To the Editor,
Point of care ultrasound (POCUS) is rapidly evolving as a valuable adjunct to bedside clinical examination in nephrology practice [1]. Objective assessment of fluid volume status is a frequent challenge faced by nephrologists and there is accumulating evidence supporting the role of POCUS in this scenario [2]. However, there is no single accurate sonographic application to assess volume status. While sonographic assessment of inferior vena cava (IVC) is popular among novice POCUS users, its isolated use to determine and monitor fluid status is subject to numerous limitations [3]. Similarly, lung ultrasound gives an idea of left-sided filling pressures but does not quantify venous congestion, which can have deleterious consequences in various organ systems including the kidney [4]. Novel scoring systems like venous excess ultrasound grading (VExUS) allow objective assessment of volume status using portal and hepatic venous Doppler waveforms in addition to IVC measurements [5]. Herein, we demonstrate the natural history of these waveforms in a patient with advanced chronic kidney disease (CKD) during the course of ultrafiltration.
A 39-year-old man with a history of CKD stage 5 secondary to diabetic nephropathy presented with generalized weakness, shortness of breath on exertion, worsening leg edema and weight gain despite being compliant with prescribed diuretic therapy. Serum creatinine at presentation was 8.93 mg/dL. He was admitted and initiated on hemodialysis for refractory volume overload. POCUS showed mild pericardial and pleural effusion as well as an enlarged IVC of ~ 3 cm with less than 50% collapse. In addition, Doppler ultrasound demonstrated 100% pulsatility of the portal vein (normal is less than 30%) with systolic flow reversal. Hepatic vein Doppler showed systolic (S) wave reversal and only diastolic (D) wave below the baseline, that is venous return only during ventricular filling. These findings constitute severe venous congestion. While IVC continued to indicate high right atrial pressures, the Doppler waveforms showed parallel improvement with ultrafiltration, showing only mild congestion at the time of discharge. Figures 1 and 2 illustrate the changes in these waveforms. Total amount of ultrafiltration by the time of discharge since initiation of hemodialysis was 13 L. No episodes of intradialytic hypotension occurred.
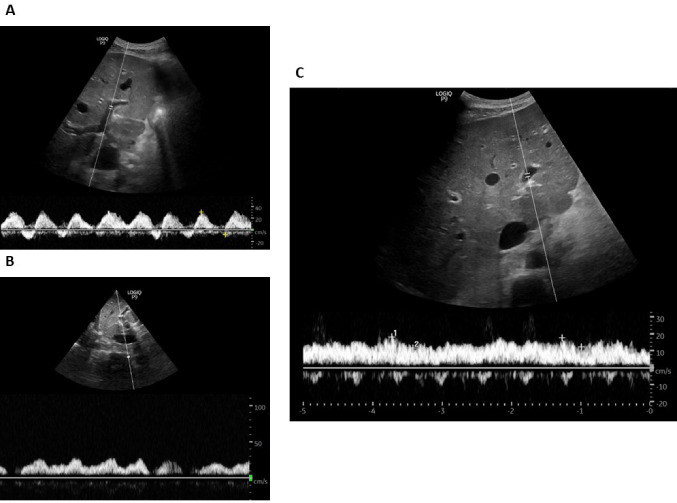
Fig. 1.
a Pulsatile portal vein Doppler waveform at presentation with systolic flow reversal (below the baseline flow); b Portal vein waveform after 6 L ultrafiltration (2 dialysis sessions) showing considerable improvement in pulsatility; c near-normal waveform at discharge (after 13 L ultrafiltration)
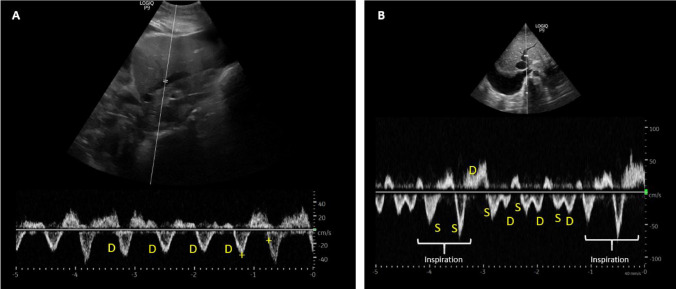
Fig. 2.
Hepatic vein waveform a at presentation demonstrating only D-wave [diastolic] below the baseline; b at discharge showing the appearance of S-wave [systolic] below the baseline. High-amplitude flows are expected during inspiration, but D-wave reversal here indicates poor right ventricular compliance (that is, right atrial pressure not completely normalized)
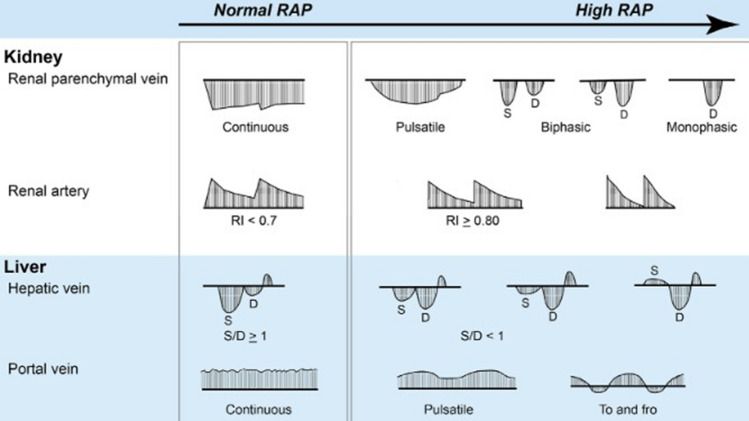
The deleterious effects of venous congestion on abdominal organs are often under-appreciated. For instance, persistent congestion is associated with chronic congestive hepatopathy and progressive decline of glomerular filtration rate in patients with pulmonary hypertension [4]. POCUS enables physicians to non-invasively evaluate the vascular anatomy and blood flow in real time and hence assess organ congestion at the bedside. POCUS-derived venous waveforms aid not only in diagnosing congestion, but also objectively monitoring the effectiveness of decongestive therapy and guiding the amount of ultrafiltration or diuretic dosing. In addition to hepatic and portal vein waveforms, intra-renal vein Doppler waveforms also reflect changes in right atrial pressure (RAP), though higher operator skill is needed to acquire optimal images. The normal pattern is relatively continuous similar to that of portal vein and as the RAP increases, the flow becomes pulsatile and biphasic with distinct S and D waves. Further increases in RAP lead to a monophasic (diastolic only) pattern. Similarly, intra-renal arterial resistive index increases with the degree of congestion. Figure 3 illustrates the qualitative changes in hepatic, portal, and intra-renal vein and arterial waveforms with increasing RAP [6].
Fig. 3.
Qualitative changes seen in Doppler-derived waveforms with increasing right atrial pressure (RAP): Intra-renal vein, intra-renal artery, hepatic, and portal vein patterns are shown. S systolic, D diastolic, RI resistive index. Figure
adapted from reference no. 6 with the kind permission of the publisher
Future research is needed to elucidate whether adding this parameter to traditional physical examination and/or IVC ultrasound to guide therapy leads to improvement in outcomes. Further, whether a personalized ultrafiltration strategy in the outpatient dialysis unit aimed at preventing or reversing portal and hepatic flow alterations reduces the incidence of intradialytic hypotension is another interesting research question. Nonetheless, the ability to perform Doppler ultrasound at the bedside is an important addition to nephrologists’ skill set.
Author contributions
Both the authors have made substantial contribution to the preparation of this manuscript. The authors are solely responsible for the writing and preparation of this manuscript.
Funding
No specific financial support was obtained for preparation of this article.
Compliance with ethical standards
Conflict of interest
The authors have declared that no conflict of interest exists.
Human and animal rights (with IRB approval number)
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Obtained from the patient.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hassanzadeh Rad A, Badeli H. Point-of-care ultrasonography: is it time nephrologists were equipped with the 21st century's stethoscope? Iran J Kidney Dis. 2017;11(4):259–262. [PubMed] [Google Scholar]
- 2.Koratala A, Ronco C, Kazory A. The promising role of lung ultrasound in assessment of volume status for patients receiving maintenance renal replacement therapy. Blood Purif. 2020 doi: 10.1159/000505529. [DOI] [PubMed] [Google Scholar]
- 3.Via G, Tavazzi G, Price S. Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med. 2016;42(7):1164–1167. doi: 10.1007/s00134-016-4357-9. [DOI] [PubMed] [Google Scholar]
- 4.Rosenkranz S, Howard LS, Gomberg-Maitland M, Hoeper MM. Systemic consequences of pulmonary hypertension and right-sided heart failure. Circulation. 2020;141(8):678–693. doi: 10.1161/CIRCULATIONAHA.116.022362. [DOI] [PubMed] [Google Scholar]
- 5.Beaubien-Souligny W, Rola P, Haycock K, et al. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12(1):16. doi: 10.1186/s13089-020-00163-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang WH, Kitai T. Intrarenal venous flow: a window into the congestive kidney failure phenotype of heart failure? JACC Heart Fail. 2016;4(8):683–686. doi: 10.1016/j.jchf.2016.05.009. [DOI] [PubMed] [Google Scholar]