Highlights
-
•
Midgut volvulus related to adult intestinal malrotation found with weight loss is rare.
-
•
The development of collateral circulation from SMV to portal vein did not lead to intestinal necrosis.
-
•
It’s controversial whether it should be an emergency surgery or an elective surgery.
-
•
In the chronic course, there is a high degree of adhesions, and countermeasures against postoperative ileus are necessary.
-
•
If a patient complains of gastrointestinal symptoms, intestinal malrotation should be raised in the differential diagnosis.
Keywords: Case report, Intestinal malrotation, Midgut volvulus, Weight loss, Collateral vessels, Adult
Abstract
Introduction and importance
The incidence of intestinal malrotation is 1 in 6000 births, and 90% of cases occur within the first year of life. Adult cases are rare, with a reported incidence of 0.2%–0.5% of all cases. The significance of reporting this case is to recognize that some adult-onset cases require surgery even in the absence of intestinal necrosis.
Case presentation
A 36-year-old man was infected with streptococcus and treated with antibiotics. He developed appetite loss and his weight decreased 12 kg in 4 months. His abdomen was flat and soft with no tenderness. A computed tomography scan showed that the horizontal duodenal leg was not anchored to the retroperitoneum. Rotation of the mesentery, which was wrapped around the superior mesenteric artery in a clockwise direction, was observed, suggesting midgut volvulus. We performed emergency surgery and Ladd’s procedure.
Clinical discussion
A previous study reported that the most common symptom in the chronic course of intestinal malrotation was abdominal pain in 41.2% of cases, and weight loss was observed in only 2.6% of patients. The high degree of intestinal adhesion suggests that repeated torsion and release and the development of collateral vessels may have contributed to the asymptomatic course.
Conclusion
Adult-onset intestinal malrotation should be considered as a differential diagnosis in the presence of weight loss and gastrointestinal symptoms. The timing of surgery is still controversial. In chronic cases, severe adhesion might be expected and laparoscopic surgery should be considered carefully.
1. Introduction
The normal bowel rotation is 270°; however, Wang et al. reported that intestinal malrotation can be divided into four types based on the type of rotation [1]: non-rotation, which stops at 90°; malrotation, which stops at 180°; reverse rotation, and paraduodenal hernia. The incidence of intestinal malrotation is 1 in 6000 births [2], and 90% of cases occur within the first year of life because of midgut volvulus [3]. Adult cases are rare, with a reported incidence of 0.2%–0.5% of all cases. Midgut volvulus due to intestinal malrotation is common in infantile cases, but it is estimated to occur in 15% of adult cases [1,4,5]. We report a case of midgut volvulus associated with intestinal malrotation, which was discovered in an adult with a rare complaint of weight loss. The significance of reporting this case is to recognize that some adult-onset cases require surgery, even in the absence of intestinal necrosis. This case report was reported in line with the SCARE criteria [6].
2. Case presentation
A 36-year-old man was referred to our hospital with a chief complaint of weight loss. Four months earlier, he had a streptococcal infection that was treated with antibiotics. Thereafter, he developed anorexia and weight loss (78 kg→66 kg), and then he visited our hospital. However, he had no abdominal pain during the infection or weight loss. There was nothing noteworthy in his medical history, drug history, psychosocial history, or family history. He had no unusual use of alcohol, smoking, or recreational drugs. There were no episodes of recurring abdominal pain in childhood. His height was 172 cm and his body mass index (BMI) was 22.3. He had normal body temperature and no abnormalities in his vital signs. His abdomen was flat and soft with no tenderness. The laboratory data were normal: WBC 4100/μl, RBC 469 × 104/μl, Plt 250 × 103/μl, Neu 45.7%, LDH 129 IU/l, CPK 60 IU/l, and CRP 0.02 mg/dl.
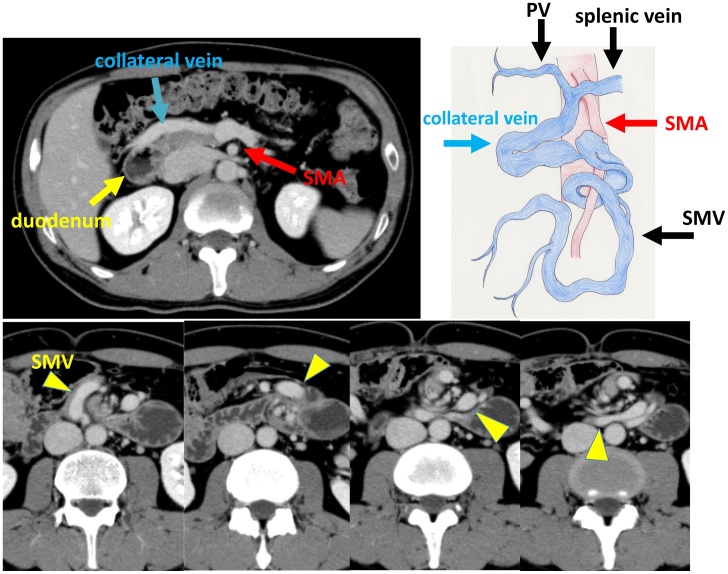
A computed tomography scan was performed and a diagnosis of midgut volvulus was made because of the narrowing of the intestinal tract and the clockwise rotation of the mesentery, as if it were wrapped around the SMA (whirlpool sign). There was a beak sign-like appearance in the small intestine at the torsional area, although the contrast effect of the intestinal wall was preserved without prominent dilatation of the small intestine (Fig. 1). Because of the strong irreversible twisting and a report that massive bowel resection is more likely to be required in cases with midgut volvulus [7], we decided to perform emergency surgery before the intestine became necrotic. We explained the condition and the surgery to the patient and his family, and obtained their consent for the emergency surgery.
Fig. 1.
Axial contrast-enhanced computed tomography images. The horizontal duodenal leg is not anchored to the retroperitoneum and passes through the ventral side of the superior mesenteric artery (SMA). There is clockwise rotation of the mesentery around the SMA and narrowing of the intestine. The main trunk of the superior mesenteric vein (SMV) is disrupted at the tortuosity, and collateral vessels to the portal vein are well developed.
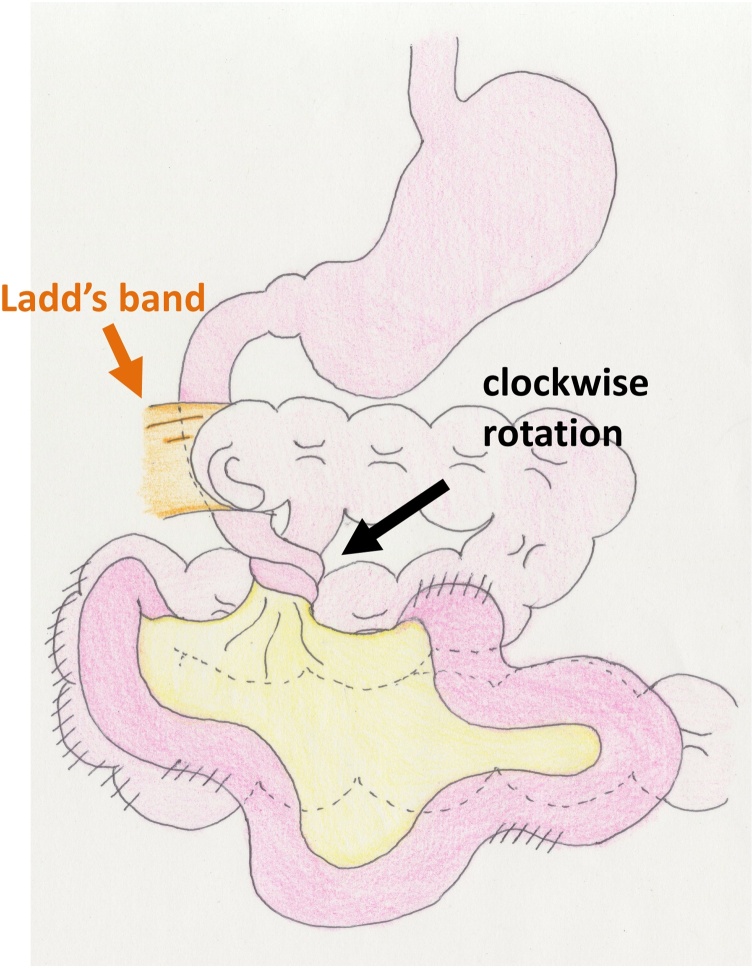
The operator was a board-certified surgeon of the Japan Surgical Society with six years of experience in general surgery. The small intestine had gathered on the right side of the abdomen and the ileocecum presented at the center of the upper abdomen. Fortunately, there were no ischemic changes in the intestine. The superior mesenteric vein (SMV) ended at the volvulus point and thick collateral veins were observed from the SMV to the portal vein. We peeled away the heavy adhesions and divided the Ladd’s band. Then, we repaired the volvulus and expanded the basal mesenteric area (Ladd’s procedure) before performing prophylactic appendectomy (Fig. 2). Finally, the intestinal tracts were of the non-rotation type. The operative time was 147 min and the estimated blood loss was 30 ml.
Fig. 2.
Surgical findings. The ileocecum presented at the center of the upper abdomen, and the Ladd ligament was present. The intestine was highly adherent.
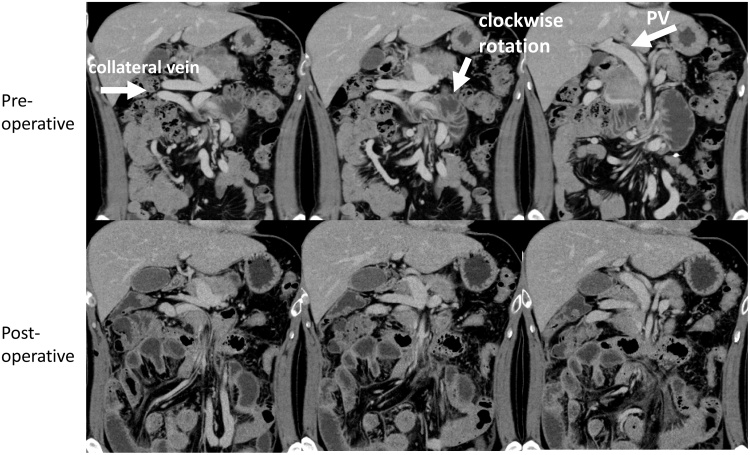
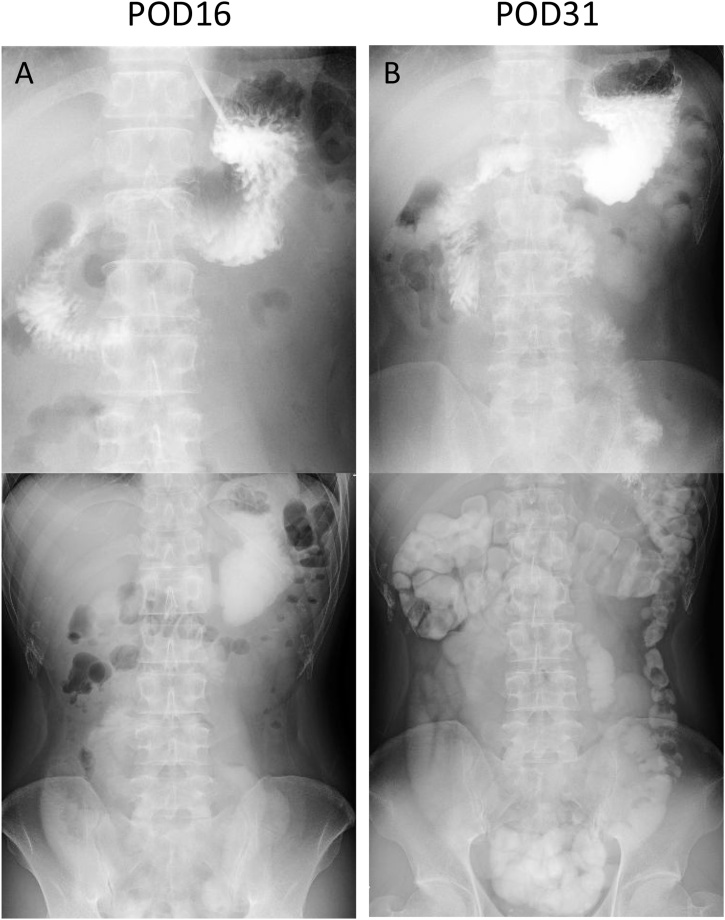
It was expected that after the surgery, the collateral blood vessels would be invisible and the bowel would be untwisted, and that the patient could be discharged rapidly. Comparing pre- and post-operative computed tomography images, the preoperative torsion of the mesentery around the SMA had been released but the collateral vessels remained (Fig. 3). On postoperative day 10, paralytic ileus developed as soon as he started eating, and a gastric tube was reinserted. On postoperative day 16, consecutive X-ray bowel examinations showed that most of the contrast medium remained in the stomach (Fig. 4A). He was able to start enteral feeding from postoperative day 23 and was discharged from the hospital on postoperative day 26 with nutritional supplementation. A consecutive bowel examination on postoperative day 31 showed that the contrast agent had reached the large intestine and he was able to ingest a meal (Fig. 4B). Two years after the operation, he was eating normal food as before, and his body weight recovered to 76 kg.
Fig. 3.
Computed tomography findings during the operation. The preoperative torsion of the mesentery around the superior mesenteric artery axis was removed. The formed collateral vessels were still present.
Fig. 4.
Consecutive bowel examinations. On postoperative day 16, the contrast medium remained in the stomach. On postoperative day 31, the contrast medium has reached the colon.
3. Discussion
Whereas midgut volvulus in infancy presents suddenly with clinical symptoms including bilious vomiting, some adult cases present with an acute onset or with chronic symptoms only. It was reported that adult patients with a chronic course of intestinal malrotation tend to be difficult to diagnose and have a long disease period with a mean age at diagnosis of 38.9 years [8]. Neville et al. reported that the most common symptom in a chronic course was abdominal pain in 41.2% of cases, followed by vomiting in 12.4% of cases. Weight loss was observed in only 2.6% of patients [8]. The asymptomatic and chronic courses in adults might be for the following two reasons. First, the development of adipose tissue in the mesentery of adult patients increases the thickness of the mesentery, so the volvulus is mild. Second, the repetition of midgut volvulus and spontaneous release leads to the development of collateral vessels, making intestinal necrosis less likely to occur.
In the present case, the patient was obese with an original BMI of 26, and his torsion was thought to be mild. However, his infection might have decreased his appetite, resulting in a thinning of the mesenteric fat and a slightly stronger torsion. This might have exacerbated the torsion, which may have led to further anorexia and weight loss. In addition, the high degree of intestinal adhesions suggests that repeated torsion and spontaneous release as well as the development of collateral vessels may have contributed to the asymptomatic course. Necrosis of the intestine due to midgut torsion follows the course of congestion of the venous system, edema of the intestine and mesentery, exacerbation of torsion and strangulation, ischemia of the arteries, and finally, necrosis of the intestine. We think that the development of the collateral circulation prevented the congestion and edema of the intestine, even if the torsion became more severe.
In this case, we decided to perform emergency surgery, but previous studies have reported asymptomatic patients who underwent elective surgery [8,9]. However, once ischemia occurs, massive bowel resection is necessary. Butterworth et al., reported a study on the presence of midgut volvulus, where 19% of cases required bowel resection and the mean resection length was 121 cm [7]. If the torsion is severe, emergency surgery should be considered, even if the patient is asymptomatic. In addition, there is an option to perform the Ladd procedure with open laparotomy or laparoscopy. Laparoscopic surgery for intestinal malrotation with midgut volvulus in neonates was reported to be feasible and safe compared with open surgery [10]. There have been several reports of laparoscopic Ladd's procedure for intestinal malrotation without midgut volvulus in adults [11]. However, in the case of chronic midgut volvulus with intestinal malrotation, it is difficult to perform Ladd’s procedure laparoscopically because of the high number of adhesions.
The patient developed postoperative ileus and had difficulty recovering, which may have been caused by the extensive dissection of adhesions in the abdomen, including the colon. If a high number of adhesions are present at the time of surgery, it might be necessary to consider the creation of an intestinal colostomy for postoperative management, and the administration of drugs to promote intestinal peristalsis.
4. Conclusions
Although adult-onset intestinal malrotation is rare, it should be considered as a differential diagnosis in the presence of weight loss and gastrointestinal symptoms with a chronic course. The timing of surgery in asymptomatic cases of adult intestinal malrotation with midgut volvulus is still controversial. In chronic cases, severe adhesion might be expected. Therefore, laparoscopic surgery should be considered carefully.
Declaration of Competing Interest
All authors declare that there is no financial or personal conflict of interest related to this work.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study was exempted from ethical approval by our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Yuri Higashi: Investigation, Writing – Original Draft, Writing – review and editing.
Ichiro Onishi: Editing manuscript, Writing – review and editing.
Masato Kayahara: Supervision.
Shunsuke Kano: Investigation.
Naoki Makita: Investigation.
Masayoshi Munemoto: Investigation.
Yasumichi Yagi: Investigation.
Registration of research studies
Not applicable.
Guarantor
Masato Kayahara.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgments
We thank J. Ludovic Croxford, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
References
- 1.Wang C., Welch C. Anomalies of intestinal rotation in adolescents and adults. Surgery. 1963;54:839–855. [PubMed] [Google Scholar]
- 2.Fischer J., Bland K. Lippincott Williams and Wilkins; 2007. Mastery of Surgery. [Google Scholar]
- 3.von Flüe M., Herzog U., Ackermann C., Tondelli P., Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis. Colon Rectum. 1994;37:192–198. doi: 10.1007/BF02047549. [DOI] [PubMed] [Google Scholar]
- 4.Torres A.M., Ziegler M.M. Malrotation of the intestine. World J. Surg. 1993;17:326–331. doi: 10.1007/BF01658699. [DOI] [PubMed] [Google Scholar]
- 5.Dietz D.W., Walsh R.M., Broniatowski S.G., Lavery L.C., Fazio V.W., Vogt D.P. Intestinal malrotation: a rare but important cause of bowel obstruction in adults. Dis. Colon Rectum. 2002;45:1381–1386. doi: 10.1097/01.DCR.0000029637.48119.8D. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Butterworth W.A., Butterworth J.W. An adult presentation of midgut volvulus secondary to intestinal malrotation: a case report and literature review. Int. J. Surg. Case Rep. 2018;50:46–49. doi: 10.1016/j.ijscr.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neville J.J., Gallagher J., Mitra A., Sheth H. Adult presentations of congenital midgut malrotation: a systematic review. World J. Surg. 2020;44:1771–1778. doi: 10.1007/s00268-020-05403-7. [DOI] [PubMed] [Google Scholar]
- 9.Moldrem A.W., Papaconstantinou H., Broker H., Megison S., Jeyarajah D.R. Late presentation of intestinal malrotation: an argument for elective repair. World J. Surg. 2008;32:1426–1431. doi: 10.1007/s00268-008-9490-3. [DOI] [PubMed] [Google Scholar]
- 10.Ferrero L., Ahmed Y.B., Philippe P., Reinberg O., Lacreuse I., Schneider A. Intestinal malrotation and volvulus in neonates: laparoscopy versus open laparotomy. J. Laparoendosc. Adv. Surg. Tech. A. 2017;27:318–321. doi: 10.1089/lap.2015.0544. [DOI] [PubMed] [Google Scholar]
- 11.Panda N., Bansal N.K., Narasimhan M., Ardhanari R. Laparoscopic correction of intestinal malrotation in adult. J. Minim. Access Surg. 2014;10:90–92. doi: 10.4103/0972-9941.129961. [DOI] [PMC free article] [PubMed] [Google Scholar]