Abstract
Background
The time dedicated to teaching gross anatomy, including cadaveric dissection, has been decreasing in North American medical schools. The impact of this trend on surgical residency applications is unknown. We sought to identify trends in surgical residency applications in Canada and to determine if medical schools with more gross anatomy instruction and mandatory cadaveric dissection produced more applicants ranking surgical residency programs as their first choice.
Methods
Canadian Resident Matching Service (CaRMS) data from 1997 to 2016 were analyzed. A questionnaire was distributed to Canadian medical schools requesting current and historic information on their anatomy curricula and the number of hours of anatomy instruction.
Results
The survey response rate was 35% (6 of the 17 Canadian medical schools responded); partial data were available for 16 (94%) of the 17 Canadian medical schools. A total of 4.3% of graduating students ranked general surgery as their first choice in the CaRMS match and 17.2% ranked any surgical program first. Over time, the percentage of graduating students who ranked surgical programs as their first choice decreased (p < 0.001). Three schools were significantly more likely than the others to produce graduates ranking general surgery as their first choice. Between 2012 and 2016 the percentage of graduating students ranking surgical programs first was significantly higher (2.2%, p = 0.024) in schools with mandatory cadaver dissection. There was no correlation between the number of hours of gross anatomy instruction and the percentage of graduates ranking any surgical program or a general surgical program first.
Conclusion
The number of applications to surgical programs has decreased in Canada over the past 20 years. Certain schools are more likely than others to produce graduates ranking general surgery as their first choice. Programs with mandatory cadaver dissection produced more graduates favouring surgical programs.
Abstract
Contexte
Le temps alloué à l’enseignement de l’anatomie macroscopique, y compris la dissection cadavérique, est en baisse dans les facultés de médecine nord-américaines. Les répercussions de cette tendance sur le nombre de demandes dans les programmes de résidence en chirurgie sont encore inconnues. Nous avons cherché à dégager des tendances concernant les demandes aux programmes de résidence en chirurgie au Canada et à déterminer si les facultés de médecine intégrant une plus grande proportion d’enseignement de l’anatomie macroscopique et de dissection cadavérique obligatoires produisaient plus de candidats indiquant la résidence en chirurgie comme premier choix.
Méthodes
Nous avons analysé les données du Service canadien de jumelage des résidents (CaRMS) de 1997 à 2016. Un questionnaire recueillant les données actuelles et historiques sur la matière enseignée en anatomie et le nombre d’heures d’enseignement consacrées à la discipline a été distribué aux facultés de médecine canadiennes.
Résultats
Le taux de réponse au sondage était de 35 % (6 des 17 facultés de médecine canadiennes ont répondu), et des données partielles ont été recueillies pour 16 (94 %) des 17 facultés. Au total, 4,3 % des finissants ont mis la chirurgie générale comme premier choix au jumelage du CaRMS, et 17,2 % ont mis un programme de chirurgie comme premier choix. Le pourcentage de finissants ayant mis les programmes chirurgicaux comme premier choix a diminué avec le temps (p < 0,001). Trois écoles étaient toutefois significativement plus susceptibles que les autres de produire des étudiants indiquant la chirurgie générale comme premier choix. Entre 2012 et 2016, le pourcentage d’étudiants inscrivant un programme chirurgical comme premier choix était significativement plus élevé (2,2 %, p = 0,024) dans les facultés ayant des dissections cadavériques obligatoires. Aucune corrélation n’a été observée entre le nombre d’heures d’enseignement de l’anatomie macroscopique et le pourcentage d’étudiants mettant un programme chirurgical comme premier choix.
Conclusion
Le nombre de demandes pour les programmes chirurgicaux est en baisse au Canada depuis les 20 dernières années. Certaines écoles sont toutefois plus susceptibles que les autres de produire des finissants indiquant la chirurgie générale comme premier choix de programme de résidence. Les programmes intégrant la dissection cadavérique obligatoire produisent plus d’étudiants choisissant les programmes chirurgicaux pour la résidence.
Anatomy education has long been regarded as an essential part of the medical curriculum. Traditionally, cadaver dissection has been at the core of anatomy education. In fact, the word “anatomy” is derived from the Greek word for “cutting up,” and it is a commonly held belief that cadaver dissection is “the most universal and recognizable step in becoming a doctor.”1
In the early 1900s in most American medical schools, between 800 and 1000 hours of lectures and laboratory courses were dedicated to gross anatomy, accounting for approximately one-fifth of the entire curriculum. In 1923, the Association of American Medical Colleges recommended that the time allocated to anatomy be restricted; however, the average number of curriculum hours remained greater than 700 into the 1930s. Rapid changes in medical curricula began in the 1990s, emphasizing basic biomedical science and social determinants of health.2
The hours devoted to instruction in gross anatomy, including cadaver dissection, have been declining steadily. Just over half of American medical schools still offer cadaver dissection in their curricula.2 There is a lack of objective data on the effectiveness of cadaver dissection as a teaching method,3 and the implications of declining instruction in gross anatomy are unknown. Indeed, there have been no studies published on the current state of anatomy instruction in medical curricula in Canada. Although the need for expertise in anatomy seems evident for surgical residents, data to support anatomy training in medical school are lacking.
Applications to all residency programs in Canada are facilitated through the Canadian Resident Matching Service (CaRMS), a centralized application service and matching algorithm that provides applicants and programs with the highest likelihood of matching participants to their desired selections.4 Applications to surgical residency programs in Canada have been declining. From 2002 to 2013, family medicine programs experienced significant increases in first-choice applications while programs in general surgery, neurosurgery, orthopedic surgery, otolaryngology, plastic surgery and urology all saw decreases in the average number of first-choice applications.5 The reasons for this decline are not fully understood, but it has been postulated that decreasing surgical experiences in medical school and applicants’ preference for more lifestyle-friendly specialties are contributing factors.6,7 Among the many factors that have been associated with choice of specialty, length of residency, the desirability of the lifestyle associated with the specialty, working hours, financial considerations, the timing of surgical clerkship rotations and early exposure to positive role models are pertinent to students’ decisions to pursue surgical careers.8–10 Experience with gross anatomy instruction in general and cadaver dissection in particular has not been studied as a possible motivator for pursuing a surgical career.
We hypothesized a priori that schools with more time dedicated to gross anatomy teaching, in particular cadaveric dissection, produced more applicants ranking surgical residency positions as their first choice. Our objective was to analyze 20 years of CaRMS residency matching data with respect to the anatomy teaching approaches used in all Canadian medical schools. We also sought to examine the trend in medical school graduates’ choice of surgical disciplines for their residency over the last 2 decades.
Methods
Study design
We conducted a retrospective study of CaRMS residency matching data and a cross-sectional survey of Canadian medical schools. We analyzed CaRMS data from first-year resident match reports from 1997 to 2016. Matching data were obtained from the publicly available online CaRMS database.4 Data were organized by year and by school.
An original questionnaire was distributed to each Canadian medical school requesting information on the institution’s anatomy teaching methods and the number of hours devoted to anatomy instruction over the past 20 years. To maximize response rates, the questionnaire was sent by email to the dean of each medical school and the head of the anatomy department. For questionnaire details see Appendix 1, available at canjsurg.ca/019218-a1. A group of 5 clinicians and methodologists (T.S., S.E., F.F., A.A.-C., K.K.) reviewed the questionnaire for face and content validity before it was distributed to the medical schools. A French version was included for schools in Quebec. Nonresponders were contacted a second time by email and then by phone. When we were unable to obtain a response to our questionnaire, we used results from a related study being conducted by the Department of Anatomy at McMaster University that was examining curriculum hours in gross anatomy, embryology and histology across Canadian medical schools.11
Historic data about hours of anatomy instruction overall and cadaver dissection in particular were not sufficient for robust analysis, but data for 2016 were available for 94% of schools. In light of this, we selected the most recent 5-year cohort of graduates (2012–2016) for our statistical analysis regarding the association between anatomy education (mandatory cadaver dissection and hours of gross anatomy instruction overall) and surgical residency applications.
Statistical analysis
Descriptive statistics were performed. The mean, standard deviation (SD), median, minimum and maximum were calculated for the percentage of graduating students ranking general surgery and any surgical program as their first choice. Multivariable generalized linear regression was performed to compare the mean percentage of graduates ranking surgical residency programs as their first choice. The model included university attended as the independent variable of interest. Year was included to adjust for the potential confounding effect of graduation year. Mandatory cadaver dissection was not included as a variable, as this information was not reliably available for most schools before 2011/12. The Tukey test was used for pair-wise mean comparisons. Adjusted means and 95% confidence intervals (CIs) were reported. Information on the presence of mandatory cadaver dissection and mean hours of gross anatomy instruction collected on the questionnaire was applied for the latest 5-year cohort of graduates (2012–2016). We used t tests to compare the mean percent rankings between universities. We used Pearson correlation analysis to correlate the percent rankings and mean hours of gross anatomy instruction. A p value of 0.05 was considered statistically significant. SPSS version 25.0 (IBM) was used for data analysis.
Results
The response rate for the survey was 35%; complete questionnaires were received from 6 of the 17 medical schools in Canada. Data on cadaver dissection were available for 16 of the 17 schools (94%), and data on gross anatomy hours were available for 12 schools (71%). The mean number of hours dedicated to gross anatomy instruction in 2016 was 97.0 (SD 35.5) and the median number of hours was 97.5 (range 47.0–159.0) (Table 1). Overall, cadaver dissection was mandatory in 50% of schools.
Table 1.
Amount of gross anatomy instruction at participating Canadian medical schools in 2016
| University | No. of hours, mean |
|---|---|
| Memorial University of Newfoundland | 47 |
| Dalhousie University | 81 |
| Université Laval | NA |
| Université de Sherbrooke | NA |
| Université de Montréal | NA |
| McGill University | 96 |
| University of Ottawa | 51 |
| Queen’s University | 58 |
| Northern Ontario School of Medicine | 80 |
| University of Toronto | 150 |
| McMaster University | 114 |
| Western University | 125 |
| University of Manitoba | NA |
| University of Saskatchewan | 102 |
| University of Alberta | 159 |
| University of Calgary | NA |
| University of British Columbia | 100 |
NA = not applicable.
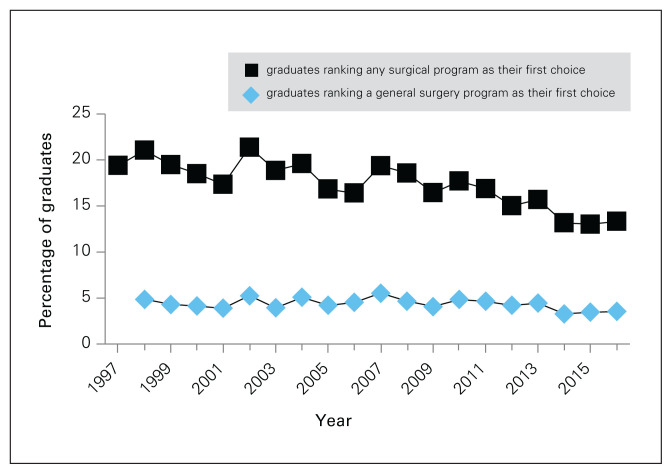
Between 1997 and 2016, 17.2% of graduating students ranked a surgical program as their first choice in the CaRMS match, and 4.3% ranked general surgery as their first choice (Fig. 1). Over time, the percentage of graduating medical students ranking any surgical program as their first choice decreased (p < 0.001), but the percentage of students ranking general surgery first did not change (p = 0.25).
Fig. 1.
Percentage of graduating students who ranked any surgical program or a general surgery program as their first choice, by year.
When we adjusted the results for year, the Northern Ontario School of Medicine was the least likely to produce graduating students ranking general surgery first (p = 0.008) (Table 2) and it had the smallest percentage of graduates ranking surgical programs first (adjusted mean 6.2%, p = 0.004) (Table 3). Three programs produced significantly more graduates who ranked general surgery first than the other schools: Western University (p < 0.001), McGill University (p < 0.001) and the University of Toronto (p < 0.026) (Table 2). In addition to the Northern Ontario School of Medicine, the schools that had the smallest percentages of graduates ranking surgical programs first were Université de Montréal (adjusted mean 13.0%, p = 0.49), McMaster University (adjusted mean 13.5%, p = 0.33) and Université Laval (adjusted mean 14.9%, p = 0.69).
Table 2.
Mean percentage of medical school graduates ranking general surgery first, adjusted for year, and coefficient from generalized regression model*
| University | Adjusted mean % (95% CI)† | Coefficient (95% CI)‡ | Coefficient p value |
|---|---|---|---|
| Memorial University of Newfoundland | 4.25 (3.52 to 4.97) | 0.02 (−0.06 to 0.11) | 0.54 |
| Dalhousie University | 3.77 (3.04 to 4.50) | −0.02 (−0.109 to 0.06) | 0.56 |
| Université Laval | 3.55 (1.97 to 5.13) | 0.05 (−0.27 to 0.13) | 0.59 |
| Université de Sherbrooke | 5.00 (3.42 to 6.57) | 0.10 (−0.07 to 0.28) | 0.25 |
| Université de Montréal | 4.74 (3.16 to 6.32) | 0.08 (−0.10 to 0.25) | 0.39 |
| McGill University | 5.90 (5.17 to 6.62) | 0.20 (0.12 to 0.28) | < 0.001 |
| University of Ottawa | 3.82 (3.10 to 4.55) | −0.02 (−0.10 to 0.06) | 0.65 |
| Queen’s University | 4.32 (3.59 to 5.04) | 0.03 (−0.05 to 0.12) | 0.43 |
| Northern Ontario School of Medicine | 0.47 (−2.03 to 2.97) | −0.37 (−0.65 to 0.01) | 0.008 |
| University of Toronto | 4.90 (4.17 to 5.62) | 0.09 (0.01 to 0.18) | 0.026 |
| McMaster University | 3.62 (2.90 to 4.35) | −0.04 (−0.12 to 0.04) | 0.34 |
| Western University | 6.26 (5.53 to 6.98) | 0.24 (0.15 to 0.32) | < 0.001 |
| University of Manitoba | 3.98 (3.25 to 4.70) | −0.00 (−0.08 to 0.08) | 0.94 |
| University of Saskatchewan | 4.33 (3.61 to 5.06) | 0.03 (−0.05 to 0.12) | 0.41 |
| University of Alberta | 4.36 (3.63 to 5.08) | 0.04 (−0.46 to 0.12) | 0.38 |
| University of Calgary | 3.84 (3.11 to 4.57) | −0.02 (−0.10 to 0.06) | 0.69 |
| University of British Columbia | 3.69 (2.96 to 4.41) | −0.03 (−0.11 to 0.05) | 0.44 |
CI = confidence interval.
The overall year-adjusted mean percentages of graduates ranking general surgery first among universities were significantly different (p < 0.001).
The adjusted mean represents the overall mean percentage of graduates’ rankings by school adjusted for year.
The coefficient represents the mean yearly increase in percent rankings in each school starting in 1997.
Table 3.
Mean percentage of medical school graduates ranking any surgical program first, adjusted for year, and coefficient from generalized regression model*
| University | Adjusted mean % (95% (CI)† | Coefficient (95% CI)‡ | Coefficient p value |
|---|---|---|---|
| Memorial University of Newfoundland | 16.3 (14.9 to 17.7) | 0.21 (0.05 to 0.37) | 0.008 |
| Dalhousie University | 17.6 (16.2 to 19.0) | 0.34 (0.18 to 0.50) | < 0.001 |
| Université Laval | 14.9 (11.6 to 18.2) | 0.07 (−0.28 to 0.43) | 0.69 |
| Université de Sherbrooke | 17.9 (14.6 to 21.2) | 0.37 (0.01 to 0.72) | 0.041 |
| Université de Montréal | 13.0 (9.7 to 16.3) | −0.12 (−0.48 to 0.23) | 0.49 |
| McGill University | 20.9 (19.4 to 22.3) | 0.67 (0.52 to 0.83) | < 0.001 |
| University of Ottawa | 16.1 (14.7 to 17.6) | 0.20 (0.04 to 0.35) | 0.014 |
| Queen’s University | 19.5 (18.1 to 20.9) | 0.54 (0.38 to 0.69) | < 0.001 |
| Northern Ontario School of Medicine | 6.2 (0.99 to 11.5) | −0.81 (−1.6 to −0.25) | 0.004 |
| University of Toronto | 19.1 (17.7 to 20.5) | 0.50 (−0.40 to 0.70) | < 0.001 |
| McMaster University | 13.5 (12.1 to 14.9) | −0.07 (−0.23 to 0.08) | 0.33 |
| Western University | 19.6 (18.2 to 21.0) | 0.54 (0.39 to 0.70) | < 0.001 |
| University of Manitoba | 15.8 (14.4 to 17.2) | 0.16 (0.00 to 0.31) | 0.045 |
| University of Saskatchewan | 19.1 (17.7 to 20.6) | 0.50 (0.34 to 0.65) | < 0.001 |
| University of Alberta | 16.1 (14.7 to 17.6) | 0.20 (0.40 to 0.35) | 0.015 |
| University of Calgary | 16.6 (15.2 to 18.0) | 0.24 (0.08 to 0.40) | 0.003 |
| University of British Columbia | 16.8 (15.4 to 18.2) | 0.26 (0.11 to 0.42) | 0.001 |
CI = confidence interval.
The overall year-adjusted mean percentages of graduates ranking surgery first among universities were significantly different (p < 0.001).
The adjusted mean represents the overall mean percentage of graduates’ rankings by school adjusted for year.
The coefficient represents the mean yearly increase in percent rankings in each school starting in 1997.
The presence of mandatory cadaver dissection at the school of graduation, as indicated in the 2017 survey, was applied to the cohort of graduates from 2012 to 2016. The percentage of graduating students who ranked general surgery first was not higher for schools with mandatory cadaver dissection. However, the percentage of graduating students who ranked any surgical program first was 2.2% higher (95% CI 0.30% to 4.07%, p = 0.024) among graduates of schools with mandatory cadaver dissection than among graduates of schools without mandatory cadaver dissection. The number of graduates ranking general surgery (r = 0.73, p = 0.58) or any surgical program (r = 0.011, p = 0.93) first did not correlate with mean hours of gross anatomy instruction for the 2012–2016 cohort.
Discussion
To our knowledge, the relationship between anatomy education during medical school and students’ ranking of surgical residency programs has never been explored. This study provides insights into the evolving landscape of medical education in Canada and sheds light on potential implications of eliminating mandatory dissection from medical school curricula. Our study findings indicate that applications to surgical programs have been decreasing and that certain medical schools are more likely than others to produce graduates ranking general surgery as their first choice. We also identified a trend in which programs with mandatory cadaver dissection produced more surgical applicants between 2012 and 2016. Given the scrutiny that match rates are currently receiving and the issues associated with unmatched students and the ever-changing job market, studies that further our understanding of factors influencing students’ match rankings will become increasingly valuable. Although this study was not designed to detect causation, it did identify several interesting trends that warrant further study.
The extent of anatomy education in medical school has been diminishing over time, and there continues to be much debate about the optimal method of teaching anatomy.12 Canadian medical schools dedicated a mean of 97.0 hours to gross anatomy instruction in 2016. In contrast, in an American study, Drake and colleagues reported a mean of 149 hours in 2009. Cadaver dissection is mandatory in only 50% of Canadian medical schools and 58% of American medical schools.2 A previous study found that 99% of American general surgery residency program directors who responded to a survey believed gross anatomy knowledge was either very important or extremely important for their incoming residents. Only 14% of these program directors felt their incoming residents had adequate gross anatomy knowledge, 62% believed they needed a refresher and 24% believed they were seriously lacking in their anatomic knowledge.13 With our questionnaire we attempted to gauge how curricula have evolved over time; however, many responses were incomplete and therefore inadequate for robust analysis. Subjectively, several schools described changing from lecture-based hours to a more integrated approach incorporating anatomy teaching into interactive sessions such as problem-based learning or e-modules. This made it difficult to quantify the total number of hours of dedicated anatomy instruction and limited our ability to make meaningful comparisons between curricula.
Identifying the percentage of graduating students ranking particular programs first can be a useful way for medical schools to identify trends among their graduating cohorts. We demonstrated that on average, 17.2% of graduates of Canadian medical schools rank surgical programs first and 4.3% rank general surgery first. Surgical residency programs included cardiac surgery, general surgery, neurosurgery, ophthalmology, orthopedic surgery, otolaryngology — head and neck surgery, plastic surgery, urology and vascular surgery. Obstetrics and gynecology was not considered a surgical program in this study based on the published CaRMS data. It is interesting that the percentage of graduates ranking general surgery first did not change significantly over the study period but the percentage of graduates ranking any surgical program first decreased. Each surgical and medical specialty can be analyzed independently using the CaRMS data if programs wish to study trends in their specialty.
Our results indicate that among Canadian medical schools there were 3 schools that produced significantly more graduates who ranked general surgery first than the other schools (Western University, McGill University and the University of Toronto). Cadaver dissection continues to be mandatory at these schools, and in general they are considered to emphasize more traditional medical curricula. Examining other differences in school curricula, such as length and timing of surgical clerkship or preclerkship surgical exposure, was beyond the scope of this study but probably would have influenced students’ career choices. In 2015, the University of Toronto had 95 mandatory hours of cadaver dissection alone, which is nearly equal to the mean number of hours of total gross anatomy instruction by all methods combined across Canadian schools. Université de Sherbrooke was similar to these 3 schools in producing graduates ranking general surgery first but the comparison did not reach statistical significance.
To attempt to identify trends, we examined a cohort of students graduating in 2012–2016. We chose this cohort because these students represented the group enrolled in medical school during the years corresponding to our questionnaire data. There was no correlation between mean number of hours of gross anatomy instruction and the percentage of graduates ranking any surgical program or a general surgery program first. The percentage of graduating students ranking surgical programs as their first choice was 2.2% higher among graduates of schools with mandatory cadaver dissection than among graduates of schools that did not have mandatory cadaver dissection. This supports the observation that schools that have mandatory cadaver dissection may produce more surgical residents than those that do not. Nevertheless, our study cannot comment on a cause-and-effect relationship and further study is ongoing to survey current surgical residents on the factors that influenced their ranking of surgical programs and elucidate if exposure to anatomy instruction in general or cadaver dissection in particular was a key factor.
A previous analysis of Canadian match data showed a decline in first-choice applications to surgical specialties, including general surgery, from 1996 to 2001.8 Our data support this in terms of surgical programs as a whole, but we found that interest in general surgery remained relatively constant over our study period. A similar trend has been documented in the United States, where surgical applications have decreased and the field of surgery has become an increasingly unappealing specialty.10 Top-tier medical students have also been found to be more likely to enrol in residency programs that are perceived to be more lifestyle friendly than surgical programs or have “controllable” lifestyles.”14
Limitations
This study was limited by the fact that we were not able to obtain complete historical data from the medical schools. All survey respondents were able to provide current information on their anatomy programs, but many could not give detailed data regarding their curricula in the past. Historical data are not kept in a database and therefore any data obtained through surveys will have some degree of recall bias. This made it impossible to examine the relationships between the total number of hours of gross anatomy instruction, the presence of mandatory cadaver dissection and the percentage of graduates ranking surgical programs first over the desired 20-year time frame. Further limitations included smaller sample sizes for the Northern Ontario School of Medicine because its first graduating cohort entered the CaRMS match in 2009. Moreover, the French-language universities in Quebec participated in the match for the first time in 2005. Before this, their results were grouped together into 1 category and were not available for analysis. It was also difficult to quantify the nature of anatomy education as well as the number of dedicated hours in many institutions because of the current trend of replacing formal didactic lectures and dissection laboratory courses with integrated models. Nonmandatory curriculum hours, such as elective time, were not included in the analysis as they varied across schools and were not applicable to all students.
Conclusion
Applications to surgical programs as a whole have decreased in Canada over the past 20 years. Graduates from Western University, McGill University and the University of Toronto are significantly more likely to rank general surgery as their first choice in the CaRMS match than graduates of other Canadian schools. Between 2012 and 2016, programs offering mandatory cadaver dissection produced more graduates ranking surgical programs first, but this correlation was not observed in the general surgery subgroup. There was no correlation between the number of mandatory hours of gross anatomy instruction and the percentage of graduates ranking surgical programs first. Further study is required to understand why these discrepancies exist and if exposure to anatomy education in general and to cadaver dissection in particular plays a role in graduating medical students’ choices to pursue surgical careers.
Footnotes
Presented at the Canadian Surgery Forum, Sept. 13–15, 2018, St. John’s, Nfld.
Competing interests: None declared.
Contributors: T. Schroeder, S. Elkheir, F. Farrokhyar and K. Kahnamoui designed the study. T. Schroeder, S. Elkheir and A. Allard-Coutu acquired the data, which T. Schroeder, S. Elkheir, F. Farrokhyar and K. Khanamoui analyzed. K. Kahnamoui wrote the article, which all authors critically reviewed. All authors approved the final version to be published.
References
- 1.McLachlan JC, Bligh J, Bradley P, et al. Teaching anatomy without cadavers. Med Educ. 2004;38:418–24. doi: 10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 2.Drake RL, McBride JM, Lachman N, et al. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2:253–9. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]
- 3.Winkelmann A. Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ. 2007;41:15–22. doi: 10.1111/j.1365-2929.2006.02625.x. [DOI] [PubMed] [Google Scholar]
- 4.Canadian Resident Matching Service. R-1 data and reports. Ottawa: Canadian Resident Matching Service; 2018. [accessed 2018 Mar. 23]. Available: www.carms.ca/data-reports/r1-data-reports/ [Google Scholar]
- 5.Austin RE, Wanzel KR. Supply versus demand: a review of application trends to Canadian surgical training programs. Can J Surg. 2015;58:143–4. doi: 10.1503/cjs.006614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall DC, Salciccioli JD, Walton SJ, et al. Medical student experience in surgery influences their career choices: a systematic review of the literature. J Surg Educ. 2015;72:438–45. doi: 10.1016/j.jsurg.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Eckleberry-Hunt J, Tucciarone J. The challenges and opportunities of teaching “Generation Y”. J Grad Med Educ. 2011;3:458–61. doi: 10.4300/JGME-03-04-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marschall JG, Karimuddin AA. Decline in popularity of general surgery as a career choice in North America: review of postgraduate residency training selection in Canada, 1996–2001. World J Surg. 2003;27:249–52. doi: 10.1007/s00268-002-6642-8. [DOI] [PubMed] [Google Scholar]
- 9.Erzurum VZ, Obermeyer RJ, Fecher A, et al. What influences medical students’ choice of surgical careers. Surgery. 2000;128:253–6. doi: 10.1067/msy.2000.108214. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt LE, Cooper CA, Guo WA. Factors influencing US medical students’ decision to pursue surgery. J Surg Res. 2016;203:64–74. doi: 10.1016/j.jss.2016.03.054. [DOI] [PubMed] [Google Scholar]
- 11.Rockarts J, Wainman B, Shali A, et al. Anatomy in medical education: a Canadian review [abstract] FASEB J. 2019;33(1 Suppl) [Google Scholar]
- 12.Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl. 2007;89:104–7. doi: 10.1308/003588407X168244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cottam WW. Adequacy of medical school gross anatomy education as perceived by certain postgraduate residency programs and anatomy course directors. Clin Anat. 1999;12:55–65. doi: 10.1002/(SICI)1098-2353(1999)12:1<55::AID-CA8>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz RW, Jarecky RK, Strodel WE, et al. Controllable lifestyle: a new factor in career choice by medical students. Acad Med. 1989;64:606–9. [PubMed] [Google Scholar]