Abstract
Cutaneous melanoma is the deadliest type of skin cancer, characterized by a high molecular and metabolic heterogeneity which contributes to therapy resistance. Despite advances in treatment, more efficient therapies are needed. Olive oil compounds have been described as having anti-cancer properties. Here, we clarified the cytotoxic potential of oleic acid, homovanillyl alcohol, and hydroxytyrosol on melanoma cells. Metabolic viability was determined 48 h post treatment of A375 and MNT1 cells. Metabolic gene expression was assessed by qRT-PCR and Mitogen-Activated Protein Kinase (MAPK) activation by Western blot. Hydroxytyrosol treatment (100 and 200 µM) significantly reduced A375 cell viability (p = 0.0249; p < 0.0001) which, based on the expression analysis performed, is more compatible with a predominant glycolytic profile and c-Jun N-terminal kinase (JNK) activation. By contrast, hydroxytyrosol had no effect on MNT1 cell viability, which demonstrates an enhanced oxidative metabolism and extracellular signal-regulated kinase (ERK) activation. This compound triggered cell detoxification and the use of alternative energy sources in A375 cells, inhibiting JNK and ERK pathways. Despite oleic acid and homovanillyl alcohol demonstrating no effect on melanoma cell viability, they influenced the MNT1 glycolytic rate and A375 detoxification mechanisms, respectively. Both compounds suppressed ERK activation in MNT1 cells. The distinct cell responses to olive oil compounds depend on the metabolic and molecular mechanisms preferentially activated. Hydroxytyrosol may have a cytotoxic potential in melanoma cells with predominant glycolytic metabolism and JNK activation.
Keywords: cutaneous melanoma, oleic acid, homovanillyl alcohol, hydroxytyrosol, cell metabolism, molecular mechanisms
1. Introduction
Cutaneous melanoma (CM) arises from the malignant transformation of melanocytes found in the skin [1]. Despite representing only 5% of all skin malignancies, CM is the most lethal type of skin cancer, accounting for more than 70% of all skin cancer-related deaths [2,3]. Indeed, the high mortality rate of CM patients is mainly related to its elevated potential to metastasize to surrounding tissues [4]. Melanoma progression and metastasis are influenced by the molecular and metabolic heterogeneity of melanoma cells, crucial in survival and acquisition of different nutrient sources [5]. In addition, this heterogeneity is also thought to play an active role in the development of therapy resistance, allowing melanoma cells to change and respond to microenvironmental cues [5]. In fact, it represents one of the main barriers to the efficiency of therapeutic approaches [6]. Currently, the available treatments for advanced-stage CM patients are surgical excision, when it is possible, targeted therapies, and immunotherapies. In the case of V-raf murine sarcoma viral oncogene homolog B1 (BRAF)-mutant melanomas, highly selective BRAF and mitogen-activated protein kinase (MEK) inhibitors have shown to improve patient survival [7,8,9]. However, only half of these patients demonstrate a positive response to targeted therapies, which tends to be limited over time [10]. On the other hand, immunotherapies targeting cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and programmed cell-death protein 1 (PD-1) can lead to more durable responses compared to targeted therapies, also providing a survival benefit [9,11,12]. Nonetheless, response to immunotherapies is still limited, and acquired resistance is a problem for 40–70% of metastatic melanoma patients [11,13,14]. Thus, the identification of new potential therapeutic approaches is needed.
During recent years, several studies have described the medicinal properties of both olives and olive oil (reviewed in [15,16]). It is now widely accepted that monounsaturated fatty acids, phenolic compounds, and other phytochemicals present in olives and olive oil have numerous beneficial and protective effects, in regards to oxidative damage, inflammation, cardiovascular and neurodegenerative diseases, and cancer [15,16]. In addition, these bioactive compounds may influence the expression of genes involved in these processes, notably inflammation and oxidative stress [17]. As such, there is growing evidence that personalized and natural therapeutic approaches could be a promising alternative to prevent cancer progression [18].
Some studies have already explored the effect of compounds derived from olive oil in melanoma. D’Angelo et al. found that hydroxytyrosol, a phenolic compound, has a protective effect in UVA-irradiated melanoma cells, decreasing oxidative damage at lower concentrations (100–400 µM), while at higher concentrations, it inhibits cell proliferation and activates caspase 3, thereby promoting cell apoptosis [19]. Oleic acid, a monounsaturated fatty acid, is also thought to have a protective role against malignancy, reducing cell invasiveness by inhibiting the secretion of SPARC and cathepsin B in melanoma cell lines [20]. However, another study has recently reported that oleic acid did not influence the proliferative capability and melanogenesis of human melanocytes [21]. Thus far, no study has reported the effect of homovanillyl alcohol, a metabolite of hydroxytyrosol, on the viability or aggressiveness of melanoma cells. However, this compound has also been associated with some health benefits, including lower risk for cardiovascular disease across the elderly population [22] and the ability to decrease oxidative stress by scavenging ROS [23,24]. Still, the lack of information about the underlying mechanisms that might explain the reported beneficial effects of olive oil-derived compounds on melanoma remains. Specifically, the effects of hydroxytyrosol, oleic acid, and homovanillyl alcohol, which belong to distinct chemical classes of olive oil compounds, on melanoma are not fully understood yet, since the few available data are controversial. By exploring different classes of olive oil compounds, with distinct features and mechanisms, it might be possible to identify the most promising group of compounds associated with the beneficial effects of olive oil.
In this context, we analyzed the potential of three olive oil compounds: oleic acid, homovanillyl alcohol, and hydroxytyrosol as cytotoxic agents and their implications for the metabolic reprogramming of melanoma cell models.
2. Results
2.1. Impact of Oleic Acid, Homovanillyl Alcohol, and Hydroxytyrosol on A375 and MNT1 Melanoma Cell Viability
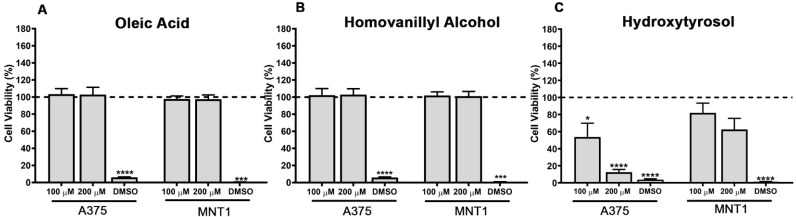
The effects of oleic acid, homovanillyl alcohol, and hydroxytyrosol on CM were assessed using viability assays performed 48 h post treatment of two BRAF mutated melanoma cell lines (A375 and MNT1). The concentrations tested were selected based on the literature available about the effects of these compounds on different types of cancer, as well as on the reported concentrations of oleic acid in plasma [19,20,25,26,27,28,29,30]. The treatment with oleic acid and homovanillyl alcohol did not affect the viability of either melanoma cell line in a statistically significant manner (Figure 1A,B). However, the treatment with 100 µM and 200 µM of hydroxytyrosol significantly reduced the viability (p = 0.0249; p < 0.0001) of A375 cells to approximately 50% and 15% compared to control cells, respectively (Figure 1C). Interestingly, this phenolic compound did not have the same impact on MNT1 cells, but there was a trend for viability reduction, mainly when these cells were treated with a higher concentration of hydroxytyrosol (200 µM).
Figure 1.
Effects of (A) oleic acid, (B) homovanillyl alcohol, and (C) hydroxytyrosol treatment at concentrations of 100 µM and 200 µM on the metabolic viability of A375 and MNT1 cells, 48 h post incubation. Cell viability of untreated control cells is represented by the dashed line at 100%. Cells treated with 5% dimethyl sulfoxide (DMSO) were used as a positive control of cell viability. Results are representative of at least three independent experiments, performed in triplicate. Data obtained are shown as mean ± standard error of the mean (SEM). Student’s t-test was used to compare each experimental condition with the respective untreated control, * p < 0.05, *** p < 0.001, **** p < 0.0001.
2.2. Metabolic Gene Expression in A375 and MNT1 Melanoma Cells
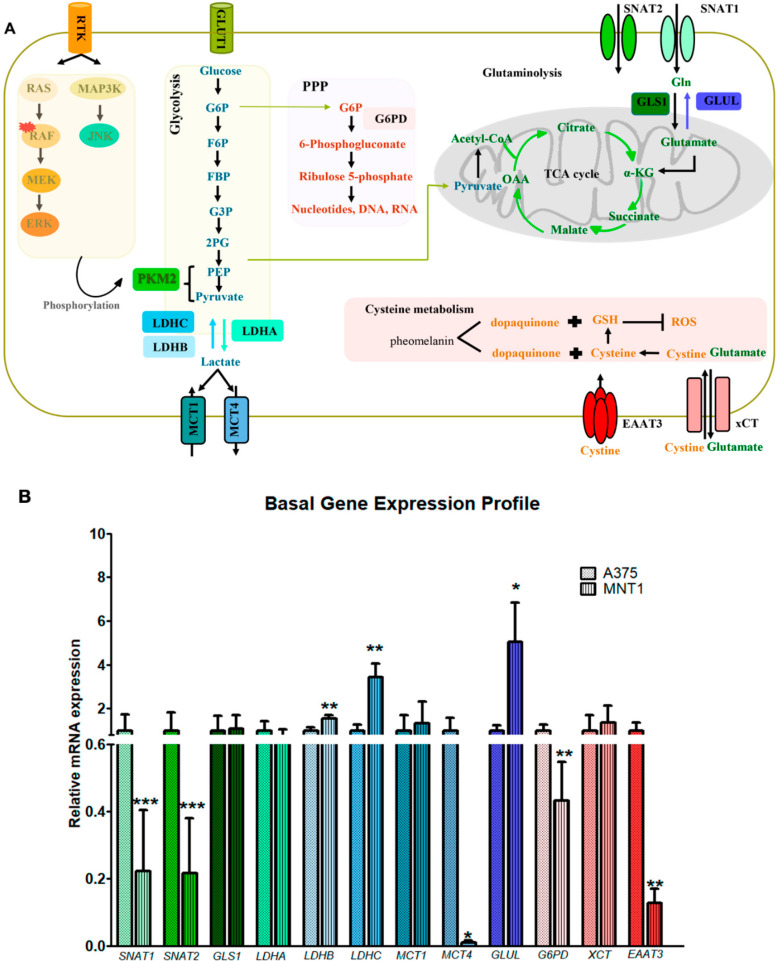
MNT1 cells seem to be more resistant to the cytotoxic effect exerted by hydroxytyrosol than A375 cells. In this context, we hypothesized that these two cell models have different metabolic profiles, and we evaluated the expression of genes involved in glutamine and lactate transport and metabolism, pentose phosphate pathway and cysteine transport, hereinafter referred to as metabolic gene expression (Figure 2A). Molecular and metabolic pathways could impact melanoma survival. Rat sarcoma (RAS)/rapidly accelerated fibrosarcoma, (RAF)/mitogen-activated protein kinase (MEK)/extracellular signal-regulated kinase (ERK), and mitogen-activated protein kinase kinase kinase (MAP3K)/c-Jun N-terminal kinase (JNK) pathways mediate pyruvate kinase M2 (PKM2) phosphorylation, ultimately promoting glycolysis. In glycolysis, glucose is converted into pyruvate after several enzymatic reactions involving the following substrates: glucose 6 phosphate (G6P), fructose-6-phosphate (F6P), fructose-1,6-biphosphate (FBP), glyceraldeyde-3-phosphate (G3P), 2-phosphoglycerate (2PG), and phosphoenolpyruvate (PEP). Pyruvate is then converted into lactate by lactate dehydrogenase A (LDHA), and the opposite reaction is mediated by lactate dehydrogenase B and C (LDHB and LDHC). Monocarboxylate transporter 1 and 4 (MCT1 and MCT4) are responsible for lactate import and export from the intracellular space, respectively. In the pentose phosphate pathway (PPP), glucose-6-phosphate dehydrogenase (G6PD) converts glucose-6-phosphate into 6-phosphogluconate. Glutamine is transported to the intracellular medium mainly through Sodium-coupled neutral amino acid transporter 1 and 2 (SNAT1 and SNAT2). Thereafter, glutamine can be converted into glutamate by glutaminase 1 (GLS1), which will supply the TCA cycle by promoting α ketoglutarate (α-KG) production. Contrarily, glutamine synthetase (GLUL) promotes glutamine synthesis via glutamate. To prevent the oxidative stress induced by ROS and maintaining redox balance, melanoma cells possess the ability to induce antioxidant adaptive mechanisms, namely through glutathione (GSH) biosynthesis. Cystine uptake by the transporter cystine glutamate transporter (xCT) and excitatory amino acid transporter 3 (EAAT3) is of the utmost importance to ensure cell detoxification mechanisms (Figure 2A).
Figure 2.
Metabolic characterization of A375 and MNT1 melanoma cells. (A) Schematic representation of the main metabolic pathways activated in melanoma cells and their association with MAPK pathways (c-Jun N-terminal kinase (JNK) and extracellular signal-regulated kinase (ERK) activation). Glycolysis, pentose phosphate pathway (PPP), TCA cycle, glutaminolysis, and cysteine metabolism are the main metabolic pathways represented. (B) Expression analysis of several genes involved in the metabolic pathways previously mentioned in A375 and MNT1 cells by RT qPCR. Error bars represent the standard deviation of mean values obtained from triplicate experiments. Student’s t-test was used to compare two independent groups * p < 0.05; ** p < 0.01; and *** p < 0.001.
This gene expression analysis showed the downregulation of genes encoding transporters involved in the uptake of neutral α-amino-acids, mostly glutamine, such as SNAT1 and SNAT2 in MNT1 cells (p = 0.0002; p = 0.0014) (Figure 2B). Considering that these transporters are mainly responsible for glutamine uptake, these results suggest that A375 cells are more dependent on the exogenous supply of glutamine and other neutral amino-acids as alternative energy sources compared to MNT1. Interestingly, LDHB and LDHC, but not LDHA were upregulated in MNT1 cells (p = 0.0025; p = 0.0018). LDHB and LDHC genes encode enzymes that convert l-lactate into pyruvate when oxygen is abundant, while LDHA encodes an isoform responsible for the opposite reaction—conversion of pyruvate into l-lactate, in anaerobic conditions, as previously represented in Figure 2A. According to these data, MNT1 cells seem to be more dependent on oxidative metabolism compared to A375 cells. In addition, MCT4, which encodes a transporter that facilitates lactate efflux, was downregulated in MNT1 cells (p = 0.0128). The downregulation of this transporter could corroborate with the idea that large amounts of lactate remain in the intracellular medium, being directed to the TCA cycle. No differences were found in MCT1 expression, seeming to indicate that lactate import is not affected. The GLUL gene encodes an enzyme, glutamine synthetase, crucial for glutamate conversion into glutamine and it was found upregulated in MNT1 compared to A375 cells (p = 0.0256), which indicates that MNT1 cells are less dependent on the exogenous supply of glutamine. G6PD was also downregulated in MNT1 cells, probably suggesting that glucose-6-phosphate is being directed for glycolysis and not to PPP (p = 0.0081). EAAT3 was also downregulated in MNT1 cells (p = 0.0031), although no differences were observed in xCT expression.
2.3. Effects of Oleic Acid, Homovanillyl Alcohol, and Hydroxytyrosol Induced Metabolic Gene Expression Changes on A375 and MNT1 Melanoma Cells
Further, we assessed the metabolic changes promoted by oleic acid, homovanillyl alcohol, and hydroxytyrosol on both melanoma cell models. To clarify the distinct effect of hydroxytyrosol on both melanoma cell lines, the activation of several metabolic pathways was assessed to detect whether the differences in viability were dependent on the activation of specific metabolic pathways in each cell line. For that purpose, A375 and MNT1 melanoma cells were treated with the same concentrations of hydroxytyrosol used in the viability assays. Despite oleic acid and homovanillyl alcohol showing no effect on melanoma cell viability, we also investigated if the absence of a cytotoxic effect was due to the activation of metabolic pathways.
The treatment with oleic acid (100 µM) induced LDHA, LDHB, and LDHC downregulation in MNT1 cells (p = 0.043; p = 0.039; p = 0.042, respectively) (Table 1; Figure S1). Considering that all these genes belong to the same family, oleic acid seems to affect the conversion of pyruvate into lactate, as well as the opposite reaction. Consequently, the energy produced through glycolysis is significantly reduced after oleic acid treatment. According to the previous results (Figure 2B), MNT1 cells seem to be more dependent on an oxidative metabolism and less dependent on the exogenous supply of glutamine. Thus, it is likely that deficiencies in the glycolytic rate might not be determinant in causing cytotoxic effects. Contrarily to MNT1 cells, oleic acid treatment did not significantly alter the expression of any of the analyzed genes in A375 cells (Table 1; Figure S1).
Table 1.
Effects of oleic acid, homovanillyl alcohol, and hydroxytyrosol treatment on metabolic gene expression in A375 and MNT1 cells after 48 h of exposure by RT-qPCR analysis.
| A375 Melanoma Cells | MNT1 Melanoma Cells | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Oleic Acid | Homovanillyl Alcohol | Hydroxytyrosol | Oleic Acid | Homovanillyl Alcohol | Hydroxytyrosol | |||||||
| Gene | 100 µM | 200 µM | 100 µM | 200 µM | 100 µM | 200 µM | 100 µM | 200 µM | 100 µM | 200 µM | 100 µM | 200 µM |
| SNAT1 | nss | nss | nss | nss | nss | p = 0.017 | Nss | nss | Nss | nss | nss | nss |
| SNAT2 | nss | nss | nss | nss | nss | nss | Nss | nss | Nss | nss | nss | nss |
| GLS1 | nss | nss | nss | nss | nss | nss | Nss | nss | Nss | nss | nss | nss |
| LDHA | nss | nss | nss | nss | nss | nss | p = 0.043 | nss | Nss | nss | p = 0.037 | p = 0.012 |
| LDHB | nss | nss | nss | nss | nss | nss | p = 0.039 | nss | nss | nss | nss | nss |
| LDHC | nss | nss | nss | nss | nss | nss | p = 0.042 | nss | nss | nss | nss | p = 0.042 |
| MCT1 | nss | nss | nss | nss | nss | nss | Nss | nss | nss | nss | nss | nss |
| MCT4 | nss | nss | nss | nss | nss | nss | Nss | nss | nss | nss | nss | nss |
| GLUL | nss | nss | nss | nss | nss | nss | Nss | nss | nss | nss | nss | nss |
| G6PD | nss | nss | nss | nss | nss | nss | Nss | nss | nss | nss | nss | nss |
| xCT | nss | nss | p = 0.047 | nss | nss | p = 0.009 | Nss | nss | nss | nss | nss | nss |
| EAAT3 | nss | nss | nss | nss | nss | p = 0.008 | Nss | nss | nss | nss | nss | nss |
nss—Not statistically significant. Green—genes upregulated. Red—genes downregulated.
On the other hand, homovanillyl alcohol at a concentration of 100 µM increased xCT expression in A375 cells (p = 0.047) (Table 1; Figure S1), which could be related to the efficient mechanisms of cell defense in reverting the oxidative stress as an indirect consequence of the treatment with this compound. The same was not observed in MNT1 cells.
Furthermore, the treatment with 200 µM hydroxytyrosol seemed to significantly increase SNAT1 expression (p = 0.017) and a trend towards an increase of SNAT2 and GLS1 expression was also verified in A375 cells (Table 1; Figure S1). In fact, 200 µM hydroxytyrosol treatment reduced A375 cell viability, which is consistent with the increased uptake of neutral amino acids as alternative energy sources to increase the energetic yield as a mechanism to overcome the harmful effects caused by this compound. Hence, the stress condition created by the treatment with this compound may increase the need for new energy sources to resist the toxicity caused by hydroxytyrosol treatment. Moreover, 200 µM hydroxytyrosol also induced xCT upregulation and EAAT3 downregulation (p = 0.009; p = 0.008, respectively). The increased xCT expression can have a pro-survival function under stress conditions, by promoting higher levels of cystine uptake and glutathione biosynthesis, as an attempt by A375 cells to protect themselves from the oxidative stress generated by hydroxytyrosol. Indeed, this result is in accordance with the cytotoxic effect observed in A375 cells after treatment with 200 µM hydroxytyrosol, showing that the cells are activating detoxification mechanisms to survive. Lastly, the treatment with 200 µM hydroxytyrosol significantly decreased LDHA and LDHC expression in MNT1 cells (p = 0.037; p = 0.012; p = 0.042) (Table 1; Figure S1) preventing the conversion of pyruvate into lactate and the opposite reaction, ultimately inhibiting glycolysis.
2.4. Effects of Oleic Acid, Homovanillyl Alcohol, and Hydroxytyrosol on the Activation of ERK and JNK Molecular Pathways in A375 and MNT1 Melanoma Cells
The previous results suggest that the glycolytic process of the selected melanoma cell models is significantly affected mainly by oleic acid and hydroxytyrosol treatments (Table 1). From the three types of MAPK pathways, ERK and JNK have been indicated as the main regulators of energy harvest through glycolysis in melanoma (Figure 2A) [31]. Indeed, these signaling cascades control distinct cellular functions such as cell proliferation, survival, differentiation, and senescence [32]. Particularly, in melanoma cells containing a BRAF mutation, it is thought that glycolysis is enhanced and oxidative metabolism suppressed, promoting resistance to energy stress through ERK activation [33]. To investigate if the differences found in cell viability after hydroxytyrosol treatment and in melanoma metabolism upon treatment with olive oil compounds could be associated with the differential activation of two families of MAPK pathways, ERK and JNK activation was evaluated by Western blot.
In basal conditions, differences in ERK and JNK pathway activation were observed between A375 and MNT1 cell lines. Higher levels of JNK phosphorylation were detected in A375, and increased ERK activation was verified in MNT1, reflected by its phosphorylation on residues required for the activity of this protein (Figure 3).
Figure 3.
Impact of (A) oleic acid, (B) homovanillyl alcohol, and (C) hydroxytyrosol at concentrations of 100 µM and 200 µM on ERK and JNK pathway activation in A375 and MNT1 cells. Protein expression was detected by Western blot after 48 h of exposure to the three olive oil compounds.
In addition, the treatment with 200 µM oleic acid induced a slight increase in JNK activation and a reduction in phosphorylated ERK expression in MNT1 cells (Figure 3A). Since our results suggest that this cell line is more dependent on ERK pathway activation, the treatment with this compound may alter the preferential survival pathway selected by these cells to overcome the microenvironmental changes caused. This trend was not observed in A375 cells. Similarly, a decrease in the levels of phosphorylated ERK was also detected in MNT1 cells after treatment with homovanillyl alcohol (Figure 3B). Overall, oleic acid and homovanillyl alcohol treatments suppressed ERK activation in MNT1 cells.
Finally, hydroxytyrosol treatment reduced the total expression of JNK protein, as well as the levels of phosphorylated ERK, in A375 cells. Similarly, in MNT1 cells, the levels of total JNK expression and phosphorylated ERK were also reduced.
3. Discussion
Various compounds present in olives and olive oil have been described as possessing antioxidant, anti-carcinogenic, anti-inflammatory, and neuro-protective properties [15,16]. As such, we sought to analyze the cytotoxic potential of three different olive oil compounds—oleic acid, homovanillyl alcohol (hydroxytyrosol metabolite), and hydroxytyrosol—on melanoma cell models, in order to clarify whether they could represent promising anti-cancer agents to be tested in pre-clinical melanoma models. From the three compounds tested, only hydroxytyrosol had a statistically significant cytotoxic effect on A375 cells, inhibiting their proliferative capability. MNT1 cells seem to be more resistant to the effect of this compound, although there is a tendency to a reduction in viability after treatment. The concentrations tested in this study were selected based on the available literature on the effect of these compounds in other types of cancer and also on the available data about plasma concentrations of oleic acid in a healthy population [28,29,30].
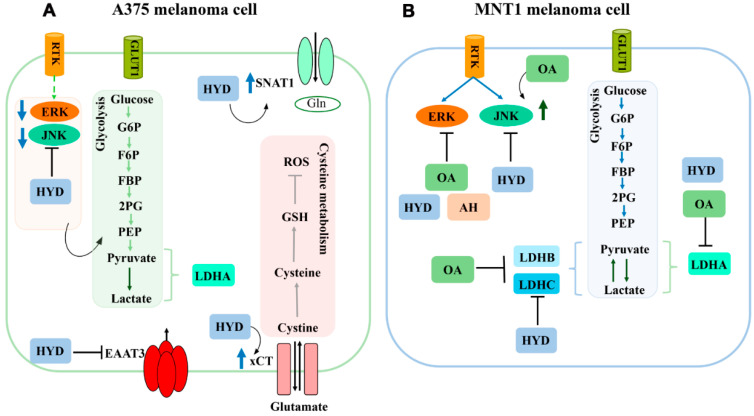
Considering the differences induced by hydroxytyrosol treatment in the viability of both melanoma cell models analyzed, we hypothesized that this effect could be mediated by the distinct molecular and metabolic mechanisms preferentially activated in each cell line. We found that both cell models used rely on distinct molecular and metabolic mechanisms, even in the absence of treatment. A375 cells seem to be more dependent on the JNK pathway and MNT1 cells may be more dependent on ERK activation to ensure cell survival and proliferation. In addition, MNT1 cells manifest a predominantly oxidative metabolism compared to A375 cells, as supported by LDHB and LDHC upregulation, and MCT4 downregulation. The differential effect caused by hydroxytyrosol could be mediated by the distinct molecular and metabolic pathways predominantly active in each cell line, which could lead to different responses after treatment with this compound. Indeed, hydroxytyrosol treatment led to SNAT1 and xCT upregulation, and to EAAT3 downregulation in A375 cells, while inducing only LDHA and LDHC downregulation in MNT1 cells (Figure 4). However, it also resulted in a decrease in total JNK as well as in ERK phosphorylation in both melanoma cell lines. By contrast, oleic acid and homovanillyl alcohol do not seem to affect the viability of either melanoma cell line. However, that does not exclude the possibility of these compounds being able to activate compensatory mechanisms to overcome the stress caused intracellularly, resisting cell death. Oleic acid treatment seems to enhance JNK phosphorylation and reduce ERK pathway activation in MNT1 cells, while also inhibiting LDHA, LDHB and LDHC expression and, consequently, the energy produced through glycolysis (Figure 4). In addition, the treatment with homovanillyl alcohol had a suppressive effect on phosphorylated ERK activation in MNT1 cells. Regarding A375 cells, homovanillyl alcohol increased xCT expression at a lower concentration.
Figure 4.
Schematic illustration summarizing the specific effects of oleic acid (OA), homovanillyl alcohol (HA), and hydroxytyrosol (HYD) on key metabolic pathways activated in A375 and MNT1 melanoma cell lines. (A) Hydroxytyrosol treatment seems to have a significant effect on A375 cells, reducing total JNK and phosphorylated ERK levels, and consequently decreasing the glycolytic rate via PKM2 inhibition. This compound also increased SNAT1 and xCT expression, probably in order to activate alternative mechanisms of energy production and detoxification in an attempt to resist the cytotoxic stimulus induced by hydroxytyrosol. EAAT3 downregulation could suggest that these cells are less dependent on the transport of l-glutamate, l-aspartate, and d-aspartate. (B) In MNT1 cells, hydroxytyrosol also reduced total JNK and phosphorylated ERK levels. In addition, homovanillyl alcohol and oleic acid decreased ERK phosphorylation. The glycolytic rate of this melanoma cell line was also affected by hydroxytyrosol and oleic acid treatments.
Presently there is evidence showing that hydroxytyrosol is an anticancer agent in various human cancers including colorectal, breast, thyroid, digestive, lung, brain, blood, and cervical cancers (reviewed in [34]). In fact, several studies have reported the anti-tumoral effect of hydroxytyrosol on different types of cancer, and the distinct anti-proliferative and pro-apoptotic mechanisms triggered in each cancer cell type (reviewed in [35]). In human breast cancer MCF-7 cells, hydroxytyrosol treatment reduced cell viability and proliferation, and promoted cell apoptosis [36]. In addition, in LNCaP prostate cancer cells, hydroxytyrosol inhibited cell proliferation in a concentration dependent manner (IC50 = 176 µM 48 h post treatment) through the suppression of Akt/STAT3 phosphorylation and by the cytoplasmic retention of NF-κB [37]. Nevertheless, hydroxytyrosol did not affect the viability of normal prostate epithelial cells, indicating a targeted effect against cancer cells [37].
In cutaneous melanoma cell lines, a dual role of hydroxytyrosol was previously reported when used in different concentrations (0–1000 µM) [19]. In lower concentrations (100–400 µM), this phenolic compound was photoprotective against ultraviolet radiation A, although in higher concentrations (600–1000 µM) it inhibited cell proliferation and activated caspase 3, consequently promoting cell apoptosis [19]. According to this study, hydroxytyrosol has a dual role in melanoma, based on the concentration administered, which is of utmost relevance since these compounds are present in cosmetics and functional foods. In our study, we did not address the range of concentrations tested by the previous authors. However, similarly to the aforementioned study, our results might corroborate a cytotoxic effect of this compound according to the mechanisms predominantly active in melanoma cells.
The distinct behavior of A375 and MNT1 cells after hydroxytyrosol treatment is consistent with the hypothesis that both melanoma cell lines rely on different predominant molecular and metabolic mechanisms to survive, which is also expected since A375 and MNT1 correspond to a primary [38] and metastatic [39] melanoma cell line, respectively. Previous studies postulate that metastatic melanoma cells differ from non-metastatic melanoma and normal melanocytes by preferentially showing higher levels of oxidative metabolism, fatty acid oxidation, and glutaminolysis [40,41,42]. Perhaps by increasing the oxidation of specific substrates, metastatic melanoma cells are able to acquire the spare energy they need to migrate and invade other tissues [41]. Indeed, MNT1 cells seem to maintain lactate in the intracellular environment, reducing its export by MCT4, certainly to be converted into pyruvate by LDHB and LDHC [43,44,45], which will then supply the TCA cycle and enhance the oxidative phosphorylation cascade [46,47]. These results are in accordance with the idea that a subset of melanomas rely extensively on oxidative phosphorylation to meet their bioenergetic needs, which could condition therapy response. Since most metastatic melanomas rely on a more oxidative metabolism, the study of targets involved in these metabolic pathways should be explored.
In addition, MNT1 cells seem to be less dependent on the exogenous supply of glutamine and are able to obtain this amino acid through glutamate conversion [48], which could explain the downregulation of SNAT1 and SNAT2, and GLUL upregulation. These metastatic cells also seem to direct glucose-6-phosphate to glycolysis instead of being used in the pentose phosphate pathway, which was previously described as an indicator of reduced melanoma aggressiveness [49]. Based on EAAT3 downregulation, MNT1 are also less dependent on the transport of l-glutamate, l-aspartate, and d-aspartate.
The decrease verified in total JNK as well as in ERK phosphorylation after hydroxytyrosol treatment in A375 and MNT1 cells could possibly have a negative impact on the glycolytic rate, since MAPK pathways are known to increase glycolytic activity though M2 pyruvate kinase (PKM2) activation [32,33,34]. In a condition of nutrient scarcity, melanoma cells try to acquire the available energy sources to maintain cell homeostasis and survival [50]. Consistently, A375 cells also take up glutamine more efficiently and activate detoxification pathways dependent on the xCT transporter, as was previously described for endometrial cancer [51], in an attempt to survive the deleterious effects of hydroxytyrosol treatment [52]. EAAT3 downregulation could be related to the difficulty of these cells in performing the antiport of cystine and glutamate under stress conditions. On the other hand, in MNT1 cells, this compound increased the levels of pyruvate being directed to the TCA cycle through LDHA downregulation. Possibly, the fact that MNT1 cells rely more on an oxidative metabolism might give them an advantage regarding hydroxytyrosol treatment, since LDHA downregulation will favor this metabolism, diminishing its cytotoxic effects.
Concerning oleic acid, a study reported that this compound did not influence the proliferative capability and melanogenesis of human melanocytes [21]. Furthermore, a previous study demonstrated that oleic acid was involved in protection against melanoma malignancy, modifying tumor microenvironment and reducing melanoma cell invasiveness [20]. Despite the reduced sampling used (n = 51), serum oleic acid was not associated with the risk of CM development [53]. In contrast to what was verified in melanoma, oleic acid was associated with cancer growth and metastasis through the activation of the ERK1/2 pathway in cervical cancer [54]. Perhaps the absence of an effect on melanoma cell viability of oleic acid treatment is due to compensatory and detoxifying mechanisms that are activated. In particular, different survival and metabolic pathways are selected and activated after the addition of this compound to MNT1 cells, as an attempt to overcome the microenvironmental alterations caused. These cells become more dependent on other energy sources such as glutamine to maintain the TCA cycle after oleic acid treatment. Accordingly, a previous study demonstrated that oleic acid can promote an adaptive response and enhance cell tolerance through its increased cellular antioxidative capacity via lipid peroxidation, which ultimately protects cells against oxidative stress-related injury [55]. In addition, it was already reported that the JNK pathway has a suppressive effect on ERK pathway activation, as an attempt to regulate cell apoptosis [56], which is coherent with our observation that oleic acid increases JNK activation while inhibiting ERK phosphorylation. The constant crosstalk between survival and proliferation pathways could be an alternative adaptation that allows resistance to the consequences of cellular stress.
Regarding homovanillyl alcohol, to our knowledge this is the first study exploring the impact of this hydroxytyrosol metabolite on the viability of two different melanoma cell lines. Based on the available literature, the impact of hydroxytyrosol in the context of cancer has been much more explored than the role that oleic acid and homovanillyl alcohol play under pathological conditions. However, no differences were verified in the viability of melanoma cells after homovanillyl alcohol treatment, perhaps meaning that other alternative survival and detoxification mechanisms dependent on xCT transporters are being activated. Under stress conditions, cells use different energy sources to resist and adapt to microenvironmental changes.
4. Materials and Methods
4.1. Cell Culture
Human melanoma cell lines A375 (malignant, ATCC CRL-1619) and MNT1 (metastatic, ATCC CRL-3450), both BRAF V600E mutated. A375 cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) without sodium pyruvate, supplemented with 10% fetal bovine serum (FBS), and 1% penicillin/streptomycin (all from Gibco; Thermo Fisher Scientific, Waltham, MA, USA). MNT1 cells were cultured in DMEM high glucose, supplemented with 10% FBS, 1% penicillin/streptomycin, 1% l-glutamine, and 1% non-essential amino acids (all from Gibco; Thermo Fisher Scientific, Waltham, MA, USA). Both cell lines were grown in a humidified incubator at 37 °C, 5% CO2 atmosphere.
4.2. Compounds
The exponentially growing melanoma cell lines were treated with 100 µM and 200 µM of three olive oil compounds, namely oleic acid (O1008, Sigma-Aldrich, Merck KGaA, Darmstadt, Germany), homovanillyl alcohol (148830, Sigma-Aldrich, Merck KGaA, Darmstadt, Germany), and hydroxytyrosol (4999 S, Extrasynthese, Genay, France). The concentrations used to treat A375 and MNT1 cells were selected based on the literature available about the effects of these compounds on different types of cancer. In addition, articles describing the concentrations of oleic acid in the plasma of healthy individuals were also considered to choose the concentrations to be used in this study [28,29,30]. Oleic acid was detected in a range of concentrations between 0.03 and 3.2 mmol/L (30 µM and 3200 µM) in plasma of a population of healthy young Canadian adults (n = 826) [30]. Stock solutions of 100 mM were prepared in MilliQ water for hydroxytyrosol, homovanillyl alcohol, and oleic acid.
4.3. Viability Assays
Cell counting kit-8 (CCK8) (Dojindo, Munich, Germany) was used to analyze cell viability 48 h post treatment with homovanillyl alcohol, oleic acid, and hydroxytyrosol. Cells were seeded in 24-well plates at a density of 1 × 105 cells/well. Cells treated with 5% dimethyl sulfoxide (DMSO) were used as a positive control of cell death. After 48 h, CCK8 solution was added to the wells in a dilution of 1:10 and cells were incubated for 30 min. Four independent assays were performed, and absorption was read at 450 nm using a microplate reader (BioRad, Hercules, CA, USA).
4.4. Quantitative Real Time Polymerase Chain Reaction (qRT-PCR)
Cells were seeded in 6-well plates at a density of 2.5 × 105 cells/well and after 24 h treated with 100 µM and 200 µM of three olive oil compounds. RNA was extracted from A375 and MNT1 cells 48 h post treatment with olive oil compounds using NZY Total RNA Isolation kit, following manufacturer instructions (Nzytech, Portugal). RNA quantification was assessed using a NanoDrop® 2000 Spectrophotometer (NanoDrop Technologies, Inc., Wilmington, DE, USA) and cDNA synthesis was performed using 1 µg of RNA, reversely transcribed by SuperScript III Reverse Transcriptase (RT) (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA) following manufacturer’s recommendations for a final reaction volume of 20 µL.
qRT-PCR reactions were carried out using SYBR Green master mix (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA) during 40 cycles in Lightcycler® 480 System instrument (Roche, Basel, Switzerland). The amplification program consisted of a holding stage (95 °C, 10 min), followed by amplification cycles (95 °C, 15 s and 60 °C, 1 min). The primers used for the expression analysis of sodium-coupled neutral amino acid transporter 1 and 2 (SNAT1 and SNAT2), glutaminase 1 (GLS1), glutamine synthetase (GLUL), lactate dehydrogenase A, B, and C (LDHA, LDHB and LDHC), monocarboxylate transporter 1 and 4 (MCT1 and MCT4), glucose-.6-phosphate dehydrogenase (G6PD), cystine-glutamate transporter (xCT) and excitatory amino acid transporter 3 (EAAT3) are listed in Table 2. Hypoxanthine-guanine phosphoribosyltransferase (HPRT1) and TATA-box binding protein (TBP) were selected as housekeeping genes (Table 1). Gene expression was evaluated by comparative CT method (ΔΔCT) [57] and each gene was normalized to the endogenous human reference housekeeping TBP and HPRT1 genes. Experiments were performed in biological and practical triplicates.
Table 2.
Primer sequences used for qRT-PCR.
| Gene | Primer Forward | Primer Reverse |
|---|---|---|
| SNAT1 | CATTCTATGACAACGTGCAGTCC | CAGCAACAATGACAGCCAGC |
| SNAT2 | CTGAGCAATGCGATTGTGGG | CTCCTTCATTGGCAGTCTTC |
| GLS1 | CTTCTACTTCCAGCTGTGCTC | CACCAGTAATTGGGCAGAAACC |
| GLUL | GAATGGTCTGAAGTACATCGAGG | GTTAGACGTCGGGCATTGTC |
| LDHA | CTTGCTCTTGTTGATGTCATC | CAGCCGTGATAATGACCAGC |
| LDHB | GAGCCTTCTCTCTCCTGTG | CTGATAGCACACGCCATACC |
| LDHC | GGATCTTCAGCATGGCAGTC | CTATTCTGGAGTTTGCAGATA |
| MCT1 | GCTGGGCAGTGGTAATTGGA | CAGTAATTGATTTGGGAAATGCAT |
| MCT4 | CACAAGTTCTCCAGTGC | CGCATCCAGGAGTTTGC |
| G6PD | GGCAACAGATACAAGAACGTGAAG | GCAGAAGACGTCCAGGATGAG |
| XCT | GGTCCTGTCACTATTTGGAGC | GAGGAGTTCCACCCAGACTC |
| EAAT3 | GTATCACGGCCACATCTGCC | GCAATGATCAGGGTGACATCC |
| TBP | GAGCTGTGATGTGAAGTTTCC | TCTGGGTTTGATCATTCTGTAG |
| HPRT1 | TGAGGATTTGGAAAGGGTGT | GAGCACACAGAGGGCTACAA |
4.5. Western Blot
A375 and MNT1 cells were seeded in T25 flasks at a density of 6.5 × 105 cells/flask and after 24 h these cells were treated with 100 µM and 200 µM of oleic acid, homovanillyl alcohol, and hydroxytyrosol. Cells collected 48 h post treatment with olive oil compounds were washed with phosphatase buffered saline and lysed for 1 h using ice-cold RIPA lysis buffer (Gibco, Thermo Fisher Scientific, Waltham, MA, USA) supplemented with a protease and phosphatase inhibitor cocktail (Sigma-Aldrich, Merck KGaA, Darmstadt, Germany). Protein concentration was determined using Pierce BCA protein assay kit (Thermo Fisher Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. Protein extracts (40 μg) were separated using 10% and 12% SDS-polyacrylamide gels and transferred onto PVDF membranes (BioRad, Hercules, CA, USA) with the Trans-Blot® Turbo TM Blotting system (BioRad, Hercules, CA, USA). Immunostaining was achieved using the following primary antibodies: anti-phospho-JNK (Thr183/Tyr185, Thr221/Tyr223) (1:500 dilution; 72 h incubation; 07-175, Merck KGaA, Darmstadt, Germany), anti-JNK/SAPK1 (1:165 dilution; overnight incubation; 06-748, Merck, Darmstadt, Germany), anti-phospho-ERK1/2 (pT202/pY204), clone AW39 (1:125 dilution; 72 h incubation; 612358, BD Biosciences, San Jose, CA, USA), anti-p44/42 MAPK (ERK1/2) (1:500 dilution; 72 h incubation; 168-10069, Raybiotech, Norcross, GA, USA), anti-α-tubulin, clone B-5-1-2 (1:4000 dilution; 1 h incubation; T5168, Merck KGaA, Darmstadt, Germany), and anti-β-actin, clone AC-15 (1:5000 dilution; 1 h incubation; A5441, Merck KGaA, Darmstadt, Germany). Primary antibodies were detected using horseradish peroxidase-conjugated secondary goat anti-rabbit and anti-mouse antibodies (1:5000 dilution; 1 h incubation; 31,460 and 31,430, ThermoFisher Scientific, Waltham, MA, USA), followed by enhanced chemiluminescence detection using Clarity Max Western ECL Substrate (BioRad, Hercules, CA, USA). Membranes were imaged by ChemiDoc XRS+ (BioRad, Hercules, CA, USA).
4.6. Statistical Analysis
The differences in the mean viability and gene expression of control cells and cells treated with oleic acid, homovanillyl alcohol, and hydroxytyrosol were assessed by employing Student’s t-tests. Sample data were represented as the mean ± standard deviation or the mean ± SEM for the metabolic viability results. All tests were two-sided, and we considered a significance level of 5%. Statistical analysis and graphic representation were performed using GraphPad Prism (version 5).
5. Conclusions
This study demonstrates that melanoma cells have a distinct response to natural olive oil compounds, which could be explained by a considerable metabolic and molecular heterogeneity. Here, we showed that oleic acid and homovanillyl alcohol are likely not a reliable therapeutic strategy in melanoma by themselves, because these compounds may facilitate the activation of compensatory mechanisms which increase cell detoxification and/or the dependence on an oxidative metabolism, essential for melanoma cells to resist to stress conditions. Hydroxytyrosol was the only compound to have a significant impact in melanoma cell viability, but this effect was only observed for the primary melanoma cell line. Future studies should be performed using other melanoma cell lines (primary and metastatic), in order to assess whether the impact of these three olive oil compounds is consistently influenced by the specific metabolic and molecular mechanisms predominantly activated in each cell line. Nevertheless, the present study corroborates the idea that hydroxytyrosol could represent a promising compound to be tested in pre-clinical melanoma models, mainly in melanoma tumors with a predominant glycolytic metabolism and preference for JNK pathway activation. Indeed, therapies focused on specific metabolic and molecular features of each melanoma subset could be more efficient since they will rely on distinct targets according to tumor characterization.
Acknowledgments
The authors thank Liga Portuguesa Contra o Cancro—Núcleo Regional do Sul and INTERFACE Programme (Innovation, Technology and Circular Economy Fund (FITEC). ATS also acknowledge Fundação para a Ciência e Tecnologia/Ministério da Educação e Ciência for the Individual Grant CEECIND/04801/2017.
Supplementary Materials
The following are available online, Figure S1—Effect of oleic acid, homovanillyl alcohol, and hydroxytyrosol (100 µM and 200 µM) treatment on SNAT1, SNAT2, GLS1, LDHA, LDHB, LDHC, MCT1, MCT4, GLUL, G6PD, EAAT3, and xCT mRNA expression in A375 and MNT1 cells after 48 h of exposure, by RT-qPCR analysis. Error bars represent the standard deviation of mean values obtained from triplicate experiments. Student’s t-test was used to compare each experimental condition with the respective untreated control * p < 0.05; ** p < 0.01.
Author Contributions
Conceptualization: M.P., M.R.B., and A.T.S.; methodology: C.B., A.T., A.T.S., and S.S.; investigation: C.B., A.T., S.S., M.R.B., A.T.S., and M.P.; data curation: C.B. and A.T.; writing—original draft preparation: C.B., A.T., and M.P.; writing—review and editing: M.P., M.R.B., S.S., and A.T.S.; supervision: M.P.; project administration: M.P.; funding acquisition: M.P., A.T.S., and M.R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by iNOVA4Health—UIDB/04462/2020, a program financially supported by Fundação para a Ciência e Tecnologia/Ministério da Educação e Ciência.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples used during the current study are available from the authors on reasonable request.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leonardi G.C., Falzone L., Salemi R., Zanghì A., Spandidos D.A., McCubrey J.A., Candido S., Libra M. Cutaneous melanoma: From pathogenesis to therapy (Review) Int. J. Oncol. 2018;52:1071–1080. doi: 10.3892/ijo.2018.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 3.Bandarchi B., Ma L., Navab R., Seth A., Rasty G. From Melanocyte to Metastatic Malignant Melanoma. Dermatol. Res. Pract. 2010;2010:583748. doi: 10.1155/2010/583748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Budczies J., von Winterfeld M., Klauschen F., Bockmayr M., Lennerz J.K., Denkert C., Wolf T., Warth A., Dietel M., Anagnostopoulos I., et al. The landscape of metastatic progression patterns across major human cancers. Oncotarget. 2015;6:570–583. doi: 10.18632/oncotarget.2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luís R., Brito C., Pojo M. Melanoma Metabolism: Cell Survival and Resistance to Therapy. In: Serpa J., editor. Tumor Microenvironment: The Main Driver of Metabolic Adaptation. Springer; Cham, Switzerland: 2020. pp. 203–223. [DOI] [PubMed] [Google Scholar]
- 6.Avagliano A., Fiume G., Pelagalli A., Sanità G., Ruocco M.R., Montagnani S., Arcucci A. Metabolic Plasticity of Melanoma Cells and Their Crosstalk with Tumor Microenvironment. Front. Oncol. 2020;10:722. doi: 10.3389/fonc.2020.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grimaldi A.M., Simeone E., Festino L., Vanella V., Strudel M., Ascierto P.A. MEK Inhibitors in the Treatment of Metastatic Melanoma and Solid Tumors. Am. J. Clin. Dermatol. 2017;18:745–754. doi: 10.1007/s40257-017-0292-y. [DOI] [PubMed] [Google Scholar]
- 8.Sosman J.A., Kim K.B., Schuchter L., Gonzalez R., Pavlick A.C., Weber J.S., McArthur G.A., Hutson T.E., Moschos S.J., Flaherty K.T., et al. Survival in BRAF V600–Mutant Advanced Melanoma Treated with Vemurafenib. N. Engl. J. Med. 2012;366:707–714. doi: 10.1056/NEJMoa1112302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luke J.J., Flaherty K.T., Ribas A., Long G.V. Targeted agents and immunotherapies: Optimizing outcomes in melanoma. Nat. Rev. Clin. Oncol. 2017;14:463–482. doi: 10.1038/nrclinonc.2017.43. [DOI] [PubMed] [Google Scholar]
- 10.Eroglu Z., Ribas A. Combination therapy with BRAF and MEK inhibitors for melanoma: Latest evidence and place in therapy. Ther. Adv. Med. Oncol. 2016;8:48–56. doi: 10.1177/1758834015616934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Domingues B., Lopes J., Soares P., Populo H. Melanoma treatment in review. ImmunoTargets Ther. 2018;7:35–49. doi: 10.2147/ITT.S134842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu C., Liu X., Yang J., Zhang M., Jin H., Ma X., Shi H. Combination of Immunotherapy with Targeted Therapy: Theory and Practice in Metastatic Melanoma. Front. Immunol. 2019;10:990. doi: 10.3389/fimmu.2019.00990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong D.J.L., Ribas A. Targeted Therapy for Melanoma. Cancer Res. 2016;79:251–262. doi: 10.1007/978-3-319-22539-5_10. [DOI] [PubMed] [Google Scholar]
- 14.Gide T.N., Wilmott J.S., Scolyer R.A., Long G.V. Primary and acquired resistance to immune checkpoint inhibitors in metastatic melanoma. Clin. Cancer Res. 2018;24:1260–1270. doi: 10.1158/1078-0432.CCR-17-2267. [DOI] [PubMed] [Google Scholar]
- 15.Gouvinhas I., Carbas B., Sobreira C., Domínguez-Perles R., Gomes S., Rosa E.A.S., Barros A.I.R.N.A. Critical Review on the Significance of Olive Phytochemicals in Plant Physiology and Human Health. Molecules. 2017;22:1986. doi: 10.3390/molecules22111986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Omar S.H. Cardioprotective and neuroprotective roles of oleuropein in olive. Saudi Pharm. J. 2010;18:111–121. doi: 10.1016/j.jsps.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konstantinidou V., Covas M.I., Sola R., Fitó M. Up-to date knowledge on the in vivo transcriptomic effect of the Mediterranean diet in humans. Mol. Nutr. Food Res. 2013;57:772–783. doi: 10.1002/mnfr.201200613. [DOI] [PubMed] [Google Scholar]
- 18.Aung T.N., Qu Z., Kortschak R.D., Adelson D.L. Understanding the effectiveness of natural compound mixtures in cancer through their molecular mode of action. Int. J. Mol. Sci. 2017;18:656. doi: 10.3390/ijms18030656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Angelo S., Ingrosso D., Migliardi V., Sorrentino A., Donnarumma G., Baroni A., Masella L., Tufano M.A., Zappia M., Galletti P. Hydroxytyrosol, a natural antioxidant from olive oil, prevents protein damage induced by long-wave ultraviolet radiation in melanoma cells. Free Radic. Biol. Med. 2005;38:908–919. doi: 10.1016/j.freeradbiomed.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 20.Bellenghi M., Puglisi R., Pedini F., De Feo A., Felicetti F., Bottero L., Sangaletti S., Errico M.C., Petrini M., Gesumundo C., et al. SCD5-induced oleic acid production reduces melanoma malignancy by intracellular retention of SPARC and cathepsin B. J. Pathol. 2015;236:315–325. doi: 10.1002/path.4535. [DOI] [PubMed] [Google Scholar]
- 21.Yamada H., Hakozaki M., Uemura A., Yamashita T. Effect of fatty acids on melanogenesis and tumor cell growth in melanoma cells. J. Lipid Res. 2019;60:1491–1502. doi: 10.1194/jlr.M090712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De La Torre R., Corella D., Castañer O., Martínez-González M.A., Pintó X., Vila J., Estruch R., Sorlí J.V., Arós F., Fiol M., et al. Protective effect of homovanillyl alcohol on cardiovascular disease and total mortality: Virgin olive oil, wine, and catechol-methylathion. Am. J. Clin. Nutr. 2017;105:1297–1304. doi: 10.3945/ajcn.116.145813. [DOI] [PubMed] [Google Scholar]
- 23.Rietjens S.J., Bast A., Haenen G.R.M.M. New Insights into Controversies on the Antioxidant Potential of the Olive Oil Antioxidant Hydroxytyrosol. J. Agric. Food Chem. 2007;55:7609–7614. doi: 10.1021/jf0706934. [DOI] [PubMed] [Google Scholar]
- 24.Deiana M., Incani A., Rosa A., Corona G., Atzeri A., Loru D., Melis M.P., Dessì M.A. Protective effect of hydroxytyrosol and its metabolite homovanillic alcohol on H2O2 induced lipid peroxidation in renal tubular epithelial cells. Food Chem. Toxicol. 2008;46:2984–2990. doi: 10.1016/j.fct.2008.05.037. [DOI] [PubMed] [Google Scholar]
- 25.Liotti A., Cosimato V., Mirra P., Calì G., Conza D., Secondo A., Luongo G., Terracciano D., Formisano P., Beguinot F., et al. Oleic acid promotes prostate cancer malignant phenotype via the G protein-coupled receptor FFA1/GPR40. J. Cell. Physiol. 2018;233:7367–7378. doi: 10.1002/jcp.26572. [DOI] [PubMed] [Google Scholar]
- 26.Calahorra J., Martínez-Lara E., Granadino-Roldán J.M., Martí J.M., Cañuelo A., Blanco S., Oliver F.J., Siles E. Crosstalk between hydroxytyrosol, a major olive oil phenol, and HIF-1 in MCF-7 breast cancer cells. Sci. Rep. 2020;10:6361. doi: 10.1038/s41598-020-63417-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Serreli G., Deiana M. Biological relevance of extra virgin olive oil polyphenols metabolites. Antioxidants. 2018;7:170. doi: 10.3390/antiox7120170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teubert A., Thome J., Büttner A., Richter J., Irmisch G. Elevated oleic acid serum concentrations in patients suffering from alcohol dependence. J. Mol. Psychiatry. 2013;1:13. doi: 10.1186/2049-9256-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nilsson A.K., Sjöbom U., Christenson K., Hellström A. Lipid profiling of suction blister fluid: Comparison of lipids in interstitial fluid and plasma. Lipids Health Dis. 2019;18:164. doi: 10.1186/s12944-019-1107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdelmagid S.A., Clarke S.E., Nielsen D.E., Badawi A., El-Sohemy A., Mutch D.M., Ma D.W.L. Comprehensive Profiling of Plasma Fatty Acid Concentrations in Young Healthy Canadian Adults. PLoS ONE. 2015;10:e0116195. doi: 10.1371/journal.pone.0116195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abildgaard C., Guldberg P. Molecular drivers of cellular metabolic reprogramming in melanoma. Trends Mol. Med. 2015;21:164–171. doi: 10.1016/j.molmed.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Meier F., Schittek B., Busch S., Garbe C., Smalley K., Satyamoorthy K., Li G., Herlyn M. The RAS/RAF/MEK/ERK and PI3K/AKT signaling pathways present molecular targets for the effective treatment of advanced melanoma. Front. Biosci. 2005;10:2986–3001. doi: 10.2741/1755. [DOI] [PubMed] [Google Scholar]
- 33.Papa S., Choy P.M., Bubici C. The ERK and JNK pathways in the regulation of metabolic reprogramming. Oncogene. 2019;38:2223–2240. doi: 10.1038/s41388-018-0582-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Imran M., Nadeem M., Gilani S.A., Khan S., Sajid M.W., Amir R.M. Antitumor Perspectives of Oleuropein and Its Metabolite Hydroxytyrosol: Recent Updates. J. Food Sci. 2018;83:1781–1791. doi: 10.1111/1750-3841.14198. [DOI] [PubMed] [Google Scholar]
- 35.Rigacci S., Stefani M. Nutraceutical properties of olive oil polyphenols. An itinerary from cultured cells through animal models to humans. Int. J. Mol. Sci. 2016;17:843. doi: 10.3390/ijms17060843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han J., Talorete T.P.N., Yamada P., Isoda H. Anti-proliferative and apoptotic effects of oleuropein and hydroxytyrosol on human breast cancer MCF-7 cells. Cytotechnology. 2009;59:45–53. doi: 10.1007/s10616-009-9191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zubair H., Bhardwaj A., Ahmad A., Srivastava S.K., Khan M.A., Patel G.K., Singh S., Singh A.P. Hydroxytyrosol Induces Apoptosis and Cell Cycle Arrest and Suppresses Multiple Oncogenic Signaling Pathways in Prostate Cancer Cells. Nutr. Cancer. 2017;69:932–942. doi: 10.1080/01635581.2017.1339818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giard D.J., Aaronson S.A., Todaro G.J., Arnstein P., Kersey J.H., Parks W.P. In vitro cultivation of human tumors: Establishment of cell lines derived from a series of solid tumors. J. Natl. Cancer Inst. 1973;51:1417–1423. doi: 10.1093/jnci/51.5.1417. [DOI] [PubMed] [Google Scholar]
- 39.Cuomo M., Nicotra M.R., Apollonj C., Fraioli R., Giacomini P., Natali P.G. Production and Characterization of the Murine Monoclonal Antibody 2G10 to a Human T4-Tyrosinase Epitope. J. Investig. Dermatol. 1991;96:446–451. doi: 10.1111/1523-1747.ep12470092. [DOI] [PubMed] [Google Scholar]
- 40.Fischer G.M., Gopal Y.N.V., Mcquade J.L., Peng W., Ralph J., Davies M.A. Metabolic Strategies of Melanoma Cells: Mechanisms, Interactions with the Tumor Microenvironment, and Therapeutic Implications. Pigment Cell Melanoma Res. 2018;31:11–30. doi: 10.1111/pcmr.12661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodrigues M.F., Obre E., De Melo F.H., Santos J.G.C., Galina A., Jasiulionis M.G., Rossignol R., Rumjanek F.D., Amoedo N.D. Enhanced OXPHOS, glutaminolysis and β-oxidation constitute the metastatic phenotype of melanoma cells. Biochem. J. 2016;473:703–715. doi: 10.1042/BJ20150645. [DOI] [PubMed] [Google Scholar]
- 42.De Moura M.B., Vincent G., Fayewicz S.L., Bateman N.W., Hood B.L., Sun M., Suhan J., Duensing S., Yin Y., Sander C., et al. Mitochondrial Respiration—An Important Therapeutic Target in Melanoma. PLoS ONE. 2012;7:e40690. doi: 10.1371/journal.pone.0040690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brisson L., Bański P., Sboarina M., Dethier C., Danhier P., Fontenille M.-J., Van Hée V.F., Vazeille T., Tardy M., Falces J., et al. Lactate Dehydrogenase B Controls Lysosome Activity and Autophagy in Cancer. Cancer Cell. 2016;30:418–431. doi: 10.1016/j.ccell.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 44.Draoui N., Feron O. Lactate shuttles at a glance: From physiological paradigms to anti-cancer treatments. DMM Dis. Model. Mech. 2011;4:727–732. doi: 10.1242/dmm.007724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Urbańska K., Orzechowski A. Unappreciated role of LDHA and LDHB to control apoptosis and autophagy in tumor cells. Int. J. Mol. Sci. 2019;20:2085. doi: 10.3390/ijms20092085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Doherty J.R., Cleveland J.L., Doherty J.R., Cleveland J.L. Targeting lactate metabolism for cancer therapeutics. J. Clin. Investig. 2013;123:3685–3692. doi: 10.1172/JCI69741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mishra D., Banerjee D. Lactate Dehydrogenases as Metabolic Links between Tumor and Stroma in the Tumor Microenvironment. Cancers. 2019;11:750. doi: 10.3390/cancers11060750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cluntun A.A., Lukey M.J., Cerione R.A., Locasale J.W. Glutamine Metabolism in Cancer: Understanding the Heterogeneity. Trends Cancer. 2017;3:169–180. doi: 10.1016/j.trecan.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang H.-C., Wu Y.-H., Yen W.-C., Liu H.-Y., Hwang T.-L., Stern A., Chiu D.T.-Y. The Redox Role of G6PD in Cell Growth, Cell Death, and Cancer. Cells. 2019;8:1055. doi: 10.3390/cells8091055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ratnikov B.I., Scott D.A., Osterman A.L., Smith J.W., Ronai Z.A. Metabolic rewiring in melanoma. Oncogene. 2017;36:147–157. doi: 10.1038/onc.2016.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marshall A.D., Van Geldermalsen M., Otte N.J., Lum T., Vellozzi M., Thoeng A., Pang A., Nagarajah R., Zhang B., Wang Q., et al. ASCT2 regulates glutamine uptake and cell growth in endometrial carcinoma. Oncogenesis. 2017;6:e367. doi: 10.1038/oncsis.2017.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koppula P., Zhang Y., Zhuang L., Gan B. Amino acid transporter SLC7A11/xCT at the crossroads of regulating redox homeostasis and nutrient dependency of cancer. Cancer Commun. 2018;38:12. doi: 10.1186/s40880-018-0288-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vinceti M., Malagoli C., Iacuzio L., Crespi C.M., Sieri S., Krogh V., Marmiroli S., Pellacani G., Venturelli E. Serum Fatty Acids and Risk of Cutaneous Melanoma: A Population-Based Case-Control Study. Dermatol. Res. Pract. 2013;2013:659394. doi: 10.1155/2013/659394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang P., Su C., Luo X., Zeng H., Zhao L., Wei L., Zhang X., Varghese Z., Moorhead J.F., Chen Y., et al. Dietary oleic acid-induced CD36 promotes cervical cancer cell growth and metastasis via up-regulation Src/ERK pathway. Cancer Lett. 2018;438:76–85. doi: 10.1016/j.canlet.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 55.Haeiwa H., Fujita T., Saitoh Y., Miwa N. Oleic acid promotes adaptability against oxidative stress in 3T3-L1 cells through lipohormesis. Mol. Cell Biochem. 2014;386:73–83. doi: 10.1007/s11010-013-1846-9. [DOI] [PubMed] [Google Scholar]
- 56.Junttila M.R., Li S., Westermarck J. Phosphatase-mediated crosstalk between MAPK signaling pathways in the regulation of cell survival. FASEB J. 2008;22:954–965. doi: 10.1096/fj.06-7859rev. [DOI] [PubMed] [Google Scholar]
- 57.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2-ΔΔCT method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.