Abstract
Simple Summary
Multiple Myeloma (MM) is a hematologic malignancy caused by aberrant plasma cell proliferation in the bone marrow (BM) and constitutes the second most common hematological disease after non-Hodgkin lymphoma. The disease progression is drastically regulated by the immunosuppressive tumor microenvironment (TME) generated by soluble factors and different cells that naturally reside in the BM. This microenvironment does not remain unchanged and alterations favor cancer dissemination. Despite therapeutic advances over the past 15 years, MM remains incurable and therefore understanding the elements that control the TME in MM would allow better-targeted therapies to cure this disease. In this review, we discuss the main events and changes that occur in the BM milieu during MM development.
Abstract
Multiple myeloma (MM) is a hematologic cancer characterized by clonal proliferation of plasma cells in the bone marrow (BM). The progression, from the early stages of the disease as monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) to MM and occasionally extramedullary disease, is drastically affected by the tumor microenvironment (TME). Soluble factors and direct cell–cell interactions regulate MM plasma cell trafficking and homing to the BM niche. Mesenchymal stromal cells, osteoclasts, osteoblasts, myeloid and lymphoid cells present in the BM create a unique milieu that favors MM plasma cell immune evasion and promotes disease progression. Moreover, TME is implicated in malignant cell protection against anti-tumor therapy. This review describes the main cellular and non-cellular components located in the BM, which condition the immunosuppressive environment and lead the MM establishment and progression.
Keywords: multiple myeloma, tumor microenvironment, immunosuppression, adhesion molecules, migration, bone marrow niche
1. Introduction
Multiple Myeloma (MM) is a hematologic malignancy characterized by clonal proliferation of plasma cells in the bone marrow (BM) and constitutes the second most common hematological disease after non-Hodgkin lymphoma [1]. This illness normally evolves from premalignant states called monoclonal gammopathy of undetermined significance (MGUS), with or without intermediate stages as smoldering multiple myeloma (SMM) or solitary plasmacytoma, and eventually progresses to plasma cell leukemia or extramedullary myeloma [2]. The transition among the stages of the disease and its resistance to treatment are regulated by the BM microenvironment. Cellular and non-cellular components of MM BM niche contribute to the generation of an immunosuppressive tumor microenvironment (TME), which supports MM cell growth and survival. In this review, we update the mechanisms of myeloma cell trafficking and the involvement of BM mesenchymal stromal cells and the immune compartment in the establishment and exacerbation of the disease.
2. Myeloma Cell Trafficking
Different trafficking events of MM cells allow them to reach and colonize distinct BM niches, eventually recirculate, and finally egress from the BM during the extramedullary stages of the disease (Figure 1) [3,4]. Although it has not been completely elucidated, it is likely that normal plasma cells and MM cells use the BM sinusoids as an entry route into the BM, similarly to the hematopoietic stem cells (HSC) entry gates [5,6,7,8]. A main molecule mediating homing, lodging, and retention of both normal and malignant plasma cells into the BM is the chemokine receptor CXCR4, which interacts with CXCL12, a chemokine highly expressed in the BM microenvironment [3,4,5,8,9,10,11,12]. Notably, blocking CXCL12–CXCR4 interaction with the CXCR4 inhibitor plerixafor (AMD3100) disrupts MM cell contacts with the BM microenvironment [13], leading to MM cell mobilization into the circulation [14]. Among other signaling responses, the interaction of CXCL12 with CXCR4 on the surface of MM cells upregulates the activity of the α4β1 integrin, allowing high binding to its ligand VCAM-1 expressed on the BM microvasculature [15,16,17]. This adhesive event represents a key step in MM cell trafficking into the BM milieu and likely plays key roles during MM cell recirculation.
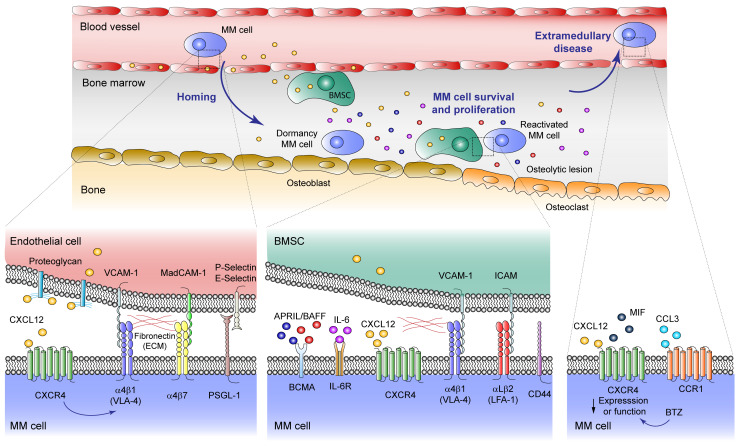
Figure 1.
Malignant plasma cell trafficking events in multiple myeloma (MM) development. MM plasma cells reach the bone marrow (BM) niche through sinusoids, proliferate favored by the tumor microenvironment (TME) and, occasionally, egress to the circulation causing extramedullary disease. Homing: The interaction of the CXCL12 chemokine with its CXCR4 receptor, mediates homing, lodging and retention of both normal and malignant plasma cells into the BM. CXCL12–CXCR4 interaction upregulates the activity of the α4β1 integrin, allowing high binding to its ligand VCAM-1 expressed on the BM microvasculature. Other important adhesion molecules mediating MM cell homing into the BM are the α4β7 integrin, a receptor for MAdCAM-1 and fibronectin, and PSGL-1 which interacts with P- and E-selectin expressed on the endothelial cell surface. MM cell survival and proliferation: Inside the BM milieu, BM mesenchymal stromal cells (BMSC) secrete high levels of CXCL12 that, along with α4β1, α4β7, and αLβ2 integrins, as well as CD44, are important for anchoring and retention of MM cells into BM niches. During this stage, survival and proliferation of malignant plasma cells is contributed by two main soluble mediators, a proliferation-inducing ligand (APRIL) and B-cell activating factor (BAFF), which bind B-cell maturation antigen (BCMA) in the cancer cell surface, and IL-6, whose receptor is also expressed on MM cells. In MM patients there is a pathological osteolineage imbalance with reduced osteoblasts in favor of osteoclasts which produce lytic lesions. BM osteoblastic niche facilitates the dormancy of MM cells, while osteoclasts induce MM cell reactivation. Extramedullary disease: In this context, cancer cells become independent from the TME, and CXCR4 function or expression is downregulated, an event that also occurs after bortezomib (BTZ) treatment. Macrophage migration inhibitory factor (MIF) can also bind to CXCR4, inducing the expression of adhesion molecules. Expression of CCR1 chemokine receptor is linked to MM plasma cell circulation.
Two other important adhesion molecules mediating MM cell homing into the BM are the α4β7 integrin, a receptor for MAdCAM-1 and fibronectin, and CD44 [18,19,20]. In addition, MM cell attachment to the BM microvasculature is also contributed by P- and E-selectin and their ligands. Thus, the P-selectin glycoprotein ligand-1 (PSGL-1) is expressed on the surface of MM cells [21,22], playing key roles in the very initial interactions of MM cells with BM endothelial cells [22], by facilitating malignant plasma cell rolling on P-selectin expressed by the microvasculature [16]. The involvement of E-selectin during MM cell homing to the BM has been demonstrated using inhibitors of sialyltransferase ST3Gal-6, an enzyme required for the generation of E-selectin ligands [23,24], and by E-selectin-blocking antibodies [16].
Once inside the BM milieu, the α4β1 integrin is also important for anchoring the MM cells to BM niches, and for retaining them in the BM TME [16,25,26,27,28]. α4β1-dependent MM cell attachment was early shown to contribute to MM progression in in vivo models [29,30]. Its interaction with both VCAM-1 and fibronectin present in the BM triggers MM cell signaling leading to stimulation of their growth involving interleukin-6 (IL-6) [25,31,32], and promoting cell adhesion-mediated drug resistance [33,34]. At this stage, MM cell attachment to the BM microenvironment is also facilitated by α4β7- and by CD44-dependent adhesion, overall contributing to the retention of MM cells in the BM [18,19,20,25,35].
The final phases in MM involve egress of myeloma cells from the BM to the bloodstream to colonize different organs, once they become independent from growth signals provided by the BM milieu, a condition named extramedullary disease [4]. Decreased CXCR4 expression and function represents a possible candidate event inducing a reduction in MM cell retention associated with egress from the BM. In line with this model, treatment of MM cells with the proteasome inhibitor bortezomib decreases CXCR4 expression, which might contribute to MM cell migration from the BM and promote extramedullary disease [36], an unwanted clinical response. Furthermore, macrophage migration inhibitory factor (MIF) is also capable of binding CXCR4 [37], and its silencing causes downregulation of MM cell adhesion to BM stroma and leads to extramedullary disease [38]. The chemokine receptor CCR1 is also expressed on MM cells [12,39], and its expression is associated with increased circulating MM cells [40]. Interestingly, its ligand CCL3 inhibited MM cell migration towards CXCL12 [40], raising the possibility that the CCL3–CCR1 axis might actively promote MM cell exit from the BM, possibly by competition with retention signals from the CXCR4–α4β1 interaction.
3. Bone Marrow Niche
3.1. Bone Marrow Niche and Stromal Cells
The BM harbors hematopoietic and non-hematopoietic cells, as well as non-cellular components such as extracellular matrix (ECM) proteins and soluble factors, which work together to maintain the HSC pool and its descendants, the lineage-committed hematopoietic progenitor cells (HPCs) [41,42,43]. The non-hematopoietic cell pool includes mesenchymal stem cells (MSC) and their descendant stromal cells, as well as endothelial cells and pericytes, adipocytes, osteolineage cells and osteoclasts, and sympathetic neurons with their associated Schwann cells. Two HSC niches supporting normal hematopoiesis, the vascular and the endosteal niches, contain different cellular types, express distinct soluble factors required for HSC maintenance, retention, and proliferation, and also include HPCs which can also regulate the HSC compartment [41,42,43]. Yet, as the endosteal region of the BM is highly vascularized, it is likely that some cell type overlap exists between the endosteal and vascular HSC niches. A large portion of HSC resides perivascularly mainly surrounding fenestrated sinusoidal blood vessels, which represent important sites of migration between blood and BM [42,44]. Several perivascularly-located BM mesenchymal stromal cell types have been identified, including CXCL12-abundant reticular (CAR) cells, leptin-receptor (LPR+) expressing cells, Nes-CreER, and NG2-CreER cells [45]. These cells provide key factors for HSC retention, maintenance and proliferation in defined niches, such as CXCL12 and SCF (also named c-kit ligand), both expressed by LPR+ perivascular stroma and by endothelial cells [41,42,45]. Furthermore, these mesenchymal stromal cells express adhesive molecular anchors for HSC, including α4β1 [46,47,48] and α5β1 integrin ligands [48,49,50], CD44 [48,51] and E-selectin [52,53]. Other soluble factors modulating but likely not required for HSC maintenance are bone morphogenetic proteins (BMP), IL-6, fibroblast growth factor (FGF) and Notch ligands [54,55,56,57,58,59], whereas transforming growth factor-β (TGF-β) induces HSC quiescence and self-renewal [60].
Other cell populations influencing the HSC niche include HSC descendants such as osteolineage cells, macrophages and megakaryocytes [41,42,45]. Moreover, BM skeletal stem cells (SSC) capable of generating colony-forming units-fibroblast (CFU-Fs) secrete HSC niche factors including angiopoietin 1, and Nestin+ BM stromal cells or those expressing SCF or CXCL12 are enriched for CFU-Fs and regulate the formation of HSC niches [61,62,63,64]. Macrophages control CXCL12 expression in the BM environment and induce HSC mobilization [65,66], whereas megakaryocytes have been shown to associate with HSC at sinusoids [67,68,69]. Whether HSC and their progeny occupy identical, distinct, or overlapping spatial locations in the BM is actively being investigated. As macrophages and megakaryocytes represent HSC niche constituents, it could be proposed that HSC and their descendants take up overlapping spaces and share key soluble factors for differentiation [43].
Two other elements controlling HSC function are the oxygen tension and the sympathetic nerves [41,42,43]. The HSC niche is highly hypoxic, causing stabilization of the hypoxia-inducible factor 1-α (HIF-1α), which transcriptionally activates the expression of CXCL12 and CXCR4, therefore indirectly contributing to HSC retention [70,71,72,73]. Besides being vascularized, the BM is highly innervated, especially next to arterioles [74]. Nerve fibers and non-myelinating associated Schwann cells are required for regeneration of hematopoiesis after chemotherapy [60,75], and are needed for regulation of the circadian clock that controls the daily mobilization of HSC into blood, likely by modulating CXCL12 supply from the niche BM mesenchymal stromal cells [76].
3.2. Bone Marrow Niches for Normal Plasma Cells
Plasma cells require extrinsic factors for their migration to and survival in the BM [5,8,77,78]. As mentioned above, BM mesenchymal stromal cells secrete high levels of CXCL12 [79,80,81], which is a critical factor for attracting and lodging CXCR4+ normal plasma cells in the BM [8,9,82]. Thus, plasma cells from chimeric mice reconstituted with CXCR4-deficient fetal liver cells failed to accumulate in the BM [9], and specific deletion of CXCR4 in mature B cells led to a severe reduction in plasma cells in the BM [10]. Notably, using CXCL12-GFP knock-in mice, Tokoyoda et al. demonstrated that plasma cells are in contact with processes extended from CAR cells [10], suggesting that these cells constitute a favorable niche for normal plasma cells. Whether other stromal cell types also expressing CXCL12 such as LPR+ cells, Nes-CreER or NG2-CreER cells represent lodging niches for plasma cells remains to be investigated.
Adhesion receptors provide plasma cell attachment to the BM microvasculature, as well as retention at appropriate niches. The Shp phosphatase activates the α4β1 integrin on plasma cells, stimulating their homing to the BM via cell attachment to VCAM-1 [83]. Blockade of the integrins α4β1 and αLβ2 (also called LFA-1) leads to a depletion of long-lived plasma cells from their BM niches [84,85]. The BM stromal cells that mediate the lodging of plasma cells via α4β1 are positive for the expression of VCAM-1 [10,86]. Fibronectin harbors a α4β1 binding motif called CS-1 [87], and it has also been shown to provide plasma cell attachment and survival in BM niches [88]. The αLβ2 ligands on the stromal cells which could facilitate plasma cell lodging are currently unknown.
Several soluble mediators are needed for plasma cell survival and proliferation at suitable BM niches, including IL-6, as well as the B-cell maturation antigen (BCMA) ligands: a proliferation-inducing ligand (APRIL) and B-cell activating factor (BAFF) [5,8,78]. Different cell types supply these factors to the plasma cells. Recently, IL-6 was found to be mainly produced by perivascular cells in the BM [89], but other mesenchymal stromal cells might also contribute to IL-6 expression, especially upon contact with plasma cells [84,90]. Both IL-6 and APRIL are also produced by eosinophils [91], which was suggested to be required for the maintenance of plasma cells in the BM niche. Yet, two other reports concluded that eosinophils were not needed for plasma cell survival in the BM [92,93]. Megakaryocytes are also a source of IL-6 and APRIL in the BM, and notably, megakaryocyte-deficient c-mpl mice display a reduction in plasma cell numbers [94], indicating that megakaryocytes are critical components of the plasma cell BM niche. The involvement of the BAFF–BCMA-dependent signaling on plasma cell survival has been suggested [95], but it remains to be formally demonstrated.
3.3. Bone Marrow Niches for Myeloma Cells
3.3.1. The Premetastatic Niche
The BM microenvironment not only regulates HSC and HPC homeostasis but can also promote the expansion of hematologic tumor cells [6,7]. The BM stromal cells and ECM components are essential for the establishment of premetastatic niches, which attract and maintain incoming tumor cells. Upon lodging, the malignant cells locally transform the BM niche phenotype through altered release of cytokines and growth factors, and by remodeling adhesion receptor-mediated cell–cell contacts, ultimately educating their own growth and survival at the expense of the rest of the cell community of the microenvironment [6,41].
The presence of genetic mutations in BM stromal cells has been proposed to generate a local BM region with selective growth pressure in favor of tumor cells, as was demonstrated during BM transplantation [41]. As an example, transplant studies in RARγ−/− mice displaying myeloproliferative syndromes revealed that this disease was non-hematopoietic cell-intrinsic instead of being hematopoietic cell-autonomous [96], which involved a TNF-α-triggered pro-inflammatory environment, and therefore suggesting the participation of the BM microenvironment in hematopoietic disorders. Another example is represented by activating mutations in PTPN11 in BM MSCs, which promote the development and progression of myelomonocytic leukemia [97]. In this case, secretion by BM MSCs of the chemokine CCL3 stimulated the recruitment of inflammatory monocytes, causing an increase in inflammation based on IL-1β activity, which favored the expansion of BM MSCs, osteoblasts, and fibroblasts [97]. Together, these data reveal that the induction by BM stromal cells of an inflammatory microenvironment contributes to malignant cell growth [6,7]. Whether premetastatic niches harboring MSCs with genetic alterations previous to MM cell lodging could predispose to the survival and expansion of MM cells remains an interesting possibility to be addressed.
Exosomes are intraluminal vesicles of the multivesicular bodies, which are formed by invagination and budding of the late endosomal membrane. They are released after the fusion of multivesicular bodies with the plasma membrane and differ from other extracellular vesicles by their small size (30–150 nm) [98,99]. Exosomes represent a source of local and long-distance transfer of molecular information that can reach cell components of the BM microenvironment, and which might alter their phenotype to foster a suitable premetastatic niche for expansion and drug resistance of arriving tumor cells [98,99]. These vesicles are released by all types of cells in the body, including MSCs, stromal, and endothelial cells, fibroblasts, osteoclasts, osteoblasts and immune cells [98,100]. Exosome cargo includes DNA, mRNAs and miRNAs, integrins, growth factors, signal transduction molecules, and metabolic enzymes [100]. Vascular disruption and leakiness, angiogenesis, suppression of immune responses, and alterations in the composition of the ECM represent common responses promoted by exosomes in the premetastatic niche [98]. In MM, it has been shown that MM cells alter BM-derived cells to secrete exosomes that generate a welcome and growth-supporting environment that stimulate the dissemination of the malignant plasma cells [101,102]. Furthermore, exosomes influence the migration of pre-osteoclasts as well as osteoclast differentiation, involving activation of CXCR4-dependent signaling that leads to upregulation of osteoclast markers [103]. As pointed out above, exosomes carry and deliver miRNAs to target cells. Roccaro et al. showed that the miRNA content in exosomes from MM-MSCs was different from that of normal MSCs, with a higher content of oncogenic proteins, cytokines, and adhesion molecules [101]. Moreover, they showed a reduction in miR-15a in MM-MSC exosomes compared to normal counterparts. In addition, it has been reported that exosomal miR-135b shed from hypoxic MM cells stimulates angiogenesis by targeting factor-inhibiting HIF-1 [104].
3.3.2. Finding the Right Niches
After the adhesive and migratory events controlling MM cell entrance into the BM microenvironment and trafficking inside the BM [16], malignant cells must find suitable niches, including premetastatic ones, for their survival, proliferation, and resistance to chemotherapy. Experimental evidence suggests that tumor cells compete with normal hematopoietic cells for niche occupancy [105,106,107], though they seem to become independent from niche control during disease progression. MM cells probably use identical cellular and extracellular components in the BM microenvironment as their normal plasma cell counterparts to look for and develop a favorable niche. A CXCL12-rich environment is a likely niche for attraction and retention of CXCR4+ MM cells. Notably, blockade of the CXCL12–CXCR4 interaction causes MM cell release to circulation [13,14]. Therefore, CXCL12-expressing mesenchymal stromal cells including CAR cells should be considered constituents of MM cell niches. In addition, similar to normal plasma cells, MM cells become anchored to BM niches where ligands for the α4β1 and α5β1 integrins, as well for CD44, are expressed [31,32].
Patients with MM have a pathological imbalance with depletion of osteoblasts in favor of proliferation and activation of bone-resorbing osteoclasts [31,108,109,110]. Like solid tumors displaying BM tropism [111], it has been proposed that the BM osteoblastic niche might facilitate the dormancy of MM cells, whereas the vascular niche could promote tumor cell proliferation in the BM [112]. Thus, it was recently shown that MM cells colonize and reside in the bone niche, in close proximity with osteoblasts [112]. This osteoblastic niche stimulates the survival of MM cells by triggering a dormant or quiescence state, which is turned off upon remodeling of the endosteal niche by osteoclasts, leading to reactivation of MM cells and their displacement from the niche [113,114]. Therefore, extrinsic factors remodeling the niche contribute to the release of these cells from dormancy and MM cell expansion.
Likely contributions to the suppression of osteoblastic activity in BM niches and to the induction of lytic bone lesions in MM patients include the deregulation of the Wnt and Notch signaling pathways, and the blockade of Runx2-dependent functions [115]. For instance, DKK1, an MSC-secreted Wnt pathway inhibitor and whose expression is elevated in BM from MM patients, binds to the LRP5/6 receptor, thus preventing Wnt signaling, and leading to β-catenin translocation to the nucleus and ultimately causing bone lesions [116,117,118]. Furthermore, Wnt5, an abundant growth factor in the BM of MM patients, binds to its receptor ROR2 and mediates MM cell interactions with BM stromal cells [119], and notably, ROR2 depletion leads to detachment of MM cells from their BM niche [120]. Interestingly, inhibition of Notch signaling leads to a reduction in CXCR4-dependent MM cell homing to and infiltration in the BM [121], and Dll1- and Jagged1-induced Notch activation accelerates MM disease by promoting MM cell proliferation [122,123]. With regard to Runx2, its osteoblastogenic activity is suppressed by MM cells, causing osteolysis [109,124]. This suppression is in part mediated by MM cell–osteoblast contacts dependent on α4β1–VCAM-1 interaction [29,124], and also by IL-7 [124].
3.3.3. Educating the BM Niche
Upon stabilization of the MM niche, malignant plasma cells reprogram the local BM microenvironment, either by direct contact with stromal, endothelial or osteolineage cells, or involving the stimulation of supportive cytokines for MM cells, and by facilitating immune evasion [6,7]. These responses provide further expansion signals for MM cells, which become gradually independent from initial normal niche support, leading to the generation of a favorable TME. Notably, MM-MSCs display distinct gene profiles from normal MSC counterparts [125,126]. Furthermore, as mentioned above, MM cells can now act at a distance to prepare further premetastatic niches for tumor dissemination in other bone regions, by releasing cytokines, growth factors, and exosomes that remodel the ECM at these new sites [32,98,101,127].
The direct contacts between MM cells and the surrounding stroma stimulate several signaling pathways such as PI3K/Akt, MAPK, Wnt and Notch, and the induction of NF-κB signaling, leading to upregulation of IL-6, VEGF, IGF-1 and GDF15 expression, as well as increased expression of anti-apoptotic proteins [25,31,32,108,128,129]. In addition to the non-hematopoietic cell components, the TME encompasses hematopoietic cells which might have anti-tumor functions such as T cells and NK cells, or tumor-promoting activity including macrophages, myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) [32,127,130,131,132]. The complex relationships between MM cells and the cellular components, exosomes, ECM and soluble factors of the TME, overall generate a permissive microenvironment favoring MM cell growth and disease progression. Excellent reviews specifically describing the role of non-hematopoietic cells in MM development and progression have been recently presented [32,127,133,134], and thus we are not discussing it in the present review.
4. Myeloid Cells Involved in MM Progression
4.1. Macrophages
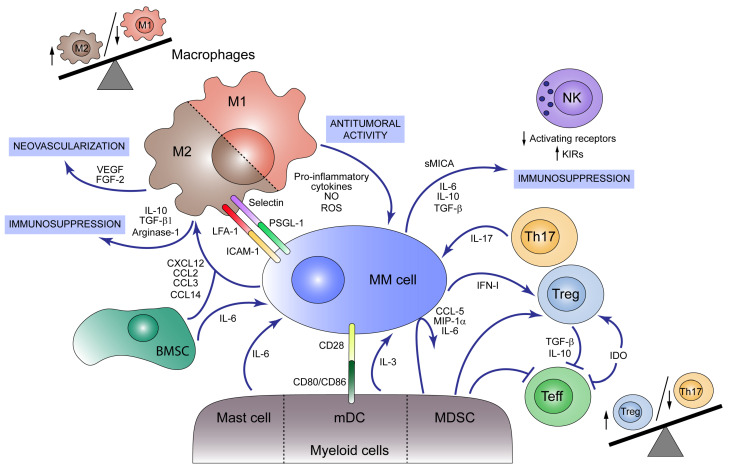
Macrophages are one of the main components of the tumor microenvironment in MM [135]. They are terminally differentiated myeloid cells derived from monocytic precursors and can be typically divided into two subgroups according to their functional role. The “classically activated” or M1 macrophages act as antitumoral agents by secreting pro-inflammatory cytokines, reactive oxygen species and nitric oxide while expressing high levels of MHC Class II. On the contrary, “alternatively activated” or M2 macrophages, in which tumor-associated macrophages (TAMs) are included, play an immunosuppressive role that facilitates tumor progression and are characterized by high expression levels of scavenging (CD163) and mannose (CD206) receptors, arginase and the production of IL-10, VEGF and matrix metalloproteinases (MMP). The M1/M2 polarization depends on the activation signaling present in the environment: Th1-derived cytokines such as interferon-γ (IFN-γ) and bacterial products, including bacterial lipopolysaccharides (LPS), promote M1 differentiation, whereas Th2-derived cytokines like IL-10 and glucocorticoid hormones drive the differentiation of macrophages towards an M2 phenotype [136,137]. In MM, it has been reported that both tumor cells and BM mesenchymal stromal cells produce chemokines such as CXCL12, CCL2, CCL3, and CCL14 that promote macrophage migration to the tumor niche and polarize macrophages towards an M2-like phenotype in vitro (Figure 2) [138,139,140]. Moreover, inhibition of the Jak1/2 pathway by Ruxolitinib or blockade of the colony-stimulating factor 1 receptor (CSF1R) seems to inhibit the differentiation of these pro-tumoral macrophages [139,141,142].
Figure 2.
Immunosuppressive tumor microenvironment (TME) in multiple myeloma (MM). Both myeloid and lymphoid cells present in bone marrow (BM) participate in MM development. M1 macrophages act as antitumoral agents producing pro-inflammatory cytokines, nitric oxide (NO) and reactive oxygen species (ROS) and acting as antigen-presenting cells (APC) that activate immune response against MM cells. MM cells and BM mesenchymal stromal cells (BMSCs) produce the chemokines CXCL12, CCL2, CCL3, and CCL14, which promote macrophage M2 polarization and migration to the tumor niche, unbalancing M1/M2 ratio towards the M2 population. M2 macrophages play a pro-tumoral role secreting immunosuppressive agents such as IL-10, TGF-β1 and Arginase-1 and neovascularization factors like VEGF and FGF-2. M2 macrophages act as MM cell protectors through the expression of selectins and LFA-1 in the macrophage surface, which binds to PSGL-1 and ICAM-1 in the plasma cell, respectively. Mast cells, although contributing to an initial tumoricidal host response, secrete IL-6 which promotes MM cell growth. Myeloid dendritic cells (mDCs) foster MM cell proliferation and survival by cell–cell interactions with tumor cells via CD80/CD86-CD28 and secretion of IL-3. Additionally, myeloid-derived suppressor cells (MDSCs) induce the secretion of cytokines such as CCL5, MIP-1α and IL-6 by MM cells and modulate the cytotoxic T cell responses inhibiting effector T cell functions and activating regulatory T cells (Treg). Other signals that promote Treg cell expansion are IFN-I, produced by MM cells, and indoleamine 2, 3-dioxygenase (IDO) activity which at the same time inhibits effector T cells. Cytokines produced by Tregs, such as IL-10 and TGF-β, together with other MM cell-derived signals attenuate effector T cell function. Th17 lymphocytes are also present in BM from MM patients and foster tumor growth through IL-17 secretion. NK cell cytotoxic activity is modulated during disease progression by cytokines and soluble factors (e.g., sMICA) secreted by MM cells that induce a reduction in activating receptors and an increase in inhibitory receptors (KIRs).
Several clinical studies associate high infiltration of M2 macrophages in BM from MM patients with poor prognosis and worse response to chemotherapy and autologous stem cell transplantation (ASCT), whereas patients with high infiltration of M1 macrophages showed better outcomes [139,143,144]. In fact, although M2 macrophages can be detected in BM from MM independently of the stage disease, the grade of infiltration and its correlation with poor prognosis is notable within relapsed MM patients compared to patients with MGUS or SMM [138,145]. In line with these data, some serum receptors such as soluble CD206 and CD163, as well as chemokines like CCL2 and MIF have been proposed as biomarkers for disease progression, prognosis and treatment response [38,146,147,148].
M2 macrophages play key roles in myeloma progression, and they are involved in the emergence of drug-resistant tumor cells. In vitro studies have shown that TAMs induce myeloma cell proliferation and protect them from chemotherapy-induced apoptosis [135,138,141,149,150]. Despite the positive outcomes obtained in MM patients with bortezomib treatment, results showed that this proteasome inhibitor also promotes the accumulation of pro-inflammatory macrophages and fosters MM cell survival and aggressiveness linked to MM disease progression, which could represent one of the mechanisms associated with MM resistance to bortezomib [151]. Moreover, depletion of macrophages or blockade of M2-polarization in murine MM models inhibits tumor growth and disease progression in vivo, and enhances survival after stem cell transplantation, providing strong evidence that macrophages are important for myeloma progression and a promising therapeutic target [142,152,153].
Understanding the mechanisms by which macrophages protect myeloma cells and support their survival will provide new targets for anti-MM therapies. The inhibition of the interaction between myeloma cells and macrophages via PSGL-1/selectins and intercellular adhesion molecule-1 (ICAM-1)/LFA-1 compromised macrophage-mediated protection in vitro, suggesting that cell–cell contact between surface proteins in MM cells and macrophages is important for macrophage-mediated protection of myeloma cells from chemotherapy-induced apoptosis [22,135,150]. Macrophages are also involved in neovascularization through vasculogenic mimicry [154]. VEGF and FGF-2 along with other pro-angiogenic factors promote macrophage recruitment and activation to mimic MM endothelial cells and collaborate with them in vessel formation [155,156]. Furthermore, it was shown that macrophages play a direct role in MM tumor cell homing and migration in vitro [153], while they inhibit T cell proliferation by generating an immunosuppressive environment that favors tumor development [138].
Nevertheless, macrophages can play an opposite role as tumoricidal agents. Infiltrating macrophages can act as antigen-presenting cells (APC) exposing myeloma antigens that activate Th1 CD4+ lymphocytes [142,157,158], which reciprocally induce macrophage differentiation to an M1-phenotype by an IFN-γ-dependent mechanism. These M1 macrophages induce myeloma tumor cell death by activation of the intrinsic apoptotic pathway [159], and secrete CXCL9 and CXCL10, two angiostatic chemokines that contribute to the control of tumor development [160]. However, some myeloma cells are able to modulate antigen secretion, leading to the escape from this immunosurveillance mechanism [161,162]. In this sense, macrophage reprogramming by granulocyte macrophage colony-stimulating factor (GM-CSF), added to the blockade of MIF could have a potential anti-myeloma therapeutic effect [163].
4.2. Myeloid-Derived Suppressor Cells
Apart from macrophages, some myeloid lineages present in the BM microenvironment play a key role in MM progression. Myeloid-derived suppressor cells (MDSCs), a heterogeneous group of immature cells and their precursors, which can be divided into granulocytic (G-MDSC) and monocytic (M-MDSC), are well-described in the niche of this tumor. Several groups have reported a significant increase in MDSCs in BM from MM patients compared to those from MGUS and healthy donors (HD) [164,165,166,167,168,169]. Likewise, the frequency of M-MDSCs correlates with the amount of M protein detected in serum, and a failure to achieve, at least, a very good partial response (VGPR) after treatment with lenalidomide [164]. By contrast, the use of this common drug in MM has other contradictory actions regarding MDSCs, such as the notable repression of MDSC induction from peripheral blood cells (PBMCs) [170], and the downregulation of programmed death-ligand1 (PD-L1) expression on this myeloid subtype [171]. MDSCs mightily take part in MM progression, as they can induce Treg differentiation [169,170], decrease in T cell proliferation [172], promote MM proliferation [173] and angiogenesis, and even differentiate themselves into functional osteoclasts [165,170]. All these actions could be caused by the MDSCs’ ability to take up MM exosomes through membrane fusion. These vesicles promote MDSC survival by activating STAT-3 and STAT-1 pathways, and by increasing the levels of anti-apoptotic proteins Bcl-xL and Mcl-1 [174,175]. Furthermore, some studies have revealed that MM cells secrete cytokines such as CCL5, MIP-1α [170] and large amounts of IL-6 when MDSCs are present [167,170,173], suggesting that not only do MDSCs contribute to MM progression by direct cell–cell contact or exosome intercellular communication, but also through cytokine secretion.
4.3. Other Myeloid Cells
Other myeloid cells such as dendritic cells (DCs), neutrophils, eosinophils, mast cells and platelets are involved in MM development in different ways.
Some studies have demonstrated that both myeloid DCs (mDCs) and plasmacytoid DCs (pDCs) accumulate in BM during the progression from MGUS to MM [176,177], but their functionality is impaired. pDCs from MM BM are incapable of triggering T-cell proliferation compared to pDCs from HD [177,178] and they can promote osteolysis through IL-3 secretion. This cytokine also stimulates pDCs survival and MM cell growth [177]. Migration and secretion of the cytokines IL12p70 and IFN-γ are significantly reduced in vitro in monocyte-derived DCs generated from MM patients. This impaired functionality could be caused by autocrine secretion of IL-6 and activation of the p38 MAPK pathway, both affecting CCR7-dependent migration [179]. Additionally, mDCs support MM proliferation and survival via engagement of CD80/CD86 receptors with their ligand CD28 expressed on MM cells [176].
Neutrophils have also been described to play a role in MM progression. High-density neutrophils (HDNs) present in MM BM exhibit different morphology and phenotype compared to those from HD [180,181]. Five genes (CSK, GSA, MEGF, PGM1, and PROK2), which are especially associated with MGUS-to-MM progression, have been reported to be up-regulated in HDNs from MM patients. Furthermore, these neutrophils show an impaired phagocytosis and oxidative burst in MM [180] while they are able to decrease T cell proliferation, suggesting an immunosuppressive effect of HDNs in the MM microenvironment. Surprisingly, only mature neutrophils, and not any other granulocytic subset, have a significant impact on progression-free survival (PFS) of MM patients [182].
The role of eosinophils in MM progression remains controversial. Although eosinophils have been found in close proximity to plasma cells within the BM [183] and they are known to secrete the soluble factors APRIL and IL-6 [91,92], which somehow could be involved in MM cell proliferation, it remains unclear whether their activity is relevant to BM plasma cells maintenance [91] or not [93,184].
Mast cells and platelets have been also described to have an impact on MM progression. Although mast cells accumulate in the BM to display tumoricidal activity as a host response, they also secrete other factors inducing MM growth, such as IL-6, promoting angiogenesis and participating, mainly indirectly, in MM bone disease [185]. Similarly, platelets are highly activated during MM progression, and their activation status correlates with disease progression from MGUS to SMM and MM [186].
5. Lymphoid Cells and Bone Marrow Niche for MM Exacerbation
In addition to the previously discussed subtypes of immune cells, T cell populations are altered in MM patients and switch along with the disease progression. A higher number of Th17 cells has been detected in peripheral blood (PB) and BM from MM patients, and although secreted IL-17 fosters tumor growth [187], an increased population of Th17 cells has been also described in Long-Term Survival (LTS)-MM patients [188]. In this study, Bryant et al. showed that the Treg/Th17 ratio increased in MM patients, but it was lower in LTS-MM subjects. Treg cells produce TGF-β and IL-10, cytokines essential to maintain self-tolerance as they repress effector T cell proliferation. However, an anomalous Treg proliferation or activity could result in immune dysfunction. The role of Tregs in MM has remained controversial and some authors assigned an important but not major role to Treg cells in the progression from MGUS to MM [189]. Nevertheless, analysis of BM-infiltrated T cell populations has detected a higher frequency of activated Tregs in untreated MM patients compared to HD, which was associated with a shorter PFS [190,191,192]. Myeloma-cell-secreted type 1 IFN has been suggested as a mediator of Treg activation and expansion in a syngeneic transplantable murine myeloma model, in which treatment with a blocking IFNAR1 antibody inhibited myeloma progression [193]. Moreover, APRIL, mainly secreted by myeloid cells and osteoclasts, induces proliferation and survival of Tregs in MM [167], and the increased activity found in MM patients of indoleamine 2,3-dioxygenase (IDO), an inducible enzyme that catalyzes tryptophan to kynurenine, led to inhibition of effector T cell function and induction of Treg differentiation [194]. A recently reported subpopulation of Treg CD38+ was found to be more immunosuppressive than Tregs CD38− and were decreased in patients treated with daratumumab suggesting an additional mechanism of action for this anti-CD38 antibody used to treat MM patients. [195].
Immune checkpoints have been described as tumor escape mechanisms in different types of cancer. PD-1 and PD-L1 are highly expressed in T cells and plasma cells of MM patients, respectively [196,197]. Furthermore, the expression levels of PD-L1 have been proposed as a prognosis predictor in newly diagnosed MM patients [198]. However, anti-PD-1 blockade therapy has shown limited clinical benefits in MM patients and serious adverse events have been reported in combination with immunomodulatory drugs (IMiDs) therapies [199,200]. The presence of expanded CD8+ T cell clones has been associated with good prognosis in MM. Suen et al. described that these lymphocytes express low levels of anergic or exhausted markers (LAG-3, Tim-3, PD-1, and CTLA-4) while displaying a senescent profile (KLRG-1+, CD57+, CD160+, and CD28−) [201]. In addition, high-dimensional single-cell RNA-sequencing (scRNA-Seq) and mass cytometry analysis unveiled that T cells in MGUS are enriched in stem-like memory profile whilst MM patients show higher lytic genes (e.g., Granzyme A) and senescence marker expression [202]. Notably, these results contrast with a study from Zelle-Rieser et al. describing both exhaustion and senescence T cell profiles in MM [203]. Additionally, other molecules such as carcinoembryonic antigen-related cell adhesion molecule-6 (CEACAM-6) expressed in MM plasma cells inhibit T cell activation and their cytotoxic response against MM cells [204].
One additional role has been described for T cells in the development of MM lytic bone lesion. Osteoclast differentiation and activation are induced by binding of the receptor activator of nuclear factor-κB (RANK) to its ligand (RANKL) expressed in stromal/osteoblastic cells and activated T lymphocytes. RANKL over-expression in T cells is induced by MM cells [205]. Cytokines such as IL-3 and IL-17 have also been associated with lytic bone lesions in MM [124,206]. In addition, CD4+ T cells from MM patients but not from MGUS subjects produce IL-3 [207], a cytokine with both osteoclastogenic and antiosteoblastic effects, and it was shown that IL-17 BM plasma levels correlate with the grade of bone disease [208].
Natural Killer (NK) cells play an important role in immune surveillance against viral infections and cancer. The NK response or tolerance against target cells depends on the balance between stimulatory and suppressive signals through their activating and inhibitory receptors. The reported proportion of NK cells in MM is controversial. Some data revealed a decreased population of NK cells in MM patients [209]. By contrast, other studies showed an increased number of NK cells in BM and PB of MM patient samples [210], although the NK cell cytotoxic activity is reduced and further decreases in advanced stages of this disease [211,212]. Reduction in activating receptors (NKG2D, DNAM-1, CD161) and increased expression of CD158a inhibitory Killer Immunoglobulin-like Receptor (KIR) has been described in NK cells from MM patients [213,214,215,216]. In addition, tumor growth in a murine model of MM induces dysregulation of CXCR3 and CXCR4/ligand expression, which results in a reduction in more functional KLRG1− NK cell subsets in bone marrow [217]. Moreover, NKT cells, an immune population that expresses both T cell and NK cell receptors, also present limited cytotoxic capacity in MM patients [218].
Apart from the aforementioned cytokines and chemokines that regulate MM disease, additional soluble components present in the BM milieu may also be involved in MM exacerbation. Extracellular adenosine (ADO) is an immunosuppressive metabolite whose levels in BM plasma correlate with disease progression in MM [219]. ADO hampers antitumoral immune response through the reduction in CD8+ and NK cell cytotoxic function and Th1 CD4+ T-cell response, while increasing the proportion of Treg cells [220,221,222,223]. Adenosine triphosphate (ATP), nicotinamide adenine dinucleotide (NAD+), and cyclic adenosine monophosphate (cAMP) can be metabolized by ectoenzymatic pathways to generate ADO. The canonical pathway starts from extracellular ATP and involves the ecto-nucleoside triphosphate diphosphohydrolase CD39 and the 5′-nucleotidase CD73 [224]. Furthermore, an alternative route entailing the NAD+-glycohydrolase CD38, the ecto-nucleotide pyrophosphatase/phosphodiesterase CD203a and CD73 has also been described [225]. CD39 is localized on the plasma membrane of regulatory T and B cells, and recent studies have also shown its expression in malignant plasma cells from MM patients [226]. Meanwhile, CD38 is expressed in T, B, NK and myeloid cells, and at higher levels in MM cells. Although the ectoenzymes from canonical and non-canonical pathways are present in the MM BM niche, some authors suggested that the hypoxic acidic environment might hinder CD39 enzymatic activity [224], and thus the implication of each pathway for ADO generation in MM has yet to be defined.
Another important factor is the soluble major histocompatibility complex class I-related chain A (MICA), liberated by shedding from the MM cell surface, which downregulates Natural Killer receptor group 2 member (NKG2D) expression in NK and T cells and is a prognostic factor for the overall survival (OS) and PFS of MM patients [227,228].
6. Conclusions
The BM microenvironment is essential for MM disease establishment and progression. MM plasma cell trafficking and homing to the BM are regulated by soluble factors, mainly chemokines such as CXCL12, as well as by direct cell–cell interactions through adhesion molecules expressed by plasma and bone marrow-resident cells. Once inside the BM niche, MM plasma cells transform the microenvironment through the secretion of cytokines and growth factors, which along with BM stromal cell activity induce additional mechanisms implicated in MM plasma cell retention, proliferation and drug resistance. Some patients develop extramedullary disease, caused by changes in chemokine receptor expression or function in plasma cells, and also by the MM plasma cell independency of survival factors from BM niche.
The immunosuppressive TME generated by deficient antigen presentation, effector cell dysfunction, proliferation of immunosuppressive cell populations, and high levels of immunosuppressive soluble factors allows the MM cell to escape from the immunosurveillance mechanisms. Targeting the molecular links between MM plasma cells and the bone marrow niche and restoring the homeostasis of the immune system should be crucial steps to cure myeloma disease.
Author Contributions
A.G.-O. and Y.R.-G. organized the content of manuscript, literature collection and writing; J.E., E.M.-M. and E.C. were involved in the literature collection and writing; J.T. and J.M.-L. were involved in the organization and proofreading of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Research Institute Hospital 12 de Octubre (i+12) and grants PI18/01519 from Instituto de Salud Carlos III (ISCIII) and from the CRIS foundation to J.M.-L.; and grant SAF2017-85146-R from Spanish Ministry of Science, Innovation and Universities to J.T. A.G.-O. is supported by a Fellowship from the Spanish Society of Hematology and Hemotherapy. J.E. is supported by a Fellowship from Instituto de Salud Carlos III (ISCIII) (IFI18/00034). E.M.-M. is supported by a Fellowship from Instituto de Salud Carlos III (ISCIII) (PI18/01519). E.C. is supported by a Fellowship from Spanish Ministry of Science, Innovation and Universities (FPU18/02963).
Conflicts of Interest
The authors declare no potential conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA A Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Kumar S.K., Rajkumar V., Kyle R.A., van Duin M., Sonneveld P., Mateos M.V., Gay F., Anderson K.C. Multiple myeloma. Nat. Rev. Dis. Primers. 2017;3:17046. doi: 10.1038/nrdp.2017.46. [DOI] [PubMed] [Google Scholar]
- 3.Redondo-Munoz J., Garcia-Pardo A., Teixido J. Molecular Players in Hematologic Tumor Cell Trafficking. Front Immunol. 2019;10:156. doi: 10.3389/fimmu.2019.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghobrial I.M. Myeloma as a model for the process of metastasis: Implications for therapy. Blood. 2012;120:20–30. doi: 10.1182/blood-2012-01-379024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu V.T., Berek C. The establishment of the plasma cell survival niche in the bone marrow. Immunol. Rev. 2013;251:177–188. doi: 10.1111/imr.12011. [DOI] [PubMed] [Google Scholar]
- 6.Méndez-Ferrer S., Bonnet D., Steensma D.P., Hasserjian R.P., Ghobrial I.M., Gribben J.G., Andreeff M., Krause D.S. Bone marrow niches in haematological malignancies. Nat. Rev. Cancer. 2020;20:285–298. doi: 10.1038/s41568-020-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghobrial I.M., Detappe A., Anderson K.C., Steensma D.P. The bone-marrow niche in MDS and MGUS: Implications for AML and MM. Nat. Rev. Clin. Oncol. 2018;15:219–233. doi: 10.1038/nrclinonc.2017.197. [DOI] [PubMed] [Google Scholar]
- 8.Lindquist R.L., Niesner R.A., Hauser A.E. In the Right Place, at the Right Time: Spatiotemporal Conditions Determining Plasma Cell Survival and Function. Front Immunol. 2019;10:788. doi: 10.3389/fimmu.2019.00788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hargreaves D.C., Hyman P.L., Lu T.T., Ngo V.N., Bidgol A., Suzuki G., Zou Y.R., Littman D.R., Cyster J.G. A coordinated change in chemokine responsiveness guides plasma cell movements. J. Exp. Med. 2001;194:45–56. doi: 10.1084/jem.194.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tokoyoda K., Egawa T., Sugiyama T., Choi B.I., Nagasawa T. Cellular niches controlling B lymphocyte behavior within bone marrow during development. Immunity. 2004;20:707–718. doi: 10.1016/j.immuni.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Nie Y., Waite J., Brewer F., Sunshine M.J., Littman D.R., Zou Y.R. The role of CXCR4 in maintaining peripheral B cell compartments and humoral immunity. J. Exp. Med. 2004;200:1145–1156. doi: 10.1084/jem.20041185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moller C., Stromberg T., Juremalm M., Nilsson K., Nilsson G. Expression and function of chemokine receptors in human multiple myeloma. Leukemia. 2003;17:203–210. doi: 10.1038/sj.leu.2402717. [DOI] [PubMed] [Google Scholar]
- 13.Alsayed Y., Ngo H., Runnels J., Leleu X., Singha U.K., Pitsillides C.M., Spencer J.A., Kimlinger T., Ghobrial J.M., Jia X., et al. Mechanisms of regulation of CXCR4/SDF-1 (CXCL12)-dependent migration and homing in multiple myeloma. Blood. 2007;109:2708–2717. doi: 10.1182/blood-2006-07-035857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azab A.K., Runnels J.M., Pitsillides C., Moreau A.S., Azab F., Leleu X., Jia X., Wright R., Ospina B., Carlson A.L., et al. CXCR4 inhibitor AMD3100 disrupts the interaction of multiple myeloma cells with the bone marrow microenvironment and enhances their sensitivity to therapy. Blood. 2009;113:4341–4351. doi: 10.1182/blood-2008-10-186668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanz-Rodriguez F., Hidalgo A., Teixido J. Chemokine stromal cell-derived factor-1alpha modulates VLA-4 integrin-mediated multiple myeloma cell adhesion to CS-1/fibronectin and VCAM-1. Blood. 2001;97:346–351. doi: 10.1182/blood.V97.2.346. [DOI] [PubMed] [Google Scholar]
- 16.Martinez-Moreno M., Leiva M., Aguilera-Montilla N., Sevilla-Movilla S., Isern de Val S., Arellano-Sanchez N., Gutierrez N.C., Maldonado R., Martinez-Lopez J., Buno I., et al. In vivo adhesion of malignant B cells to bone marrow microvasculature is regulated by alpha4beta1 cytoplasmic-binding proteins. Leukemia. 2016;30:861–872. doi: 10.1038/leu.2015.332. [DOI] [PubMed] [Google Scholar]
- 17.Wright N., de Lera T.L., Garcia-Moruja C., Lillo R., Garcia-Sanchez F., Caruz A., Teixido J. Transforming growth factor-beta1 down-regulates expression of chemokine stromal cell-derived factor-1: Functional consequences in cell migration and adhesion. Blood. 2003;102:1978–1984. doi: 10.1182/blood-2002-10-3190. [DOI] [PubMed] [Google Scholar]
- 18.Neri P., Ren L., Azab A.K., Brentnall M., Gratton K., Klimowicz A.C., Lin C., Duggan P., Tassone P., Mansoor A., et al. Integrin β7-mediated regulation of multiple myeloma cell adhesion, migration, and invasion. Blood. 2011;117:6202–6213. doi: 10.1182/blood-2010-06-292243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurt E.M., Wiestner A., Rosenwald A., Shaffer A.L., Campo E., Grogan T., Bergsagel P.L., Kuehl W.M., Staudt L.M. Overexpression of c-maf is a frequent oncogenic event in multiple myeloma that promotes proliferation and pathological interactions with bone marrow stroma. Cancer Cell. 2004;5:191–199. doi: 10.1016/S1535-6108(04)00019-4. [DOI] [PubMed] [Google Scholar]
- 20.Asosingh K., Gunthert U., De Raeve H., Van Riet I., Van Camp B., Vanderkerken K. A unique pathway in the homing of murine multiple myeloma cells: CD44v10 mediates binding to bone marrow endothelium. Cancer Res. 2001;61:2862–2865. [PubMed] [Google Scholar]
- 21.Snapp K.R., Ding H., Atkins K., Warnke R., Luscinskas F.W., Kansas G.S. A novel P-selectin glycoprotein ligand-1 monoclonal antibody recognizes an epitope within the tyrosine sulfate motif of human PSGL-1 and blocks recognition of both P- and L-selectin. Blood. 1998;91:154–164. doi: 10.1182/blood.V91.1.154. [DOI] [PubMed] [Google Scholar]
- 22.Azab A.K., Quang P., Azab F., Pitsillides C., Thompson B., Chonghaile T., Patton J.T., Maiso P., Monrose V., Sacco A., et al. P-selectin glycoprotein ligand regulates the interaction of multiple myeloma cells with the bone marrow microenvironment. Blood. 2012;119:1468–1478. doi: 10.1182/blood-2011-07-368050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glavey S.V., Manier S., Natoni A., Sacco A., Moschetta M., Reagan M.R., Murillo L.S., Sahin I., Wu P., Mishima Y., et al. The sialyltransferase ST3GAL6 influences homing and survival in multiple myeloma. Blood. 2014;124:1765–1776. doi: 10.1182/blood-2014-03-560862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Natoni A., Farrell M.L., Harris S., Falank C., Kirkham-McCarthy L., Macauley M.S., Reagan M.R., O’Dwyer M. Sialyltransferase inhibition leads to inhibition of tumor cell interactions with E-selectin, VCAM1, and MADCAM1, and improves survival in a human multiple myeloma mouse model. Haematologica. 2020;105:457–467. doi: 10.3324/haematol.2018.212266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lokhorst H.M., Lamme T., de Smet M., Klein S., de Weger R.A., van Oers R., Bloem A.C. Primary tumor cells of myeloma patients induce interleukin-6 secretion in long-term bone marrow cultures. Blood. 1994;84:2269–2277. doi: 10.1182/blood.V84.7.2269.2269. [DOI] [PubMed] [Google Scholar]
- 26.Sanz-Rodriguez F., Ruiz-Velasco N., Pascual-Salcedo D., Teixido J. Characterization of VLA-4-dependent myeloma cell adhesion to fibronectin and VCAM-1. Br. J. Haematol. 1999;107:825–834. doi: 10.1046/j.1365-2141.1999.01762.x. [DOI] [PubMed] [Google Scholar]
- 27.Michigami T., Shimizu N., Williams P.J., Niewolna M., Dallas S.L., Mundy G.R., Yoneda T. Cell-cell contact between marrow stromal cells and myeloma cells via VCAM-1 and alpha(4)beta(1)-integrin enhances production of osteoclast-stimulating activity. Blood. 2000;96:1953–1960. doi: 10.1182/blood.V96.5.1953. [DOI] [PubMed] [Google Scholar]
- 28.Podar K., Zimmerhackl A., Fulciniti M., Tonon G., Hainz U., Tai Y.T., Vallet S., Halama N., Jager D., Olson D.L., et al. The selective adhesion molecule inhibitor Natalizumab decreases multiple myeloma cell growth in the bone marrow microenvironment: Therapeutic implications. Br. J. Haematol. 2011;155:438–448. doi: 10.1111/j.1365-2141.2011.08864.x. [DOI] [PubMed] [Google Scholar]
- 29.Mori Y., Shimizu N., Dallas M., Niewolna M., Story B., Williams P.J., Mundy G.R., Yoneda T. Anti-alpha4 integrin antibody suppresses the development of multiple myeloma and associated osteoclastic osteolysis. Blood. 2004;104:2149–2154. doi: 10.1182/blood-2004-01-0236. [DOI] [PubMed] [Google Scholar]
- 30.Olson D.L., Burkly L.C., Leone D.R., Dolinski B.M., Lobb R.R. Anti-alpha4 integrin monoclonal antibody inhibits multiple myeloma growth in a murine model. Mol. Cancer Ther. 2005;4:91–99. [PubMed] [Google Scholar]
- 31.Anderson K.C., Carrasco R.D. Pathogenesis of myeloma. Annu. Rev. Pathol. 2011;6:249–274. doi: 10.1146/annurev-pathol-011110-130249. [DOI] [PubMed] [Google Scholar]
- 32.Bianchi G., Munshi N.C. Pathogenesis beyond the cancer clone(s) in multiple myeloma. Blood. 2015;125:3049–3058. doi: 10.1182/blood-2014-11-568881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Damiano J.S., Cress A.E., Hazlehurst L.A., Shtil A.A., Dalton W.S. Cell adhesion mediated drug resistance (CAM-DR): Role of integrins and resistance to apoptosis in human myeloma cell lines. Blood. 1999;93:1658–1667. doi: 10.1182/blood.V93.5.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noborio-Hatano K., Kikuchi J., Takatoku M., Shimizu R., Wada T., Ueda M., Nobuyoshi M., Oh I., Sato K., Suzuki T., et al. Bortezomib overcomes cell-adhesion-mediated drug resistance through downregulation of VLA-4 expression in multiple myeloma. Oncogene. 2009;28:231–242. doi: 10.1038/onc.2008.385. [DOI] [PubMed] [Google Scholar]
- 35.Garcés J.J., Simicek M., Vicari M., Brozova L., Burgos L., Bezdekova R., Alignani D., Calasanz M.J., Growkova K., Goicoechea I., et al. Transcriptional profiling of circulating tumor cells in multiple myeloma: A new model to understand disease dissemination. Leukemia. 2020;34:589–603. doi: 10.1038/s41375-019-0588-4. [DOI] [PubMed] [Google Scholar]
- 36.Stessman H.A., Mansoor A., Zhan F., Janz S., Linden M.A., Baughn L.B., Van Ness B. Reduced CXCR4 expression is associated with extramedullary disease in a mouse model of myeloma and predicts poor survival in multiple myeloma patients treated with bortezomib. Leukemia. 2013;27:2075–2077. doi: 10.1038/leu.2013.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tarnowski M., Grymula K., Liu R., Tarnowska J., Drukala J., Ratajczak J., Mitchell R.A., Ratajczak M.Z., Kucia M. Macrophage migration inhibitory factor is secreted by rhabdomyosarcoma cells, modulates tumor metastasis by binding to CXCR4 and CXCR7 receptors and inhibits recruitment of cancer-associated fibroblasts. Mol. Cancer Res. 2010;8:1328–1343. doi: 10.1158/1541-7786.MCR-10-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zheng Y., Wang Q., Li T., Qian J., Lu Y., Li Y., Bi E., Reu F., Qin Y., Drazba J., et al. Role of Myeloma-Derived MIF in Myeloma Cell Adhesion to Bone Marrow and Chemotherapy Response. J. Natl. Cancer Inst. 2016;108 doi: 10.1093/jnci/djw131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vande Broek I., Leleu X., Schots R., Facon T., Vanderkerken K., Van Camp B., Van Riet I. Clinical significance of chemokine receptor (CCR1, CCR2 and CXCR4) expression in human myeloma cells: The association with disease activity and survival. Haematologica. 2006;91:200–206. [PubMed] [Google Scholar]
- 40.Vandyke K., Zeissig M.N., Hewett D.R., Martin S.K., Mrozik K.M., Cheong C.M., Diamond P., To L.B., Gronthos S., Peet D.J., et al. HIF-2alpha Promotes Dissemination of Plasma Cells in Multiple Myeloma by Regulating CXCL12/CXCR4 and CCR1. Cancer Res. 2017;77:5452–5463. doi: 10.1158/0008-5472.CAN-17-0115. [DOI] [PubMed] [Google Scholar]
- 41.Hoggatt J., Kfoury Y., Scadden D.T. Hematopoietic Stem Cell Niche in Health and Disease. Annu. Rev. Pathol. 2016;11:555–581. doi: 10.1146/annurev-pathol-012615-044414. [DOI] [PubMed] [Google Scholar]
- 42.Crane G.M., Jeffery E., Morrison S.J. Adult haematopoietic stem cell niches. Nat. Rev. Immunol. 2017;17:573–590. doi: 10.1038/nri.2017.53. [DOI] [PubMed] [Google Scholar]
- 43.Wei Q., Frenette P.S. Niches for Hematopoietic Stem Cells and Their Progeny. Immunity. 2018;48:632–648. doi: 10.1016/j.immuni.2018.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kiel M.J., Yilmaz O.H., Iwashita T., Terhorst C., Morrison S.J. SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell. 2005;121:1109–1121. doi: 10.1016/j.cell.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 45.Pinho S., Frenette P.S. Haematopoietic stem cell activity and interactions with the niche. Nat. Rev. Mol. Cell. Biol. 2019;20:303–320. doi: 10.1038/s41580-019-0103-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Teixidó J., Hemler M.E., Greenberger J.S., Anklesaria P. Role of beta 1 and beta 2 integrins in the adhesion of human CD34hi stem cells to bone marrow stroma. J. Clin. Investig. 1992;90:358–367. doi: 10.1172/JCI115870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Simmons P.J., Masinovsky B., Longenecker B.M., Berenson R., Torok-Storb B., Gallatin W.M. Vascular cell adhesion molecule-1 expressed by bone marrow stromal cells mediates the binding of hematopoietic progenitor cells. Blood. 1992;80:388–395. doi: 10.1182/blood.V80.2.388.bloodjournal802388. [DOI] [PubMed] [Google Scholar]
- 48.Vermeulen M., Le Pesteur F., Gagnerault M.C., Mary J.Y., Sainteny F., Lepault F. Role of adhesion molecules in the homing and mobilization of murine hematopoietic stem and progenitor cells. Blood. 1998;92:894–900. doi: 10.1182/blood.V92.3.894. [DOI] [PubMed] [Google Scholar]
- 49.Lévesque J.P., Leavesley D.I., Niutta S., Vadas M., Simmons P.J. Cytokines increase human hemopoietic cell adhesiveness by activation of very late antigen (VLA)-4 and VLA-5 integrins. J. Exp. Med. 1995;181:1805–1815. doi: 10.1084/jem.181.5.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peled A., Kollet O., Ponomaryov T., Petit I., Franitza S., Grabovsky V., Slav M.M., Nagler A., Lider O., Alon R., et al. The chemokine SDF-1 activates the integrins LFA-1, VLA-4, and VLA-5 on immature human CD34(+) cells: Role in transendothelial/stromal migration and engraftment of NOD/SCID mice. Blood. 2000;95:3289–3296. doi: 10.1182/blood.V95.11.3289. [DOI] [PubMed] [Google Scholar]
- 51.Schmits R., Filmus J., Gerwin N., Senaldi G., Kiefer F., Kundig T., Wakeham A., Shahinian A., Catzavelos C., Rak J., et al. CD44 regulates hematopoietic progenitor distribution, granuloma formation, and tumorigenicity. Blood. 1997;90:2217–2233. doi: 10.1182/blood.V90.6.2217. [DOI] [PubMed] [Google Scholar]
- 52.Frenette P.S., Subbarao S., Mazo I.B., von Andrian U.H., Wagner D.D. Endothelial selectins and vascular cell adhesion molecule-1 promote hematopoietic progenitor homing to bone marrow. Proc. Natl. Acad. Sci. USA. 1998;95:14423–14428. doi: 10.1073/pnas.95.24.14423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Katayama Y., Hidalgo A., Furie B.C., Vestweber D., Furie B., Frenette P.S. PSGL-1 participates in E-selectin-mediated progenitor homing to bone marrow: Evidence for cooperation between E-selectin ligands and alpha4 integrin. Blood. 2003;102:2060–2067. doi: 10.1182/blood-2003-04-1212. [DOI] [PubMed] [Google Scholar]
- 54.Singbrant S., Karlsson G., Ehinger M., Olsson K., Jaako P., Miharada K., Stadtfeld M., Graf T., Karlsson S. Canonical BMP signaling is dispensable for hematopoietic stem cell function in both adult and fetal liver hematopoiesis, but essential to preserve colon architecture. Blood. 2010;115:4689–4698. doi: 10.1182/blood-2009-05-220988. [DOI] [PubMed] [Google Scholar]
- 55.Bernad A., Kopf M., Kulbacki R., Weich N., Koehler G., Gutierrez-Ramos J.C. Interleukin-6 is required in vivo for the regulation of stem cells and committed progenitors of the hematopoietic system. Immunity. 1994;1:725–731. doi: 10.1016/S1074-7613(94)80014-6. [DOI] [PubMed] [Google Scholar]
- 56.Zhao M., Ross J.T., Itkin T., Perry J.M., Venkatraman A., Haug J.S., Hembree M.J., Deng C.X., Lapidot T., He X.C., et al. FGF signaling facilitates postinjury recovery of mouse hematopoietic system. Blood. 2012;120:1831–1842. doi: 10.1182/blood-2011-11-393991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karanu F.N., Murdoch B., Gallacher L., Wu D.M., Koremoto M., Sakano S., Bhatia M. The notch ligand jagged-1 represents a novel growth factor of human hematopoietic stem cells. J. Exp. Med. 2000;192:1365–1372. doi: 10.1084/jem.192.9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stier S., Cheng T., Dombkowski D., Carlesso N., Scadden D.T. Notch1 activation increases hematopoietic stem cell self-renewal in vivo and favors lymphoid over myeloid lineage outcome. Blood. 2002;99:2369–2378. doi: 10.1182/blood.V99.7.2369. [DOI] [PubMed] [Google Scholar]
- 59.Maillard I., Koch U., Dumortier A., Shestova O., Xu L., Sai H., Pross S.E., Aster J.C., Bhandoola A., Radtke F., et al. Canonical notch signaling is dispensable for the maintenance of adult hematopoietic stem cells. Cell Stem. Cell. 2008;2:356–366. doi: 10.1016/j.stem.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yamazaki S., Ema H., Karlsson G., Yamaguchi T., Miyoshi H., Shioda S., Taketo M.M., Karlsson S., Iwama A., Nakauchi H. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell. 2011;147:1146–1158. doi: 10.1016/j.cell.2011.09.053. [DOI] [PubMed] [Google Scholar]
- 61.Sacchetti B., Funari A., Michienzi S., Di Cesare S., Piersanti S., Saggio I., Tagliafico E., Ferrari S., Robey P.G., Riminucci M., et al. Self-renewing osteoprogenitors in bone marrow sinusoids can organize a hematopoietic microenvironment. Cell. 2007;131:324–336. doi: 10.1016/j.cell.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 62.Chan C.K., Chen C.C., Luppen C.A., Kim J.B., DeBoer A.T., Wei K., Helms J.A., Kuo C.J., Kraft D.L., Weissman I.L. Endochondral ossification is required for haematopoietic stem-cell niche formation. Nature. 2009;457:490–494. doi: 10.1038/nature07547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mendez-Ferrer S., Michurina T.V., Ferraro F., Mazloom A.R., Macarthur B.D., Lira S.A., Scadden D.T., Ma’ayan A., Enikolopov G.N., Frenette P.S. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature. 2010;466:829–834. doi: 10.1038/nature09262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Omatsu Y., Sugiyama T., Kohara H., Kondoh G., Fujii N., Kohno K., Nagasawa T. The essential functions of adipo-osteogenic progenitors as the hematopoietic stem and progenitor cell niche. Immunity. 2010;33:387–399. doi: 10.1016/j.immuni.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 65.Chow A., Lucas D., Hidalgo A., Mendez-Ferrer S., Hashimoto D., Scheiermann C., Battista M., Leboeuf M., Prophete C., van Rooijen N., et al. Bone marrow CD169+ macrophages promote the retention of hematopoietic stem and progenitor cells in the mesenchymal stem cell niche. J. Exp. Med. 2011;208:261–271. doi: 10.1084/jem.20101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Winkler I.G., Sims N.A., Pettit A.R., Barbier V., Nowlan B., Helwani F., Poulton I.J., van Rooijen N., Alexander K.A., Raggatt L.J., et al. Bone marrow macrophages maintain hematopoietic stem cell (HSC) niches and their depletion mobilizes HSCs. Blood. 2010;116:4815–4828. doi: 10.1182/blood-2009-11-253534. [DOI] [PubMed] [Google Scholar]
- 67.Bruns I., Lucas D., Pinho S., Ahmed J., Lambert M.P., Kunisaki Y., Scheiermann C., Schiff L., Poncz M., Bergman A., et al. Megakaryocytes regulate hematopoietic stem cell quiescence through CXCL4 secretion. Nat. Med. 2014;20:1315–1320. doi: 10.1038/nm.3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhao M., Perry J.M., Marshall H., Venkatraman A., Qian P., He X.C., Ahamed J., Li L. Megakaryocytes maintain homeostatic quiescence and promote post-injury regeneration of hematopoietic stem cells. Nat. Med. 2014;20:1321–1326. doi: 10.1038/nm.3706. [DOI] [PubMed] [Google Scholar]
- 69.Olson T.S., Caselli A., Otsuru S., Hofmann T.J., Williams R., Paolucci P., Dominici M., Horwitz E.M. Megakaryocytes promote murine osteoblastic HSC niche expansion and stem cell engraftment after radioablative conditioning. Blood. 2013;121:5238–5249. doi: 10.1182/blood-2012-10-463414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Staller P., Sulitkova J., Lisztwan J., Moch H., Oakeley E.J., Krek W. Chemokine receptor CXCR4 downregulated by von Hippel-Lindau tumour suppressor pVHL. Nature. 2003;425:307–311. doi: 10.1038/nature01874. [DOI] [PubMed] [Google Scholar]
- 71.Danet G.H., Pan Y., Luongo J.L., Bonnet D.A., Simon M.C. Expansion of human SCID-repopulating cells under hypoxic conditions. J. Clin. Investig. 2003;112:126–135. doi: 10.1172/JCI17669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ceradini D.J., Kulkarni A.R., Callaghan M.J., Tepper O.M., Bastidas N., Kleinman M.E., Capla J.M., Galiano R.D., Levine J.P., Gurtner G.C. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat. Med. 2004;10:858–864. doi: 10.1038/nm1075. [DOI] [PubMed] [Google Scholar]
- 73.Takubo K., Goda N., Yamada W., Iriuchishima H., Ikeda E., Kubota Y., Shima H., Johnson R.S., Hirao A., Suematsu M., et al. Regulation of the HIF-1alpha level is essential for hematopoietic stem cells. Cell Stem. Cell. 2010;7:391–402. doi: 10.1016/j.stem.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 74.Kunisaki Y., Bruns I., Scheiermann C., Ahmed J., Pinho S., Zhang D., Mizoguchi T., Wei Q., Lucas D., Ito K., et al. Arteriolar niches maintain haematopoietic stem cell quiescence. Nature. 2013;502:637–643. doi: 10.1038/nature12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lucas D., Scheiermann C., Chow A., Kunisaki Y., Bruns I., Barrick C., Tessarollo L., Frenette P.S. Chemotherapy-induced bone marrow nerve injury impairs hematopoietic regeneration. Nat. Med. 2013;19:695–703. doi: 10.1038/nm.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mendez-Ferrer S., Lucas D., Battista M., Frenette P.S. Haematopoietic stem cell release is regulated by circadian oscillations. Nature. 2008;452:442–447. doi: 10.1038/nature06685. [DOI] [PubMed] [Google Scholar]
- 77.Cyster J.G. Homing of antibody secreting cells. Immunol Rev. 2003;194:48–60. doi: 10.1034/j.1600-065X.2003.00041.x. [DOI] [PubMed] [Google Scholar]
- 78.Nutt S.L., Hodgkin P.D., Tarlinton D.M., Corcoran L.M. The generation of antibody-secreting plasma cells. Nat. Rev. Immunol. 2015;15:160–171. doi: 10.1038/nri3795. [DOI] [PubMed] [Google Scholar]
- 79.Tashiro K., Tada H., Heilker R., Shirozu M., Nakano T., Honjo T. Signal sequence trap: A cloning strategy for secreted proteins and type I membrane proteins. Science. 1993;261:600–603. doi: 10.1126/science.8342023. [DOI] [PubMed] [Google Scholar]
- 80.Nagasawa T., Kikutani H., Kishimoto T. Molecular cloning and structure of a pre-B-cell growth-stimulating factor. Proc. Natl. Acad. Sci. USA. 1994;91:2305–2309. doi: 10.1073/pnas.91.6.2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bleul C.C., Fuhlbrigge R.C., Casasnovas J.M., Aiuti A., Springer T.A. A highly efficacious lymphocyte chemoattractant, stromal cell-derived factor 1 (SDF-1) J. Exp. Med. 1996;184:1101–1109. doi: 10.1084/jem.184.3.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hauser A.E., Debes G.F., Arce S., Cassese G., Hamann A., Radbruch A., Manz R.A. Chemotactic responsiveness toward ligands for CXCR3 and CXCR4 is regulated on plasma blasts during the time course of a memory immune response. J. Immunol. 2002;169:1277–1282. doi: 10.4049/jimmunol.169.3.1277. [DOI] [PubMed] [Google Scholar]
- 83.Li Y.F., Xu S., Ou X., Lam K.P. Shp1 signalling is required to establish the long-lived bone marrow plasma cell pool. Nat. Commun. 2014;5:4273. doi: 10.1038/ncomms5273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Minges Wols H.A., Underhill G.H., Kansas G.S., Witte P.L. The role of bone marrow-derived stromal cells in the maintenance of plasma cell longevity. J. Immunol. 2002;169:4213–4221. doi: 10.4049/jimmunol.169.8.4213. [DOI] [PubMed] [Google Scholar]
- 85.DiLillo D.J., Hamaguchi Y., Ueda Y., Yang K., Uchida J., Haas K.M., Kelsoe G., Tedder T.F. Maintenance of long-lived plasma cells and serological memory despite mature and memory B cell depletion during CD20 immunotherapy in mice. J. Immunol. 2008;180:361–371. doi: 10.4049/jimmunol.180.1.361. [DOI] [PubMed] [Google Scholar]
- 86.Zehentmeier S., Roth K., Cseresnyes Z., Sercan Ö., Horn K., Niesner R.A., Chang H.D., Radbruch A., Hauser A.E. Static and dynamic components synergize to form a stable survival niche for bone marrow plasma cells. Eur. J. Immunol. 2014;44:2306–2317. doi: 10.1002/eji.201344313. [DOI] [PubMed] [Google Scholar]
- 87.Pulido R., Elices M.J., Campanero M.R., Osborn L., Schiffer S., García-Pardo A., Lobb R., Hemler M.E., Sánchez-Madrid F. Functional evidence for three distinct and independently inhibitable adhesion activities mediated by the human integrin VLA-4. Correlation with distinct alpha 4 epitopes. J. Biol. Chem. 1991;266:10241–10245. doi: 10.1016/S0021-9258(18)99215-X. [DOI] [PubMed] [Google Scholar]
- 88.Nguyen D.C., Garimalla S., Xiao H., Kyu S., Albizua I., Galipeau J., Chiang K.Y., Waller E.K., Wu R., Gibson G., et al. Factors of the bone marrow microniche that support human plasma cell survival and immunoglobulin secretion. Nat. Commun. 2018;9:3698. doi: 10.1038/s41467-018-05853-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Baryawno N., Przybylski D., Kowalczyk M.S., Kfoury Y., Severe N., Gustafsson K., Kokkaliaris K.D., Mercier F., Tabaka M., Hofree M., et al. A Cellular Taxonomy of the Bone Marrow Stroma in Homeostasis and Leukemia. Cell. 2019;177:1915–1932.e16. doi: 10.1016/j.cell.2019.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kawano M.M., Mihara K., Huang N., Tsujimoto T., Kuramoto A. Differentiation of early plasma cells on bone marrow stromal cells requires interleukin-6 for escaping from apoptosis. Blood. 1995;85:487–494. doi: 10.1182/blood.V85.2.487.487. [DOI] [PubMed] [Google Scholar]
- 91.Chu V.T., Fröhlich A., Steinhauser G., Scheel T., Roch T., Fillatreau S., Lee J.J., Löhning M., Berek C. Eosinophils are required for the maintenance of plasma cells in the bone marrow. Nat. Immunol. 2011;12:151–159. doi: 10.1038/ni.1981. [DOI] [PubMed] [Google Scholar]
- 92.Haberland K., Ackermann J.A., Ipseiz N., Culemann S., Pracht K., Englbrecht M., Jäck H.M., Schett G., Schuh W., Krönke G. Eosinophils are not essential for maintenance of murine plasma cells in the bone marrow. Eur. J. Immunol. 2018;48:822–828. doi: 10.1002/eji.201747227. [DOI] [PubMed] [Google Scholar]
- 93.Bortnick A., Chernova I., Spencer S.P., Allman D. No strict requirement for eosinophils for bone marrow plasma cell survival. Eur. J. Immunol. 2018;48:815–821. doi: 10.1002/eji.201747229. [DOI] [PubMed] [Google Scholar]
- 94.Winter O., Moser K., Mohr E., Zotos D., Kaminski H., Szyska M., Roth K., Wong D.M., Dame C., Tarlinton D.M., et al. Megakaryocytes constitute a functional component of a plasma cell niche in the bone marrow. Blood. 2010;116:1867–1875. doi: 10.1182/blood-2009-12-259457. [DOI] [PubMed] [Google Scholar]
- 95.Benson M.J., Dillon S.R., Castigli E., Geha R.S., Xu S., Lam K.P., Noelle R.J. Cutting edge: The dependence of plasma cells and independence of memory B cells on BAFF and APRIL. J. Immunol. 2008;180:3655–3659. doi: 10.4049/jimmunol.180.6.3655. [DOI] [PubMed] [Google Scholar]
- 96.Walkley C.R., Olsen G.H., Dworkin S., Fabb S.A., Swann J., McArthur G.A., Westmoreland S.V., Chambon P., Scadden D.T., Purton L.E. A microenvironment-induced myeloproliferative syndrome caused by retinoic acid receptor gamma deficiency. Cell. 2007;129:1097–1110. doi: 10.1016/j.cell.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dong L., Yu W.M., Zheng H., Loh M.L., Bunting S.T., Pauly M., Huang G., Zhou M., Broxmeyer H.E., Scadden D.T., et al. Leukaemogenic effects of Ptpn11 activating mutations in the stem cell microenvironment. Nature. 2016;539:304–308. doi: 10.1038/nature20131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wortzel I., Dror S., Kenific C.M., Lyden D. Exosome-Mediated Metastasis: Communication from a Distance. Dev. Cell. 2019;49:347–360. doi: 10.1016/j.devcel.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 99.Théry C., Zitvogel L., Amigorena S. Exosomes: Composition, biogenesis and function. Nat. Rev. Immunol. 2002;2:569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 100.Mathieu M., Martin-Jaular L., Lavieu G., Théry C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat. Cell Biol. 2019;21:9–17. doi: 10.1038/s41556-018-0250-9. [DOI] [PubMed] [Google Scholar]
- 101.Roccaro A.M., Sacco A., Maiso P., Azab A.K., Tai Y.T., Reagan M., Azab F., Flores L.M., Campigotto F., Weller E., et al. BM mesenchymal stromal cell-derived exosomes facilitate multiple myeloma progression. J. Clin. Investig. 2013;123:1542–1555. doi: 10.1172/JCI66517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang J., Hendrix A., Hernot S., Lemaire M., De Bruyne E., Van Valckenborgh E., Lahoutte T., De Wever O., Vanderkerken K., Menu E. Bone marrow stromal cell-derived exosomes as communicators in drug resistance in multiple myeloma cells. Blood. 2014;124:555–566. doi: 10.1182/blood-2014-03-562439. [DOI] [PubMed] [Google Scholar]
- 103.Raimondi L., De Luca A., Amodio N., Manno M., Raccosta S., Taverna S., Bellavia D., Naselli F., Fontana S., Schillaci O., et al. Involvement of multiple myeloma cell-derived exosomes in osteoclast differentiation. Oncotarget. 2015;6:13772–13789. doi: 10.18632/oncotarget.3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Umezu T., Tadokoro H., Azuma K., Yoshizawa S., Ohyashiki K., Ohyashiki J.H. Exosomal miR-135b shed from hypoxic multiple myeloma cells enhances angiogenesis by targeting factor-inhibiting HIF-1. Blood. 2014;124:3748–3757. doi: 10.1182/blood-2014-05-576116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Colmone A., Amorim M., Pontier A.L., Wang S., Jablonski E., Sipkins D.A. Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science. 2008;322:1861–1865. doi: 10.1126/science.1164390. [DOI] [PubMed] [Google Scholar]
- 106.Boyd A.L., Campbell C.J., Hopkins C.I., Fiebig-Comyn A., Russell J., Ulemek J., Foley R., Leber B., Xenocostas A., Collins T.J., et al. Niche displacement of human leukemic stem cells uniquely allows their competitive replacement with healthy HSPCs. J. Exp. Med. 2014;211:1925–1935. doi: 10.1084/jem.20140131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Akinduro O., Weber T.S., Ang H., Haltalli M.L.R., Ruivo N., Duarte D., Rashidi N.M., Hawkins E.D., Duffy K.R., Lo Celso C. Proliferation dynamics of acute myeloid leukaemia and haematopoietic progenitors competing for bone marrow space. Nat. Commun. 2018;9:519. doi: 10.1038/s41467-017-02376-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kuehl W.M., Bergsagel P.L. Molecular pathogenesis of multiple myeloma and its premalignant precursor. J. Clin. Investig. 2012;122:3456–3463. doi: 10.1172/JCI61188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Giuliani N., Rizzoli V., Roodman G.D. Multiple myeloma bone disease: Pathophysiology of osteoblast inhibition. Blood. 2006;108:3992–3996. doi: 10.1182/blood-2006-05-026112. [DOI] [PubMed] [Google Scholar]
- 110.Raje N., Roodman G.D. Advances in the biology and treatment of bone disease in multiple myeloma. Clin. Cancer Res. 2011;17:1278–1286. doi: 10.1158/1078-0432.CCR-10-1804. [DOI] [PubMed] [Google Scholar]
- 111.Ghajar C.M. Metastasis prevention by targeting the dormant niche. Nat. Rev. Cancer. 2015;15:238–247. doi: 10.1038/nrc3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen Z., Orlowski R.Z., Wang M., Kwak L., McCarty N. Osteoblastic niche supports the growth of quiescent multiple myeloma cells. Blood. 2014;123:2204–2208. doi: 10.1182/blood-2013-07-517136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Khoo W.H., Ledergor G., Weiner A., Roden D.L., Terry R.L., McDonald M.M., Chai R.C., De Veirman K., Owen K.L., Opperman K.S., et al. A niche-dependent myeloid transcriptome signature defines dormant myeloma cells. Blood. 2019;134:30–43. doi: 10.1182/blood.2018880930. [DOI] [PubMed] [Google Scholar]
- 114.Lawson M.A., McDonald M.M., Kovacic N., Hua Khoo W., Terry R.L., Down J., Kaplan W., Paton-Hough J., Fellows C., Pettitt J.A., et al. Osteoclasts control reactivation of dormant myeloma cells by remodelling the endosteal niche. Nat. Commun. 2015;6:8983. doi: 10.1038/ncomms9983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roodman G.D. Osteoblast function in myeloma. Bone. 2011;48:135–140. doi: 10.1016/j.bone.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 116.Tian E., Zhan F., Walker R., Rasmussen E., Ma Y., Barlogie B., Shaughnessy J.D., Jr. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N. Engl. J. Med. 2003;349:2483–2494. doi: 10.1056/NEJMoa030847. [DOI] [PubMed] [Google Scholar]
- 117.Heath D.J., Chantry A.D., Buckle C.H., Coulton L., Shaughnessy J.D., Jr., Evans H.R., Snowden J.A., Stover D.R., Vanderkerken K., Croucher P.I. Inhibiting Dickkopf-1 (Dkk1) removes suppression of bone formation and prevents the development of osteolytic bone disease in multiple myeloma. J. Bone Miner. Res. 2009;24:425–436. doi: 10.1359/jbmr.081104. [DOI] [PubMed] [Google Scholar]
- 118.van Andel H., Kocemba K.A., Spaargaren M., Pals S.T. Aberrant Wnt signaling in multiple myeloma: Molecular mechanisms and targeting options. Leukemia. 2019;33:1063–1075. doi: 10.1038/s41375-019-0404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bolzoni M., Donofrio G., Storti P., Guasco D., Toscani D., Lazzaretti M., Bonomini S., Agnelli L., Capocefalo A., Dalla Palma B., et al. Myeloma cells inhibit non-canonical wnt co-receptor ror2 expression in human bone marrow osteoprogenitor cells: Effect of wnt5a/ror2 pathway activation on the osteogenic differentiation impairment induced by myeloma cells. Leukemia. 2013;27:451–463. doi: 10.1038/leu.2012.190. [DOI] [PubMed] [Google Scholar]
- 120.Frenquelli M., Caridi N., Antonini E., Storti F., Viganò V., Gaviraghi M., Occhionorelli M., Bianchessi S., Bongiovanni L., Spinelli A., et al. The WNT receptor ROR2 drives the interaction of multiple myeloma cells with the microenvironment through AKT activation. Leukemia. 2020;34:257–270. doi: 10.1038/s41375-019-0486-9. [DOI] [PubMed] [Google Scholar]
- 121.Mirandola L., Apicella L., Colombo M., Yu Y., Berta D.G., Platonova N., Lazzari E., Lancellotti M., Bulfamante G., Cobos E., et al. Anti-Notch treatment prevents multiple myeloma cells localization to the bone marrow via the chemokine system CXCR4/SDF-1. Leukemia. 2013;27:1558–1566. doi: 10.1038/leu.2013.27. [DOI] [PubMed] [Google Scholar]
- 122.Jundt F., Pröbsting K.S., Anagnostopoulos I., Muehlinghaus G., Chatterjee M., Mathas S., Bargou R.C., Manz R., Stein H., Dörken B. Jagged1-induced Notch signaling drives proliferation of multiple myeloma cells. Blood. 2004;103:3511–3515. doi: 10.1182/blood-2003-07-2254. [DOI] [PubMed] [Google Scholar]
- 123.Houde C., Li Y., Song L., Barton K., Zhang Q., Godwin J., Nand S., Toor A., Alkan S., Smadja N.V., et al. Overexpression of the NOTCH ligand JAG2 in malignant plasma cells from multiple myeloma patients and cell lines. Blood. 2004;104:3697–3704. doi: 10.1182/blood-2003-12-4114. [DOI] [PubMed] [Google Scholar]
- 124.Giuliani N., Colla S., Morandi F., Lazzaretti M., Sala R., Bonomini S., Grano M., Colucci S., Svaldi M., Rizzoli V. Myeloma cells block RUNX2/CBFA1 activity in human bone marrow osteoblast progenitors and inhibit osteoblast formation and differentiation. Blood. 2005;106:2472–2483. doi: 10.1182/blood-2004-12-4986. [DOI] [PubMed] [Google Scholar]
- 125.Garayoa M., Garcia J.L., Santamaria C., Garcia-Gomez A., Blanco J.F., Pandiella A., Hernandez J.M., Sanchez-Guijo F.M., del Canizo M.C., Gutierrez N.C., et al. Mesenchymal stem cells from multiple myeloma patients display distinct genomic profile as compared with those from normal donors. Leukemia. 2009;23:1515–1527. doi: 10.1038/leu.2009.65. [DOI] [PubMed] [Google Scholar]
- 126.Corre J., Mahtouk K., Attal M., Gadelorge M., Huynh A., Fleury-Cappellesso S., Danho C., Laharrague P., Klein B., Rème T., et al. Bone marrow mesenchymal stem cells are abnormal in multiple myeloma. Leukemia. 2007;21:1079–1088. doi: 10.1038/sj.leu.2404621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kawano Y., Moschetta M., Manier S., Glavey S., Görgün G.T., Roccaro A.M., Anderson K.C., Ghobrial I.M. Targeting the bone marrow microenvironment in multiple myeloma. Immunol. Rev. 2015;263:160–172. doi: 10.1111/imr.12233. [DOI] [PubMed] [Google Scholar]
- 128.Gupta D., Treon S.P., Shima Y., Hideshima T., Podar K., Tai Y.T., Lin B., Lentzsch S., Davies F.E., Chauhan D., et al. Adherence of multiple myeloma cells to bone marrow stromal cells upregulates vascular endothelial growth factor secretion: Therapeutic applications. Leukemia. 2001;15:1950–1961. doi: 10.1038/sj.leu.2402295. [DOI] [PubMed] [Google Scholar]
- 129.Tanno T., Lim Y., Wang Q., Chesi M., Bergsagel P.L., Matthews G., Johnstone R.W., Ghosh N., Borrello I., Huff C.A., et al. Growth differentiating factor 15 enhances the tumor-initiating and self-renewal potential of multiple myeloma cells. Blood. 2014;123:725–733. doi: 10.1182/blood-2013-08-524025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nakamura K., Smyth M.J., Martinet L. Cancer immunoediting and immune dysregulation in multiple myeloma. Blood. 2020 doi: 10.1182/blood.2020006540. [DOI] [PubMed] [Google Scholar]
- 131.Hoyos V., Borrello I. The immunotherapy era of myeloma: Monoclonal antibodies, vaccines, and adoptive T-cell therapies. Blood. 2016;128:1679–1687. doi: 10.1182/blood-2016-05-636357. [DOI] [PubMed] [Google Scholar]
- 132.Cohen A.D., Raje N., Fowler J.A., Mezzi K., Scott E.C., Dhodapkar M.V. How to Train Your T Cells: Overcoming Immune Dysfunction in Multiple Myeloma. Clin. Cancer Res. 2020;26:1541–1554. doi: 10.1158/1078-0432.CCR-19-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xu S., De Veirman K., De Becker A., Vanderkerken K., Van Riet I. Mesenchymal stem cells in multiple myeloma: A therapeutical tool or target? Leukemia. 2018;32:1500–1514. doi: 10.1038/s41375-018-0061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lomas O.C., Tahri S., Ghobrial I.M. The microenvironment in myeloma. Curr. Opin. Oncol. 2020;32:170–175. doi: 10.1097/CCO.0000000000000615. [DOI] [PubMed] [Google Scholar]
- 135.Zheng Y., Cai Z., Wang S., Zhang X., Qian J., Hong S., Li H., Wang M., Yang J., Yi Q. Macrophages are an abundant component of myeloma microenvironment and protect myeloma cells from chemotherapy drug-induced apoptosis. Blood. 2009;114:3625–3628. doi: 10.1182/blood-2009-05-220285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lorenzo-Sanz L., Muñoz P. Tumor-Infiltrating Immunosuppressive Cells in Cancer-Cell Plasticity, Tumor Progression and Therapy Response. Cancer Microenviron. 2019;12:119–132. doi: 10.1007/s12307-019-00232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Petty A.J., Yang Y. Tumor-Associated Macrophages in Hematologic Malignancies: New Insights and Targeted Therapies. Cells. 2019;8:1526. doi: 10.3390/cells8121526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Beider K., Bitner H., Leiba M., Gutwein O., Koren-Michowitz M., Ostrovsky O., Abraham M., Wald H., Galun E., Peled A., et al. Multiple myeloma cells recruit tumor-supportive macrophages through the CXCR4/CXCL12 axis and promote their polarization toward the M2 phenotype. Oncotarget. 2014;5:11283–11296. doi: 10.18632/oncotarget.2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen H., Li M., Sanchez E., Soof C.M., Bujarski S., Ng N., Cao J., Hekmati T., Zahab B., Nosrati J.D., et al. JAK1/2 pathway inhibition suppresses M2 polarization and overcomes resistance of myeloma to lenalidomide by reducing TRIB1, MUC1, CD44, CXCL12, and CXCR4 expression. Br. J. Haematol. 2020;188:283–294. doi: 10.1111/bjh.16158. [DOI] [PubMed] [Google Scholar]
- 140.Li Y., Zheng Y., Li T., Wang Q., Qian J., Lu Y., Zhang M., Bi E., Yang M., Reu F., et al. Chemokines CCL2, 3, 14 stimulate macrophage bone marrow homing, proliferation, and polarization in multiple myeloma. Oncotarget. 2015;6:24218–24229. doi: 10.18632/oncotarget.4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.De Beule N., De Veirman K., Maes K., De Bruyne E., Menu E., Breckpot K., De Raeve H., Van Rampelbergh R., Van Ginderachter J.A., Schots R., et al. Tumour-associated macrophage-mediated survival of myeloma cells through STAT3 activation. J. Pathol. 2017;241:534–546. doi: 10.1002/path.4860. [DOI] [PubMed] [Google Scholar]
- 142.Wang Q., Lu Y., Li R., Jiang Y., Zheng Y., Qian J., Bi E., Zheng C., Hou J., Wang S., et al. Therapeutic effects of CSF1R-blocking antibodies in multiple myeloma. Leukemia. 2018;32:176–183. doi: 10.1038/leu.2017.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chen X., Chen J., Zhang W., Sun R., Liu T., Zheng Y., Wu Y. Prognostic value of diametrically polarized tumor-associated macrophages in multiple myeloma. Oncotarget. 2017;8:112685–112696. doi: 10.18632/oncotarget.22340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wang H., Hu W.M., Xia Z.J., Liang Y., Lu Y., Lin S.X., Tang H. High numbers of CD163+ tumor-associated macrophages correlate with poor prognosis in multiple myeloma patients receiving bortezomib-based regimens. J. Cancer. 2019;10:3239–3245. doi: 10.7150/jca.30102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Panchabhai S., Kelemen K., Ahmann G., Sebastian S., Mantei J., Fonseca R. Tumor-associated macrophages and extracellular matrix metalloproteinase inducer in prognosis of multiple myeloma. Leukemia. 2016;30:951–954. doi: 10.1038/leu.2015.191. [DOI] [PubMed] [Google Scholar]
- 146.Andersen M.N., Andersen N.F., Rødgaard-Hansen S., Hokland M., Abildgaard N., Møller H.J. The novel biomarker of alternative macrophage activation, soluble mannose receptor (sMR/sCD206): Implications in multiple myeloma. Leuk. Res. 2015;39:971–975. doi: 10.1016/j.leukres.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 147.Wang Q., Zhao D., Xian M., Wang Z., Bi E., Su P., Qian J., Ma X., Yang M., Liu L., et al. MIF as a biomarker and therapeutic target for overcoming resistance to proteasome inhibitors in human myeloma. Blood. 2020 doi: 10.1182/blood.2020005795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Xu R., Li Y., Yan H., Zhang E., Huang X., Chen Q., Chen J., Qu J., Liu Y., He J., et al. CCL2 promotes macrophages-associated chemoresistance via MCPIP1 dual catalytic activities in multiple myeloma. Cell Death Dis. 2019;10:781. doi: 10.1038/s41419-019-2012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kim J., Denu R.A., Dollar B.A., Escalante L.E., Kuether J.P., Callander N.S., Asimakopoulos F., Hematti P. Macrophages and mesenchymal stromal cells support survival and proliferation of multiple myeloma cells. Br. J. Haematol. 2012;158:336–346. doi: 10.1111/j.1365-2141.2012.09154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zheng Y., Yang J., Qian J., Qiu P., Hanabuchi S., Lu Y., Wang Z., Liu Z., Li H., He J., et al. PSGL-1/selectin and ICAM-1/CD18 interactions are involved in macrophage-induced drug resistance in myeloma. Leukemia. 2013;27:702–710. doi: 10.1038/leu.2012.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Beyar-Katz O., Magidey K., Ben-Tsedek N., Alishekevitz D., Timaner M., Miller V., Lindzen M., Yarden Y., Avivi I., Shaked Y. Bortezomib-induced pro-inflammatory macrophages as a potential factor limiting anti-tumour efficacy. J. Pathol. 2016;239:262–273. doi: 10.1002/path.4723. [DOI] [PubMed] [Google Scholar]
- 152.Minnie S.A., Kuns R.D., Gartlan K.H., Zhang P., Wilkinson A.N., Samson L., Guillerey C., Engwerda C., MacDonald K.P.A., Smyth M.J., et al. Myeloma escape after stem cell transplantation is a consequence of T-cell exhaustion and is prevented by TIGIT blockade. Blood. 2018;132:1675–1688. doi: 10.1182/blood-2018-01-825240. [DOI] [PubMed] [Google Scholar]
- 153.Opperman K.S., Vandyke K., Clark K.C., Coulter E.A., Hewett D.R., Mrozik K.M., Schwarz N., Evdokiou A., Croucher P.I., Psaltis P.J., et al. Clodronate-Liposome Mediated Macrophage Depletion Abrogates Multiple Myeloma Tumor Establishment In Vivo. Neoplasia. 2019;21:777–787. doi: 10.1016/j.neo.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Scavelli C., Nico B., Cirulli T., Ria R., Di Pietro G., Mangieri D., Bacigalupo A., Mangialardi G., Coluccia A.M., Caravita T., et al. Vasculogenic mimicry by bone marrow macrophages in patients with multiple myeloma. Oncogene. 2008;27:663–674. doi: 10.1038/sj.onc.1210691. [DOI] [PubMed] [Google Scholar]
- 155.Alexandrakis M.G., Goulidaki N., Pappa C.A., Boula A., Psarakis F., Neonakis I., Tsirakis G. Interleukin-10 Induces Both Plasma Cell Proliferation and Angiogenesis in Multiple Myeloma. Pathol. Oncol. Res. 2015;21:929–934. doi: 10.1007/s12253-015-9921-z. [DOI] [PubMed] [Google Scholar]
- 156.Berardi S., Ria R., Reale A., De Luisi A., Catacchio I., Moschetta M., Vacca A. Multiple myeloma macrophages: Pivotal players in the tumor microenvironment. J. Oncol. 2013;2013:183602. doi: 10.1155/2013/183602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bogen B., Fauskanger M., Haabeth O.A., Tveita A. CD4(+) T cells indirectly kill tumor cells via induction of cytotoxic macrophages in mouse models. Cancer Immunol. Immunother. 2019;68:1865–1873. doi: 10.1007/s00262-019-02374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Haabeth O.A.W., Hennig K., Fauskanger M., Løset G., Bogen B., Tveita A. CD4+ T-cell killing of multiple myeloma cells is mediated by resident bone marrow macrophages. Blood Adv. 2020;4:2595–2605. doi: 10.1182/bloodadvances.2020001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Fauskanger M., Haabeth O.A.W., Skjeldal F.M., Bogen B., Tveita A.A. Tumor Killing by CD4+ T Cells Is Mediated via Induction of Inducible Nitric Oxide Synthase-Dependent Macrophage Cytotoxicity. Front Immunol. 2018;9:1684. doi: 10.3389/fimmu.2018.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Haabeth O.A., Lorvik K.B., Hammarström C., Donaldson I.M., Haraldsen G., Bogen B., Corthay A. Inflammation driven by tumour-specific Th1 cells protects against B-cell cancer. Nat. Commun. 2011;2:240. doi: 10.1038/ncomms1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Tveita A.A., Schjesvold F., Haabeth O.A., Fauskanger M., Bogen B. Tumors Escape CD4+ T-cell-Mediated Immunosurveillance by Impairing the Ability of Infiltrating Macrophages to Indirectly Present Tumor Antigens. Cancer Res. 2015;75:3268–3278. doi: 10.1158/0008-5472.CAN-14-3640. [DOI] [PubMed] [Google Scholar]
- 162.Tveita A.A., Schjesvold F.H., Sundnes O., Haabeth O.A., Haraldsen G., Bogen B. Indirect CD4+ T-cell-mediated elimination of MHC II(NEG) tumor cells is spatially restricted and fails to prevent escape of antigen-negative cells. Eur. J. Immunol. 2014;44:2625–2637. doi: 10.1002/eji.201444659. [DOI] [PubMed] [Google Scholar]
- 163.Gutiérrez-González A., Martínez-Moreno M., Samaniego R., Arellano-Sánchez N., Salinas-Muñoz L., Relloso M., Valeri A., Martínez-López J., Corbí Á.L., Hidalgo A., et al. Evaluation of the potential therapeutic benefits of macrophage reprogramming in multiple myeloma. Blood. 2016;128:2241–2252. doi: 10.1182/blood-2016-01-695395. [DOI] [PubMed] [Google Scholar]
- 164.Lee S.E., Lim J.Y., Ryu D.B., Kim T.W., Yoon J.H., Cho B.S., Eom K.S., Kim Y.J., Kim H.J., Lee S., et al. Circulating immune cell phenotype can predict the outcome of lenalidomide plus low-dose dexamethasone treatment in patients with refractory/relapsed multiple myeloma. Cancer Immunol. Immunother. 2016;65:983–994. doi: 10.1007/s00262-016-1861-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Giallongo C., Tibullo D., Parrinello N.L., La Cava P., Di Rosa M., Bramanti V., Di Raimondo C., Conticello C., Chiarenza A., Palumbo G.A., et al. Granulocyte-like myeloid derived suppressor cells (G-MDSC) are increased in multiple myeloma and are driven by dysfunctional mesenchymal stem cells (MSC) Oncotarget. 2016;7:85764–85775. doi: 10.18632/oncotarget.7969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Favaloro J., Liyadipitiya T., Brown R., Yang S., Suen H., Woodland N., Nassif N., Hart D., Fromm P., Weatherburn C., et al. Myeloid derived suppressor cells are numerically, functionally and phenotypically different in patients with multiple myeloma. Leuk. Lymphoma. 2014;55:2893–2900. doi: 10.3109/10428194.2014.904511. [DOI] [PubMed] [Google Scholar]
- 167.Tai Y.T., Lin L., Xing L., Cho S.F., Yu T., Acharya C., Wen K., Hsieh P.A., Dulos J., van Elsas A., et al. APRIL signaling via TACI mediates immunosuppression by T regulatory cells in multiple myeloma: Therapeutic implications. Leukemia. 2019;33:426–438. doi: 10.1038/s41375-018-0242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Romano A., Parrinello N.L., La Cava P., Tibullo D., Giallongo C., Camiolo G., Puglisi F., Parisi M., Pirosa M.C., Martino E., et al. PMN-MDSC and arginase are increased in myeloma and may contribute to resistance to therapy. Expert Rev. Mol. Diagn. 2018;18:675–683. doi: 10.1080/14737159.2018.1470929. [DOI] [PubMed] [Google Scholar]
- 169.Wang Z., Zhang L., Wang H., Xiong S., Li Y., Tao Q., Xiao W., Qin H., Wang Y., Zhai Z. Tumor-induced CD14+HLA-DR (-/low) myeloid-derived suppressor cells correlate with tumor progression and outcome of therapy in multiple myeloma patients. Cancer Immunol. Immunother. 2015;64:389–399. doi: 10.1007/s00262-014-1646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kuwahara-Ota S., Shimura Y., Steinebach C., Isa R., Yamaguchi J., Nishiyama D., Fujibayashi Y., Takimoto-Shimomura T., Mizuno Y., Matsumura-Kimoto Y., et al. Lenalidomide and pomalidomide potently interfere with induction of myeloid-derived suppressor cells in multiple myeloma. Br. J. Haematol. 2020 doi: 10.1111/bjh.16881. [DOI] [PubMed] [Google Scholar]
- 171.Gorgun G., Samur M.K., Cowens K.B., Paula S., Bianchi G., Anderson J.E., White R.E., Singh A., Ohguchi H., Suzuki R., et al. Lenalidomide Enhances Immune Checkpoint Blockade-Induced Immune Response in Multiple Myeloma. Clin. Cancer Res. 2015;21:4607–4618. doi: 10.1158/1078-0432.CCR-15-0200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.De Veirman K., Van Ginderachter J.A., Lub S., De Beule N., Thielemans K., Bautmans I., Oyajobi B.O., De Bruyne E., Menu E., Lemaire M., et al. Multiple myeloma induces Mcl-1 expression and survival of myeloid-derived suppressor cells. Oncotarget. 2015;6:10532–10547. doi: 10.18632/oncotarget.3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zhou J., Lin H., Hu L., Li G., Zhang X. Decitabine shows potent anti-myeloma activity by depleting monocytic myeloid-derived suppressor cells in the myeloma microenvironment. J. Cancer Res. Clin. Oncol. 2019;145:329–336. doi: 10.1007/s00432-018-2790-6. [DOI] [PubMed] [Google Scholar]
- 174.Wang J., De Veirman K., Faict S., Frassanito M.A., Ribatti D., Vacca A., Menu E. Multiple myeloma exosomes establish a favourable bone marrow microenvironment with enhanced angiogenesis and immunosuppression. J. Pathol. 2016;239:162–173. doi: 10.1002/path.4712. [DOI] [PubMed] [Google Scholar]
- 175.Wang J., De Veirman K., De Beule N., Maes K., De Bruyne E., Van Valckenborgh E., Vanderkerken K., Menu E. The bone marrow microenvironment enhances multiple myeloma progression by exosome-mediated activation of myeloid-derived suppressor cells. Oncotarget. 2015;6:43992–44004. doi: 10.18632/oncotarget.6083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Leone P., Berardi S., Frassanito M.A., Ria R., De Re V., Cicco S., Battaglia S., Ditonno P., Dammacco F., Vacca A., et al. Dendritic cells accumulate in the bone marrow of myeloma patients where they protect tumor plasma cells from CD8+ T-cell killing. Blood. 2015;126:1443–1451. doi: 10.1182/blood-2015-01-623975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Ray A., Das D.S., Song Y., Macri V., Richardson P., Brooks C.L., Chauhan D., Anderson K.C. A novel agent SL-401 induces anti-myeloma activity by targeting plasmacytoid dendritic cells, osteoclastogenesis and cancer stem-like cells. Leukemia. 2017;31:2652–2660. doi: 10.1038/leu.2017.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lamarthee B., de Vassoigne F., Malard F., Stocker N., Boussen I., Mediavilla C., Tang R., Fava F., Garderet L., Marjanovic Z., et al. Quantitative and functional alterations of 6-sulfo LacNac dendritic cells in multiple myeloma. Oncoimmunology. 2018;7:e1444411. doi: 10.1080/2162402X.2018.1444411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shinde P., Fernandes S., Melinkeri S., Kale V., Limaye L. Compromised functionality of monocyte-derived dendritic cells in multiple myeloma patients may limit their use in cancer immunotherapy. Sci. Rep. 2018;8:5705. doi: 10.1038/s41598-018-23943-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Romano A., Parrinello N.L., Simeon V., Puglisi F., La Cava P., Bellofiore C., Giallongo C., Camiolo G., D’Auria F., Grieco V., et al. High-density neutrophils in MGUS and multiple myeloma are dysfunctional and immune-suppressive due to increased STAT3 downstream signaling. Sci. Rep. 2020;10:1983. doi: 10.1038/s41598-020-58859-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Puglisi F., Parrinello N.L., Giallongo C., Cambria D., Camiolo G., Bellofiore C., Conticello C., Del Fabro V., Leotta V., Markovic U., et al. Plasticity of High-Density Neutrophils in Multiple Myeloma is Associated with Increased Autophagy Via STAT3. Int. J. Mol. Sci. 2019;20:3548. doi: 10.3390/ijms20143548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Perez C., Botta C., Zabaleta A., Puig N., Cedena M.T., Goicoechea I., Alameda D., San Jose-Eneriz E., Merino J., Rodriguez-Otero P., et al. Immunogenomic identification and characterization of granulocytic myeloid-derived suppressor cells in multiple myeloma. Blood. 2020;136:199–209. doi: 10.1182/blood.2019004537. [DOI] [PubMed] [Google Scholar]
- 183.Wong T.W., Kita H., Hanson C.A., Walters D.K., Arendt B.K., Jelinek D.F. Induction of malignant plasma cell proliferation by eosinophils. PLoS ONE. 2013;8:e70554. doi: 10.1371/journal.pone.0070554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Glatman Zaretsky A., Konradt C., Dépis F., Wing J.B., Goenka R., Atria D.G., Silver J.S., Cho S., Wolf A.I., Quinn W.J., et al. T Regulatory Cells Support Plasma Cell Populations in the Bone Marrow. Cell Rep. 2017;18:1906–1916. doi: 10.1016/j.celrep.2017.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Vyzoukaki R., Tsirakis G., Pappa C.A., Devetzoglou M., Tzardi M., Alexandrakis M.G. The Impact of Mast Cell Density on the Progression of Bone Disease in Multiple Myeloma Patients. Int. Arch Allergy Immunol. 2015;168:263–268. doi: 10.1159/000443275. [DOI] [PubMed] [Google Scholar]
- 186.Takagi S., Tsukamoto S., Park J., Johnson K.E., Kawano Y., Moschetta M., Liu C.J., Mishima Y., Kokubun K., Manier S., et al. Platelets Enhance Multiple Myeloma Progression via IL-1beta Upregulation. Clin. Cancer Res. 2018;24:2430–2439. doi: 10.1158/1078-0432.CCR-17-2003. [DOI] [PubMed] [Google Scholar]
- 187.Prabhala R.H., Pelluru D., Fulciniti M., Prabhala H.K., Nanjappa P., Song W., Pai C., Amin S., Tai Y.T., Richardson P.G., et al. Elevated IL-17 produced by TH17 cells promotes myeloma cell growth and inhibits immune function in multiple myeloma. Blood. 2010;115:5385–5392. doi: 10.1182/blood-2009-10-246660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bryant C., Suen H., Brown R., Yang S., Favaloro J., Aklilu E., Gibson J., Ho P.J., Iland H., Fromm P., et al. Long-term survival in multiple myeloma is associated with a distinct immunological profile, which includes proliferative cytotoxic T-cell clones and a favourable Treg/Th17 balance. Blood Cancer J. 2013;3:e148. doi: 10.1038/bcj.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lad D., Huang Q., Hoeppli R., Garcia R., Xu L., Levings M., Song K., Broady R. Evaluating the role of Tregs in the progression of multiple myeloma. Leuk. Lymphoma. 2019;60:2134–2142. doi: 10.1080/10428194.2019.1579324. [DOI] [PubMed] [Google Scholar]
- 190.Alrasheed N., Lee L., Ghorani E., Henry J.Y., Conde L., Chin M., Galas-Filipowicz D., Furness A.J.S., Chavda S.J., Richards H., et al. Marrow-Infiltrating Regulatory T Cells Correlate with the Presence of Dysfunctional CD4+PD-1+ Cells and Inferior Survival in Patients with Newly Diagnosed Multiple Myeloma. Clin. Cancer Res. 2020;26:3443–3454. doi: 10.1158/1078-0432.CCR-19-1714. [DOI] [PubMed] [Google Scholar]
- 191.Giannopoulos K., Kaminska W., Hus I., Dmoszynska A. The frequency of T regulatory cells modulates the survival of multiple myeloma patients: Detailed characterisation of immune status in multiple myeloma. Br. J. Cancer. 2012;106:546–552. doi: 10.1038/bjc.2011.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Wang J.N., Cao X.X., Zhao A.L., Cai H., Wang X., Li J. Increased activated regulatory T cell subsets and aging Treg-like cells in multiple myeloma and monoclonal gammopathy of undetermined significance: A case control study. Cancer Cell Int. 2018;18:187. doi: 10.1186/s12935-018-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kawano Y., Zavidij O., Park J., Moschetta M., Kokubun K., Mouhieddine T.H., Manier S., Mishima Y., Murakami N., Bustoros M., et al. Blocking IFNAR1 inhibits multiple myeloma-driven Treg expansion and immunosuppression. J. Clin. Investig. 2018;128:2487–2499. doi: 10.1172/JCI88169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Bonanno G., Mariotti A., Procoli A., Folgiero V., Natale D., De Rosa L., Majolino I., Novarese L., Rocci A., Gambella M., et al. Indoleamine 2,3-dioxygenase 1 (IDO1) activity correlates with immune system abnormalities in multiple myeloma. J. Transl. Med. 2012;10:247. doi: 10.1186/1479-5876-10-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Krejcik J., Casneuf T., Nijhof I.S., Verbist B., Bald J., Plesner T., Syed K., Liu K., van de Donk N.W., Weiss B.M., et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128:384–394. doi: 10.1182/blood-2015-12-687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Rosenblatt J., Glotzbecker B., Mills H., Vasir B., Tzachanis D., Levine J.D., Joyce R.M., Wellenstein K., Keefe W., Schickler M., et al. PD-1 blockade by CT-011, anti-PD-1 antibody, enhances ex vivo T-cell responses to autologous dendritic cell/myeloma fusion vaccine. J. Immunother. 2011;34:409–418. doi: 10.1097/CJI.0b013e31821ca6ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yousef S., Marvin J., Steinbach M., Langemo A., Kovacsovics T., Binder M., Kröger N., Luetkens T., Atanackovic D. Immunomodulatory molecule PD-L1 is expressed on malignant plasma cells and myeloma-propagating pre-plasma cells in the bone marrow of multiple myeloma patients. Blood Cancer J. 2015;5:e285. doi: 10.1038/bcj.2015.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lee B.H., Park Y., Kim J.H., Kang K.W., Lee S.J., Kim S.J., Kim B.S. PD-L1 expression in bone marrow plasma cells as a biomarker to predict multiple myeloma prognosis: Developing a nomogram-based prognostic model. Sci. Rep. 2020;10:12641. doi: 10.1038/s41598-020-69616-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Usmani S.Z., Schjesvold F., Oriol A., Karlin L., Cavo M., Rifkin R.M., Yimer H.A., LeBlanc R., Takezako N., McCroskey R.D., et al. Pembrolizumab plus lenalidomide and dexamethasone for patients with treatment-naive multiple myeloma (KEYNOTE-185): A randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6:e448–e458. doi: 10.1016/S2352-3026(19)30109-7. [DOI] [PubMed] [Google Scholar]
- 200.Mateos M.V., Blacklock H., Schjesvold F., Oriol A., Simpson D., George A., Goldschmidt H., Larocca A., Chanan-Khan A., Sherbenou D., et al. Pembrolizumab plus pomalidomide and dexamethasone for patients with relapsed or refractory multiple myeloma (KEYNOTE-183): A randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6:e459–e469. doi: 10.1016/S2352-3026(19)30110-3. [DOI] [PubMed] [Google Scholar]
- 201.Suen H., Brown R., Yang S., Weatherburn C., Ho P.J., Woodland N., Nassif N., Barbaro P., Bryant C., Hart D., et al. Multiple myeloma causes clonal T-cell immunosenescence: Identification of potential novel targets for promoting tumour immunity and implications for checkpoint blockade. Leukemia. 2016;30:1716–1724. doi: 10.1038/leu.2016.84. [DOI] [PubMed] [Google Scholar]
- 202.Bailur J.K., McCachren S.S., Doxie D.B., Shrestha M., Pendleton K., Nooka A.K., Neparidze N., Parker T.L., Bar N., Kaufman J.L., et al. Early alterations in stem-like/resident T cells, innate and myeloid cells in the bone marrow in preneoplastic gammopathy. JCI Insight. 2019;5 doi: 10.1172/jci.insight.127807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zelle-Rieser C., Thangavadivel S., Biedermann R., Brunner A., Stoitzner P., Willenbacher E., Greil R., Jöhrer K. T cells in multiple myeloma display features of exhaustion and senescence at the tumor site. J. Hematol. Oncol. 2016;9:116. doi: 10.1186/s13045-016-0345-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Witzens-Harig M., Hose D., Jünger S., Pfirschke C., Khandelwal N., Umansky L., Seckinger A., Conrad H., Brackertz B., Rème T., et al. Tumor cells in multiple myeloma patients inhibit myeloma-reactive T cells through carcinoembryonic antigen-related cell adhesion molecule-6. Blood. 2013;121:4493–4503. doi: 10.1182/blood-2012-05-429415. [DOI] [PubMed] [Google Scholar]
- 205.Giuliani N., Colla S., Sala R., Moroni M., Lazzaretti M., La Monica S., Bonomini S., Hojden M., Sammarelli G., Barillè S., et al. Human myeloma cells stimulate the receptor activator of nuclear factor-kappa B ligand (RANKL) in T lymphocytes: A potential role in multiple myeloma bone disease. Blood. 2002;100:4615–4621. doi: 10.1182/blood-2002-04-1121. [DOI] [PubMed] [Google Scholar]
- 206.Ehrlich L.A., Chung H.Y., Ghobrial I., Choi S.J., Morandi F., Colla S., Rizzoli V., Roodman G.D., Giuliani N. IL-3 is a potential inhibitor of osteoblast differentiation in multiple myeloma. Blood. 2005;106:1407–1414. doi: 10.1182/blood-2005-03-1080. [DOI] [PubMed] [Google Scholar]
- 207.Giuliani N., Morandi F., Tagliaferri S., Colla S., Bonomini S., Sammarelli G., Rizzoli V. Interleukin-3 (IL-3) is overexpressed by T lymphocytes in multiple myeloma patients. Blood. 2006;107:841–842. doi: 10.1182/blood-2005-07-2719. [DOI] [PubMed] [Google Scholar]
- 208.Noonan K., Marchionni L., Anderson J., Pardoll D., Roodman G.D., Borrello I. A novel role of IL-17-producing lymphocytes in mediating lytic bone disease in multiple myeloma. Blood. 2010;116:3554–3563. doi: 10.1182/blood-2010-05-283895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Schütt P., Brandhorst D., Stellberg W., Poser M., Ebeling P., Müller S., Buttkereit U., Opalka B., Lindemann M., Grosse-Wilde H., et al. Immune parameters in multiple myeloma patients: Influence of treatment and correlation with opportunistic infections. Leuk. Lymphoma. 2006;47:1570–1582. doi: 10.1080/10428190500472503. [DOI] [PubMed] [Google Scholar]
- 210.García-Sanz R., González M., Orfão A., Moro M.J., Hernández J.M., Borrego D., Carnero M., Casanova F., Bárez A., Jiménez R., et al. Analysis of natural killer-associated antigens in peripheral blood and bone marrow of multiple myeloma patients and prognostic implications. Br. J. Haematol. 1996;93:81–88. doi: 10.1046/j.1365-2141.1996.4651006.x. [DOI] [PubMed] [Google Scholar]
- 211.Jurisic V., Srdic T., Konjevic G., Markovic O., Colovic M. Clinical stage-depending decrease of NK cell activity in multiple myeloma patients. Med. Oncol. 2007;24:312–317. doi: 10.1007/s12032-007-0007-y. [DOI] [PubMed] [Google Scholar]
- 212.Frassanito M.A., Silvestris F., Cafforio P., Silvestris N., Dammacco F. IgG M-components in active myeloma patients induce a down-regulation of natural killer cell activity. Int. J. Clin. Lab Res. 1997;27:48–54. doi: 10.1007/BF02827242. [DOI] [PubMed] [Google Scholar]
- 213.Konjević G., Vuletić A., Mirjačić Martinović K., Colović N., Čolović M., Jurišić V. Decreased CD161 activating and increased CD158a inhibitory receptor expression on NK cells underlies impaired NK cell cytotoxicity in patients with multiple myeloma. J. Clin. Pathol. 2016 doi: 10.1136/jclinpath-2016-203614. [DOI] [PubMed] [Google Scholar]
- 214.Fauriat C., Mallet F., Olive D., Costello R.T. Impaired activating receptor expression pattern in natural killer cells from patients with multiple myeloma. Leukemia. 2006;20:732–733. doi: 10.1038/sj.leu.2404096. [DOI] [PubMed] [Google Scholar]
- 215.Jinushi M., Vanneman M., Munshi N.C., Tai Y.T., Prabhala R.H., Ritz J., Neuberg D., Anderson K.C., Carrasco D.R., Dranoff G. MHC class I chain-related protein A antibodies and shedding are associated with the progression of multiple myeloma. Proc. Natl. Acad. Sci. USA. 2008;105:1285–1290. doi: 10.1073/pnas.0711293105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.El-Sherbiny Y.M., Meade J.L., Holmes T.D., McGonagle D., Mackie S.L., Morgan A.W., Cook G., Feyler S., Richards S.J., Davies F.E., et al. The requirement for DNAM-1, NKG2D, and NKp46 in the natural killer cell-mediated killing of myeloma cells. Cancer Res. 2007;67:8444–8449. doi: 10.1158/0008-5472.CAN-06-4230. [DOI] [PubMed] [Google Scholar]
- 217.Ponzetta A., Benigni G., Antonangeli F., Sciumè G., Sanseviero E., Zingoni A., Ricciardi M.R., Petrucci M.T., Santoni A., Bernardini G. Multiple Myeloma Impairs Bone Marrow Localization of Effector Natural Killer Cells by Altering the Chemokine Microenvironment. Cancer Res. 2015;75:4766–4777. doi: 10.1158/0008-5472.CAN-15-1320. [DOI] [PubMed] [Google Scholar]
- 218.Dhodapkar M.V., Geller M.D., Chang D.H., Shimizu K., Fujii S., Dhodapkar K.M., Krasovsky J. A reversible defect in natural killer T cell function characterizes the progression of premalignant to malignant multiple myeloma. J. Exp. Med. 2003;197:1667–1676. doi: 10.1084/jem.20021650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Horenstein A.L., Quarona V., Toscani D., Costa F., Chillemi A., Pistoia V., Giuliani N., Malavasi F. Adenosine Generated in the Bone Marrow Niche Through a CD38-Mediated Pathway Correlates with Progression of Human Myeloma. Mol. Med. 2016;22:694–704. doi: 10.2119/molmed.2016.00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lappas C.M., Rieger J.M., Linden J. A2A adenosine receptor induction inhibits IFN-gamma production in murine CD4+ T cells. J. Immunol. 2005;174:1073–1080. doi: 10.4049/jimmunol.174.2.1073. [DOI] [PubMed] [Google Scholar]
- 221.Stagg J., Divisekera U., Duret H., Sparwasser T., Teng M.W., Darcy P.K., Smyth M.J. CD73-deficient mice have increased antitumor immunity and are resistant to experimental metastasis. Cancer Res. 2011;71:2892–2900. doi: 10.1158/0008-5472.CAN-10-4246. [DOI] [PubMed] [Google Scholar]
- 222.Young A., Ngiow S.F., Gao Y., Patch A.M., Barkauskas D.S., Messaoudene M., Lin G., Coudert J.D., Stannard K.A., Zitvogel L., et al. A2AR Adenosine Signaling Suppresses Natural Killer Cell Maturation in the Tumor Microenvironment. Cancer Res. 2018;78:1003–1016. doi: 10.1158/0008-5472.CAN-17-2826. [DOI] [PubMed] [Google Scholar]
- 223.Zarek P.E., Huang C.T., Lutz E.R., Kowalski J., Horton M.R., Linden J., Drake C.G., Powell J.D. A2A receptor signaling promotes peripheral tolerance by inducing T-cell anergy and the generation of adaptive regulatory T cells. Blood. 2008;111:251–259. doi: 10.1182/blood-2007-03-081646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Horenstein A.L., Bracci C., Morandi F., Malavasi F. CD38 in Adenosinergic Pathways and Metabolic Re-programming in Human Multiple Myeloma Cells: In-tandem Insights From Basic Science to Therapy. Front. Immunol. 2019;10:760. doi: 10.3389/fimmu.2019.00760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Horenstein A.L., Chillemi A., Zaccarello G., Bruzzone S., Quarona V., Zito A., Serra S., Malavasi F. A CD38/CD203a/CD73 ectoenzymatic pathway independent of CD39 drives a novel adenosinergic loop in human T lymphocytes. Oncoimmunology. 2013;2:e26246. doi: 10.4161/onci.26246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Yang R., Elsaadi S., Misund K., Abdollahi P., Vandsemb E.N., Moen S.H., Kusnierczyk A., Slupphaug G., Standal T., Waage A., et al. Conversion of ATP to adenosine by CD39 and CD73 in multiple myeloma can be successfully targeted together with adenosine receptor A2A blockade. J. Immunother Cancer. 2020;8 doi: 10.1136/jitc-2020-000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Rebmann V., Schütt P., Brandhorst D., Opalka B., Moritz T., Nowrousian M.R., Grosse-Wilde H. Soluble MICA as an independent prognostic factor for the overall survival and progression-free survival of multiple myeloma patients. Clin. Immunol. 2007;123:114–120. doi: 10.1016/j.clim.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 228.Groh V., Wu J., Yee C., Spies T. Tumour-derived soluble MIC ligands impair expression of NKG2D and T-cell activation. Nature. 2002;419:734–738. doi: 10.1038/nature01112. [DOI] [PubMed] [Google Scholar]