3255 | ||||||
| Slope, Coeff. p-value | <1.0 × 10−14 | <1.0 × 10−14 | 4.61 × 10−12 | ||||||
| (6) CAVIo_aoPWV_Radial_SCOR vs. CAVIo_aoPWV_Carotid_SCOR vs. CAVIo_aoPWV_Brachial_MOG | |||||||||
| Method A | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Radial_SCOR | CAVIo_aoPWV_Carotid_SCOR | ||||||
| Method B | CAVIo_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Brachial_MOG | CAVIo_aoPWV_Brachial_MOG | ||||||
| Differences (Method A-Method B) | |||||||||
| Mean error | 1.02 | 4.82 | 4.45 | ||||||
| Mean error, 95% CI | 0.7615 to 1.2788 | 4.3819 to 5.2562 | 3.8948 to 5.0112 | ||||||
| Mean error, P (H0: Mean = 0) | 4.22 × 10−14 | <1.0 × 10−14 | <1.0 × 10−14 | ||||||
| Mean error, Lower limit | −5.2235 | −4.6138 | −6.2933 | ||||||
| Mean error, 95% CI | −5.6658 to −4.7812 | −5.3615 to −3.8662 | −7.2482 to −5.3384 | ||||||
| Mean error, Upper limit | 7.2638 | 14.2519 | 15.1993 | ||||||
| Mean error, 95% CI | 6.8215 to 7.7061 | 13.5042 to 14.9995 | 14.2444 to 16.1542 | ||||||
| Mean error, Regression Eq. | y = 1.4747 − 0.03782x | y = 3.9543 + 0.09114x | y = 4.3849 + 0.007097x | ||||||
| Intercept | |||||||||
| Intercept, Coeff. | 1.4747 | 3.9543 | 4.3849 | ||||||
| Intercept, Coeff. 95% CI | 0.4438 to 2.5056 | 2.4230 to 5.4856 | 2.3751 to 6.3948 | ||||||
| Intercept, Coeff. p-value | 0.0051 | 0.000000562 | 0.0000228 | ||||||
| Slope | |||||||||
| Slope, Coeff. | −0.03782 | 0.09114 | 0.007097 | ||||||
| Slope, Coeff. 95% CI | −0.1209 to 0.04522 | −0.06354 to 0.2458 | −0.1941 to 0.2083 | ||||||
| Slope, Coeff. p-value | 0.3714 | 0.2475 | 0.9447 | ||||||
Eq.: Equation. C.I.: confidence interval. SE: standard error. m: meter. s: second. y: year. Coeff.: Coefficient.
Figure 3.
Top: Association (scatter diagram) between cfPWV_RealSCOR and aoPWV_Radial-SCOR for the RI Group. r: 0.4980 (95% C.I.: 0.4429–0.5493). p < 1.0 × 10−14. Bottom: Bland–Altman diagram. There were statistically significant mean (−0.41 m/s) and proportional errors. Table 5 (Part 1) shows quantitative data.
Fourth, we analyzed the association between carotid and/or femoral atherosclerotic plaque presence (asymptomatic subjects) and PWV data by means of point-biserial correlations without and with Bootstrapping (sample number = 1000; bias-corrected accelerated confidence intervals; simple sampling) (Table 6). In subjects non-exposed to CRFs (RIs Group), plaque presence was not associated with cfPWV, crPWV or aoPWV levels. Then, subjects with atherosclerotic plaques were not excluded from that group. As a result, our exclusion criteria agreed with those of the European Reference Values for Arterial Measurements Collaboration Group [18,19,20,21].
Table 6.
Association between stiffness parameter and plaque presence or sex (adjusted by age and/or sex).
| aoPWV | ||||||
|---|---|---|---|---|---|---|
| cfPWV_Real_SCOR (m/s) | crPWV_SCOR (m/s) | Radial_SCOR (m/s) | Carotid_SCOR (m/s) | Brachial_MOG (m/s) | ||
| Atherosclerotic plaques (Yes: 1; No:0) (*) | r * | 0.107 | −0.109 | −0.054 | −0.034 | 0.090 |
| p (2-tailed) | 0.072 | 0.066 | 0.362 | 0.563 | 0.130 | |
| Boot, Bias | −0.003 | 0.001 | −0.002 | −0.002 | 0.003 | |
| Boot, SE | 0.085 | 0.057 | 0.057 | 0.035 | 0.097 | |
| Boot 95%CI LL | −0.069 | −0.216 | −0.166 | −0.102 | −0.100 | |
| Boot 95%CI UL | 0.269 | −0.002 | 0.056 | 0.037 | 0.283 | |
| Atherosclerotic plaques (Yes: 1; No:0] (**) | r ** | 0.104 | −0.108 | −0.052 | −0.036 | 0.086 |
| p (2-tailed) | 0.080 | 0.071 | 0.384 | 0.552 | 0.149 | |
| Boot, Bias | −0.007 | −0.003 | 0.002 | −0.001 | 0.004 | |
| Boot, SE | 0.090 | 0.055 | 0.062 | 0.036 | 0.104 | |
| Boot 95%CI LL | −0.082 | −0.222 | −0.169 | −0.104 | −0.110 | |
| Boot 95%CI UL | 0.272 | −0.006 | 0.070 | 0.037 | 0.294 | |
| Sex (Female: 1; Male:0) (*) | r * | −0.123 | 0.079 | 0.091 | −0.038 | −0.224 |
| p (2-tailed) | 0.039 | 0.184 | 0.127 | 0.526 | 0.000 | |
| Boot, Bias | 0.002 | 0.003 | 0.002 | −0.001 | −0.005 | |
| Boot, SE | 0.056 | 0.059 | 0.055 | 0.060 | 0.060 | |
| Boot 95%CI, LL | −0.229 | −0.038 | −0.016 | −0.153 | −0.351 | |
| Boot 95%CI UL | −0.009 | 0.192 | 0.194 | 0.076 | −0.115 | |
(*) adjusted by age (years). (**) adjusted by age (years) and sex (Female: 1; Male: 0). Boot: bootstrap. SE: standard error. CI: confidence interval. LL: lower limit. UL: Upper limit.
Fifth, we evaluated whether it was necessary to define sex-specific RIs using: (i) bivariate partial correlations (age-adjusted) and (ii) interaction analysis (Sex*Age) with theJohnson-Neyman significance regions definition (Table 7). Variables “y”, “x” and “w” (moderating variable) were assigned, respectively, to the stiffness parameter (e.g., cfPWV_Real_SCOR), sex and age. Then we identified: (i) parameters that would require RIs for males and females only from a certain age (cfPWV_Real_SCOR and crPWV_SCOR), (ii) parameters that would require sex-specific RIs for all ages (aoPWV_Brachial_MOG) and (iii) parameters that would not require sex-specific RIs (aoPWV_Radial_SCOR and aoPWV_Carotid_SCOR) (Table 7). In all cases, however, we decided to define RIs for all the subjects, as well as for females and males separately.
Table 7.
(Part 1). Interaction between age and sex as a determinant of cfPWV_Real_SCOR (m/s). (Part 2). Interaction between age and sex as a determinant of crPWV_SCOR (m/s). (Part 3). Interaction between age and sex as a determinant of aoPWV values.
| Part 1 | |||||||||||||||
| Model Summary (y: cfPWV_Real_SCOR; x: Sex; w: Age): R = 0.803; R2 = 0.6534; p = <0.0001 | |||||||||||||||
| Coeff | SE | p | 95% CI LL | 95% CI UL | |||||||||||
| Intercept | 4.4829 | 0.0617 | <0.0001 | 4.3618 | 4.604 | ||||||||||
| Sex (Female: 1; Male: 0) | 0.0641 | 0.0882 | 0.4671 | −0.1088 | 0.2371 | ||||||||||
| Age (years) | 0.0784 | 0.0021 | <0.0001 | 0.0743 | 0.0825 | ||||||||||
| Sex * Age | −0.0087 | 0.003 | 0.0041 | −0.0146 | −0.0028 | ||||||||||
| Moderator value(s) defining Johnson-Neyman significance region(s) | |||||||||||||||
| Value (years) | % below | % above | |||||||||||||
| 19.6737 | 60.4344 | 39.5656 | |||||||||||||
| Conditional effect of focal predictor at values of the moderator | |||||||||||||||
| Age (years) | Effect | SE | p | 95% CI LL | 95% CI UL | ||||||||||
| 2.80 | 0.0398 | 0.0816 | 0.626 | −0.1203 | 0.1998 | ||||||||||
| 6.87 | 0.0044 | 0.0727 | 0.952 | −0.1384 | 0.1471 | ||||||||||
| 10.94 | −0.031 | 0.065 | 0.633 | −0.1586 | 0.0966 | ||||||||||
| 15.01 | −0.0665 | 0.0589 | 0.260 | −0.1821 | 0.0491 | ||||||||||
| 19.08 | −0.1019 | 0.0549 | 0.064 | −0.2096 | 0.0059 | ||||||||||
| 19.67 | −0.107 | 0.0546 | 0.050 | −0.2141 | 0 | ||||||||||
| 23.15 | −0.1373 | 0.0535 | 0.011 | −0.2423 | −0.0323 | ||||||||||
| 27.22 | −0.1727 | 0.0549 | 0.002 | −0.2804 | −0.0649 | ||||||||||
| 31.29 | −0.2081 | 0.0589 | 0.000 | −0.3237 | −0.0925 | ||||||||||
| 35.36 | −0.2435 | 0.065 | 0.000 | −0.3711 | −0.1159 | ||||||||||
| 39.43 | −0.2789 | 0.0728 | 0.000 | −0.4216 | −0.1362 | ||||||||||
| 43.50 | −0.3143 | 0.0816 | 0.000 | −0.4744 | −0.1542 | ||||||||||
| 47.57 | −0.3497 | 0.0913 | 0.000 | −0.5288 | −0.1707 | ||||||||||
| 51.64 | −0.3851 | 0.1015 | 0.000 | −0.5842 | −0.186 | ||||||||||
| 55.71 | −0.4205 | 0.1121 | 0.000 | −0.6405 | −0.2005 | ||||||||||
| 59.78 | −0.456 | 0.1231 | 0.000 | −0.6975 | −0.2144 | ||||||||||
| 63.85 | −0.4914 | 0.1343 | 0.000 | −0.7548 | −0.2279 | ||||||||||
| 67.92 | −0.5268 | 0.1457 | 0.000 | −0.8126 | −0.241 | ||||||||||
| 71.99 | −0.5622 | 0.1572 | 0.000 | −0.8706 | −0.2538 | ||||||||||
| 76.06 | −0.5976 | 0.1688 | 0.000 | −0.9288 | −0.2664 | ||||||||||
| 80.13 | −0.633 | 0.1806 | 0.001 | −0.9872 | −0.2788 | ||||||||||
| 84.20 | −0.6684 | 0.1924 | 0.001 | −1.0458 | −0.291 | ||||||||||
| Part 2 | |||||||||||||||
| Model Summary (y: crPWV_SCOR; x: Sex; w: Age): R = 0.5664; R2 = 0.3208; p = <0.0001 | |||||||||||||||
| Coeff | SE | P | 95% CI LL | 95% CI UL | |||||||||||
| Intercept | 7.3354 | 0.1244 | 0.000 | 7.0913 | 7.5796 | ||||||||||
| Sex (Female: 1; Male: 0) | 0.1806 | 0.1831 | 0.324 | −0.1789 | 0.5401 | ||||||||||
| Age (years) | 0.0615 | 0.0042 | 0.000 | 0.0532 | 0.0697 | ||||||||||
| Sex * Age | −0.0139 | 0.006 | 0.022 | −0.0257 | −0.002 | ||||||||||
| Moderator value(s) defining Johnson-Neyman significance region(s): | |||||||||||||||
| Value | % below | % above | |||||||||||||
| 28.9325 (years) | 74.3017 | 25.6983 | |||||||||||||
| Conditional effect of focal predictor at values of the moderator: | |||||||||||||||
| Age (years) | Effect | SE | P | 95% CI LL | 95% CI UL | ||||||||||
| 5.20 | 0.1085 | 0.159 | 0.496 | −0.2038 | 0.4207 | ||||||||||
| 9.15 | 0.0536 | 0.1427 | 0.707 | −0.2265 | 0.3337 | ||||||||||
| 13.10 | −0.0012 | 0.1286 | 0.993 | −0.2537 | 0.2513 | ||||||||||
| 17.05 | −0.056 | 0.1178 | 0.634 | −0.2872 | 0.1752 | ||||||||||
| 21.00 | −0.1109 | 0.111 | 0.319 | −0.3289 | 0.1072 | ||||||||||
| 24.95 | −0.1657 | 0.1092 | 0.130 | −0.3801 | 0.0487 | ||||||||||
| 28.90 | −0.2205 | 0.1125 | 0.050 | −0.4414 | 0.0004 | ||||||||||
| 28.93 | −0.221 | 0.1125 | 0.050 | −0.4419 | 0 | ||||||||||
| 32.85 | −0.2753 | 0.1205 | 0.023 | −0.5119 | −0.0388 | ||||||||||
| 36.80 | −0.3302 | 0.1324 | 0.013 | −0.59 | −0.0703 | ||||||||||
| 40.75 | −0.385 | 0.1471 | 0.009 | −0.6739 | −0.0961 | ||||||||||
| 44.70 | −0.4398 | 0.1641 | 0.008 | −0.7619 | −0.1177 | ||||||||||
| 48.65 | −0.4946 | 0.1825 | 0.007 | −0.853 | −0.1363 | ||||||||||
| 52.60 | −0.5495 | 0.2021 | 0.007 | −0.9463 | −0.1526 | ||||||||||
| 56.55 | −0.6043 | 0.2225 | 0.007 | −1.0412 | −0.1674 | ||||||||||
| 60.50 | −0.6591 | 0.2436 | 0.007 | −1.1373 | −0.1809 | ||||||||||
| 64.45 | −0.714 | 0.2651 | 0.007 | −1.2344 | −0.1935 | ||||||||||
| 68.40 | −0.7688 | 0.2869 | 0.008 | −1.3322 | −0.2054 | ||||||||||
| 72.35 | −0.8236 | 0.3091 | 0.008 | −1.4305 | −0.2167 | ||||||||||
| 76.30 | −0.8784 | 0.3315 | 0.008 | −1.5293 | −0.2276 | ||||||||||
| 80.25 | −0.9333 | 0.3541 | 0.009 | −1.6284 | −0.2381 | ||||||||||
| 84.20 | −0.9881 | 0.3768 | 0.009 | −1.7279 | −0.2483 | ||||||||||
| Part 3 | |||||||||||||||
| Model Summary (y: aoPWV_Radial_SCOR; x: Sex; w: Age): R = 0.5356; R2 = 0.2869; p = <0.0001 | |||||||||||||||
| Coeff | SE | p | 95% CI LL | 95% CI UL | |||||||||||
| Intercept | 5.7863 | 0.0808 | 0.000 | 5.6277 | 5.945 | ||||||||||
| Sex (Female: 1; Male: 0) | 0.2259 | 0.1176 | 0.055 | −0.0049 | 0.4567 | ||||||||||
| Age (years) | 0.0362 | 0.0026 | <0.0001 | 0.0311 | 0.0412 | ||||||||||
| Sex * Age | −0.0059 | 0.0038 | 0.121 | −0.0134 | 0.0016 | ||||||||||
| aoPWV_Carotid_SCOR (m/s) | |||||||||||||||
| Model Summary (y: aoPWV_Carotid_SCOR; x: Sex; w: Age): R = 0.2791; R2 = 0.0779; p = <0.0001 | |||||||||||||||
| Coeff | SE | p | 95% CI LL | 95% CI UL | |||||||||||
| Intercept | 6.3469 | 0.0937 | 0.000 | 6.1629 | 6.5308 | ||||||||||
| Sex (Female: 1; Male: 0) | −0.1391 | 0.1356 | 0.306 | −0.4055 | 0.1273 | ||||||||||
| Age (years) | 0.0139 | 0.0028 | <0.0001 | 0.0085 | 0.0194 | ||||||||||
| Sex * Age | 0.0009 | 0.0041 | 0.823 | −0.0072 | 0.009 | ||||||||||
| aoPWV_Brachial_MOG (m/s)) | |||||||||||||||
| Model Summary (y: aoPWV_Brachial_MOG; x: Sex; w: Age): R = 0.8928; R2 = 0.797; p = <0.0001 | |||||||||||||||
| Coeff | SE | p | 95% CI LL | 95% CI UL | |||||||||||
| Intercept | 3.7984 | 0.042 | <0.0001 | 3.7158 | 3.8811 | ||||||||||
| Sex (Female: 1; Male: 0) | −0.262 | 0.058 | <0.0001 | −0.376 | −0.1481 | ||||||||||
| Age (years) | 0.0715 | 0.002 | <0.0001 | 0.0676 | 0.0754 | ||||||||||
| Sex * Age | 0.0034 | 0.003 | 0.2074 | −0.002 | 0.0086 | ||||||||||
CI: confidence interval. LL and UL: lower and upper limit. Coeff: coefficient. SE: standard error.
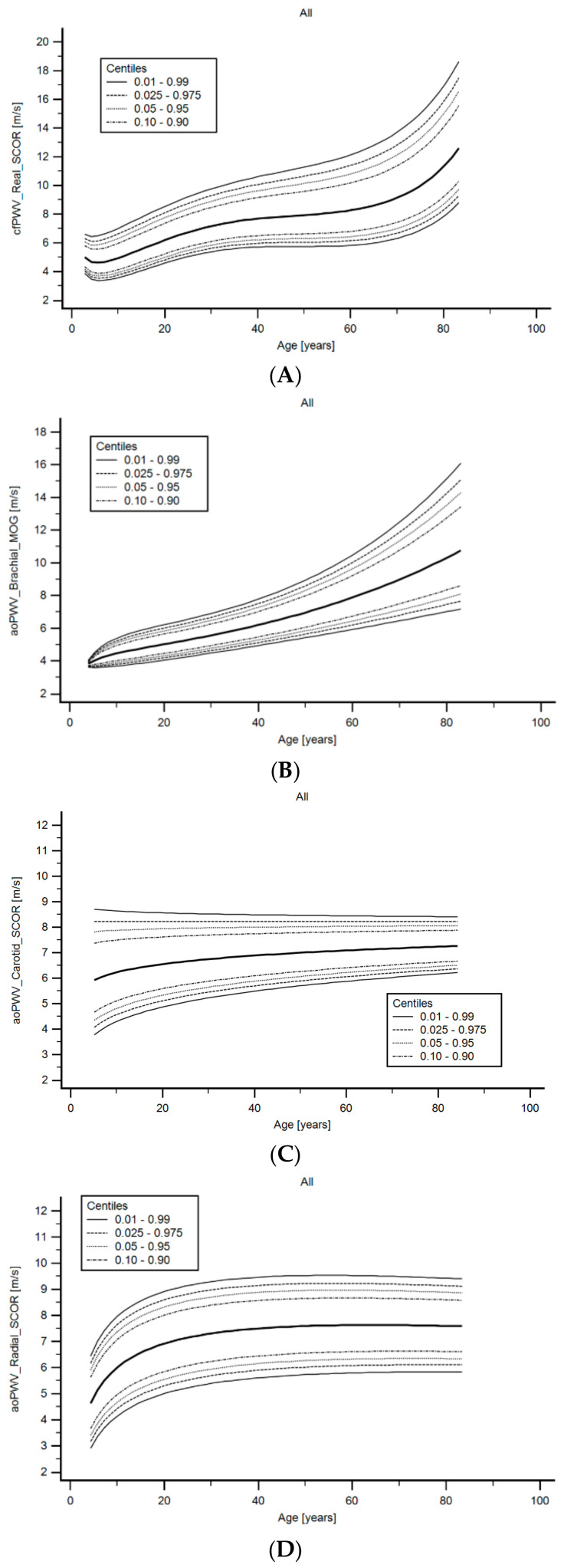
Finally, as a sixth step, age-related RIs were obtained. Age-related equations were obtained for mean values (MV) and standard deviation (SD). Then, we implemented parametric regression methods based on fractional polynomials (FPs), described by Royston and Wright [34], included in the European Reference Values for Arterial Measurements Collaboration Group methodological strategy [18,19,20,21] and already used by our group [13,35,36,37].
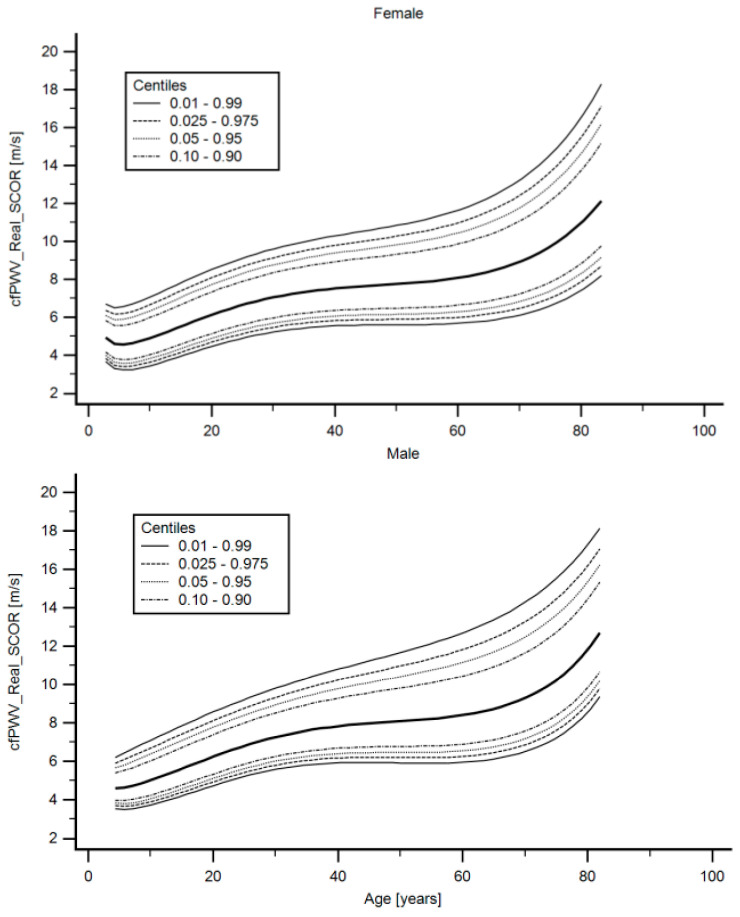
Briefly, fitting FPs age-specific MV and SD regression curves for the different variables (e.g., cfPWV_Real_SCOR) were defined using an iterative procedure (generalized least squares). Then, age-specific equations were obtained for the different parameters. For instance, the cfPWV_Real_SCOR MV equation would be cfPWV_Real_SCOR MV = a + b*Agep + c*Ageq + …, where a, b, c, … are the coefficients, and p, q, … are the powers, with numbers selected from the set [−2, −1, −0.5, 0, 0.5, 1, 2, 3] estimated from the regression for mean cfPWV_Real_SCOR curve, and likewise from the regression for SD curve. Continuing the example, FPs with powers [1,2], that is, with p = 1 and q = 2, illustrate an equation with the form a + b*age + c*age2 [34]. Residuals were used to assess the model fit, which was deemed appropriate if the scores were normally distributed, with a mean of 0 and an SD of 1, randomly scattered above and below 0 when plotted against age. Best fitted curves, considering visual and mathematical criteria (Kurtosis and Skewness coefficients) were selected. Using the equations obtained for MV and SD (Supplementary Material 1, Table S4), age-specific percentiles were defined using the standard normal distribution (Z). The 1st, 2.5th, 5th, 10th, 25th, 50th, 75th, 90th, 95th, 97.5th and 99th percentiles were calculated, for example for cfPWV_Real_SCOR: mean cfPWV_Real_SCOR + Zp*SD, where Zp assumed the values −2.3263, −1.9599, −1.6448, −1.2815, −0.6755, 0, 0.6755, 1.2815, 1.6448, 1.9599 and 2.3263, respectively (Table 8, Table 9, Table 10, Table 11, Table 12 and Table 13). Applying this approach, RIs were quantified for the parameters listed in Table 1. Year by year RI data can be found in Supplementary Material 1 (Tables S5–S58). Supplementary Material 2 shows percentile curves (for all subjects, females and males) corresponding to the different stiffness parameters studied. Figure 4 illustratesthe age-related profiles obtained for cfPWV_Real_SCOR. Similar data were obtained for the remaining parameters (Supplementary Material 2).
Table 8.
cfPWV _Real_SCOR levels and related parameters (CAVI and CAVIo) reference intervals: All.
| cfPWV_Real_SCOR (m/s) | CAVI_cfPWV_Real_SCOR | CAVIo_cfPWV_Real_SCOR | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 4.6 | 5.1 | 5.5 | 5.8 | 6.1 | 6.5 | 4.5 | 5.5 | 6.7 | 7.5 | 8.3 | 9.3 | 6.4 | 7.8 | 9.2 | 10.3 | 11.3 | 12.6 |
| 10 | 5.0 | 5.5 | 6.0 | 6.3 | 6.6 | 7.0 | 4.8 | 5.7 | 6.8 | 7.6 | 8.4 | 9.4 | 7.1 | 8.5 | 10.0 | 11.1 | 12.2 | 13.6 |
| 15 | 5.6 | 6.1 | 6.7 | 7.0 | 7.4 | 7.8 | 5.7 | 6.8 | 8.0 | 8.9 | 9.7 | 10.8 | 8.4 | 10.0 | 11.7 | 12.9 | 14.1 | 15.6 |
| 20 | 6.2 | 6.8 | 7.4 | 7.8 | 8.1 | 8.5 | 6.8 | 8.1 | 9.4 | 10.4 | 11.3 | 12.4 | 9.8 | 11.5 | 13.4 | 14.8 | 16.1 | 17.7 |
| 25 | 6.7 | 7.4 | 8.0 | 8.4 | 8.8 | 9.2 | 7.9 | 9.2 | 10.8 | 11.8 | 12.8 | 14.1 | 11.0 | 12.9 | 15.0 | 16.5 | 17.8 | 19.6 |
| 30 | 7.2 | 7.8 | 8.5 | 8.9 | 9.3 | 9.8 | 8.7 | 10.3 | 11.9 | 13.0 | 14.1 | 15.5 | 12.0 | 14.1 | 16.3 | 17.8 | 19.3 | 21.2 |
| 35 | 7.5 | 8.2 | 8.9 | 9.3 | 9.7 | 10.2 | 9.4 | 11.0 | 12.8 | 14.0 | 15.2 | 16.7 | 12.7 | 14.9 | 17.3 | 18.9 | 20.5 | 22.5 |
| 40 | 7.7 | 8.4 | 9.2 | 9.6 | 10.1 | 10.6 | 9.8 | 11.6 | 13.5 | 14.8 | 16.1 | 17.8 | 13.2 | 15.5 | 18.0 | 19.8 | 21.4 | 23.6 |
| 45 | 7.8 | 8.6 | 9.4 | 9.9 | 10.4 | 11.0 | 10.2 | 12.1 | 14.1 | 15.5 | 16.9 | 18.7 | 13.6 | 16.0 | 18.7 | 20.5 | 22.3 | 24.6 |
| 50 | 7.9 | 8.8 | 9.6 | 10.2 | 10.7 | 11.3 | 10.5 | 12.5 | 14.7 | 16.2 | 17.7 | 19.7 | 13.9 | 16.5 | 19.4 | 21.4 | 23.3 | 25.8 |
| 55 | 8.1 | 9.0 | 9.8 | 10.4 | 11.0 | 11.7 | 10.8 | 13.0 | 15.4 | 17.1 | 18.8 | 20.9 | 14.4 | 17.2 | 20.4 | 22.6 | 24.7 | 27.5 |
| 60 | 8.3 | 9.2 | 10.2 | 10.8 | 11.4 | 12.2 | 11.4 | 13.8 | 16.5 | 18.4 | 20.3 | 22.7 | 15.2 | 18.4 | 21.9 | 24.4 | 26.8 | 30.0 |
| 65 | 8.6 | 9.6 | 10.7 | 11.4 | 12.0 | 12.8 | 12.4 | 15.1 | 18.2 | 20.4 | 22.6 | 25.4 | 16.6 | 20.2 | 24.3 | 27.2 | 30.1 | 33.9 |
| 70 | 9.1 | 10.3 | 11.4 | 12.1 | 12.8 | 13.7 | 14.1 | 17.3 | 21.0 | 23.7 | 26.3 | 29.8 | 19.0 | 23.3 | 28.3 | 31.8 | 35.4 | 40.1 |
| 75 | 10.0 | 11.2 | 12.5 | 13.3 | 14.1 | 15.1 | 17.0 | 21.0 | 25.7 | 29.1 | 32.5 | 36.9 | 23.0 | 28.6 | 34.9 | 39.6 | 44.2 | 50.4 |
| 80 | 11.3 | 12.7 | 14.1 | 15.0 | 15.9 | 17.0 | 22.0 | 27.6 | 33.9 | 38.6 | 43.2 | 49.4 | 30.2 | 37.8 | 46.7 | 53.2 | 59.7 | 68.5 |
Table 9.
crPWV_SCOR levels and related parameters (CAVI and CAVIo) reference intervals: All.
| crPWV_SCOR (m/s) | CAVI_crPWV_SCOR | CAVIo_crPWV_SCOR | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 7.0 | 7.9 | 8.9 | 9.5 | 10.0 | 10.7 | 10.5 | 13.4 | 16.5 | 18.7 | 20.7 | 23.2 | 14.4 | 18.1 | 22.1 | 24.7 | 27.2 | 30.3 |
| 10 | 7.7 | 8.6 | 9.5 | 10.0 | 10.5 | 11.2 | 11.6 | 14.4 | 17.4 | 19.3 | 21.2 | 23.5 | 16.4 | 20.2 | 24.0 | 26.6 | 29.0 | 32.0 |
| 15 | 8.2 | 9.1 | 10.0 | 10.5 | 11.0 | 11.6 | 12.6 | 15.4 | 18.3 | 20.2 | 22.0 | 24.2 | 17.8 | 21.6 | 25.5 | 28.0 | 30.4 | 33.3 |
| 20 | 8.6 | 9.5 | 10.4 | 10.9 | 11.4 | 12.0 | 13.4 | 16.2 | 19.1 | 21.1 | 22.8 | 25.1 | 19.0 | 22.8 | 26.6 | 29.2 | 31.6 | 34.5 |
| 25 | 8.9 | 9.8 | 10.7 | 11.3 | 11.8 | 12.4 | 14.1 | 17.0 | 20.0 | 21.9 | 23.7 | 26.0 | 19.9 | 23.7 | 27.7 | 30.2 | 32.6 | 35.6 |
| 30 | 9.2 | 10.2 | 11.1 | 11.6 | 12.2 | 12.8 | 14.9 | 17.8 | 20.8 | 22.8 | 24.6 | 26.9 | 20.7 | 24.6 | 28.6 | 31.2 | 33.6 | 36.5 |
| 35 | 9.5 | 10.5 | 11.4 | 12.0 | 12.5 | 13.1 | 15.5 | 18.6 | 21.6 | 23.7 | 25.5 | 27.9 | 21.5 | 25.4 | 29.4 | 32.1 | 34.5 | 37.5 |
| 40 | 9.7 | 10.7 | 11.7 | 12.3 | 12.8 | 13.5 | 16.2 | 19.3 | 22.4 | 24.5 | 26.4 | 28.8 | 22.2 | 26.2 | 30.2 | 32.9 | 35.3 | 38.3 |
| 45 | 10.0 | 11.0 | 12.0 | 12.6 | 13.1 | 13.8 | 16.8 | 20.0 | 23.2 | 25.4 | 27.3 | 29.7 | 22.8 | 26.9 | 31.0 | 33.7 | 36.1 | 39.2 |
| 50 | 10.2 | 11.2 | 12.3 | 12.9 | 13.5 | 14.1 | 17.4 | 20.7 | 24.0 | 26.2 | 28.2 | 30.7 | 23.4 | 27.5 | 31.7 | 34.4 | 36.9 | 40.0 |
| 55 | 10.4 | 11.5 | 12.5 | 13.2 | 13.8 | 14.5 | 18.0 | 21.4 | 24.8 | 27.0 | 29.1 | 31.7 | 23.9 | 28.1 | 32.4 | 35.1 | 37.7 | 40.8 |
| 60 | 10.6 | 11.7 | 12.8 | 13.4 | 14.1 | 14.8 | 18.6 | 22.1 | 25.6 | 27.9 | 30.0 | 32.6 | 24.5 | 28.7 | 33.0 | 35.8 | 38.4 | 41.6 |
| 65 | 10.8 | 11.9 | 13.0 | 13.7 | 14.3 | 15.1 | 19.2 | 22.7 | 26.3 | 28.7 | 30.9 | 33.6 | 25.0 | 29.3 | 33.7 | 36.5 | 39.1 | 42.3 |
| 70 | 11.0 | 12.1 | 13.3 | 14.0 | 14.6 | 15.4 | 19.7 | 23.4 | 27.1 | 29.5 | 31.7 | 34.5 | 25.5 | 29.8 | 34.3 | 37.1 | 39.8 | 43.0 |
| 75 | 11.1 | 12.3 | 13.5 | 14.2 | 14.9 | 15.7 | 20.3 | 24.0 | 27.8 | 30.3 | 32.6 | 35.5 | 25.9 | 30.4 | 34.9 | 37.8 | 40.4 | 43.7 |
| 80 | 11.3 | 12.5 | 13.7 | 14.5 | 15.2 | 16.0 | 20.8 | 24.7 | 28.6 | 31.1 | 33.5 | 36.4 | 26.4 | 30.9 | 35.4 | 38.4 | 41.1 | 44.4 |
Table 10.
aoPWV_Radial_SCOR levels and related parameters (CAVI and CAVIo) reference intervals: All.
| aoPWV_Radial_SCOR (m/s) | CAVI_aoPWV_Radial_SCOR | CAVIo_aoPWV_Radial_SCOR | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 4.9 | 5.4 | 5.9 | 6.2 | 6.5 | 6.8 | 5.1 | 6.2 | 7.3 | 8.0 | 8.7 | 9.6 | 7.4 | 8.9 | 10.5 | 11.6 | 12.6 | 13.9 |
| 10 | 6.0 | 6.6 | 7.1 | 7.4 | 7.7 | 8.0 | 6.9 | 8.2 | 9.6 | 10.5 | 11.3 | 12.4 | 10.0 | 12.0 | 14.1 | 15.5 | 16.8 | 18.4 |
| 15 | 6.6 | 7.1 | 7.7 | 8.0 | 8.2 | 8.6 | 8.0 | 9.4 | 10.9 | 11.9 | 12.8 | 13.9 | 11.4 | 13.7 | 16.0 | 17.6 | 19.0 | 20.9 |
| 20 | 6.9 | 7.5 | 8.0 | 8.3 | 8.6 | 8.9 | 8.6 | 10.1 | 11.7 | 12.7 | 13.7 | 14.9 | 12.3 | 14.6 | 17.1 | 18.8 | 20.3 | 22.2 |
| 25 | 7.2 | 7.7 | 8.2 | 8.6 | 8.8 | 9.1 | 9.0 | 10.6 | 12.2 | 13.3 | 14.3 | 15.5 | 12.8 | 15.2 | 17.7 | 19.4 | 21.0 | 23.0 |
| 30 | 7.3 | 7.9 | 8.4 | 8.7 | 9.0 | 9.3 | 9.3 | 10.9 | 12.6 | 13.7 | 14.7 | 15.9 | 13.1 | 15.5 | 18.1 | 19.8 | 21.4 | 23.4 |
| 35 | 7.4 | 8.0 | 8.5 | 8.8 | 9.1 | 9.4 | 9.5 | 11.1 | 12.8 | 13.9 | 14.9 | 16.2 | 13.2 | 15.7 | 18.2 | 19.9 | 21.5 | 23.5 |
| 40 | 7.5 | 8.1 | 8.6 | 8.9 | 9.2 | 9.5 | 9.6 | 11.2 | 12.9 | 14.0 | 15.0 | 16.3 | 13.3 | 15.7 | 18.2 | 19.9 | 21.5 | 23.5 |
| 45 | 7.6 | 8.1 | 8.6 | 8.9 | 9.2 | 9.5 | 9.6 | 11.3 | 13.0 | 14.1 | 15.1 | 16.4 | 13.2 | 15.6 | 18.2 | 19.8 | 21.4 | 23.3 |
| 50 | 7.6 | 8.1 | 8.7 | 9.0 | 9.2 | 9.5 | 9.6 | 11.3 | 13.0 | 14.1 | 15.1 | 16.4 | 13.1 | 15.5 | 18.0 | 19.6 | 21.2 | 23.1 |
| 55 | 7.6 | 8.2 | 8.7 | 9.0 | 9.2 | 9.5 | 9.6 | 11.3 | 13.0 | 14.1 | 15.1 | 16.4 | 13.0 | 15.3 | 17.8 | 19.4 | 20.9 | 22.7 |
| 60 | 7.6 | 8.2 | 8.7 | 9.0 | 9.2 | 9.5 | 9.6 | 11.2 | 12.9 | 14.0 | 15.0 | 16.3 | 12.8 | 15.1 | 17.5 | 19.1 | 20.5 | 22.4 |
| 65 | 7.6 | 8.2 | 8.7 | 9.0 | 9.2 | 9.5 | 9.5 | 11.2 | 12.8 | 13.9 | 15.0 | 16.2 | 12.7 | 14.9 | 17.2 | 18.8 | 20.2 | 22.0 |
| 70 | 7.6 | 8.2 | 8.6 | 8.9 | 9.2 | 9.5 | 9.4 | 11.1 | 12.7 | 13.8 | 14.9 | 16.1 | 12.5 | 14.7 | 16.9 | 18.4 | 19.8 | 21.5 |
| 75 | 7.6 | 8.1 | 8.6 | 8.9 | 9.2 | 9.5 | 9.3 | 11.0 | 12.6 | 13.7 | 14.7 | 16.0 | 12.2 | 14.4 | 16.6 | 18.1 | 19.4 | 21.1 |
| 80 | 7.6 | 8.1 | 8.6 | 8.9 | 9.1 | 9.4 | 9.2 | 10.9 | 12.5 | 13.6 | 14.6 | 15.8 | 12.0 | 14.1 | 16.3 | 17.7 | 19.0 | 20.7 |
Table 11.
aoPWV_Carotid_SCOR levels and related parameters (CAVI and CAVIo) reference intervals: All.
| aoPWV_Carotid_SCOR (m/s) | CAVI_aoPWV_Carotid_SCOR | CAVIo_aoPWV_Carotid_SCOR | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 5.9 | 6.7 | 7.4 | 7.8 | 8.2 | 8.7 | 7.0 | 8.8 | 11.0 | 12.5 | 14.1 | 16.2 | 10.5 | 13.3 | 16.4 | 18.6 | 20.7 | 23.5 |
| 10 | 6.2 | 6.9 | 7.5 | 7.9 | 8.2 | 8.6 | 7.3 | 8.9 | 10.7 | 12.0 | 13.2 | 14.9 | 10.7 | 13.1 | 15.7 | 17.4 | 19.2 | 21.4 |
| 15 | 6.4 | 7.0 | 7.6 | 7.9 | 8.2 | 8.6 | 7.5 | 9.0 | 10.6 | 11.7 | 12.8 | 14.1 | 10.8 | 12.9 | 15.3 | 16.8 | 18.3 | 20.2 |
| 20 | 6.6 | 7.1 | 7.6 | 7.9 | 8.2 | 8.6 | 7.7 | 9.0 | 10.5 | 11.5 | 12.4 | 13.7 | 10.9 | 12.9 | 15.0 | 16.4 | 17.7 | 19.4 |
| 25 | 6.7 | 7.2 | 7.7 | 8.0 | 8.2 | 8.5 | 7.8 | 9.0 | 10.4 | 11.3 | 12.2 | 13.3 | 10.9 | 12.8 | 14.8 | 16.1 | 17.3 | 18.8 |
| 30 | 6.7 | 7.2 | 7.7 | 8.0 | 8.2 | 8.5 | 7.9 | 9.1 | 10.3 | 11.2 | 12.0 | 13.0 | 11.0 | 12.8 | 14.6 | 15.8 | 16.9 | 18.4 |
| 35 | 6.8 | 7.3 | 7.7 | 8.0 | 8.2 | 8.5 | 7.9 | 9.1 | 10.3 | 11.1 | 11.8 | 12.8 | 11.0 | 12.7 | 14.4 | 15.6 | 16.6 | 18.0 |
| 40 | 6.9 | 7.3 | 7.7 | 8.0 | 8.2 | 8.5 | 8.0 | 9.1 | 10.2 | 11.0 | 11.7 | 12.6 | 11.1 | 12.7 | 14.3 | 15.4 | 16.4 | 17.6 |
| 45 | 6.9 | 7.4 | 7.8 | 8.0 | 8.2 | 8.5 | 8.1 | 9.1 | 10.2 | 10.9 | 11.6 | 12.4 | 11.1 | 12.6 | 14.2 | 15.2 | 16.2 | 17.4 |
| 50 | 7.0 | 7.4 | 7.8 | 8.0 | 8.2 | 8.5 | 8.1 | 9.1 | 10.2 | 10.8 | 11.5 | 12.2 | 11.1 | 12.6 | 14.1 | 15.1 | 16.0 | 17.1 |
| 55 | 7.0 | 7.4 | 7.8 | 8.0 | 8.2 | 8.5 | 8.2 | 9.1 | 10.1 | 10.8 | 11.4 | 12.1 | 11.2 | 12.6 | 14.0 | 15.0 | 15.8 | 16.9 |
| 60 | 7.1 | 7.5 | 7.8 | 8.0 | 8.2 | 8.4 | 8.2 | 9.2 | 10.1 | 10.7 | 11.3 | 12.0 | 11.2 | 12.6 | 13.9 | 14.8 | 15.7 | 16.7 |
| 65 | 7.1 | 7.5 | 7.8 | 8.0 | 8.2 | 8.4 | 8.3 | 9.2 | 10.1 | 10.7 | 11.2 | 11.8 | 11.2 | 12.5 | 13.9 | 14.7 | 15.5 | 16.5 |
| 70 | 7.2 | 7.5 | 7.8 | 8.0 | 8.2 | 8.4 | 8.3 | 9.2 | 10.0 | 10.6 | 11.1 | 11.7 | 11.2 | 12.5 | 13.8 | 14.6 | 15.4 | 16.3 |
| 75 | 7.2 | 7.5 | 7.9 | 8.1 | 8.2 | 8.4 | 8.4 | 9.2 | 10.0 | 10.6 | 11.0 | 11.6 | 11.3 | 12.5 | 13.7 | 14.5 | 15.3 | 16.2 |
| 80 | 7.2 | 7.6 | 7.9 | 8.1 | 8.2 | 8.4 | 8.4 | 9.2 | 10.0 | 10.5 | 11.0 | 11.6 | 11.3 | 12.5 | 13.7 | 14.5 | 15.2 | 16.0 |
Table 12.
aoPWV_Brachial_MOG levels and related parameters (CAVI and CAVIo) reference intervals: All.
| aoPWV_Brachial_MOG (m/s) | CAVI_aoPWV_Brachial_MOG | CAVIo_aoPWV_Brachial_MOG | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 4.0 | 4.1 | 4.2 | 4.3 | 4.4 | 4.5 | 3.3 | 3.5 | 3.6 | 3.7 | 3.8 | 3.9 | 4.9 | 5.3 | 5.7 | 5.9 | 6.2 | 6.4 |
| 10 | 4.5 | 4.7 | 5.0 | 5.1 | 5.3 | 5.4 | 3.7 | 4.1 | 4.4 | 4.6 | 4.8 | 5.1 | 5.5 | 6.2 | 6.8 | 7.3 | 7.6 | 8.1 |
| 15 | 4.8 | 5.1 | 5.4 | 5.5 | 5.7 | 5.9 | 4.1 | 4.6 | 5.1 | 5.4 | 5.7 | 6.0 | 6.0 | 6.8 | 7.7 | 8.3 | 8.8 | 9.5 |
| 20 | 5.0 | 5.4 | 5.7 | 5.8 | 6.0 | 6.2 | 4.5 | 5.1 | 5.7 | 6.0 | 6.4 | 6.8 | 6.4 | 7.4 | 8.5 | 9.2 | 9.8 | 10.6 |
| 25 | 5.3 | 5.6 | 6.0 | 6.2 | 6.3 | 6.6 | 4.9 | 5.5 | 6.2 | 6.6 | 7.1 | 7.6 | 6.8 | 8.0 | 9.1 | 9.9 | 10.6 | 11.5 |
| 30 | 5.6 | 5.9 | 6.3 | 6.5 | 6.7 | 6.9 | 5.3 | 6.0 | 6.7 | 7.2 | 7.7 | 8.2 | 7.3 | 8.5 | 9.7 | 10.6 | 11.4 | 12.3 |
| 35 | 5.9 | 6.3 | 6.6 | 6.9 | 7.1 | 7.3 | 5.7 | 6.5 | 7.3 | 7.8 | 8.3 | 8.9 | 7.8 | 9.1 | 10.4 | 11.3 | 12.1 | 13.1 |
| 40 | 6.2 | 6.6 | 7.0 | 7.3 | 7.5 | 7.8 | 6.3 | 7.1 | 8.0 | 8.5 | 9.1 | 9.7 | 8.4 | 9.7 | 11.1 | 12.0 | 12.9 | 13.9 |
| 45 | 6.6 | 7.0 | 7.5 | 7.8 | 8.0 | 8.3 | 6.9 | 7.8 | 8.8 | 9.4 | 10.0 | 10.7 | 9.2 | 10.6 | 12.0 | 12.9 | 13.8 | 14.9 |
| 50 | 7.0 | 7.5 | 8.0 | 8.3 | 8.6 | 9.0 | 7.8 | 8.8 | 9.8 | 10.5 | 11.1 | 11.9 | 10.2 | 11.6 | 13.1 | 14.1 | 15.0 | 16.1 |
| 55 | 7.4 | 8.0 | 8.6 | 8.9 | 9.3 | 9.7 | 8.8 | 10.0 | 11.2 | 11.9 | 12.6 | 13.5 | 11.5 | 13.0 | 14.6 | 15.6 | 16.5 | 17.7 |
| 60 | 7.9 | 8.6 | 9.2 | 9.7 | 10.0 | 10.5 | 10.3 | 11.6 | 13.0 | 13.9 | 14.7 | 15.8 | 13.3 | 14.9 | 16.6 | 17.7 | 18.7 | 20.0 |
| 65 | 8.4 | 9.2 | 10.0 | 10.5 | 10.9 | 11.4 | 12.2 | 13.9 | 15.6 | 16.7 | 17.8 | 19.1 | 15.7 | 17.6 | 19.4 | 20.7 | 21.8 | 23.2 |
| 70 | 9.0 | 9.9 | 10.8 | 11.4 | 11.9 | 12.5 | 14.8 | 17.0 | 19.2 | 20.8 | 22.2 | 23.9 | 19.0 | 21.3 | 23.5 | 24.9 | 26.2 | 27.9 |
| 75 | 9.6 | 10.7 | 11.7 | 12.4 | 13.0 | 13.8 | 18.4 | 21.4 | 24.6 | 26.8 | 28.8 | 31.3 | 23.9 | 26.6 | 29.4 | 31.2 | 32.9 | 34.9 |
| 80 | 10.3 | 11.5 | 12.8 | 13.6 | 14.3 | 15.2 | 23.5 | 28.0 | 32.8 | 36.1 | 39.2 | 43.2 | 30.9 | 34.6 | 38.3 | 40.7 | 43.0 | 45.7 |
Table 13.
PWV Ratio levels and related parameters (CAVI and CAVIo) reference intervals: All.
| PWV_Ratio | CAVI_PWV_Ratio | CAVIo_PWV_Ratio | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th | 50th | 75th | 90th | 95th | 97.5th | 99th |
| 5 | 0.58 | 0.67 | 0.76 | 0.82 | 0.88 | 0.95 | 0.33 | 0.44 | 0.57 | 0.67 | 0.76 | 0.89 | 0.35 | 0.46 | 0.59 | 0.68 | 0.78 | 0.90 |
| 10 | 0.64 | 0.73 | 0.82 | 0.87 | 0.93 | 0.99 | 0.41 | 0.53 | 0.66 | 0.76 | 0.85 | 0.98 | 0.43 | 0.54 | 0.68 | 0.77 | 0.87 | 0.99 |
| 15 | 0.69 | 0.77 | 0.85 | 0.90 | 0.95 | 1.01 | 0.47 | 0.59 | 0.72 | 0.82 | 0.91 | 1.03 | 0.48 | 0.60 | 0.74 | 0.83 | 0.92 | 1.04 |
| 20 | 0.71 | 0.79 | 0.87 | 0.92 | 0.97 | 1.03 | 0.51 | 0.63 | 0.76 | 0.86 | 0.95 | 1.06 | 0.52 | 0.64 | 0.77 | 0.86 | 0.95 | 1.07 |
| 25 | 0.73 | 0.81 | 0.89 | 0.93 | 0.98 | 1.03 | 0.53 | 0.66 | 0.79 | 0.88 | 0.97 | 1.08 | 0.54 | 0.66 | 0.80 | 0.89 | 0.97 | 1.08 |
| 30 | 0.74 | 0.82 | 0.89 | 0.94 | 0.98 | 1.04 | 0.55 | 0.67 | 0.80 | 0.89 | 0.98 | 1.09 | 0.56 | 0.68 | 0.81 | 0.90 | 0.98 | 1.09 |
| 35 | 0.75 | 0.82 | 0.90 | 0.95 | 0.99 | 1.04 | 0.56 | 0.68 | 0.81 | 0.90 | 0.99 | 1.10 | 0.57 | 0.69 | 0.82 | 0.91 | 0.99 | 1.10 |
| 40 | 0.75 | 0.83 | 0.91 | 0.95 | 1.00 | 1.05 | 0.57 | 0.69 | 0.83 | 0.92 | 1.01 | 1.12 | 0.58 | 0.70 | 0.83 | 0.92 | 1.01 | 1.12 |
| 45 | 0.76 | 0.84 | 0.92 | 0.96 | 1.01 | 1.07 | 0.58 | 0.71 | 0.84 | 0.94 | 1.03 | 1.15 | 0.59 | 0.71 | 0.85 | 0.95 | 1.04 | 1.15 |
| 50 | 0.77 | 0.85 | 0.93 | 0.98 | 1.03 | 1.09 | 0.59 | 0.73 | 0.87 | 0.98 | 1.07 | 1.20 | 0.60 | 0.74 | 0.88 | 0.98 | 1.08 | 1.20 |
| 55 | 0.78 | 0.87 | 0.96 | 1.01 | 1.06 | 1.13 | 0.62 | 0.76 | 0.92 | 1.03 | 1.14 | 1.28 | 0.63 | 0.77 | 0.93 | 1.04 | 1.15 | 1.28 |
| 60 | 0.81 | 0.90 | 1.00 | 1.06 | 1.11 | 1.18 | 0.66 | 0.82 | 1.00 | 1.12 | 1.24 | 1.40 | 0.67 | 0.83 | 1.01 | 1.13 | 1.25 | 1.41 |
| 65 | 0.85 | 0.95 | 1.05 | 1.12 | 1.18 | 1.25 | 0.72 | 0.90 | 1.11 | 1.25 | 1.39 | 1.58 | 0.73 | 0.92 | 1.12 | 1.27 | 1.41 | 1.59 |
| 70 | 0.90 | 1.01 | 1.13 | 1.20 | 1.27 | 1.36 | 0.82 | 1.03 | 1.28 | 1.45 | 1.62 | 1.84 | 0.83 | 1.05 | 1.29 | 1.47 | 1.64 | 1.86 |
| 75 | 0.98 | 1.11 | 1.24 | 1.32 | 1.40 | 1.50 | 0.96 | 1.23 | 1.53 | 1.75 | 1.96 | 2.24 | 0.97 | 1.24 | 1.55 | 1.77 | 1.98 | 2.27 |
| 80 | 1.08 | 1.23 | 1.39 | 1.49 | 1.58 | 1.69 | 1.19 | 1.53 | 1.92 | 2.20 | 2.48 | 2.84 | 1.19 | 1.54 | 1.94 | 2.23 | 2.51 | 2.89 |
Figure 4.
cfPWV_Real_SCOR age-related percentile curves for female (top) and males (bottom). Quantitative data are shown in Table 8 and Supplementary Material 1 and 2.
The minimum sample size required was 377 [38]. Like in previous works and according to the central limit theorem, normal distribution was considered (taking into account Kurtosis and Skewness coefficients distribution and sample size > 30) [39]. Data analysis was done using MedCalc-Statistical Software (version 18.5, MedCalc Inc., Ostend, Belgium) and IBM-SPSS software (SPSS Inc., Chicago, IL, USA). PROCESS version 3.5 (SPSS extension) was used for moderation (interaction) analysis [40]. Evans’s Empirical Classifications of Interpreting Correlation Strength by Using r was applied: r < 0.20, very weak; r: 0.20–0.39, weak; r: 0.40–0.59, moderate; r: 0.60–0.79, strong; r ≥ 0.80, very strong [30,41]. p < 0.05 was considered statistically significant.
3. Results
3.1. Subjects’ Characteristics
Table 2 and Table 3 show subjects’ demographic, clinical, anthropometric and CV data. Note the wide age-range considered (in the population and the RIs group) (Table 2). As shown in Table 3, each arterial stiffness determination had a corresponding BP recording.
3.2. Association between Arterial Stiffness Parameters Obtained with Different Devices and/or Algorithms
Simple bivariate and concordance correlation data are shown in Table 4. Note the differences in Pearson coefficients (r) and CCC obtained when analyzing the cfPWV_Real_SCOR correlation with aoPWV data, obtained with other approaches (aoPWV_Radial_SCOR: r = 0.498, CCC = 0.448; aoPWV_Carotid_SCOR: r = 0.3145, CCC = 0.271 and aoPWV_Brachial_MOG: r = 0.7336, CCC = 0.614). Looking at the findings, it could be said: (i) although the positive associations were significant, they were weak or moderate, (ii) association levels varied depending on the devices and parameters compared, and (iii) statistical agreement (equivalence) levels were low (Table 4).
Likewise, regardless of whether it was considered aoPWV, CAVI or CAVIo, (i) the levels of association were always significant (except for the association between CAVI and CAVIo for aoPWV_Carotid_SCOR and aoPWV_Brachial_MOG), and (ii) in all cases, CCC showed low (or even non-existent) levels of agreement between data (Table 4). CCC values were always <0.617.
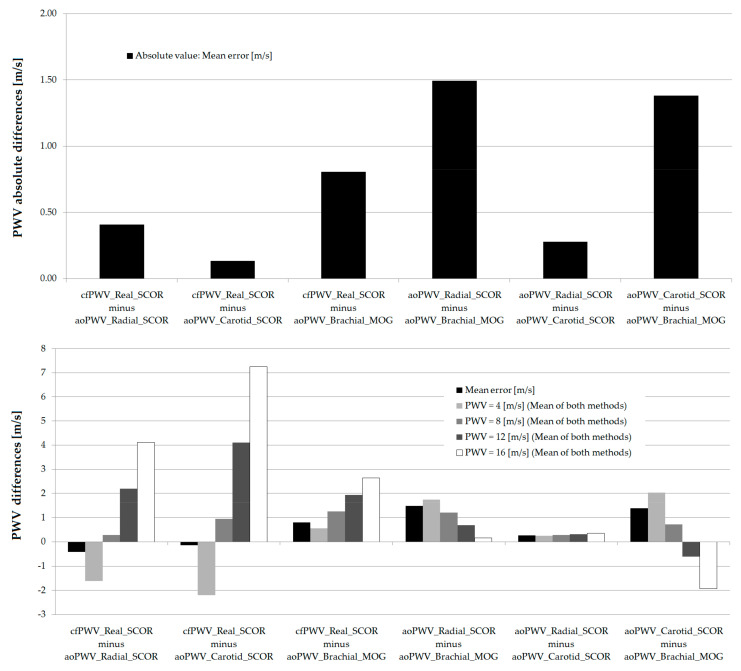
3.3. Agreement between Stiffness Parameters Obtained with Different Devices and/or Algorithms
Table 5 shows the Bland–Altman analyses carried out to determine the levels of equivalence between data obtained with different devices and/or algorithms. cfPWV_Real_SCOR and aoPWV data showed: (i) significant systematic differences (errors), whose mean values were −0.41 m/s, −0.14 m/s and 0.81 m/s, and (ii) proportional differences (errors), that is to say, differences that varied in magnitude depending on PWV values. With a negative intercept, the difference between cfPWV_Real_SCOR and any of the aoPWV indexes, had a positive slope, with the error crossing 0 at approximately 7 m/s. Thus, for low levels of stiffness, cfPWV_Real_SCOR showed lower values than aoPWV. As stiffness levels increased, the differences decreased, until the ratio was reversed and cfPWV_Real_SCOR reached higher values than aoPWV (Table 5). Likewise, methods used to quantify aoPWV showed significant systematic (mean: 0.28 m/s, 1.49 m/s and 1.38 m/s) and proportional errors (except aoPWV_Radial_SCOR and aoPWV_Carotid_SCOR) (Table 5).
CAVI data showed significant systematic differences. On the other hand, with the exception of CAVI_aoPWV_Radial_SCOR and CAVI_aoPWV_Carotid_SCOR, they also showed proportional differences. In turn, CAVIo data showed both, systematic and proportional errors (Table 5).
Jointly analyzing the findings, it could be said that the methods used to assess PWV, CAVI or CAVIo were not equivalent.
3.4. Arterial Stiffness and Atherosclerotic Plaques in Asymptomatic Subjects
There was no association between arterial stiffness (cfPWV, crPWV and aoPWV) and atherosclerotic plaque presence (Pearson coefficients ≤ 0.1, not significant) (Table 6).
3.5. Arterial Stiffness and Sex Differences
Table 6 shows that in a first analysis (simple bivariate associations), without taking into account adjustments and/or interactions with age, sex showed a slight negative association with cfPWV_Real_SCOR and aoPWV_Brachial_MOG (lower stiffness levels in females).
However, when age and sex interaction was considered, there were: (i) parameters that required sex-specific RIs from certain ages (cfPWV_Real_SCOR and crPWV_SCOR), (ii) parameters for which sex-specific RIs were necessary in all ages (aoPWV_Brachial_MOG) and (iii) parameters that did not require sex-specific RIs (aoPWV_Radial_SCOR and aoPWV_Carotid_SCOR) (Table 7, Part 1).
Females and males <19.67 y did not show significant differences in cfPWV_Real_SCOR (p > 0.05), while for older ages, cfPWV was gradually higher in males. About this: (i) at the age of ~23 y (23.15 y), cfPWV values in males were 0.1373 m/s higher than in females, (ii) at ~40 y (39.43 y), the difference was 0.2789 m/s, (iii) at the age of ~60 y (59.78 y), male values were 0.456 m/s higher than those in females whereas (iv) at ~80 y (80.13 y), the difference was 0.633 m/s. Similarly, from 29 years of age (28.9 y), the crPWV_SCOR levels were gradually higher in males than in females (0.220 m/s, 0.385 m/s, 0.659 m/s and 0.933 m/s at 28.9 y, 40.75 y, 60.50 y and 80.25 y, respectively) (Table 7, Part 2). On the other hand, aoPWV_Brachial_MOG was associated with sex, with the independence of age, whereas aoPWV_Radial_SCOR and aoPWV_Carotid_SCOR did not show an association with sex, nor an interaction between age and sex (Table 7, Part 3). In all cases, however, we decided to define RIs for all the subjects, as well as for females and males separately.
3.6. Age- and Sex-Related Reference Intervals
Table 8, Table 9, Table 10, Table 11, Table 12 and Table 13 show a summary (5 y intervals) of the reference values (p50th, p75th, p90th, p95th, p97.5th, p99th) for each stiffness parameter (its CAVI and CAVIo). Data for year-by-year intervals can be seen in Supplementary Material 1 (Tables S5–S58).
4. Discussion
4.1. Main Findings
The work’s main findings can be summarized as follows:
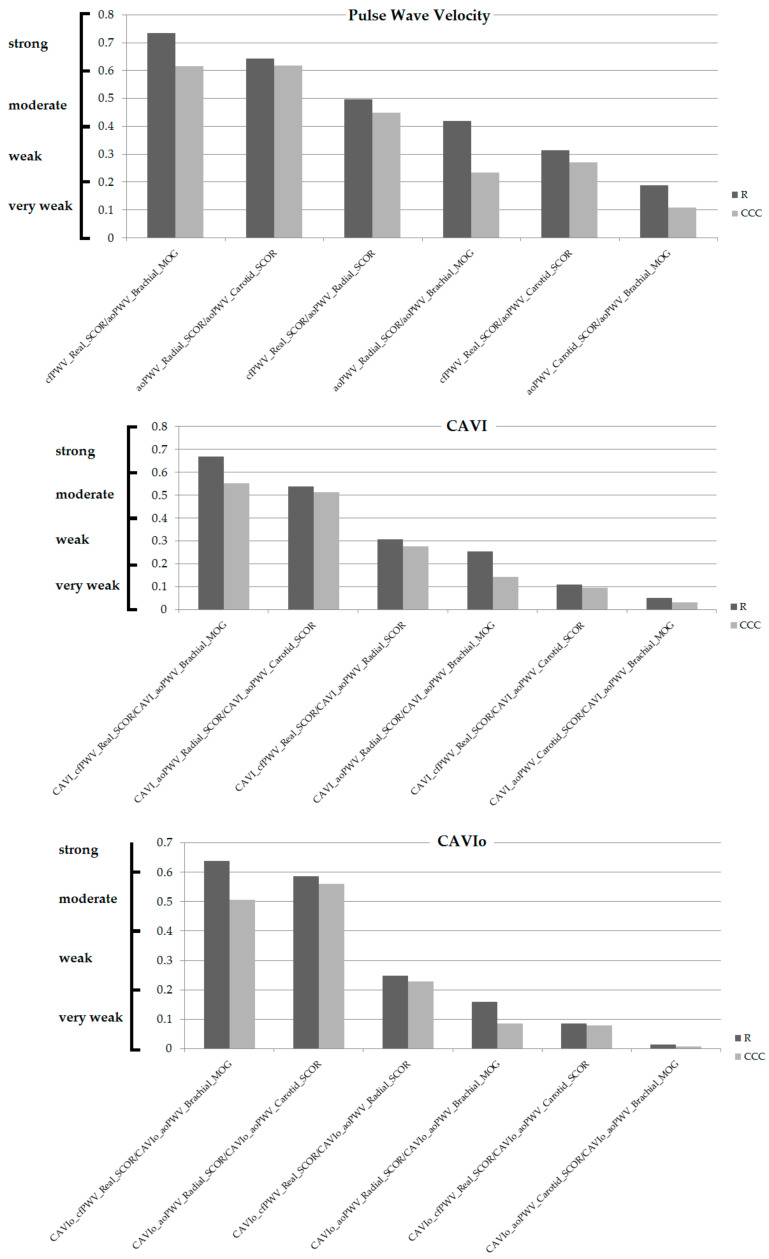
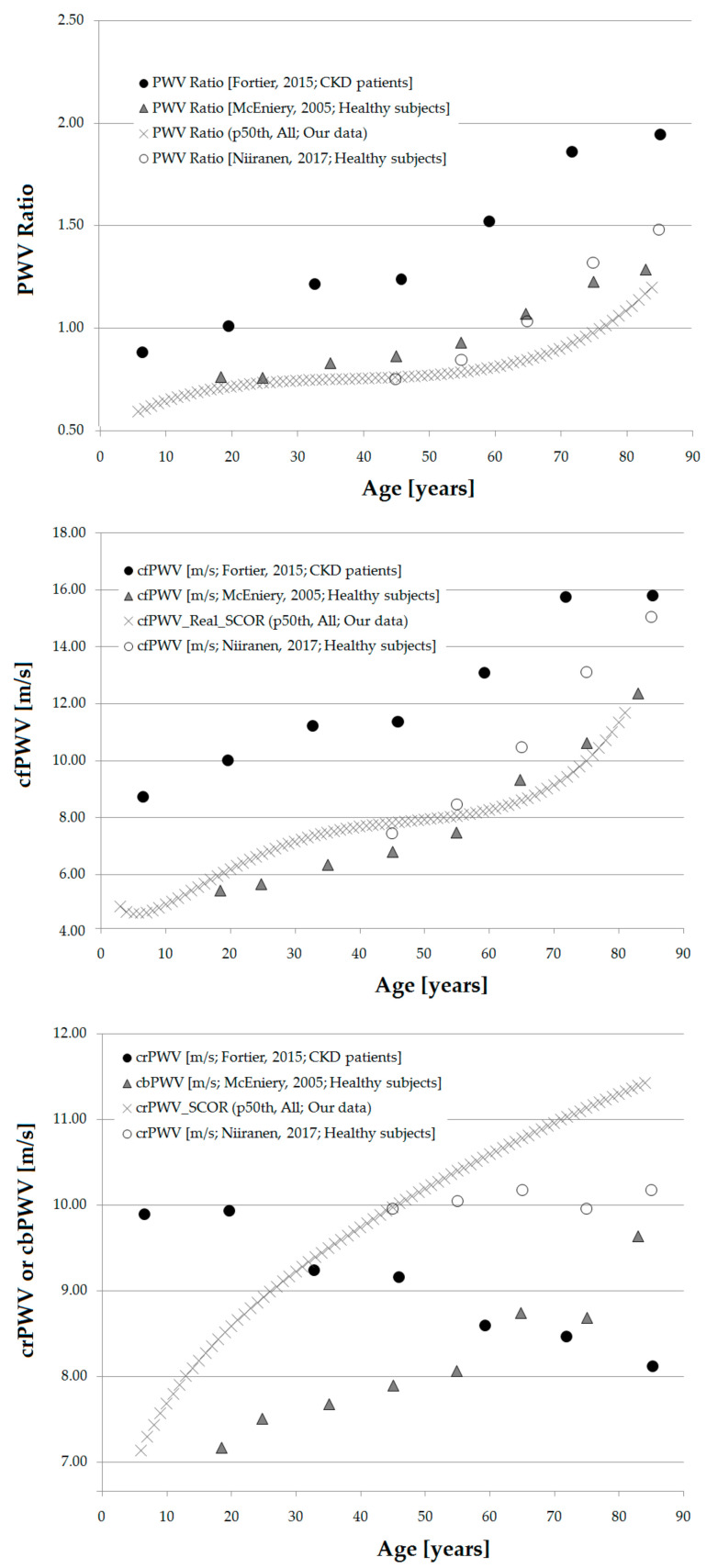
First, for methods and parameters used to assess aortic stiffness (cfPWV_Real, aoPWV_Radial, aoPWV_Carotid and aoPWV_Brachial), their CAVI and CAVIo, showed different association levels (some non-significant). In no case was the association very strong (r ≥ 0.80) (Table 4, Figure 5).
Figure 5.
Simple (Pearson, r) and concordance correlation coefficients (CCCs), ordered from highest to lowest based on r value, for PWV (top), CAVI (middle) and CAVIo (bottom). Evans’s Empirical Classifications of Interpreting Correlation Strength by Using r was applied: (i) very weak: <0.20; (ii) weak: 0.20–0.39, (iii) moderate: 0.40–0.59, (iv) strong: 0.60–0.79, (v) very strong: r ≥ 0.80 [41].
For PWV, CAVI and CAVIo, the highest levels of association were obtained for cfPWV_Real_SCOR and aoPWV_Brachial_MOG (r = 0.73, r = 0.67 and r = 0.64, respectively), whereas the lowest levels were obtained for aoPWV_Carotid_SCOR and aoPWV_Brachial_MOG (r = 0.19, r = 0.05 and r = 0.01, respectively). Regardless of whether or not there was agreement (equivalence) on absolute levels, there were methods with no association, so it would not be possible to arrive at similar conclusions from similar trends in their variations (Table 4, Figure 5).
Recently, Salvi et al. obtained an r = 0.64 (p < 0.0001; mean error/SD: 0.40 ± 2.23 m/s) for the association between aoPWV_Brachial_MOG and cfPWV_Real_SCOR [30]. Similarly, when aoPWV_Brachial_MOG was considered, the levels of association with propagated cfPWV data were heterogeneous and in no case achieved “very strong” values: (i) Complior System (n = 100, r = 0.46; p < 0.0001; mean error/SD: 0.28 ± 2.94 m/s); (ii) PulsePen ETT System (n = 99, r = 0.62; p < 0.0001; mean error/SD: 1.17 ± 2.59 m/s); (iii) PulsePen ET System (n = 102, r = 0.61; p < 0.0001; mean error/SD: 1.00 ± 2.77 m/s) [30]. In agreement with our findings (but working with an n = 102) the authors found differences in the associations between methods used to assess aortic stiffness (in some cases, they did not reach statistical significance). On the contrary, in the work of Salvi et al., methods that evaluated propagated PWV (e.g., SphygmoCor, Complior, PulsePen ET, PulsePen ETT) showed Pearson Coefficients > 0.8 [30].
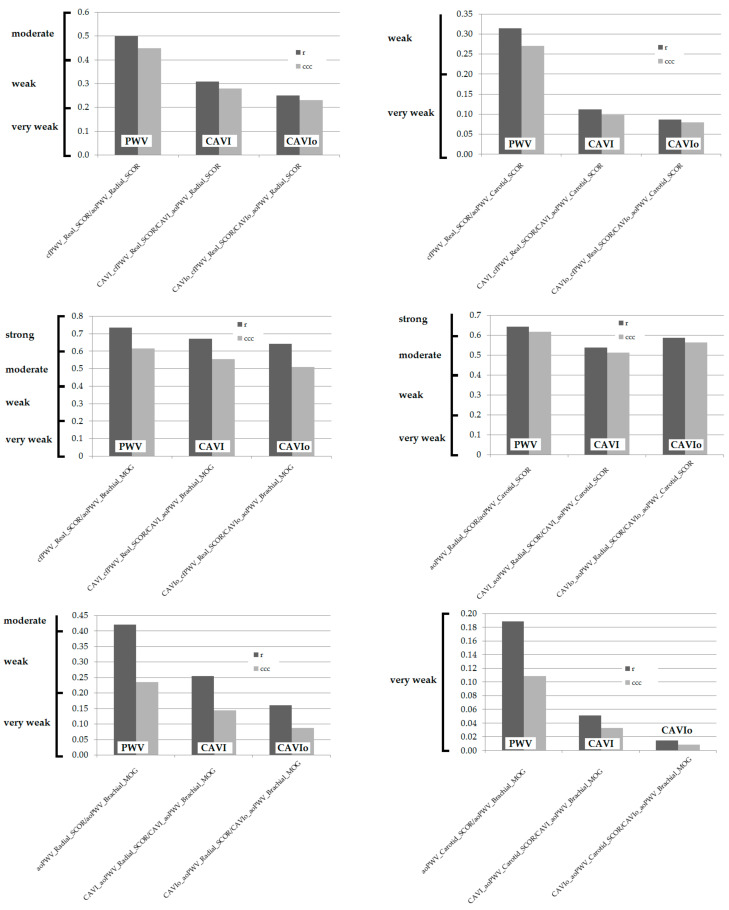
On the other hand, when BP dependence was considered (CAVI and CAVIo), there was a reduction in the levels of association (Figure 6). In all cases, there was a gradual reduction in r, from the analysis of stiffness parameters (cfPWV and/or aoPWV), their transformation into CAVI and into corrected CAVI (CAVIo). The reduction in r led to changes in the categorization of the associations (e.g., moderate for aoPWV_Radial_SCOR/aoPWV_Brachial_MOG, very weak for CAVIo_aoPWV_Radial_SCOR/CAVIo_aoPWV_Brachial_MOG) (Figure 6). Therefore, considering (becoming independent of) BP levels at the time of arterial stiffness determination, resulted in a reduction in the associations between stiffness parameters, rather than in their “strengthening” due to the elimination of a factor, potentially different and determinant of the stiffness values.
Figure 6.
Simple (Pearson, r) and concordance correlation coefficients (CCCs) for PWV, CAVI and CAVIo, ordered for “pairs” of records. Evans’s Empirical Classifications of Interpreting Correlation Strength by Using r was applied: (i) very weak: <0.20; (ii) weak: 0.20–0.39, (iii) moderate: 0.40–0.59, (iv) strong: 0.60-–0.79, (v) very strong: r ≥ 0.80 [41].
Second, approaches and parameters used to assess aortic stiffness (cfPWV_Real, aoPWV_Radial, aoPWV_Carotid and aoPWV_Brachial) were not equivalent but showed systematic and proportional errors (Table 5, Figure 7).
Figure 7.
Top: Mean error (absolute value) for PWV data from different methods (Bland–Altman analysis). Bottom: Mean error and proportional differences for PWV equal to 4, 8, 12 and 16 m/s.
Mean differences (absolute mean errors) were between 0.13 and 1.5 m/s (Table 5, Figure 7). In turn, when analyzing proportional errors: (i) three comparisons showed proportional differences, with a method always higher (or lower) than the other one, and (ii) three comparisons showed proportional differences in which the method with higher values varied depending on the stiffness level considered (Table 5, Figure 7).
Salvi et al. found a mean error equal to 0.40 ± 2.23 m/s (mean ± SD) when analyzing aoPWV_Brachial_MOG and cfPWV_Real_SCOR data. In addition, the authors found a negative proportional bias [30]. The findings agree with this work, in which a mean error equal to 0.81 m/s was observed for cfPWV_Real_SCOR and aoPWV_Brachial_MOG difference. In the work of Salvi et al., correlation (showing the equality line) and Bland–Altman graphs showed a trend that would enable the inference that as PWV increases, cfPWV_Real_SCOR would be gradually greater than aoPWV_Brachial_MOG [30]. Similarly, in this work, the differences between methods (cfPWV_Real_SCOR minus aoPWV_Brachail_MOG) increased at higher PWV values (Figure 7). For mean PWV values equal to 4, 8, 12 and 16 m/s, cfPWV_Real_SCOR was, respectively, 0.56, 1.26, 1.95 and 2.64 m/s higher than aoPWV_Brachial_MOG (Figure 7). As described in the above-mentioned work, at very low PWV values (e.g., the theoretical level close to the intercept), the relationship would be reversed. Although it is beyond this work’s scope, at least in theory the differences could be explained by the way aoPWV_Brachial_MOG is obtained. The algorithm used by the MOG device would provide PWV estimates, mainly calculated from age and bSBP data. Then, unlike propagated cfPWV measurements, aoPWV_Brachial_MOG could not show stiffness changes not explained by age and/or BP (e.g., explained by exposure to non-traditional CRFs). Related to what is stated above, Salvi et al. [30] went further and established that the Mobil-O-Graph should be considered an algorithm-based system, rather than an oscillometric cuff-based one. Indeed, they suggested the device would not provide measurements, nor estimations of aortic PWV, but would give the calculation of expected PWV values for a given age and bSBP [30]. In this context, it should be noted that in all cases, the maximum differences (absolute mean error) were found when comparing PWV data from MOG and SCOR (cfPWV_Real_SCOR, aoPWV_Radial_SCOR or aoPWV_Carotid_SCOR) (Figure 7).
PWV data showed low (the lowest) differences when aoPWV_Radial_SCOR and aoPWV_Carotid_SCOR were compared. Statistically significant mean and proportional errors were observed when they were compared to cfPWV_Real_SCOR (Table 5, Figure 7).
Third, the need for sex-specific arterial stiffness RIs relied on the approach used to assess stiffness and/or on the age considered. In this respect, according to the measurement system, sex-specific RIs were not necessary, necessary regardless of age or only needed after a certain age (Table 7).
The relationship between sex and arterial stiffening is controversial and at least two issues are still discussed: (i) whether there are sex-related differences in mean arterial stiffness as a function of age, and (ii) whether there are sex-related differences in the rate of age-associated stiffness increase. In this work, we found that both issues may be closely related. The confusion or controversy regarding them could depend on the site of recording and/or on the approach (and device) used to assess arterial stiffness.
The aoPWV_Brachial_MOG values were systematically higher in males than in females (Table 7, Part C). At least in theory (in line with the aforementioned), the algorithm used to obtain aoPWV_Brachial_MOG, in which bSBP has a significant contribution, together with the higher bSBP levels (generally) found in men, could contribute to explaining the findings. In other words, sex-related differences in stiffness could be explained by the method used to calculate aoPWV with the MOG. Related to this, aoPWV_Carotid_SCOR and aoPWV_Radial_SCOR did not show sex-related differences, although for aoPWV_Radial_SCOR they were close to the statistical significance (p = 0.055). In addition, none of the variables showed a significant interaction between age and sex. Unfortunately, the internal algorithms that allow quantifying aoPWV by means of the different approaches are unknown, which does not allow adequate analysis of factors that could explain or be associated with the findings (e.g., lack of differences).
For propagated PWV (cPWV and crPWV), there were no significant sex-related differences in childhood, but thereafter these became gradually larger (higher stiffness in males than in females). This is in agreement with previous data published by our group regarding local carotid stiffness (carotid elastic modulus) in children and adolescents [42]. The findings also agree with results (for adults) obtained in the Anglo-Cardiff Collaboration Trial cohort, in which cfPWV was on average 2% lower in women than in men, without sex-related differences in the stiffening rate [43]. In this work, sex-related differences in cfPWV were observed earlier (a decade) than in crPWV.
As was discussed the need for RIs separated by sex varied depending on the approach used to assess arterial stiffness. In all cases, we opted for defining RIs for the population as well as for males and females separately.
Fourth, this work’s main result is the definition of population-based reference values for PWV, CAVI and CAVIo indexes, obtained in the same subjects, with different non-invasive approaches. The definition of RIs is an important step when considering the introduction of PWV, CAVI and CAVIo indexes as a tool for the detection of subclinical target organ damage in the general population (Table 8, Table 9, Table 10, Table 11 and Table 12, Supplementary Material 1 (Tables S5–S55)). To our knowledge, this is the first time RIs are defined for the center-to-periphery arterial stiffness ratio (gradient) (Table 13, Supplementary Material 1 (Tables S56–S58)).
In biomechanical terms, while the impact of aortic stiffness on the myocardium is explained by increased cardiac afterload and reduced perfusion, peripheral target organ damage is best explained by the arterial stiffness gradient hypothesis [44]. As a result of the heterogeneity in vascular wall composition and geometry [45,46], arterial stiffness increases from central (e.g., ascending aorta) to peripheral (e.g., radial) arteries (center-to-periphery stiffness gradient). Central large elastic and peripheral medium-sized muscular conduit vessels, which are structurally and biomechanically different, would not be similarly affected by factors like aging, disease and drugs [47]. In this regard, the aging-related stiffness increase mainly occurs in the central elastic arteries. As the aorta stiffens, there is an attenuation and even a reversal of the stiffness gradient, resulting in a reduction in the attenuation of the forward pressure wave, and in an increased pulse pressure transmission to the microcirculation. This would lead to vascular myogenic response, endothelial dysfunction, hypoperfusion and organ damage [44,47,48]. Recent studies underlined the meaning of the stiffness gradient for both clinical conditions and outcomes [49,50,51]. It was proposed that the center-periphery PWV ratio would predict mortality better than cfPWV alone [47,48]. In this context, an issue that should be noted and addressed is the lack (so far) of: (i) data about age-related PWV ratio profiles, (ii) RIs (MV or SD equations) for PWV ratio that could, for example, allow assessing the meaning of deviations from expected levels in terms of cardiovascular status and prognosis.
In this work, RIs for stiffness parameters were obtained working with a large population of healthy subjects, selected taking into account inclusion and exclusion criteria previously used by our and other groups. Tables and Figures showing age-related (year by year) profiles for the different parameters (percentiles: 1, 2.5, 5, 25, 50, 75, 90, 95, 97.5 and 99th) are included in Supplementary Material 1 and 2.
Figure 8 shows RIs for cfPWV_Real_SCOR, crPWV_SCOR and PWV ratio (computed as cfPWV_Real_SCOR/crPWV_SCOR), obtained from our data, together with profiles published by other authors. Unfortunately, despite several groups having published cfPWV data, only a few have assessed crPWV, and even fewer have shown values as a function of age. Note the similarity between the PWV ratio data from this work and those obtained in healthy subjects by McEniery et al. [52] and Niiranen et al. [53], although in our work the PWV Ratio = 1 was obtained at older ages. McEniery et al. registered carotid-brachial PWV (cbPWV), whose values are expected to be lower than those of crPWV (forearm arteries are not considered in cbPWV calculus). As can be seen in the figure, crPWV data obtained in this work and those obtained for cbPWV by McEniery et al. showed similar profiles, although the levels of the former were higher. The lower cbPWV levels (compared to those of crPWV) could contribute to explain the differences in the age at which a PWV Ratio = 1 was observed. In other words, the more proximal the arteries or arterial territories measured, the earlier (in terms of years) the PWV ratio would reach a value = 1. On the other hand, it was difficult to carry out a similar analysis considering Niiranen et al. data because although a particular value is shown in the graph (e.g., 35 y), data published by the authors were the mean of a decade (e.g., 40–49 y, 50–59 y, 60–69 y) [53] (Figure 8).
Figure 8.
Comparative age-related profiles for PWV Ratio (Top), cfPWV (Middle) and crPWV or carotid-brachial PWV (cbPWV) (bottom).
Both cfPWV and crPWVcurves showed the expected behavior. About this, cfPWV evidenced the expected curvilinear relationship between age and aortic stiffness (Figure 8), in which age-related stiffness changes were less marked in middle-aged adults and became gradually greater after ~60 y. The steep rise in aortic PWV after the 5–6th decade mirrored the age-related widening in brachial pulse pressure, previously described in nearly all populations worldwide. In contrast to the factors described for aortic stiffness, it is recognized that peripheral (muscular) arteries are less affected by the aging process. About this, age-related increases in crPWV and cbPWV were more gradual, and the range of variation (p50) for crPWV or cbPWV was smaller than for cfPWV (Figure 8).
Finally, the different approaches used to assess aortic stiffness did not show similar age-related profiles (Figure 9). While cfPWV_Real_SCOR and aoPWV_Brachial_MOG showed the expected profile (described above), aoPWV_Carotid_SCOR and aoPWV_Radial_SCOR, showed a different behavior, with a clear rise in the first years (also seen for cfPWV_Real_SCOR), followed by a low rate increase (almost flat) (Figure 9). Then, aoPWV_Carotid_SCOR and aoPWV_Radial_SCOR, would not show the (expected) age-related stiffness profile.
Figure 9.
cfPWV_Real_SCOR (A), aoPWV_Brachial_MOG (B), aoPWV_Carotid_SCOR (C) and aoPWV_Radial_SCOR (D) age-related profiles for subjects included in the RI group.
4.2. Strengths and Limitations
Our results should be interpreted within the context of this work’s strengths and limitations. As the study is a cross-sectional one, it provides no data on longitudinal age-related changes in cfPWV, crPWV or aoPWV (and hence in CAVI and CAVIo). Since no outcome data were considered, cut-off points (e.g., p75th, p90th, p95th) were not defined based on CV risk but on value distribution in the RIs group. Whether or not the reference values should be used as cutoff values for diagnosis and treatment is not known. In this work, the concept of arterial stiffness is mainly presented as a “static process”, rather than the composite of (i) fixed (e.g., due to fibrosis or arterial wall remodeling) and (ii) variable (e.g., due to vascular smooth muscle (VSM) activation-related arterial stiffness (viscoelasticity) modulation). Two issues should be considered in this regard. First, the increases in arterial stiffness with increasing age do not necessarily reflect “concrete-like” changes, but rather a variable and less known increase in stiffness associated with increases in VSM tone (e.g., increased constrictor tone) [54,55]. This component would be of particular importance in the treatment of both hypertension and/or heart failure, and thus represents a potentially central goal in drug therapy [54]. Second, for any age, arterial stiffness can be acutely and temporarily modified by variations in the VSM tone [55,56,57,58]. Systematization of recording conditions is necessary for the evaluation of arterial stiffness considering the modulating role of the VSM tone. In this work, to systematize the records and as a way to minimize the impact of the referred source of variability, arterial stiffness levels were assessed and determined at rest, under stable hemodynamic state conditions. A major strength of the study is that arterial stiffness parameters were obtained in a large population sample (including children, adolescents and adults), and defines the trends in mean value and percentiles for almost the whole range of life expectancy. This would help to identify the physiological behavior (levels and rates) of arterial stiffness and center-to-periphery gradient throughout life, providing important information for clinical diagnosis.
5. Conclusions
Methods and parameters used to assess aortic stiffness (cfPWV_Real, aoPWV_Radial, aoPWV_Carotid and aoPWV_Brachial) and their CAVI and CAVIo, showed different association levels, which in no case were very strong (r ≥ 0.80). Data from different approaches were not equivalent but showed systematic and proportional errors.
The need to define sex-specific RIs relied on the approach used to assess the stiffness and/or on the age considered. In this work, population-based reference values for PWV, stiffness gradient, CAVI and CAVIo indexes were defined; a key step when considering the introduction of the indexes as a tool for the detection of subclinical target organ damage.
Acknowledgments
We thank the children, adolescents and adults, and their families for their participation in the study. To colleagues who integrated the CUiiDARTE Project in different stages, as part of their final degree, master (M.Sc.) and/or doctoral (Ph.D.) projects: Agustina Zinoveev, Federico Farro, Gonzalo Pelusso, Ignacio Farro, Juan M. Castro, Juan Torrado, Marcelo Bermúdez, Marco Marotta, Mariana Gómez, Mariana Marin, Santiago Curcio, Victoria García.
Abbreviations
| Abbreviation | Term |
| aoPWV | Aortic pulse wave velocity |
| bBP | Brachial blood pressure |
| bDBP | Brachial diastolic blood pressure |
| BH | Body height |
| bMBP | Brachial mean blood pressure |
| BMI | Body mass index |
| BP | Blood pressure |
| bPP | Brachial pulse pressure |
| bSBP | Brachial systolic blood pressure |
| BW | Bodyweight |
| CAVI | Cardio-ankle vascular index |
| CCA | Common carotid artery |
| CCC | Concordance correlation coefficients |
| CFA | Common femoral artery |
| cfPWV | Carotid-femoral pulse wave velocity |
| CRFs | Cardiovascular risk factors |
| crPWV | Carotid-radial pulse wave velocity |
| CV | Cardiovascular |
| FPs | Fractional polynomials |
| GTF | General transfer function |
| HR | Heart rate |
| Ln | Natural logarithm |
| MOG | Mobil-O-Graph system or device |
| MV | Mean value |
| PWA | Pulse wave analysis |
| PWV | Pulse wave velocity |
| RIs | Reference intervals |
| SCOR | SphygmoCor system or device |
| SD | Standard deviation |
| WSA | Wave separation analysis |
| y | Years old |
| z- | Z score |
| β | Arterial stiffness index |
| β-PWV | Beta-PWV (or CAVI or CAVIo) |
| ρ | Blood mass density |
Supplementary Materials
The following are available online https://www.mdpi.com/2308-3425/8/1/3/s1. Figure S1. Age-related profiles for cfPWV_Real_SCOR for the RIs group. Figure S2. Age-related profiles for CAVI_cfPWV_Real_SCOR for the RIs group.Figure S3. Age-related profiles for CAVIo_cfPWV_Real_SCOR for the RIs group. Figure S4. Age-related profiles for crPWV_SCOR for the RIs group. Figure S5. Age-related profiles for CAVI_crPWV_SCOR for the RIs group. Figure S6. Age-related profiles for CAVIo_crPWV_SCOR, for the RIs group. Figure S7. Age-related profiles for aoPWV_Radial_SCOR, for the RIs group. Figure S8. Age-related profiles for CAVI_aoPWV_Radial_SCOR for the RIs group. Figure S9. Age-related profiles for CAVIo_aoPWV_Radial_SCOR for the RIs group. Figure S10. Age-related profiles for aoPWV_Carotid_SCOR for the RIs group. Figure S11. Age-related profiles for CAVI_aoPWV_Carotid_SCOR for the RIs group. Figure S12. Age-related profiles for CAVIo_aoPWV_Carotid_SCOR for the RIs group. Figure S13. Age-related profiles for aoPWV_Brachial_MOG for the RIs group. Figure S14. Age-related profiles for CAVI_aoPWV_Brachial_MOG for the RIs group. Figure S15. Age-related profiles for CAVIo_aoPWV_Brachial_MOG for the RIs group. Figure S16. Age-related profiles for PWV_Ratio for the RIs group. Figure S17. Age-related profiles for CAVI_PWV_Ratio for the RIs group. Figure S18. Age-related profiles for CAVIo_PWV_Ratio for the RIs group. Table S1. Subjects demographic, anthropometric, clinical and cardiovascular characteristics: All (n = 3169). Table S2. Subjects demographic, anthropometric, clinical and cardiovascular characteristics: Reference Intervals group (n = 1289). Table S3. Subjects demographic, anthropometric, clinical and cardiovascular characteristics: Excluded group (n = 2330). Table S4. Age-related mean value and standard deviation equations: mathematical model summary (Reference Intervals group). Table S5. cfPWV_Real_SCOR [m/s] reference intervals: All. Table S6. cfPWV_Real_SCOR [m/s] reference intervals: Female. Table S7. cfPWV_Real_SCOR [m/s] reference intervals: Male. Table S8. CAVI_cfPWV_Real_SCOR [m/s] reference intervals: All. Table S9. CAVI_cfPWV_Real_SCOR [m/s] reference intervals: Females. Table S10. CAVI_cfPWV_Real_SCOR [m/s] reference intervals: Males. Table S11. CAVIo_cfPWV_Real_SCOR [m/s] reference intervals: All. Table S12. CAVIo_cfPWV_Real_SCOR [m/s] reference intervals: Females. Table S13. CAVIo_cfPWV_Real_SCOR [m/s] reference intervals: Males. Table S14. crPWV_SCOR [m/s] reference intervals: All. Table S15. crPWV_SOR [m/s] reference intervals: Females. Table S16. crPWV_SCOR [m/s] reference intervals: Males. Table S17. CAVI_ crPWV_SCOR [m/s] reference intervals: All. Table S18. CAVI_crPWV_SCOR [m/s] reference intervals: Females. Table S19. CAVI_crPWV_SCOR [m/s] reference intervals: Males. Table S20. CAVIo_crPWV_SCOR [m/s] reference intervals: All. Table S21. CAVIo_crPWV_SCOR [m/s] reference intervals: Females. Table S22. CAVIo_crPWV_SCOR [m/s] reference intervals: Males. Table S23. aoPWV_Radial_SCOR [m/s] reference intervals: All. Table S24. aoPWV_Radial_SCOR [m/s] reference intervals: Females. Table S25. aoPWV_Radial_SCOR [m/s] reference intervals: Males. Table S26. CAVI_aoPWV_Radial_SCOR [m/s] reference intervals: All. Table S27. CAVI_aoPWV_Radial_SCOR [m/s] reference intervals: Females. Table S28. CAVI_aoPWV_Radial_SCOR [m/s] reference intervals: Males. Table S29. CAVIo_aoPWV_Radial_SCOR [m/s] reference intervals: All. Table S30. CAVIo_aoPWV_Radial_SCOR [m/s] reference intervals: Females. Table S31. CAVIo_aoPWV_Radial_SCOR [m/s] reference intervals: Males. Table S32. aoPWV_Carotid_SCOR [m/s] reference intervals: All. Table S33. aoPWV_Carotid_SCOR [m/s] reference intervals: Females. Table S34. aoPWV_Carotid_SCOR [m/s] reference intervals: Males. Table S35. CAVI_aoPWV_Carotid_SCOR [m/s] reference intervals: All. Table S36. CAVI_aoPWV_Carotid_SCOR [m/s] reference intervals: Females. Table S37. CAVI_aoPWV_Carotid_SCOR [m/s] reference intervals: Males. Table S38. CAVIo_aoPWV_Carotid_SCOR [m/s] reference intervals: All. Table S39. CAVIo_aoPWV_Carotid_SCOR [m/s] reference intervals: Females. Table S40. CAVIo_aoPWV_Carotid_SCOR [m/s] reference intervals: Males. Table S41. aoPWV_Brachial_MOG [m/s] reference intervals: All. Table S42. aoPWV_Brachial_MOG [m/s] reference intervals: Females. Table S43. aoPWV_Brachial_MOG [m/s] reference intervals: Males. Table S44. CAVI_aoPWV_Brachial_MOG [m/s] reference intervals: All. Table S45. CAVI_aoPWV_Brachial_MOG [m/s] reference intervals: Females. Table S46. CAVI_aoPWV_Brachial_MOG [m/s] reference intervals: Males. Table S47. CAVIo_aoPWV_Brachial_MOG [m/s] reference intervals: All. Table S48. CAVIo_aoPWV_Brachial_MOG [m/s] reference intervals: Females. Table S49. CAVIo_aoPWV_Brachial_MOG [m/s] reference intervals: Males. Table S50. PWV_Ratio reference intervals: All. Table S51. PWV_Ratio reference intervals: Females. Table S52. PWV_Ratio reference intervals: Males. Table S53. CAVI_PWV_Ratio reference intervals: All. Table S54. CAVI_PWV_Ratio reference intervals: Females. Table S55. CAVI_PWV_Ratio reference intervals: Males. Table S56. CAVIo_PWV_Ratio reference intervals: All. Table S57. CAVIo_PWV_Ratio reference intervals: Females. Table S58. CAVIo_PWV_Ratio reference intervals: Males.
Author Contributions
Conceptualization, D.B. and Y.Z.; Formal analysis, D.B. and Y.Z.; Funding acquisition, D.B. and Y.Z.; Investigation, D.B. and Y.Z.; Methodology, D.B. and Y.Z.; Project administration, D.B. and Y.Z.; Visualization, D.B. and Y.Z.; Writing—original draft, D.B. and Y.Z.; Writing—review and editing, D.B. and Y.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Agencia Nacional de Investigación e Innovación (ANII), the Ministry for Social Development (MIDES), the United Nations Children’s Fund (UNICEF), grant number/code: FSPI_X_2015_1_108484, PRSCT-008-020; and extra-budgetary funds provided by the CUiiDARTE (Dr. Bia, Dr. Zócalo).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Centro Hospitalario Pereira Rossell, Universidad de la República (Protocl code: 01; Date of approval: 29-Nov-2013 and 29-Dec-2015).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in thos study are available within the article and in supplementary material.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the study design; collection, analyses or interpretation of data; in the manuscript writing, nor in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cavalcante J.L., Lima J.A., Redheuil A., Al-Mallah M.H. Aortic stiffness: Current understanding and future directions. J Am. Coll. Cardiol. 2011;57:1511–1522. doi: 10.1016/j.jacc.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 2.Lee H.Y., Oh B.H. Aging and arterial stiffness. Circ. J. 2010;74:2257–2262. doi: 10.1253/circj.CJ-10-0910. [DOI] [PubMed] [Google Scholar]
- 3.Kim H.L., Kim S.H. Pulse Wave Velocity in Atherosclerosis. Front. Cardiovasc. Med. 2019;6:41. doi: 10.3389/fcvm.2019.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Bortel L.M., Laurent S., Boutouyrie P., Chowienczyk P., Cruickshank J.K., De Backer T., Filipovsky J., Huybrechts S., Mattace-Raso F.U., Protogerou A.D., et al. European Society of Hypertension Working Group on Vascular Structure and Function; European Network for Noninvasive Investigation of Large Arteries. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J. Hypertens. 2012;30:445–448. doi: 10.1097/HJH.0b013e32834fa8b0. [DOI] [PubMed] [Google Scholar]
- 5.Jurko T., Mestanik M., Jurko A., Jr., Spronck B., Avolio A., Mestanikova A., Sekaninova N., Tonhajzerova I. Pediatric reference values for arterial stiffness parameters cardio-ankle vascular index and CAVI0. J. Am. Soc. Hypertens. 2018;12:e35–e43. doi: 10.1016/j.jash.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Shirai K., Utino J., Otsuka K., Takata M. A novel blood pressure independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI) J. Atheroscler. Thromb. 2006;13:101–107. doi: 10.5551/jat.13.101. [DOI] [PubMed] [Google Scholar]
- 7.Wassertheurer S., Hametner B., Mayer C.C., Hafez A., Negishi K., Papaioannou T.G., Protogerou A.D., Sharman J.E., Weber T. Aortic systolic pressure derived with different calibration methods: Associations to brachial systolic pressure in the general population. Blood Press Monit. 2018;23:134–140. doi: 10.1097/MBP.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 8.Yu S., McEniery C.M. Central Versus Peripheral Artery Stiffening and Cardiovascular Risk. Arterioscler. Thromb. Vasc. Biol. 2020;40:1028–1033. doi: 10.1161/ATVBAHA.120.313128. [DOI] [PubMed] [Google Scholar]
- 9.Castro J.M., García-Espinosa V., Zinoveev A., Marin M., Severi C., Chiesa P., Bia D., Zócalo Y. Arterial structural and functional characteristics at end of early Ccildhood and beginning of adulthood: Impact of body size gain during early, intermediate, late and global growth. J. Cardiovasc. Dev. Dis. 2019;6:33. doi: 10.3390/jcdd6030033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santana D.B., Zócalo Y.A., Armentano R.L. Integrated e-Health approach based on vascular ultrasound and pulse wave analysis for asymptomatic atherosclerosis detection and cardiovascular risk stratification in the community. IEEE Trans. Inf. Technol. Biomed. 2012;16:287–294. doi: 10.1109/TITB.2011.2169977. [DOI] [PubMed] [Google Scholar]
- 11.Santana D.B., Zócalo Y.A., Ventura I.F., Arrosa J.F., Florio L., Lluberas R., Armentano R.L. Health informatics design for assisted diagnosis of subclinical atherosclerosis, structural, and functional arterial age calculus and patient-specific cardiovascular risk evaluation. IEEE Trans. Inf. Technol. Biomed. 2012;16:943–951. doi: 10.1109/TITB.2012.2190990. [DOI] [PubMed] [Google Scholar]
- 12.Zinoveev A., Castro J.M., García-Espinosa V., Marin M., Chiesa P., Bia D., Zócalo Y. Aortic pressure and forward and backward wave components in children, adolescents and young-adults: Agreement between brachial oscillometry, radial and carotid tonometry data and analysis of factors associated with their differences. PLoS ONE. 2019;14:e0226709. doi: 10.1371/journal.pone.0226709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zócalo Y., García-Espinosa V., Castro J.M., Zinoveev A., Marin M., Chiesa P., Díaz A., Bia D. Stroke volume and cardiac output non-invasive monitoring based on brachial oscillometry-derived pulse contour analysis: Explanatory variables and reference intervals throughout life (3–88 years) Cardiol. J. 2020 doi: 10.5603/CJ.a2020.0031. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mancia G., De Backer G., Dominiczak A., Cifkova R., Fagard R., Germano G. Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur. Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . Definition, Diagnosis, and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation. Part 1: Diagnosis and Classification of Diabetes Mellitus. WHO; Geneva, Switzerland: 1999. [Google Scholar]
- 16.Wilson P.W., D’Agostino R.B., Levy D., Belanger A.M., Silbershatz H., Kannel W.B. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 17.WHO . Obesity: Preventing and Managing the Global Epidemic. World Health Organization; Geneva, Switzerland: 2000. [PubMed] [Google Scholar]
- 18.Bossuyt J., Engelen L., Ferreira I., Stehouwer C.D., Boutouyrie P., Laurent S., Segers P., Reesink K., Van Bortel L.M. Reference Values for Arterial Measurements Collaboration. Reference values for local arterial stiffness. Part B: Femoral artery. J. Hypertens. 2015;33:1997–2009. doi: 10.1097/HJH.0000000000000655. [DOI] [PubMed] [Google Scholar]
- 19.Engelen L., Bossuyt J., Ferreira I., van Bortel L.M., Reesink K.D., Segers P., Stehouwer C.D., Laurent S., Boutouyrie P. Reference Values for Arterial Measurements Collaboration. Reference values for local arterial stiffness. Part A: Carotid artery. J. Hypertens. 2015;33:1981–1996. doi: 10.1097/HJH.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 20.Engelen L., Ferreira I., Stehouwer C.D., Boutouyrie P., Laurent S. Reference Values for Arterial Measurements Collaboration. Reference intervals for common carotid intima-media thickness measured with echotracking: Relation with risk factors. Eur. Heart J. 2013;34:2368–2380. doi: 10.1093/eurheartj/ehs380. [DOI] [PubMed] [Google Scholar]
- 21.Herbert A., Cruickshank J.K., Laurent S., Boutouyrie P. Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure and its amplification in a general healthy population and according to cardiovascular risk factors. Eur. Heart J. 2014;35:3122–3133. doi: 10.1093/eurheartj/ehu293. [DOI] [PubMed] [Google Scholar]
- 22.Marin M., Bia D., Zócalo Y. Carotid and Femoral Atherosclerotic Plaques in Asymptomatic and Non-Treated Subjects: Cardiovascular Risk Factors, 10-Years Risk Scores, and Lipid Ratios´ Capability to Detect Plaque Presence, Burden, Fibro-Lipid Composition and Geometry. J. Cardiovasc. Dev. Dis. 2020;7:11. doi: 10.3390/jcdd7010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zócalo Y., Bia D. Ultrasonografía carotídea para detección de placas de ateroma y medición del espesor íntima-media; índice tobillo-brazo: Evaluación no invasivaen la práctica clínica: Importancia clínica y análisis de las bases metodológicas para su evaluación. Rev. Urug. Cardiol. 2016;31:47–60. [Google Scholar]
- 24.Farro I., Bia D., Zócalo Y., Torrado J., Farro F., Florio L., Olascoaga A., Alallón W., Lluberas R., Armentano R.L. Pulse wave velocity as marker of preclinical arterial disease: Reference levels in a uruguayan population considering wave detection algorithms, path lengths, aging, and blood pressure. Int. J. Hypertens. 2012;2012:169359. doi: 10.1155/2012/169359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bia D., Zócalo Y. Rigidez arterial: Evaluación no invasiva en la práctica clínica Importancia clínica y análisis de las bases metodológicas de los equipos disponibles para su evaluación. Rev. Urug. Cardiol. 2014;29:39–59. [Google Scholar]
- 26.Boutouyrie P., Briet M., Collin C., Vermeersch S., Pannier B. Assessment of pulse wave velocity. Artery Res. 2009;3:3–8. doi: 10.1016/j.artres.2008.11.002. [DOI] [Google Scholar]
- 27.Reference Values for Arterial Stiffness’ Collaboration Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur. Heart J. 2010;31:2338–2350. doi: 10.1093/eurheartj/ehq165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bia D., Valtuille R., Galli C., Wray S., Armentano R., Zócalo Y., Cabrera-Fischer E. Aortic-Radial Pulse Wave Velocity Ratio in End-stage Renal Disease Patients: Association with Age, Body Tissue Hydration Status, Renal Failure Etiology and Five Years of Hemodialysis. High Blood Press Cardiovasc. Prev. 2017;24:37–48. doi: 10.1007/s40292-017-0178-3. [DOI] [PubMed] [Google Scholar]
- 29.Bia D., Galli C., Zocalo Y., Valtuille R., Wray S., Pessana F., Cabrera-Fischer E.I. Central-To-Peripheral Arterial Stiffness Gradient in Hemodialyzed Patients Depends on the Location of the Upper-limb Vascular Access. Curr. Hypertens. Rev. 2018;14:128–136. doi: 10.2174/1573402114666180413122055. [DOI] [PubMed] [Google Scholar]
- 30.Salvi P., Scalise F., Rovina M., Moretti F., Salvi L., Grillo A., Gao L., Baldi C., Faini A., Furlanis G., et al. Noninvasive Estimation of Aortic Stiffness Through Different Approaches. Hypertension. 2019;74:117–129. doi: 10.1161/HYPERTENSIONAHA.119.12853. [DOI] [PubMed] [Google Scholar]
- 31.Wohlfahrt P., Krajčoviechová A., Seidlerová J., Mayer O., Bruthans J., Filipovský J., Laurent S., Cífková R. Arterial stiffness parameters: How do they differ? Atherosclerosis. 2013;231:359–364. doi: 10.1016/j.atherosclerosis.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Bia D., Galli C., Valtuille R., Zócalo Y., Wray S.A., Armentano R.L., Cabrera-Fischer E.I. Hydration Status Is Associated with Aortic Stiffness, but Not with Peripheral Arterial Stiffness, in Chronically Hemodialysed Patients. Int. J. Nephrol. 2015;2015:628654. doi: 10.1155/2015/628654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spronck B., Delhaas T., Butlin M., Reesink K.D., Avolio A.P. Options for Dealing with Pressure Dependence of Pulse Wave Velocity as a Measure of Arterial Stiffness: An Update of Cardio-Ankle Vascular Index (CAVI) and CAVI0. Pulse. 2018;5:106–114. doi: 10.1159/000479322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Royston P., Wright E. A method for estimating age-specific reference intervals (‘normal ranges’) based on fractional polynomials and exponential transformation. J. R. Stat. Soc. Ser. A Stat. Soc. 1998;161:79–101. doi: 10.1111/1467-985X.00091. [DOI] [Google Scholar]
- 35.Díaz A., Zócalo Y., Bia D. Percentile curves for left ventricle structural, functional and haemodynamic parameters obtained in healthy children and adolescents from echocardiography-derived data. J. Echocardiogr. 2020;18:16–43. doi: 10.1007/s12574-019-00425-0. [DOI] [PubMed] [Google Scholar]
- 36.Diaz A., Bia D., Zócalo Y., Manterola H., Larrabide I., Lo Vercio L., Del Fresno M., Cabrera Fischer E. Carotid Intima Media Thickness Reference Intervals for a Healthy Argentinean Population Aged 11–81 Years. Int. J. Hypertens. 2018;2018:8086714. doi: 10.1155/2018/8086714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Díaz A., Zócalo Y., Bia D. Normal percentile curves for left atrial size in healthy children and adolescents. Echocardiography. 2019;36:770–782. doi: 10.1111/echo.14286. [DOI] [PubMed] [Google Scholar]
- 38.Bellera C.A., Hanley J.A. A method is presented to plan the required sample size when estimating regression-based reference limits. J. Clin. Epidemiol. 2007;60:610–615. doi: 10.1016/j.jclinepi.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 39.Lumley T., Diehr P., Emerson S., Chen L. The importance of the normality assumption in large public health data sets. Annu. Rev. Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 40.Hayes A.F. Introduction to mediation, Moderation, and Conditional Proess Analysis (2nd Edition) [(accessed on 13 November 2020)]; Available online: http://www.guilford.com/p/hayes3.
- 41.Evans J.D. Straightforward Statistics for the Behavioral Sciences. Brooks-Cole Publishing; Pacific Grove, CA, USA: 1996. [Google Scholar]
- 42.Curcio S., García-Espinosa V., Arana M., Farro I., Chiesa P., Giachetto G., Zócalo Y., Bia D. Growing-Related Changes in Arterial Properties of Healthy Children, Adolescents, and Young Adults Nonexposed to Cardiovascular Risk Factors: Analysis of Gender-Related Differences. Int. J. Hypertens. 2016;2016:4982676. doi: 10.1155/2016/4982676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McEniery C.M., Yasmin N., Hall I.R., Qasem A., Wilkinson I.B., Cockcroft J.R., ACCT Investigators Normal vascular aging: Differential effects on wave reflection and aortic pulse wave velocity: The Anglo-Cardiff Collaborative Trial (ACCT) J. Am. Coll. Cardiol. 2005;46:1753–1760. doi: 10.1016/j.jacc.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 44.Mitchell G.F., Hwang S.J., Vasan R.S., Larson M.G., Pencina M.J., Hamburg N.M., Vita J.A., Levy D., Benjamin E.J. Arterial stiffness and cardiovascular events: The Framingham Heart Study. Circulation. 2010;121:505–511. doi: 10.1161/CIRCULATIONAHA.109.886655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bia D., Aguirre I., Zócalo Y., Devera L., Cabrera-Fischer E., Armentano R. Regional differences in viscosity, elasticity and wall buffering function in systemic arteries: Pulse wave analysis of the arterial pressure-diameter relationship. Rev. Esp. Cardiol. 2005;58:167–174. doi: 10.1157/13071891. [DOI] [PubMed] [Google Scholar]
- 46.Bia D., Zócalo Y., Cabrera-Fischer E., Wray W., Armentano R. Quantitative Analysis of the Relationship between Blood Vessel Wall Constituents and Viscoelastic Properties: Dynamic Biomechanical and Structural In Vitro Studies in Aorta and Carotid Arteries. Physiol. J. 2014 doi: 10.1155/2014/142421. [DOI] [Google Scholar]
- 47.Fortier C., Desjardins M.P., Agharazii M. Aortic-Brachial Pulse Wave Velocity Ratio: A Measure of Arterial Stiffness Gradient Not Affected by Mean Arterial Pressure. Pulse. 2018;5:117–124. doi: 10.1159/000480092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fortier C., Agharazii M. Arterial Stiffness Gradient. Pulse. 2016;3:159–166. doi: 10.1159/000438852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hashimoto J., Ito S. Central pulse pressure and aortic stiffness determine renal hemodynamics: Pathophysiological implication for microalbuminuria in hypertension. Hypertension. 2011;58:839–846. doi: 10.1161/HYPERTENSIONAHA.111.177469. [DOI] [PubMed] [Google Scholar]
- 50.Tarumi T., Shah F., Tanaka H., Haley A.P. Association between central elastic artery stiffness and cerebral perfusion in deep subcortical gray and white matter. Am. J. Hypertens. 2011;24:1108–1113. doi: 10.1038/ajh.2011.101. [DOI] [PubMed] [Google Scholar]
- 51.Mitchell G.F., van Buchem M.A., Sigurdsson S., Gotal J.D., Jonsdottir M.K., Kjartansson O., Garcia M., Aspelund T., Harris T.B., Gudnason V., et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: The Age, Gene/Environment Susceptibility-Reykjavik study. Brain. 2011;134:3398–3407. doi: 10.1093/brain/awr253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McEniery C., Wilkinson I., Avolio A. Age, hypertension and arterial function. Clin. Exp. Pharmacol. Physiol. 2007;34:665–671. doi: 10.1111/j.1440-1681.2007.04657.x. [DOI] [PubMed] [Google Scholar]
- 53.Niiranen T.J., Kalesan B., Larson M.G., Hamburg N.M., Benjamin E.J., Mitchell G.F., Vasan R.S. Aortic-Brachial Arterial Stiffness Gradient and Cardiovascular Risk in the Community: The Framingham Heart Study. Hypertension. 2017;69:1022–1028. doi: 10.1161/HYPERTENSIONAHA.116.08917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Armentano R.L., Barra J.G., Santana D.B., Pessana F.M., Graf S., Craiem D., Brandani L.M., Baglivo H.P., Sanchez R.A. Smart damping modulation of carotid wall energetics in human hypertension: Effects of angiotensin-converting enzyme inhibition. Hypertension. 2006;47:384–390. doi: 10.1161/01.HYP.0000205915.15940.15. [DOI] [PubMed] [Google Scholar]
- 55.Armentano R.L., Barra J.G., Pessana F.M., Craiem D.O., Graf S., Santana D.B., Sanchez R.A. Smart smooth muscle spring-dampers. Smooth muscle smart filtering helps to more efficiently protect the arterial wall. IEEE Eng. Med. Biol. Mag. 2007;26:62–70. doi: 10.1109/MEMB.2007.289123. [DOI] [PubMed] [Google Scholar]
- 56.Bia D., Zócalo Y., Armentano R., Camus J., De Forteza E., Cabrera-Fischer E. Increased reversal and oscillatory shear stress cause smooth muscle contraction-dependent changes in sheep aortic dynamics: Role in aortic balloon pump circulatory support. Acta Physiol. 2008;192:487–503. doi: 10.1111/j.1748-1716.2007.01765.x. [DOI] [PubMed] [Google Scholar]
- 57.Bia D., Armentano R.L., Grignola J.C., Craiem D., Zócalo Y.A., Ginés F.F., Levenson J. The vascular smooth muscle of great arteries: Local control site of arterial buffering function? Rev. Esp. Cardiol. 2003;56:1202–1209. doi: 10.1016/S0300-8932(03)77039-0. [DOI] [PubMed] [Google Scholar]
- 58.Fischer E.C., Santana D.B., Zócalo Y., Camus J., De Forteza E., Armentano R. Effects of removing the adventitia on the mechanical properties of ovine femoral arteries in vivo and in vitro. Circ. J. 2010;74:1014–1022. doi: 10.1253/circj.CJ-09-0496. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in thos study are available within the article and in supplementary material.