Abstract
Background:
The most common cause of cauda equina compression in the elderly is lumbar spinal stenosis. Epidural lipomatosis is an additional known but rare cause of cauda equina compression readily diagnosed on MR studies. Notably, spinal canal decompression and direct excision of the epidural fat effectively manage this combined pathology.
Case Description:
A 70-year-old male presented with progressive truncal obesity associated with refractory lumbar neurogenic claudication. The lumbar magnetic resonance imaging (MRI) showed excessive epidural fat extending from L4 to S2 resulting in thecal sac compression; this was confirmed on the MRI myelogram study. Following a decompressive laminectomy, the patient’s cauda equina syndrome resolved.
Conclusion:
Recent weight gain with increased neurogenic claudication and the onset of a cauda equina syndrome may herald the presence of significant lumbar epidural lipomatosis. Here, laminectomy for excision of the excessive epidural fat resolved the patient’s symptomatic spinal stenosis.
Keywords: Cauda equina compression, Epidural fat, Low back pain, Neurogenic claudication

INTRODUCTION
Symptomatic cauda equina compression secondary to excessive epidural fat is occasionally seen in elderly patients and is readily documented on MR studies.[4,5] Obesity and male gender together increase the risk for such symptomatic epidural lipomatosis.[1,3,7] Here, we successfully managed a 70-year-old patient with cauda equina compression secondary to epidural lipomatosis with a decompressive laminectomy alone.
CASE REPORT
A 70-year-old male presented with 6 years of increased weight gain, progressive low back pain with bilateral radiculopathy, and the newer exacerbation of neurogenic claudication. On examination, he had marked truncal obesity (body mass index = 35 Kg/m2 and waist–hip ratio of 1), straight leg raising was limited to 50° bilaterally, motor function remained intact in both lower extremities (e.g., 5/5 bilaterally), bilateral Achilles responses were absent, and he exhibited no focal sensory deficit.
The lumbosacral magnetic resonance imaging (MRI) showed excessive epidural fat with significant thecal sac compression extending from L4 to S2; this was further confirmed on the MRI myelogram [Figure 1]. He underwent an L4 to S2 decompressive laminectomy at which time the epidural lipomatosis was excised [Figure 2]. Postoperatively, he had minimal residual symptoms 5 months later.
Figure 1:
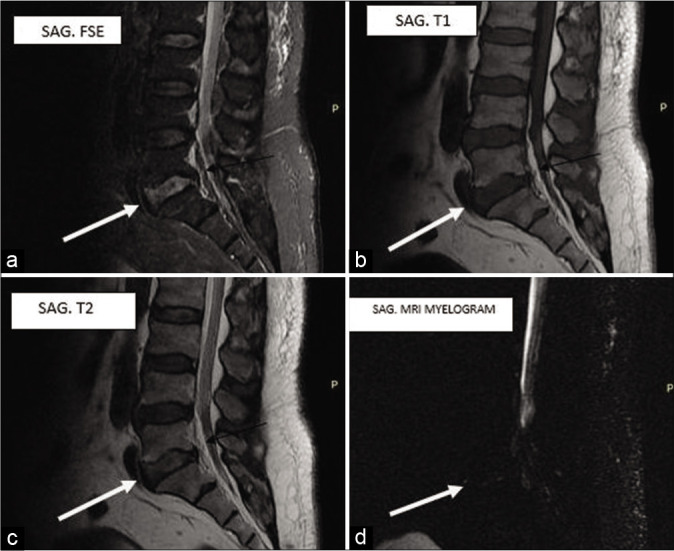
Lumbosacral spine magnetic resonance imaging (MRI) images; (a) sagittal FSE STIR, (b) sagittal T1 sequence, (c) sagittal T2 sequence, (d) sagittal MRI myelogram with thick white arrow pointing the L5/S1 intervertebral disc and thin black arrow pointing to the epidural fat.
Figure 2:
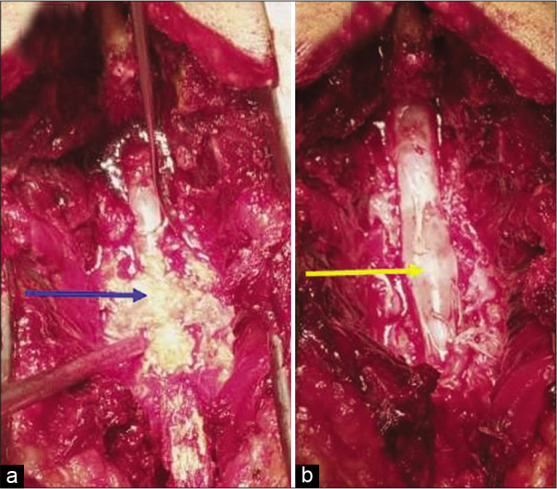
Intraoperative images; (a) blue arrow pointing to the excessive epidural fat after laminectomies, (b) yellow arrow pointing to intact dural sac after excision of the epidural fat.
DISCUSSION
In this case study, a 70-year-old male presented with the recent rapid onset of weight gain, lumbar radiculopathy and progressive neurogenic claudication.[4,7] Attempts at weight reduction and the management of low back pain failed to relieve his symptoms/signs; some studies, however, have shown that weight reduction may effectively manage symptomatic epidural lipomatosis.[2] Once the MR documented lumbar epidural lipomatosis with significant thecal sac compression L4–S2, the patient successfully underwent a decompressive laminectomy.[2,6]
Notably, in Zevgaridis et al. study, MRI readily documented the presence of epidural lipomatosis/lumbar thecal sac compression, making obtaining a myelo-CT study unnecessary.[8]
In the majority of cases, surgical excision of epidural lipomatosis in conjunction with decompressing lumbar spinal stenosis is the treatment of choice to relieve cauda equina compression.
CONCLUSION
Recent weight gain associated with lumbar stenosis and progressive neurogenic claudication attributed to MR documented epidural lipomatosis may be effectively relieved with a decompressive laminectomy.
Footnotes
How to cite this article: Okunlola AI, Orewole TO, Okunlola CK, Babalola OF, Akinmade A. Epidural lipomatosis in elderly patient: A rare cause of cauda equina compression. Surg Neurol Int 2021;12:7.
Contributor Information
Abiodun Idowu Okunlola, Email: okunlolaai@abuad.edu.ng.
Tesleem Olayinka Orewole, Email: drorewole@gmail.com.
Cecilia Kehinde Okunlola, Email: cecilia_okunlola@gmail.com.
Olakunle Fatai Babalola, Email: olakunlebabs@yahoo.com.
Akinola Akinmade, Email: drakinmade@abuad.edu.ng.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fogel GR, Cunningham PY, Esses SI. Spinal epidural lipomatosis: Case reports, literature review and meta-analysis. Spine J. 2005;5:202–11. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 2.Kim K, Mendelis J, Cho W. Spinal Epidural lipomatosis: A review of pathogenesis, characteristics, clinical presentation, and management. Global Spine J. 2019;9:658–65. doi: 10.1177/2192568218793617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malone JB, Bevan PJ, Lewis TJ, Nelson AD, Blaty DE, Kahan ME. Incidence of spinal epidural lipomatosis in patients with spinal stenosis. J Orthop. 2018;15:36–9. doi: 10.1016/j.jor.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park SK, Han JM, Lee K, Cho WJ, Oh JH, Choi YS. The clinical characteristics of spinal epidural lipomatosis in the lumbar spine. Anesth Pain Med. 2018;8:e83069. doi: 10.5812/aapm.83069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reina MA, Franco CD, López A, dé Andrés JA, van ZundertA. Clinical implications of epidural fat in the spinal canal. A scanning electron microscopic study. Acta Anaesthesiol Belg. 2009;60:7–17. [PubMed] [Google Scholar]
- 6.Walker MA, Younan Y, de la Houssaye C, Reimer N, Robertson DD, Umpierrez M, et al. Volumetric evaluation of lumbar epidural fat distribution in epidural lipomatosis and back pain in patients who are obese: Introducing a novel technique (Fat Finder algorithm) BMJ Open Diabetes Res Care. 2019;7:e000599. doi: 10.1136/bmjdrc-2018-000599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yasuda T, Suzuki K, Kawaguchi Y, Seki S, Makino H, Watanabe K, et al. Clinical and imaging characteristics in patients undergoing surgery for lumbar epidural lipomatosis. BMC Musculoskelet Disord. 2018;19:66. doi: 10.1186/s12891-018-1988-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zevgaridis D, Nanassis K, Zaramboukas T. Lumbar nerve root compression due to extradural, intraforaminal lipoma, An underdiagnosed entity? Case report. J Neurosurg Spine. 2008;9:408–10. doi: 10.3171/SPI.2008.9.11.408. [DOI] [PubMed] [Google Scholar]


