Abstract
There is a current escalating need for telehealth (TH) options in family mental health services. In the absence of replicated evidence, TH guidelines from peak bodies are largely based on assumptions of the effectiveness of TH methods. New investments in TH would optimally be based in evidence of clinical efficacy. To this end, we conducted three studies in which we (1) systematically reviewed eight professional guidelines for TH family therapy, (2) examined replicated evidence for the efficacy of TH family therapy through systematic review of 20 studies and meta-analyses of 13 effects, and (3) synthesised clinical accommodations to TH methodology from a study of 12 experienced TH family therapists. The studies found (1) a predominant focus in existing TH guidelines on operational matters pertaining to TH and relative neglect of therapeutic process; (2) meta-analyses of efficacy for child behavioural problems (k = 8) and parental depression (k = 5) showed equivalent outcomes in TH and face-to-face therapy and enhanced outcomes in TH relative to treatment as usual, resource provision (i.e. written materials), or wait-list control. Narrative review of 20 studies for a range of relational and mental health outcomes aligned with these findings; and (3) therapists defined clear conditions for enhanced engagement and therapeutic process via TH and reflected on cautions and accommodations for purposes of rapport building and mitigating risk. Given moderate-strong evidence for the efficacy of TH methods of family therapy for a range of conditions, we offer recommendations for future implementation of TH for family therapy.
Supplementary Information
The online version of this article (10.1007/s10567-020-00340-2) contains supplementary material, which is available to authorized users.
Keywords: Telehealth, Family therapy, COVID-19, Systematic review, Meta-analysis
Delivery of psychotherapy through synchronous digital or other communication technology, referred to here as telehealth (TH), has been used for some decades to enhance access to care. This delivery format overcomes obstacles to receiving therapy such as geographic distance (Kuulasmaa et al. 2004), lack of access to resources due to financial constraints (Doss et al. 2020; Stuttard et al. 2015), and transport barriers (Syed et al. 2013). In recent months, with the advent of the COVID-19 pandemic, TH use has risen in response to public health restrictions on in-person contact (Aafjes et al. 2020). This has affected multiple modes of therapy, including family therapy, the focus of this paper. In response to the rapid shift to TH delivery, guidance for the provision of family therapy delivered by TH has been sought, including necessary accommodations from in-person to online delivery and use of technology to enhance therapeutic processes. The need to gather evidence for the efficacy of online delivery of family therapy, although previously recognised (Kuulasmaa et al. 2004), has become pressing during the COVID-19 pandemic. This paper addresses knowledge gaps in three ways, by (1) reviewing existing guidelines on the implementation of TH for family therapy, (2) reviewing the replicated evidence for the efficacy of TH in family therapy via systematic review and meta-analytic methods, and (3) describing further refinements for TH delivery of family therapy, through a qualitative study of 12 Family Therapists experienced in TH methods.
Previous research has examined use of TH for other modes of therapy, such as individual psychotherapy. These have included cognitive behaviour therapy (e.g. Lichstein et al. 2013), interpersonal therapy (Heckman et al. 2017), and behavioural activation therapy (Egede et al. 2015). In these contexts, systematic reviews and meta-analyses of trials of TH have established superior outcomes of TH relative to active or wait-list control (Ahern et al. 2018). Importantly, TH-delivered individual psychotherapy has also shown equivalent outcomes to in-person delivered therapy (Ahern et al. 2018; Drago et al. 2016; Norwood et al. 2018).
In contrast to this preliminary evidence-base for TH in individual psychotherapy, review of outcomes for TH in family treatment contexts has yet to be conducted. Caution is needed in extrapolating these findings to support the use of TH in the family therapy setting. Significant differences in the application of TH to family treatment contexts include accommodating more than one person “in the room” and managing the complexity of attending to family and communication dynamics during sessions. In addition, particular techniques used in family therapy add further complexity to the move from in-person to technology, such as use of visual aids including genograms and physically re-positioning family members. These have obvious operational and therapeutic implications for how successfully family therapy may be delivered and received.
The limited literature to date focuses largely on the technical nature of TH delivery, and its possible advantages for family therapy, such as supporting the requirement to not talk over one another, and disadvantages, such as the potential for misunderstanding due to screen resolution limitations (Kuulasmaa et al. 2004). In contrast, impacts on the therapeutic process involved in delivering family therapy via TH have received limited attention.
In this context, we conducted three studies to examine technical and therapeutic considerations for delivering family therapy via TH. Study One aimed to examine current guidelines for TH delivery. Study Two aimed to examine the replicated evidence for the efficacy of TH in family therapy contexts, via a systematic review and meta-analysis. Study Three aimed to summarise the therapeutic processes core to effective TH consultations with families, via analysis of family therapists’ descriptions of effective and ineffective TH consultations.
Study One: Review of Operational and Therapeutic Guidelines for Family Therapy TH
Study One aimed to review available guidelines for delivery of family therapy via TH.
Method
Search Procedure
Grey literature for operational and therapeutic guidelines for TH was searched via the Google search engine on 10 April 2020. The search terms used were “guidelines”, “telehealth”, and “family therapy”. Results from the first 10 pages (100 results) were screened for inclusion. Guidelines were included if they were publicly available and provided advice on the conduct of TH in a therapy setting involving family consultation. One additional resource was sourced on 3 June 2020. Resources were excluded if they were secondary citations from a higher peak body, advertisements, marketing, or individual blogs. Peer-reviewed literature was excluded and examined in the systematic review section of this paper.
Resource Selection
Eight resources providing guidelines or advice for conducting TH in family therapy contexts met inclusion criteria. These are summarised below.
Results
Seven of the eight resources were designed to provide guidance for TH delivery of systemic, family and/or marriage therapy, or therapy with children and adolescents (AAFT 2020; Caldwell et al. 2017; Helps et al. 2020; ILB-MFT 2016; Myers et al. 2017; Rogers 2020; Tran-Lien 2020). One resource was for governing bodies to regulate use of TH (AMFTRB 2016). Four of the eight resources preceded the COVID-19 pandemic, and four were developed specifically in response to escalating need for TH delivery of therapy during the pandemic (AAFT 2020; Helps et al. 2020; Rogers 2020; Tran-Lien 2020).
Guidelines for Operational Arrangements
Ten themes related to operational guidelines were identified, as outlined in Table 1. The most commonly identified themes are summarised below.
Table 1.
Level of detail provided for operational guidelines for Telehealth according to resource source
| Theme | Guideline Document Source | |||||||
|---|---|---|---|---|---|---|---|---|
| AAFT | AAMFT | AMFTRB | ATA | CAMFT | Emerging minds | ILB-MFT | TP-NHSFT | |
| Security | None | Moderate | Detailed | None | None | None | Brief | None |
| Risk/specific populations | None | Brief | Detailed | Detailed | None | None | None | Very brief |
| Consent and documentation | None | Moderate | Detailed | Brief | Moderate | Very brief | Moderate | None |
| Confidentiality | Brief | None | Moderate | None | None | Brief | Brief | Brief |
| Client identify | None | Brief | Moderate | None | None | None | Very brief | None |
| Working with children | None | None | Moderate | Detailed | None | Brief | None | None |
| Platform/devices/access | None | Brief | Moderate | Moderate | Moderate | Brief | None | Moderate |
| Workspace boundaries/room setup | None | None | None | Detailed | None | Brief | None | Moderate |
| Call interruptions | None | Brief | Brief | None | None | None | None | Very brief |
| Recording sessions | None | None | Brief | None | None | None | Very brief | Brief |
AAFT Australian Association of Family Therapy, AAMFT American Association for Marriage and Family Therapists, AMFTRB Association of Marital and Family Therapy Regulatory Boards, ATA American Telemedicine Association, CAMFT California Association of Marriage and Family Therapists, ILB-MFT Idaho Licensing Board of Professional Counselors and Marriage and Family Therapists, TP-NHSFT The Tavistock and Portman NHS Foundation Trust
Technology Requirements for Conducting TH
Six of the eight resources addressed at least one issue concerning platform for TH delivery, device use, access, or how to deal with call interruptions. Recommendations for use of particular platforms were infrequently provided, with greater focus on requirements of the platforms or devices to provide reliable, private, and quality connections (ARFTRB 2016; Caldwell et al. 2017; Helps et al. 2020; Myers et al. 2017; Tran-Lien 2020). Prior testing of platforms and devices was recommended to ensure client(s) could access the TH space (Rogers 2020), and plans be made in advance to deal with call interruptions due to technology failure or connection difficulties (AMFTRB, 2016; Caldwell et al. 2017; Helps et al. 2020). One specified the video image be stable and that all members of families and their interactions, including facial features and expressions, can be viewed (Myers et al. 2017).
Client Consent and Confidentiality
Recommendations on this element of practice were made by most resources. Only two resources attended to prior written consent for recording sessions (AMFTRB 2016; Helps et al. 2020), and others referred to obtaining in situ verbal or written consent for TH (Myers et al. 2017; Tran-Lien 2020). Others provided detailed recommendations on risks and benefits of online therapy, training or credentials of the therapist in delivering TH therapy, privacy settings, alternative communication methods, and emergency procedures (AMFTRB 2016; Caldwell et al. 2017; ILB-MFT (Idaho Licensing Board of Professional Counselors and Marriage and Family Therapists 2016). Two resources noted the need for a confidential space in which to conduct TH, from both the client(s) and therapists’ perspective (AMFTRB 2016; Helps et al. 2020; Rogers 2020). The need to inform clients of the limits or risks to confidentiality from TH delivery was also advised by three resources (AAFT 2020; AMFTRB 2016; ILB-MFT 2016) and to safeguard electronic storage accessible only by authorised persons (AMFTRB 2016; ILB-MFT 2016). A recommendation for security regarding TH platforms and data storage was made by three resources (AMFTRB 2016; Caldwell et al. 2017; ILB-MFT 2016), including for password protection and that encryption be used for the therapists’ electronic communication.
The need to verify client identity was advised by three resources, from noting that the identity of the client(s) should be verified by the TH provider (ILB-MFT 2016), to continuous verification across the period of engagement, through special procedures, such as passwords, codewords, or agreed upon phrases (AMFTRB 2016; Caldwell et al. 2017).
Risk and Client Safety
One resource mentioned the need to assess risk indications that TH may be contra-indicated for some clients (Helps et al. 2020). Three others gave information on emergency planning, including the need to be aware of emergency resources in the client(s) location and to provide written information to the client(s) about emergency procedures (AMFTRB 2016; Caldwell et al. 2017; Myers et al. 2017), and the need to assess for physical risk of harm in the setting/environment in which the client accesses TH. Possible exclusions from TH in unsupervised settings included families with maltreatment histories (Myers et al. 2017).
Children and TH
Somewhat surprisingly, only three resources specifically addressed working with children in the TH setting. Matters addressed included the need for children to be familiarised with technology through game play and exploration of platform features (Rogers 2020), and that consent and identity of the parent or guardian providing the consent be verified (AMFTRB 2016). Myers et al. (2017) made numerous recommendations about supervision of the TH session, safety risks for young people including the potential of the young person to act out and attack devices, and considerations that some children may not tolerate TH due to developmental or psychotic disorders. In addition, conduct of TH in non-neutral settings that may be sites of violence or neglect, or where a volatile caregiver or parent is present were noted contraindications.
Workspace Boundaries and Room Set-Up
Three resources addressed these issues. Recommendations included obscuring the therapist’s background where possible (Rogers 2020) and ensuring clients’ space was free from interruptions, from the risk of being overheard (Helps et al. 2020), and was sufficiently large to accommodate all family members and to allow children to move around as needed (Myers et al. 2017).
Guidelines for Engagement and Therapeutic Processes on TH
Ten themes for therapeutic guidelines were identified (see Table 2). The most frequently mentioned themes are outlined below.
Table 2.
Level of detail provided for therapeutic guidelines for Telehealth according to resource source
| Guideline Document Source | ||||||||
|---|---|---|---|---|---|---|---|---|
| Theme | AAFT | AAMFT | AMFTRB | ATA | CAMFT | Emerging Minds | ILB-MFT | TP-NHSFT |
| Assessment of appropriateness for telehealth | None | Moderate | Moderate | Brief | Brief | Brief | Moderate | None |
| Session structure | Detailed | None | None | None | None | Moderate | None | Brief |
| Rapport and engagement | Moderate | None | None | None | None | Moderate | None | Very brief |
| Visual cues and use of the body | Detailed | None | Moderate | Brief | None | Moderate | None | Moderate |
| Visual tools and genograms | Brief | None | None | None | None | Brief | None | Brief |
| Reflecting conversations | None | None | None | None | None | None | None | Brief |
| Managing emotions | Moderate | None | None | None | None | None | None | Brief |
| Therapist presence / state of mind | Moderate | None | None | None | None | None | None | None |
| Monitoring progress | None | Brief | Brief | None | None | Brief | Brief | None |
| Supervision | None | None | Detailed | Brief | None | None | None | Brief |
| Session Content | None | None | None | None | None | None | None | Detailed |
AAFT Australian Association of Family Therapy, AAMFT American Association for Marriage and Family Therapists, AMFTRB Association of Marital and Family Therapy Regulatory Boards, ATA American Telemedicine Association, CAMFT California Association of Marriage and Family Therapists, ILB-MFT Idaho Licensing Board of Professional Counselors and Marriage and Family Therapists, TP-NHSFT The Tavistock and Portman NHS Foundation Trust
Assessing for Appropriateness for TH
Six guideline documents (AMFTRB 2016; Caldwell et al. 2017; ILB-MFT 2016; Myers et al. 2017; Rogers 2020; Tran-Lien 2020) stated that assessments for appropriateness of TH should be conducted, and based on varying considerations such as the nature and severity of symptoms, clients’ ability to use TH platforms, and risks and benefits of TH-delivered therapy. However, specific thresholds for indicators or contraindicators of use of TH were not provided.
In-Session Communication and Engagement
Issues here included greater concentration demands on therapists and clients of TH relative to in-person work, and acknowledged a possible need to curtail session length (Helps et al. 2020). The need for new rituals was suggested, to signal different stages of the therapy session, such as beginnings and endings (AAFT 2020; Helps et al. 2020). Similarly, different approaches to promoting engagement and rapport and clear communication were advocated (AAFT 2020; Helps et al. 2020; Rogers 2020), for example, through visual cues, variation of voice (i.e. intonation, tempo), and physical signals such as waving or the thumbs-up sign (AAFT 2020; AMFTRB 2016; Helps et al. 2020; Myers et al. 2017; Rogers 2020). The additional need for therapists to maintain attentiveness in sessions given the more effortful nature of TH was also mentioned (AAFT 2020).
Managing Intensity of Emotion and Focus in TH Delivery
Suggested strategies here included setting up a contract that outlines the planned response to escalation of emotion (Helps et al. 2020) and using directive problem-solving approaches to contain distress (AAFT 2020).
Therapist Self-Care
The added utility of supervision and use of technology to facilitate supervision was mentioned by three resources (AMFTRB 2016; Helps et al. 2020; Myers et al. 2017), including sharing of recording of video conference sessions for review by supervisors (Helps et al. 2020)..
Use of Family Therapy Specific Skills and Tools
Only two resources specifically mentioned ongoing use of tools such as use of genograms (AAFT 2020; Helps et al. 2020) and reflecting conversations (Helps et al. 2020).
Monitoring Client(s’) Progress
This issue was included in some guidelines AMFTRB (Association of Marital and Family Therapy Regulatory Boards) 2016; Caldwell et al. 2017; ILB-MFT (Idaho Licensing Board of Professional Counselors and Marriage and Family Therapists) 2016; Rogers 2020. In some instances, these were specific to monitoring the effectiveness and appropriateness of TH delivery of therapy (AMFTRB 2016; Caldwell et al. 2017; ILB-MFT 2016).
Session Content
No guideline implied that the content of a session would be affected by the differences between TH and in-person work. Continued support for the family to set the agenda for the discussion was assumed throughout. One set of guidelines developed post COVID-19 restrictions observed that COVID-19-related topics were frequently raised, and needed time to discuss, including addressing children’s worries about the virus, physical distancing, and contact between parents and children in separated families (Helps et al. 2020).
Brief Discussion
Study One reviewed publicly available documents providing guidelines for provision of TH within family therapy settings. Half of the documents had been produced specifically in response to the COVID-19 pandemic. Perhaps reflecting the rapid move to provision of TH, content of the guidelines documents was heavily weighted to providing operational guidance, including use of technology and processes for obtaining client consent and managing confidentiality. Less attention was given to guidance for adapting therapeutic processes within the TH setting and somewhat surprisingly, few resources attended to ways of working with children in TH in relation to either operational or therapeutic guidelines. No guideline attended to the evidence for effectiveness of TH.
Study Two: Systematic Review and Meta-analysis
The aim of Study Two was to conduct a systematic review of literature examining relational and mental health outcomes of family therapy via TH and, where possible, to conduct meta-analyses of commonly reported outcomes.
Method
This review was conducted in accordance with the preferred reporting items for systematic review and meta-analysis protocols (PRISMA) guidelines for systematic reviews and meta-analysis protocols (Moher et al. 2015).
Search Strategy
A systematic search of the following databases was conducted in April 2020: PsycINFO, CINAHL, FAMILY, ProQuest Psychology Journals, ProQuest Dissertations and Theses, and Google Scholar. Search terms were telemedicine OR telehealth OR “telemental health” OR telepsych* OR ehealth OR edelivery OR online AND “family health services” OR “family therapy” OR “family consult*” OR “clinical consult*” OR “group consult*” AND trial OR “randomi*ed control* trial*” OR “randomi*ed clinical trial*” OR “experimental design” OR “random sampl*” OR “case control”.
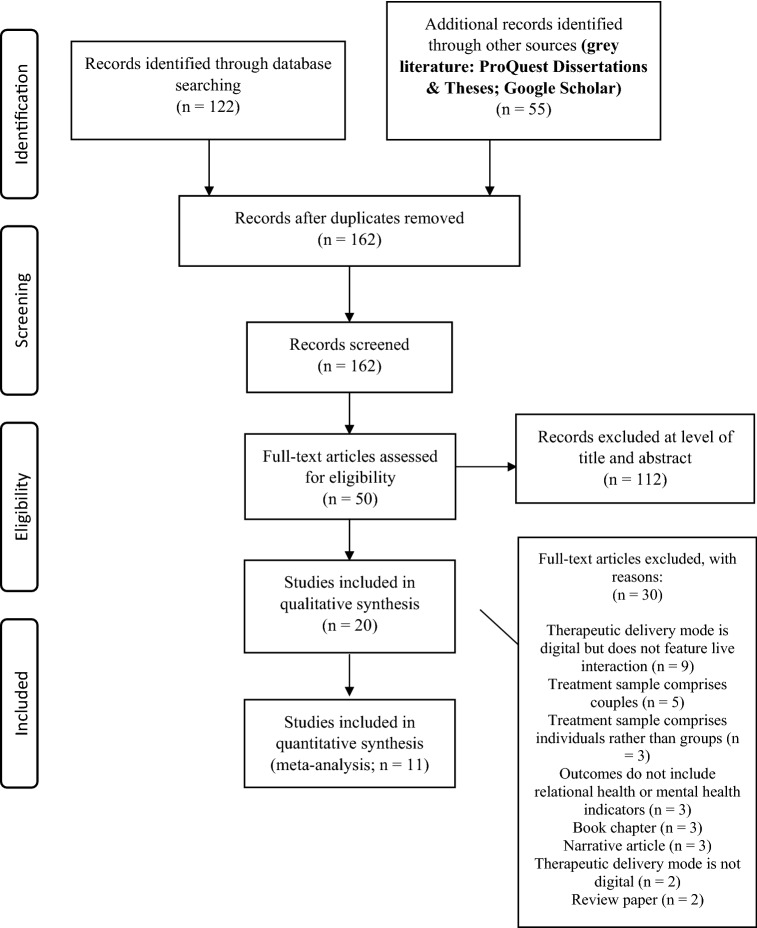
The search was restricted to English language peer-reviewed papers. The ProQuest Dissertations and Theses and Google Scholar searches were not restricted to peer-review literature to allow retrieval of grey literature. Given the large number of records from Google Scholar on irrelevant topics, screening was restricted to the first 50 returns. A total of 177 papers were retrieved. After removal of duplicates (n = 15), 162 papers remained for screening.
Study Selection
All papers (n = 162) were screened for eligibility by two authors (AB and AS) across two levels; title and abstract, and full text. Papers were included if: (a) they reported on a TH based delivery of a therapeutic intervention (i.e. synchronous audio or video consult); (b) the treatment was simultaneously received by more than one client (i.e. was a family or group); and (c) the paper reported on relational health or mental health outcome measures.
The title and abstract screen excluded 112 papers and a further 30 were excluded following full-text screen. Reasons for exclusion at this level are shown in Fig. 1. One additional paper that was already known to the authors was included. Twenty papers met eligibility criteria for inclusion. Of these, 9 reported on effects that were eligible for inclusion in meta-analysis.
Fig. 1.
Selection process of articles for inclusion in review and meta-analyses
Data Extraction
Two authors (AB and AS) extracted data from eligible papers. The data described study country, study design, treatment sample and size, intervention type and delivery formats, relevant outcomes and their measures, relevant results, and reported effect sizes. For meta-analytic categories, pre- and post-intervention means and standard deviations were extracted from studies for effect size calculation.
The quality of included studies was assessed by one author (AS) using the 12-item Methodological Index for Non-Randomized Studies (MINORS) scale (Slim et al. 2003). This scale assesses methodological quality for both non-randomised and controlled studies. Items are scored as 0 (not reported), 1 (reported but inadequate), and 2 (reported and adequate). An ideal score for a randomised controlled study is 24 and 16 for non-comparative studies. Additionally, one item from the Jadad Scale (Jadad et al. 1996) for Reporting Randomised Controlled Trials was included to assess randomisation. Studies received 2 points if described as randomised, and the method of randomisation was described and appropriate. Studies received 1 point if randomisation was mentioned but the method of randomisation was inappropriate. A score of zero was awarded if randomisation was not explicitly mentioned. A second author (AB) assessed 20% of studies for inter-rater reliability of study quality. Scores for each study are included in Supplementary Material.
Meta-analyses
Meta-analyses were possible for two outcomes, child behaviour problems and parent depression. Analyses were conducted using the Comprehensive Meta-Analysis software (Version 3; Borenstein et al. 2005). Effect sizes (Hedges g) were calculated for the interaction effect (between group (control and intervention) change from pre–post interventions) for each study. Effect sizes from individual studies were then combined to produce an aggregate effect size, using random-effects models. Given studies did not report pre–post correlations of child behaviour or caregiver depression, we used a conservative r of 0.70 as recommended by Rosenthal (1984) to calculate the group x time effect sizes. The I2 statistic was used to assess the heterogeneity of the subgroups with scores of 0.25, 0.50, and 0.75 corresponding to low, moderate, and high levels, respectively (Higgins et al. 2003). Given there were not more than five studies in any subgroup, meta-regression moderation analyses could not be conducted to assess for age or gender differences in samples.
Results
Characteristics of Included Studies
Details regarding the characteristics of included studies are shown in Table 3. The 20 papers reported on samples comprising families; mostly parent–child compositions (n = 18), with others involving adult relatives (n = 2; *Glynn et al. 2010; *Rotondi et al. 2005). Most studies were conducted in the USA (n = 16), with three Australian and one Canadian study.
Table 3.
Sample, study characteristics, and findings of included studies (N = 20)
| Study; Country | Study design & sample (N) | Intervention (s) and study conditions | Assessment time points | Attrition | Relevant outcome (s) | Outcome measure (s) | Relevant findings |
|---|---|---|---|---|---|---|---|
| *Anderson et al. (2017) |
Uncontrolled experimental trial Adolescents 13–18 years with anorexia nervosa (AN) and their parent(s) |
TH (video) FBT. 20 sessions over 6 months | Baseline, post-treatment, 6-month follow-up | 0 | Adolescent weight (BMI), eating disorder symptoms, depressive symptoms, self-esteem |
EDE BDI RSE |
Significant increase in BMI and reductions in eating disorder symptoms from baseline to post-treatment and to 6-month follow-up. Significant improvement in depressive symptoms and self-esteem from baseline to follow-up |
| *Comer et al. (2017a); USA |
RCT families; child 4–8 years, child diagnosis of obsessive–compulsive disorder (OCD) (N = 22) |
TH (video) FB-CBT; F2F FB-CBT 12 sessions over 14 weeks (both conditions) |
Baseline, post-treatment, 6-month follow-up | 2 families (1 TH, 1 F2F) |
Child OCD symptoms Family accommodation of OCD symptoms |
ADIS-IV-C/P CY-BOCS CGI-S/I CGAS FAS-PR |
Child OCD symptoms and family accommodation of OCD symptoms improved from baseline to post-treatment, and to follow-up in both conditions; no significant difference between TH and F2F. 60–80% had clinically significant improvement across both conditions |
| *Comer et al. (2017b); USA | RCT Families; children 3–5 years, child diagnosis of behavioural disorder (N = 40) |
TH (video) PCIT; F2F PCIT |
Baseline, mid-treatment, post-treatment, 6-month follow-up | 12 families (6 TH, 6 F2F) | Child behaviour problems |
K-DBDS CGI-S/I CGAS ECBI CBCL |
Both conditions had large-to-very-large positive effects on children’s behavioural difficulties. Most outcomes were comparable across conditions; significantly higher rate of “excellent responses” in TH PCIT than in F2F PCIT |
| *Dadds et al. (2019); Australia |
RCT (× 2) Study 1: Rural families; child 3–9 years, child diagnosis of oppositional defiant or conduct disorder (N = 133) Study 2: Urban families; child 3–14 years, child diagnosis of oppositional defiant or conduct disorder (N = 73) |
Both studies—TH (video) IFICCP; F2F IFICCP | Both studies: Baseline, post-treatment, 3-month follow-up |
Study 1: 11 families (7 TH, 4 F2F) Study 2: 7 families (6 F2F, 1 VTC) |
Child behaviour problems Parent depression Parent anxiety |
SDQ BSI |
Large improvements in child behavioural difficulties in both studies; no significant difference between conditions. Moderate improvements in parent depression and anxiety in both studies; no significant difference between treatment conditions |
| *Davis et al. (2016); USA |
RCT Parent–child dyads; child with BMI > 85th percentile for age/gender (N = 103) |
TH (video) FB-CBT; telephone-based FB-CBT 8 × weekly meetings, then 6 × monthly meetings in both conditions |
Baseline, post-treatment | 2 families from telephone condition | Child behaviour problems | CBCL | Children did not display any clinically significant behavioural problems at baseline or post-treatment in either group; no significant group by time interaction effects |
| Davis et al. (2013); USA |
RCT Parent–child dyads; child with BMI > 85th percentile for age/gender (N = 58) |
TH (video) psycho-educational group 8 × weekly group meetings, then 6 × monthly meetings; Primary physician visit | Baseline, post-treatment | 16 families (11 from TH group; 5 from physician group) | Child behaviour problems | CBCL | Children did not display any clinically significant behavioural problems at baseline or post-treatment in either group; no significant difference between groups |
| *Glueckauf et al. (2002); USA |
Modified randomised controlled field experiment Parent–child dyads; adolescents with seizure disorders (N = 27) |
TH (video)-IFCM; telephone-IFCM; F2F IFCM | Baseline, post-treatment, -month follow-up | 5 families (4 from F2F; one from WL) | Family problems |
ISS IFS ICS SSRS |
Significant reductions in family problem severity and frequency across all three study conditions, maintained at follow-up; no significant difference in outcomes between conditions |
| *Glynn et al. (2010); USA |
Quasi-experimental design Adult-relative dyads; person diagnosed with a psychotic disorder and a relative (N = 42) |
TH online MFG program; TAU | Baseline, 6-month follow-up, 12-month follow-up | 6 dyads |
Distress Clinical status of schizophrenia Family relationship distress Perceived social support |
BSI BPRS FAS MSPSS | No significant impact on clinical status, perceived social support, or distress in persons with schizophrenia TH. Significant reduction in family relationship distress in TH group |
| *McGrath et al. (2011); Canada |
Experimental trial Parent–child dyads in three groups; child with diagnosis of ODD, ADHD or an anxiety disorder (N = 243) |
TH (telephone coaching) skills-based intervention; TAU Anxiety group received 11-weekly sessions, ODD and ADHD groups received 12 |
Baseline, 4-month follow-up, 8-month follow-up, 12-month follow-up | 10 dyads | Child mental health (anxiety, ODD, attention difficulties) | K-SADS-PL | The TH intervention significantly increased treatment success in all three groups, at all three follow-up points, compared to TAU |
| *Narad et al. (2015); USA |
RCT Adolescent-parent dyads; adolescents 12–17 years with a traumatic brain injury (TBI) (N = 132) |
TH (video) CAPS, 7–11 sessions; IRC | Baseline, post-treatment, 12-month follow-up, 18 month follow-up | 3 dyads (all IRC) |
Parent–child conflict Family communication Family problem-solving |
PSDRS FAD-PS IFIRS |
TH CAPS led to significant decrease in severity of family conflicts for adolescents with severe TBI only. Adolescents with moderate TBI in the CAPS condition did not report a significant a decline in family communication |
| *Rayner et al. (2016); Australia |
Non-randomised feasibility study Parent–child dyads; child had been admitted to hospital with cancer, or for cardiac surgery (N = 13) |
TH (video)-ACT, 5 group sessions | Baseline, post-treatment, 2-month follow-up, 8-month follow-up | None |
Parent depression Parent anxiety Parent stress Parent PTSD symptoms |
DASS CL-S AAQ-II PECI PPF | Small, non-significant changes in parent depression, anxiety, and stress from baseline to post-intervention. No significant changes in parent PTSD symptoms |
| *Rotondi et al. (2005); USA |
RCT Adult-relative dyads; person with a psychotic disorder and support persons; (N = 51) |
TH (internet discussion board group communication and website) for three groups; family members/support persons only, persons with psychotic disorder only, and MFG for all participants. TAU |
Baseline, 3-months post-baseline, 6-months post-baseline |
No data reported | Perceived stress Perceived social support | Interview data | Participants in TH condition had greater reductions in stress compared to participants in TAU. Non-significant trend toward greater perceived social support for participants in TH condition |
| *Sibley et al. (2017); USA |
Feasibility study Parent–adolescent dyads; adolescent with diagnosis of ADHD (N = 20) |
TH (video) skills-based treatment for ADHD, 10 sessions | Baseline and post-treatment | 3 families | Inattention symptom severity | DBD | Significant improvement in inattention symptom severity scores from baseline to post-treatment |
| *Stormshak et al. (2019); USA | Case control Parent–child dyads (N = 322) |
TH (telephone support) and web resources Web resources (IRC) only WC |
Baseline and post-treatment (3 months) | 21 families (2 WC; 8 IRC; 11 from coaching group) | Child behaviour problems |
EATQ-R SDQ PTC |
TH was significantly more effective than IRC or WC. Small-medium improvements in child behavioural problems in the TH condition |
| *Vander Stoep et al. (2017); USA |
RCT Parent–child dyads; children with a diagnosis of ADHD (N = 223) |
TH (video) psychiatry and child behaviour management training, 6 sessions TAU | Baseline, one month, 10 weeks, 19 weeks, post-treatment |
13.5% TH, 9.8% TAU |
Parenting stress Parent depression Caregiver strain Family empowerment | PSI PHQ-9 CSQ FES | Participants in the TH condition showed significantly greater improvements in parenting stress, parent depression, caregiver strain, and family empowerment than participants in TAU |
| *Wade et al. (2006); USA |
RCT Parent–child dyads; children with moderate-to-severe TBI (N = 39) |
TH (video) FPS, 12 × weekly sessions IRC | Baseline and post-treatment | 5 families (all FPS) | Child behaviour problems | CBCL | Non-significant trends for greater improvement in child behaviour problems for participants in FPS compared to participants receiving IRC. Children in the FPS condition reported greater behavioural self-management/compliance with parent instructions |
| *Wade et al. (2019); USA |
RCT Parent–adolescent dyads; adolescents 14–18 years with mild-to-severe TBI with behavioural impairment (N = 150) |
TH (video) FPS, 10 group sessions F2F FPS, 10 group sessions Self-guided online FPS |
Baseline, post-treatment, 6-month follow-up, 9-month follow-up | 34 families (12 F2F; 13 TH; 9 self-guided) |
Parent depression Parent global mental health |
CES-D BSI |
TH led to significant reductions in depression, and improvements in parent global mental health maintained at final follow-up; no significant differences between conditions |
| *Wade et al. (2015); USA |
RCT Parent–child dyads; adolescents 12–17 years with TBI (N = 132) |
TH (video) FPS and internet resources, IRC 6-month duration of intervention for both conditions |
Baseline, post-treatment, 6-month follow-up, 12-month follow-up, 18-month follow-up | 6 families (3 TH; 3 IRC) | Daily functioning of child | CAFAS | TH led to significant improvements in child daily functioning; these improvements were only evident at final follow-up, 18-month post-intervention |
| Wade et al. (2018); USA |
RCT Parent–child dyads; adolescents 11–18 years, with mild-to-severe TBI (N = 152) |
TH (video) with self-guided online sessions TOPS-Family or TOPS-TO (Teenager Only); IRC Both TOPS conditions had 10 sessions |
Baseline, post-treatment, 6-month follow-up | 37 families (13 TOPS-Family; 12 TOPS-TO; 12 IRC) |
Child behaviour problems Child executive functioning |
CBCL BRIEF |
Treatment effects on child behaviour problems were only evident for parents with low educational attainment in the TOPS-Family condition. Child executive functioning improved in the TOPS-TO condition, but only for families where parents reported higher levels of family stressors; no significant differences between conditions |
| *Williams et al. (2016); Australia |
Pilot RCT Parent–child dyads; children aged 2–8 years receiving treatment for leukemia (N = 12) |
TH (video) weekly × 5 group sessions plus 3 × individual telephone calls Triple P: Positive Parenting Program; WC | Baseline, post-treatment, 2-week follow-up, 2-month follow-up | 6 families (3 from each group) | Child behaviour problems | SDQ | No significant group differences in changes in child behavioural and emotional problems. Non-significant trend toward improvement in child behaviour problems in the treatment condition relative to WC |
Outcome Measures: AAQ-II Acceptance and Action Questionnaire–II, ADIS-IV-C/P Anxiety Disorders Interview Schedule for Children and Parents for DSM–IV, ASDS Acute Stress Disorder Scale, BDI Beck Depression Inventory, BPRS Brief Psychiatric Rating Scale, BRIEF Behavior Rating Inventory of Executive Functions, BSI Brief Symptom Inventory, CAFAS Child and Adolescent Functional Assessment Scale, CBCL Child Behavior Checklist, CES-D = Center for Epidemiological Studies Depression Scale, CGAS Children’s Global Assessment Scale, CGI-S/I Clinical Global Impression-Severity and Improvement Scales, CSQ Caregiver Strain Questionnaire, CY-BOCS Children’s Yale-Brown Obsessive- Compulsive Scale, DASS Depression Anxiety Stress Scales, DBD Disruptive Behaviour Disorder Rating Scale, EATQ-R Early Adolescent Temperament Questionnaire, ECBI Eyberg Child Behavior Inventory, EDE Eating Disorder Examination (Interview), FAD-PS Family Assessment Device Problem-Solving subscale, FAS-PR Family Accommodation Scale–Parent Report, FAS Family Attitude Scale, FES Family Empowerment Scale, ICS Issue Change Scale, IFIRS Iowa Family Interaction Rating Scale, IFS Issue Frequency Scale, ISS Issue Severity Scale, K-DBDS Kiddie-Disruptive Behavior Disorders Schedule, K-SADS-PL Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Versions, SDQ Strengths and Difficulties Questionnaire, MSPSS Multidimensional Scale of Perceived Social Support, PCIT Parent–Child Interaction Therapy, PCL-S Posttraumatic Stress Disorder Checklist-Specific, PECI Parent Experience of Child Illness, PHQ-9 The Patient Health Questionnaire, PPF Parental Psychological Flexibility Questionnaire, PSDRS Problem-Solving Discussion Rating Scale, PSI Parenting Stress Index, PTC Parenting Tasks Checklist, RSE Rosenberg Self-Esteem Scale, SSRS Social Skills Rating System, Interventions: ACT Acceptance and Commitment Therapy, CAPS Counsellor-Assisted Problem-Solving, F2F Face-to-Face in-person delivery, FB-CBT Family-Based Cognitive-Behavioural Therapy, FBT Family-based Therapy, FPS Family Problem-Solving Therapy, IFCM Issue-Specific Family Counselling Model, IFICCP Integrated Family Intervention for Child Conduct Problems, IRC Internet-resource comparison, MFG Multi-Family Group, TAU Treatment As Usual, TH Telehealth, TOPS-Family Teen Online Problem Solving with Family, TOPS-TO Teen Online Problem Solving with Teen Only, WC Wait-list Control
Twelve studies were described as randomised controlled trials (RCT); others were feasibility studies or pilot trials (n = 4), experimental trials (n = 2), modified randomised controlled field experiments (n = 1), and case–control studies (n = 1). Papers were published between 2002 and 2019. In total, the included studies reported on 1992 families or parent–child/adult-relative dyads, with a mean sample size of 99.6 (SD = 91.81, range = 10–322).
The included studies drew on a range of interventions, including Family Problem-Solving Therapy (FPS; n = 5), Family-Based Cognitive Behavioural Therapy (FB-CBT; n = 2), and Parent–Child Interaction Therapy (PCIT; n = 1). Two studies used a multi-family group (MFG) approach for individuals with a psychotic illness and their adult relatives. One study used an Acceptance and Commitment Theory (ACT) framework, and one used the Triple P: Positive Parenting Program intervention. One study used family-based treatment (FBT) for anorexia nervosa. All other studies described a non-specific cognitive-behavioural and/or skills-based approach (see Table 3).
Study Quality
The average score for quality assessment ratings of included studies was 18.9 out of a possible maximum of 26. When the Jadad scale item (item 13) was removed, no studies exceeded a score of 24. Scores for each included study are presented in Online Resource 1. Many studies either reported inadequate information or did not address study blinding or prospective calculation of sample size, and many studies reported a loss of > 5% of the sample to follow-up. Twenty percent of studies were double rated. Inter-rater agreement on study quality was 100%.
The Replicated Evidence: Meta-analytic Findings
Across the 20 included studies, there were 37 relevant effects relating to mental health and/or relational health outcomes. Meta-analyses were possible for thirteen effects from eleven studies related to the efficacy of TH in addressing child behavioural problems (k = 8) and parental depression (k = 5). The remaining effects could either not be meaningfully clustered into a domain with at least one other similar effect (k = 22), or the required statistical information was not given in text nor provided by authors upon request (k = 2).
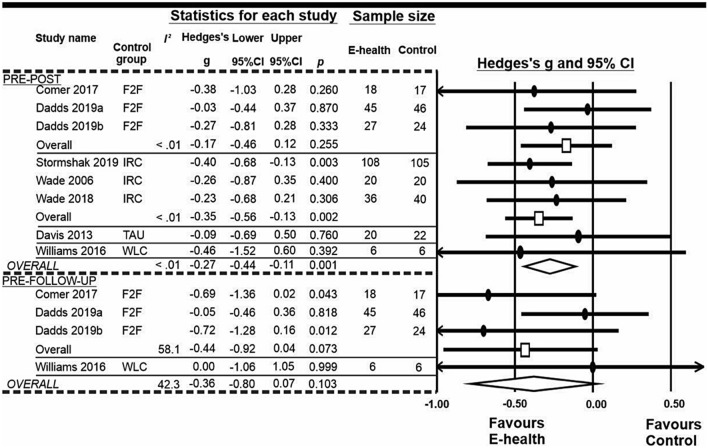
Child Behavioural Problems
In the pre- to post comparison (see Fig. 2), the efficacy of the TH interventions for child behavioural problems was somewhat superior to the control interventions (in-person, internet resources, treatment as usual, or wait-list control), with a small effect size. The Q statistic assessment of heterogeneity confirmed studies in the meta-analysis shared the same effect size (Q = 2.828, p = 0.900, I2 < 0.001). Publication bias did not appear to be an issue, with a visual inspection of the funnel plot showing an even dispersal of studies, and Egger’s regression confirming the included studies were symmetrically distributed [p (2-tailed) = 0.66]. The classic Fail-Safe N was calculated and revealed that an additional 10 studies with an effect size of zero would be required to render the current findings non-significant.
Fig. 2.
Meta-analyses of the effect of telehealth interventions for child behavioural problems. E-Health telehealth delivery, F2F face-to-face, IRC internet-resources comparison, TAU treatment as usual, WLC wait-list control
Subgroup analyses revealed the effect size did not differ across studies, based on control group type Qbetween = 1.40, df = 3, p = 0.706, or the outcome measure used (i.e. Child Behavior Checklist, Eyberg Child behaviour Inventory, or Strengths and Difficulties Questionnaire), Qbetween = 0.34, df = 2, p = 0.846. Although Fig. 2 shows significant differences between TH and provision of resources but not between TH and in-person delivery, when considered collectively the effect sizes did not differ based on comparison type.
For the four studies that collected follow-up data, meta-analysis showed a non-significant trend for persisting improved outcomes in TH relative to control, also with small effect size. Subgroup analyses revealed the effect size did not differ across studies, based on the control group type, Qbetween = 0.56, df = 1, p = 0.454, or the measure used, Qbetween = 0.93, df = 1, p = 0.336.
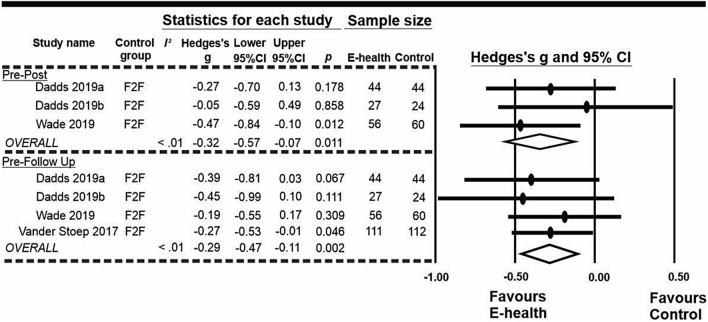
Parental Depression
As shown in Fig. 3, the efficacy of the TH interventions appeared to be superior to control interventions, all in-person comparisons, at both pre- to post intervals, Hedges g = − 0.23 (95% CI − 0.57, − 0.07) p = 0.011, and pre to follow-up, Hedges g = − 0.33 (95% CI − 0.47, − 0.11) p = 0.002, for parental depression. Both were small effects. The heterogeneity among effect sizes was low in both pre to post (Q = 1.161, p = 0.445, I2 < 0.001) and pre to follow-up (Q = 0.877, p = 0.831, I2 < 0.001).
Fig. 3.
Meta-analyses of the effect of telehealth interventions for parental depression. E-Health telehealth delivery, F2F face-to-face
Publication bias did not appear to be an issue, with a visual inspection of the funnel plot showing an even dispersal of studies, and Egger’s regression confirming the included studies were symmetrically distributed at pre to post (p (2-tailed) = 0.12) and pre to follow-up (p (2-tailed) = 0.34). The Fail-Safe N analyses show that the addition of two and seven studies at each timepoint comparison with an average effect size of zero would render the current findings non-significant.
Narrative Summary of Individual Studies
The included individual studies reported effects relating to family outcomes, child outcomes, and outcomes for individuals with a psychotic illness and their adult relatives. Study findings for effects not included in the meta-analysis are described below and details of study interventions are included in Table 3.
Family Outcomes
Included studies assessed a range of negative (e.g. distress, conflict) and positive (e.g. problem solving) family outcomes. Many studies reported improvements in outcomes following engagement with TH. However, changes in outcomes from pre- to post intervention and to follow-up were not different from changes observed in comparison conditions for any outcomes.
A family counselling intervention delivered via TH (videoconferencing) with parent–teenager dyads led to significant reductions in the severity and frequency of family problems to post-intervention. Improvements were maintained at 6-month follow-up (*Glueckauf et al. 2002). There was no evidence of any significant differences between this intervention delivered via TH or via telephone or in-person delivery.
One study of families with children with traumatic brain injury (TBI) used a web-based family problem-solving therapy with a counsellor via TH (videoconferencing) sessions. Improvements to post-treatment were observed for family problem solving. These were not maintained to 18-month follow-up (*Narad et al. 2015). Other effects were mixed and depended on differing levels of severity of TBI of adolescents. For family conflict, significant decreases were observed at 18-month follow-up only for adolescents with severe TBI. For adolescents with moderate severity of TBI, levels of effective family communication remained steady across assessment timepoints for the TH group. Declines at 12-month follow-up were observed in the control group who received internet resources.
The use of TH (videoconference) delivered family-based cognitive-behavioural therapy (FB-CBT) in families with a child with obsessive–compulsive disorder (OCD) led to improvements in family accommodation of OCD symptoms which were maintained at 6-month follow-up (*Comer et al. 2017a, b). Immediate and 6-month follow-up improvements were comparable to those in the in-person condition.
Parent Outcomes
Parent mental health outcomes were assessed in four of the included studies. Relative to primary care, a hybrid TH approach for caregivers of a child with attention-deficit hyperactivity disorder demonstrated significantly greater improvements in caregiver stress, depression, and caregiver strain (Stoep et al. 2017). This intervention comprised videoconference-delivered psychiatry sessions and skills-based behavioural training.
In other studies, interventions were implemented for child conduct disorders utilising the Integrated Family Intervention (*Dadds et al. 2019) and family problem solving following adolescent traumatic brain injury (*Wade et al. 2019). No differences were noted between TH and in-person delivery. Improvements in parent anxiety and depression at post-intervention were maintained to 3 months (*Dadds et al. 2019), and depression and distress at post-intervention maintained 9 months after baseline (*Wade et al. 2019). TH intervention (videoconferencing) in acceptance and commitment therapy for parents with a child with life-threatening illness was piloted in a non-controlled feasibility study. Small but non-significant improvements in parent depression, anxiety, stress, and PTSD symptoms were noted at post-intervention (*Rayner et al. 2016).
Child Outcomes
Studies reported a diverse array of child outcomes. One study explored the impact of TH (videoconferencing) FB-CBT on child OCD symptom severity. Improvements comparable to the in-person FB-CBT condition were noted for TH in OCD symptoms and in clinician-rated functioning, and maintained at 6-month follow-up (*Comer et al. 2017a, b).
*McGrath et al. (2011) examined a family-centred coaching intervention with online resources accessed by families and weekly TH (telephone) coaching for families with a child diagnosed with oppositional defiant disorder (ODD), attention-deficit hyperactivity disorder (ADHD), or an anxiety disorder. Successful outcomes, defined as children no longer meeting diagnostic criteria, were observed in higher rates in the TH groups relative to treatment as usual control. Effects were maintained to 8 months post baseline for the ODD group and to 12 months for the ADHD and anxiety groups (*McGrath et al. 2011). *Sibley et al. (2017) examined a 10-session family therapy skills-based TH (video-conferenced) intervention for adolescents with attention-deficit hyperactivity disorder (ADHD) and their parents. Parent and teacher-rated severity of inattention symptoms improved post-treatment. Findings reflect within-group change over time, as no control group was used. A further study examined the feasibility and preliminary effects of family-based treatment (FBT) delivered via TH (videoconferencing) in a pilot trial for adolescents with anorexia nervosa (*Anderson et al. 2017). Significant improvements in weight and eating disorder symptoms were apparent at post-treatment and maintained at 6-month follow-up. Adolescents rated the treatment as moderately positively, whereas mothers and fathers rated the treatment very positively.
Two studies utilised TH for families where a child had TBI. Family problem-solving therapy delivered by videoconferencing improved daily functioning of children relatively more than an internet resource control group, with effects evident 12 months after treatment completion (*Wade et al. 2015). Similarly, compared to individual therapy, a TH (videoconferencing)-delivered problem-solving program resulted in more improved executive functioning (parent report) post-treatment in adolescents (*Wade et al. 2018). Interaction effects between family stress levels and executive function were noted.
*Davis et al. (2016) examined the benefit of a TH intervention, delivered by videoconference or by telephone, in treating paediatric obesity on child behavioural outcomes. The sample did not display clinically significant levels of behavioural problems at baseline and there were no group by time changes over the course of the intervention. This study was not included in the meta-analysis of the same category, as no quantitative statistics were made available for analysis.
Adults with Psychotic Illnesses and Their Relatives
Two studies examined outcomes for individuals with a psychotic illness (schizophrenia and schizoaffective disorder) and their adult relatives from participation in an online support program with TH therapy/facilitated synchronous chat for persons with schizophrenia, family member groups, or multi-family groups (*Glynn et al. 2010; *Rotondi et al. 2005). Mixed findings were observed. Relative to the treatment as usual control groups, for individuals with psychotic disorder, TH intervention reduced stress in one study (*Rotondi et al. 2005) but did not reduce distress or impact clinical symptomatology in another study (*Glynn et al. 2010). In neither study were improvements in perceived social support observed (*Glynn et al. 2010; *Rotondi et al. 2005).
For adult relatives of individuals with a psychotic disorder, participation in TH did not alter perceived social support or stress (*Rotondi et al. 2005) or alter anxiety/depression or somatisation symptoms, reflective of distress (*Glynn et al. 2010), relative to treatment as usual. Relatives were found to have improved levels of family relationship stress but not perceived social support over time. However, these were not examined in comparison with change in the control group (*Glynn et al. 2010).
Brief Discussion
This systematic review and meta-analysis provides evidence that family-based therapy delivered via TH improves relational and mental health outcomes for family, parent, and child measures. Effects were equivalent to in-person delivery of interventions for many outcomes. In no studies included in the review were outcomes from TH found to be inferior to in-person delivery. These findings are preliminary, and should be interpreted in light of their limitations, including the small number of studies reviewed. Only 20 studies met inclusion criteria, a considerably smaller pool of research than has been examined for individual TH therapies.
Study Three: Qualitative Exploration of Family Therapist Experiences with TH
Study Three aimed to explore family therapists’ perspectives on delivering family therapy via TH and to understand elements of therapy that are more or less effective through TH delivery relative to in-person experiences. In addition, the study aimed to understand perceptions of risk of use of TH.
Method
Participants
Participants were family therapists (n = 12; three male and nine female) at a specialist public health funded family services centre. Invitation to participate was extended to all practitioners with experience delivering family/group therapy via a TH (videoconferencing) medium. Participation was voluntary, and required informed consent. Most (10 of 12) participants had conducted between 6 and 12 family telehealth sessions. One participant had completed about 18, and one had completed about 30. For most (10 of 12) participants, use of telehealth was new (i.e. since the beginning of the COVID-19 pandemic). There were two exceptions to this: one participant had some prior experience with family therapy telehealth in a previous role, and one had prior experience with the use of telehealth but only with individuals rather than groups or families.
Procedure
Approval was provided by the La Trobe University Human Ethics Committee (Project ID: HEC20118). The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. Each practitioner participated in a structured, one-on-one audio-recorded interview (approximately 60 min) with AB. Interview questions are presented in Table 4. Participants were not familiar with the interview questions prior to the interview.
Table 4.
Interview questions for exploration of family therapist experiences with TH
| Interview question | Domain |
|---|---|
| What core considerations would guide your judgement that a case was suitable or unsuitable for a TH medium? (E.g.: client ages, presenting problems, reflective capacity, risk, intra-family dynamics, etc.) | Suitability for TH |
| What would you consider essential for an online therapist to do in establishment of rapport and empathy with all family members? | Rapport |
| How might you handle moments of conflict between family members in the ‘online’ room—e.g. is there any difference in what you would say or do, or feel? | Conflict management |
| What accommodations would you make for younger children? | Working with children |
| Under what conditions would you not resume a treatment online that had commenced in person? | Continuation of in-person therapy via TH |
| Are there any core principles or practice elements of family therapy that seem less effective via TH? | Perceived drawbacks of TH interventions with families |
| Are there any core principles or practice elements of family therapy that seem more effective via TH? | Perceived efficacy of TH interventions |
| How would your crisis management practice change when using a TH medium, to manage risky behaviour in the room (e.g. a child starts head banging; a family member threatens another family member) | Managing risk in the moment |
| What additional vulnerabilities might you feel as the therapist? What might assist you to feel more comfortable with respect to these? | Wellbeing of the therapist in a TH context |
Data Analysis
Audio-recorded interviews were transcribed verbatim using transcription software and checked by a member of the research team. Transcript data were then subject to qualitative content analysis (Bengtsson 2016; Elo and Kyngäs 2008; Hsieh and Shannon 2005) at the manifest level. Using a deductive, predetermined coding system aligned with the interview structure, one independent coder (FP) extracted and coded transcript data using a standardised coding table. Codes and themes were reviewed by two second independent coders (AB, JM). Nine key domains were identified. Data analysis occurred across four stages: (a) decontextualization (deconstruction of the transcript into meaning units); (b) recontextualization (identification of codes); (c) categorization (identification of themes); and, (d) compilation (drawing of group-level conclusions and variations, with conferencing between coders and checking of the original text).
Results
Findings are organised by the domains corresponding to interview questions (see Table 4), including a high-level summary of key themes and significant variations in therapists’ views.
Suitability for TH
Views about the suitability of cases for TH family therapy were congruent with those made in in-person work. No blanket contraindications for the use of TH were identified for this setting. As per in-person work, contraindications included imminent family violence risks and current severe disturbance in personal functioning with cognitive, neurological, or psychiatric origins that render participation unsafe or otherwise unhelpful for any participant. As with in-person consultation, such impairments may delay the timing of the intervention rather than presenting a blanket contradiction. An example of this may be presenting as drug affected on the day of an appointment.
A series of cautions characterised by risk or complexity (e.g. history of trauma, sexual assault or suicidal ideation) emerged about the suitability of TH for cases. Suggested accommodations to manage these circumstances centred on ‘slowing the work down’ and included spending more time than usual understanding client situations, priorities, and the nuances of potential risk, and setup of risk management plans prior to therapy. A well-paced therapeutic process was key to maintaining trust and rapport, together with making open and collaborative choices with clients; devoting more time to ‘talking about the talking’; and allowing more time to develop the foundations of a therapeutic relationship with new clients.
Rapport
Relative to in-person contexts, the TH environment was seen to require (i) more time and (ii) additional accommodations to content and process for purposes of establishing rapport, described below. TH engagement was augmented by a first telephone contact with all family members to establish individual connections before commencing TH sessions. Equally important were transparent discussions about client comfort with the TH therapy modality; establishing a mutual understanding of how to communicate about the process when it is not working well and being more directive than usual to facilitate equal contributions to group conversations.
Technological factors impacted rapport, including looking directly at the camera while talking with clients to emulate eye contact, and using names when addressing clients to compensate for the challenges of deploying direct gaze and body orientation as one would in person. Consideration was also given to the influence of TH features on client experience, e.g. muting different voices at different times and using a particular screen viewing modes. Explanations were offered when doing anything off-screen such as using a notepad, providing a clear explanation to avoid confusion about practitioner inattention.
Conflict Management
Therapists noted a lower overall threshold in the TH context for intervening with conflict during a session, and a focus on methods of remaining in control if conflict occurred. All therapists noted the critical importance of mitigating the possibility of conflict prior to therapy. Preliminary discussions with clients about how conflict would be resolved in the absence of the practitioner were felt to be essential, given concerns that clients might be more inclined to abruptly walk out of a TH consult than from the therapy room in-person. Successful TH interventions included establishing permission and processes for discussing ‘hot issues’ during the session; addressing the need to intervene, and post-session regulatory strategies. Several therapists found online breakout rooms useful for speaking to clients separately where conflict had occurred or was imminent.
One key variation was noted. Some therapists felt that conflict was more difficult to manage when family members were on separate screens, as this blurs the detection of early signs of conflict, while others felt a greater sense of control when family members joined from separate devices, in separate spaces, as the risk of physical conflict was felt to be lower.
Managing Risk in the Moment
All therapists reported that managing risk via TH was more delicate than managing risk in-person. The unanimous emphasis was on risk mitigation rather than risk management in TH. As such, efforts were consistently made to ensure best possible risk assessment prior to engaging in therapy. As with in-person work, therapists agreed that imminent safety risks would contraindicate suitability for TH therapy. Immediate intervention in a context of risk would be largely congruent with intervention in the in-person setting (i.e. the need to slow down and stop where necessary and allow for breaks in instances of escalation; post-session follow-up to determine client safety; readiness to contact police, or provide details of support services or contact services on client’s behalf).
A common concern pertained to the consequence of technology failure, with the need to invest in pre-session preparation, to ensure therapists were aware of clients’ locations and alternate contact methods in case of an emergency, including phone numbers and email addresses. The normal practices of notifying police would apply if a reportable concern about dangerous behaviour arose.
Therapists agreed that given the physical distance of the therapist, TH brings increased shared involvement of the client in risk management, shared responsibility for their own self-regulation, and support of others’ self-regulation, with the assistance of emotion coaching strategies.
Working with Children
Views about suitability of TH for children varied. Common to all was the need for advance preparation and active alignment with parents to ensure the space for the session worked well for the children and was equipped with drawing and play materials, active engagement of young children, sustaining their involvement in the session through shorter sessions, and leveraging different types of play. In this, a need for therapists to manage their own expectations was evident (e.g. being prepared that the session might need to be brief or to end early).
Most therapists reported the need to be more engaging, e.g. via maximising interactive methods and minimising verbal discussion, creating a playful atmosphere by utilising virtual backgrounds, and introducing various types of play. Therapists also found it helpful to bring attention to the TH medium as a point of interest and to use its novel features (e.g. online whiteboards) to engage children in session.
Continuation of In-Person Therapy Via TH
As to the question of continuing an already established therapy process via an online medium, no differences were noted relative to those that would apply to consideration of continuing in-person therapy. These standard cautions as outlined above in the ‘Suitability for TH’ section would equally apply.
Cautions for continuing via TH amounted to concerns about participating safely and included situations where the client had inadequate support in scenarios of risk management while using TH. Ongoing monitoring of the efficacy and suitability of the medium across the course of treatment was noted by all.
Perceived Drawbacks of TH Interventions with Families
Several therapists reported that some therapeutic techniques felt more difficult or perhaps less effective online (e.g. triadic questioning when members were on different devices). The same held for pragmatic activities (e.g. moving people around the room to create a family sculpture) and several felt that their use of warmth, humour, and the ability to accurately read non-verbal cues were somewhat compromised. Nevertheless, there was uniform agreement that the core elements of family therapy were more or less maintained with the transition to TH.
Perceived Efficacy of TH Interventions
Various therapeutic experiences and access/uptake issues were improved with the transition to TH delivery. Some felt that TH offered an improved ability for therapists to empathise and align with others’ experiences due to the equal visual presentation of faces on the screen. In this, being able to see one’s own responses on the screen had potential benefits. Self-direction associated with use of TH also offered families a greater sense of ownership in their therapeutic process.
Some felt that TH promoted better equity in access and uptake. At the geographical level, there are benefits of TH for those living in remote areas. At the individual level, TH can better suit those with certain disabilities or preferences for interaction online.
Wellbeing of the Therapist in a TH Context
Several therapists reported that the usual boundaries that exist between in-session and out-of-session work done in-person were difficult to maintain when using TH. Some reported feeling detached from their work when using TH: they were disempowered and at times helpless about what they perceived as a limited capacity to detect and adequately respond to nuances of expression. To preserve wellbeing, therapists expressed a need for quality supervision; the importance of seeking and maintaining collegial support; the availability of reliable technology (to mitigate stress associated with the technological challenges of operating via TH); a manageable workload; being accepting of the constraints associated with TH; prioritising self-care activities such as breaks and exercise; and incorporating co-therapy to ease feelings of isolation.
Brief Discussion
We found congruence between the core practice and process elements of family therapy across in-person and TH modalities. Some unique benefits of practicing via TH were observed. Necessary accommodations made to therapeutic work with TH predominantly pertained to process rather than content changes, including the need to plan ahead for possible management of risk.
Discussion
This study examined the efficacy and optimization of TH-delivered family therapy from multiple perspectives, aiming to inform future use of TH for family and systemic practice. The first study found that content from existing guideline documents was heavily weighted to operational rather than therapeutic aspects of therapy delivery. We identified a significant gap in information for practitioners to guide therapeutic adjustments that may be required when working with families over digital mediums, and especially with children. Study Two examined evidence for efficacy of TH in improving outcomes for families. Although the available literature was limited in volume, consistent results emerged. Meta-analyses demonstrated improvements in child behaviour problems for family therapy with equivalency between TH and in-person delivery from pre-to-post intervention and to follow-up. Relative to treatment as usual, internet resources, or wait-list control conditions for child behaviour problems, TH family therapy had superior improvement rates, pre- to post-intervention. Similarly, for family-oriented treatment of parental depression, meta-analyses showed that improvements were superior in TH relative to in-person delivery for pre- to post-intervention and to follow-up. Narrative review of individual studies excluded from meta-analyses found that TH delivery was equivalent to in-person delivery for a range of family, parent, and child outcomes, and frequently superior to minimal intervention control conditions. In the final study, qualitative analysis of one-on-one interviews with experienced family therapists found that core processes and practices of family therapy could be preserved in the online modality. Adaptations to delivery of therapy in TH were primarily process rather than content related. Taken together, the findings of these three studies provide considerable support for ongoing delivery of family therapy via TH.
The current findings, focussed on family therapy, expand the meta-analytic evidence for TH in other contexts, mirroring findings of the superiority of individual therapies via TH relative to wait-list or information only controls, and equivalent outcomes to in-person delivery of therapy (Ahern et al. 2018; Drago et al. 2016). Consideration of the therapeutic alliance may offer some insight into the equivalence of outcomes in TH and in-person therapy. Normatively, the therapeutic alliance accounts for considerable variance in therapeutic outcomes (Fluckiger et al. 2018). Novice TH therapists in our third study echoed concerns voiced elsewhere (Bee et al. 2008), that the formation of this critical alliance could be impacted in TH relative to in-person interactions through alterations in interpersonal communication. However, in some (Jenkins-Guarnieri et al. 2015) but not all review studies (Norwood et al. 2018), and for many Study 3 experienced therapists, the alliance was observed to be unaffected by TH delivery. As found in our third qualitative study, key to this are alterations to accommodate the digital environment, in pursuit of establishing rapport and empathic connection, which may be integral to good outcomes in TH.
As with prior research (Gros et al. 2013), therapists in our qualitative study also emphasised the need to engage in pre-therapy connection and preparation strategies, such as prior telephone or digital conversations with clients, for risk mitigation and for optimised outcomes. Other scholars have suggested that it is advantageous for the pre-therapy connection meetings to take place in-person, rather than through technology (Kuulasmaa et al. 2004). It remains to be seen whether initial in-person meetings would strengthen therapist–client connections or whether conducting this meeting over telehealth would be sufficient for this purpose.
Uniquely, our qualitative results suggest some advantage of TH delivery in family therapy over face-to-face, as reported in previous research with individual or couples therapy (Richardson et al. 2015). Key factors for perceived efficacy from the client and therapist perspectives include ease of talking in telehealth, where turn taking is clearer, and ease of revealing vulnerability for some clients, invoked by a sense of distance in TH that may be conducive to disclosure (Kysely et al. 2020). Accessibility is also key. The TH platform removes obstacles to attendance for many families in compounding circumstances that render the logistics of attending in-person difficult, as with families living in remote regions, and high-needs single parent families.
Limitations
Findings should be interpreted in light of the studies’ limitations. First, the grey literature on TH Guidelines comprised a mix of pre-COVID-19 resources and others specifically generated in response to the rapid uptake of TH due to the pandemic. Studies eligible for the meta-analyses were limited by the heterogeneity in measurement methods and outcome foci. As such, a small number of studies focused only on child behaviour outcomes and parental depression were subject to meta-analysis. In relation to the qualitative study, our participants were a homogenous sample of therapists from one service, most of whom had limited pre-COVID-19 TH experience. However, due to this recent transition to TH delivery, they were well positioned to reflect on differences between TH and in-person delivery. In all three studies, examination of cultural and gender diversity was not possible. Consumer participation in the research was also not possible at this stage but is now planned.
Recommendations
The findings of these three studies provide considerable support for ongoing delivery of family therapy via TH. In this light we offer recommendations for further optimisation of TH practice in family therapy contexts.
- Progression in Guidelines
- Our evidence suggests a need for advanced clinical guidelines for enhanced engagement and therapeutic alliance. Guidelines offered by peak therapy and regulatory bodies would include but move beyond operational factors regarding the practical administration of TH delivery of services, to include critical points of difference in assessment, engagement and therapeutic alliance over TH media, for adults, and for children.
- Beyond the expectation for assessment of suitability, articulation of specific criteria for assessing the appropriateness of TH are needed. These are multi-factored, and range from operational constraints, to safety risks, to clinically based cautions and contraindications.
- Enablers of Telehealth practice
- Further work is needed to address technology and access constraints to overcome obstacles that would otherwise preclude some families from TH services, including access for clients to software and necessary equipment, basic training in their use, and support for trouble-shooting.
- Similarly, evolving technologies may better enable the use of core family therapy techniques within TH services, for example, reflective teams, joint completion of genograms in sessions, and interactive play between children and therapist.
- Training
- With rapid expansion of requirements for TH services comes the attendant need to train and support mental health workforces in the requisite skills. Where technology is likely to remain specific to local contexts and require in-house training, broader Family Therapy-specific training for TH would optimally be offered through accessible online training, consultation and support.
- Research
- Our review of the existing literature shows some early encouraging replication of evidence and justifies further exploration. For example, efficacy data spanning longer post-treatment intervals, a focus on contraindications and iatrogenic effects would support practice and policy decisions about the continuation of TH interventions as an acceptable alternative to in-person interventions.
- Greater consistency in assessment of child, parent, and family outcomes across studies would assist.
- Inclusion of diverse samples, with exploration of limits to culturally safe TH practices will be important to applying this method at scale.
- Distinctions between forms of telehealth suitable for more than one therapist are yet to be systematically researched and further knowledge about the relative efficacies of co-therapy and team interventions via telehealth would provide valuable insights for future implementation.
- Mediators of change relative to in-person therapies and questions concerning pre-existing and presenting circumstances impacting efficacy are yet to be addressed.
Conclusion
Findings of the current studies offer significant support for delivery by TH methods of family therapy services. The collective evidence suggests equivalent efficacy for relational and mental health outcomes from telehealth relative to face-to-face delivery. From both empirical review and grounded narrative perspectives, the studies included here provide a solid platform from which to advance telehealth methods for family therapy.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
No funding was received for this research.
Data Availability
The data that support the findings of Study 3 are not publicly available due to privacy and ethical approval restrictions. Data were not collected for Study 1 or Study 2.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflicts of interest or competing interests in relation to this research.
Ethical Approval
Study Three involved research with human participants. The study was performed in line with principles of the Declaration of Helsinki. Approval to conduct the study was obtained from the La Trobe University Human ethics committee (Date: 23 April 2020/No. HEC20118) and written informed consent was obtained from all participants prior to participating in this study.
Informed Consent
The authors confirm that participants provided informed consent for publication of their anonymous, grouped data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
References marked with an asterisk indicate studies included in the systematic review in Study 2.
- Aafjes-van Doorn K, Békés V, Prout TA. Grappling with our therapeutic relationship and professional self-doubt during COVID-19: Will we use video therapy again? Counselling Psychology Quarterly. 2020 doi: 10.1080/09515070.2020.1773404. [DOI] [Google Scholar]
- AAFT (Australian Association of Family Therapy). (2020). COVID-19 Response: Resources for family therapists. Retrieved from https://www.aaft.asn.au/covid-19-response/resources-for-family-therapists/.
- Ahern E, Kinsella S, Semkovska M. Clinical efficacy and economic evaluation of online cognitive behavioral therapy for major depressive disorder: A systematic review and meta-analysis. Expert Review of Pharmacoeconomics & Outcomes Research. 2018;18:25–41. doi: 10.1080/14737167.2018.1407245. [DOI] [PubMed] [Google Scholar]
- AMFTRB (Association of Marital and Family Therapy Regulatory Boards). (2016). Teletherapy guidelines. Retrieved from https://amftrb.org/wp-content/uploads/2017/05/Proposed-Teletherapy-Guidelines-DRAFT-as-of-09.12.16.pdf.
- *Anderson, K. E., Byrne, C. E., Crosby, R. D., & Le Grange, D. (2017). Utilizing telehealth to deliver family-based treatment for adolescent anorexia nervosa. International Journal of Eating Disorders, 50, 1235–1238. 10.1002/eat.22759. [DOI] [PubMed]
- Bee PE, Bower P, Lovell K, Gilbody S, Richards D, Gask L, Roach P. Psychotherapy mediated by remote communication technologies: A meta-analytic review. BMC Psychiatry. 2008;8:60. doi: 10.1186/1471-244X-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14. doi: 10.1016/j.npls.2016.01.001. [DOI] [Google Scholar]
- Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. (2005). Comprehensive meta-analysis (Version 3). Englewood: NJ: Biostat. Retrieved from http://www.meta-analysis.com.
- Caldwell, B., Bischoff, R., Derigg-Palumbo, K., & Liebert, J. (2017). Best practices in the online practice of couple and family therapy: Report of the online therapy workgroup. Retrieved from https://www.aamft.org/Documents/Products/AAMFT_Best_Practices_for_Online_MFT.pdf.
- *Comer, J. S., Furr, J. M., Kerns, C. E., Miguel, E., Coxe, S., Elkins, R. M., et al. (2017a). Internet-delivered, family-based treatment for early-onset OCD: A pilot randomized trial. Journal of Consulting and Clinical Psychology, 85, 178–186. 10.1037/ccp0000155 [DOI] [PMC free article] [PubMed]
- *Comer, J. S., Furr, J. M., Miguel, E. M., Cooper-Vince, C. E., Carpenter, A. L., Elkins, R. M., et al. (2017b). Remotely delivering real-time parent training to the home: An initial randomized trial of internet-delivered parent-child interaction therapy (I-PCIT). Journal of Consulting and Clinical Psychology, 85, 909–917. 10.1037/ccp0000230 [DOI] [PubMed]
- *Dadds, M. R., Thai, C., Diaz, A. M., Broderick, J., Moul, C., Tully, L. A., et al. (2019). Therapist-assisted online treatment for child conduct problems in rural and urban families: Two randomized controlled trials. Journal of Consulting and Clinical Psychology, 87, 706–719. 10.1037/ccp0000419 [DOI] [PubMed]
- *Davis, A. M., Sampilo, M., Gallagher, K. S., Dean, K., Saroja, M. B., Yu, Q., et al.. (2016). Treating rural paediatric obesity through telemedicine vs. telephone: Outcomes from a cluster randomized controlled trial. Journal of Telemedicine and Telecare, 22, 86–95. 10.1177/1357633x15586642 [DOI] [PMC free article] [PubMed]
- Doss BD, Knopp K, Roddy MK, Rothman K, Hatch SG, Rhoades GK. Online programs improve relationship functioning for distressed low-income couples: Results from a nationwide randomized controlled trial. Journal of Consulting and Clinical Psychology. 2020;88:283–294. doi: 10.1037/ccp0000479. [DOI] [PubMed] [Google Scholar]
- Drago A, Winding TN, Antypa N. Videoconferencing in psychiatry, a meta-analysis of assessment and treatment. European Psychiatry. 2016;36:29–37. doi: 10.1016/j.eurpsy.2016.03.007. [DOI] [PubMed] [Google Scholar]
- Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: A randomised, open-label, non-inferiority trial. The Lancet Psychiatry. 2015;2:693–701. doi: 10.1016/S2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- Elo S, Kyngäs H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Fluckiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy. 2018;55:316–340. doi: 10.1037/pst0000172. [DOI] [PubMed] [Google Scholar]
- *Glueckauf, R. L., Fritz, S. P., Ecklund-Johnson, E. P., Liss, H. J., Dages, P., & Carney, P. (2002). Videoconferencing-based family counseling for rural teenagers with epilepsy: Phase 1 findings. Rehabilitation Psychology, 47, 49–72. 10.1037/0090-5550.47.1.49
- *Glynn, S. M., Randolph, E. T., Garrick, T., & Lui, A. (2010). A proof of concept trial of an online psychoeducational program for relatives of both veterans and civilians living with schizophrenia. Psychiatric Rehabilitation Journal, 33, 278–287. 10.2975/33.4.2010.278.287 [DOI] [PubMed]
- Gros DF, Morland LA, Greene CJ, Acierno R, Strachan M, Egede LE, et al. Delivery of evidence-based psychotherapy via video telehealth. Journal of Psychopathology and Behavioral Assessment. 2013;35:506–521. doi: 10.1007/s10862-013-9363-4. [DOI] [Google Scholar]
- Heckman TG, Heckman BD, Anderson T, Lovejoy TI, Markowitz JC, Shen Y, Sutton M. Tele-interpersonal psychotherapy acutely reduces depressive symptoms in depressed HIV-infected rural persons: A randomized clinical trial. Behavioral Medicine. 2017;43:285–295. doi: 10.1080/08964289.2016.1160025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helps, S., Kerman, C., & Halliwell, C. (2020). Doing remote systemic psychotherapy during COVID-19: Some practice ideas. Retrieved from https://tavistockandportman.nhs.uk/about-us/news/stories/doing-remote-systemic-psychotherapy-during-covid-19-some-practice-ideas/.
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- ILB-MFT (Idaho Licensing Board of Professional Counselors and Marriage and Family Therapists). (2016). Telehealth guidelines for professional counselors and marriage and family therapists. Retrieved from https://ibol.idaho.gov/ibol/cou/documents/Telehealth%20Guidelines.pdf.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- Jenkins-Guarnieri MA, Pruitt LD, Luxton DD, Johnson K. Patient perceptions of telemental health: Systematic review of direct comparisons to in-person psychotherapeutic treatments. Telemedicine and e-Health. 2015;21:652–660. doi: 10.1089/tmj.2014.0165. [DOI] [PubMed] [Google Scholar]
- Kuulasmaa A, Wahlberg K-E, Kuusimäki M-L. Videoconferencing in family therapy: A review. Journal of Telemedicine and Telecare. 2004;10:125–129. doi: 10.1258/135763304323070742. [DOI] [PubMed] [Google Scholar]
- Kysely A, Bishop B, Kane R, Cheng M, De Palma M, Rooney R. Expectations and experiences of couples receiving therapy through videoconferencing: A qualitative study. Frontiers in Psychology. 2020;10:2992–2992. doi: 10.3389/fpsyg.2019.02992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein KL, Scogin F, Thomas SJ, DiNapoli EA, Dillon HR, McFadden A. Telehealth cognitive behavior therapy for co-occurring insomnia and depression symptoms in older adults. Journal of Clinical Psychology. 2013;69:1056–1065. doi: 10.1002/jclp.22030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McGrath, P. J., Lingley-Pottie, P., Thurston, C., MacLean, C., Cunningham, C., Waschbusch, D. A., et al. (2011). Telephone-based mental health interventions for child disruptive behavior or anxiety disorders: Randomized trials and overall analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 1162–1172. 10.1016/j.jaac.2011.07.013 [DOI] [PubMed]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015 doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers K, Nelson E-L, Rabinowitz T, Hilty D, Baker D, Barnwell SS, et al. American Telemedicine Association practice guidelines for telemental health with children and adolescents. Telemedicine and e-Health. 2017;23:779–804. doi: 10.1089/tmj.2017.0177. [DOI] [PubMed] [Google Scholar]
- *Narad, M. E., Minich, N., Taylor, H. G., Kirkwood, M. W., Brown, T. M., Stancin, T., & Wade, S. L. (2015). Effects of a web-based intervention on family functioning following pediatric traumatic brain injury. Journal of Developmental and Behavioral Pediatrics, 36, 700–707. 10.1097/dbp.0000000000000208 [DOI] [PMC free article] [PubMed]
- Norwood C, Moghaddam NG, Malins S, Sabin-Farrell R. Working alliance and outcome effectiveness in videoconferencing psychotherapy: A systematic review and noninferiority meta-analysis. Clinical Psychology & Psychotherapy. 2018;25:797–808. doi: 10.1002/cpp.2315. [DOI] [PubMed] [Google Scholar]
- *Rayner, M., Dimovski, A., Muscara, F., Yamada, J., Burke, K., McCarthy, M., et al. (2016). Participating from the comfort of your living room: Feasibility of a group videoconferencing intervention to reduce distress in parents of children with a serious illness or injury. Child & Family Behavior Therapy, 38, 209–224. 10.1080/07317107.2016.1203145
- Richardson L, Reid C, Dziurawiec S. “Going the extra mile”: Satisfaction and alliance findings from an evaluation of videoconferencing telepsychology in rural Western Australia. Australian Psychologist. 2015;50:252–258. doi: 10.1111/ap.12126. [DOI] [Google Scholar]
- Rogers, B. (2020). A practical guide to working with children and families through telehealth. Retrieved from https://emergingminds.com.au/resources/a-practical-guide-to-working-with-children-and-families-through-telehealth/.
- Rosenthal R. Meta-analytic procedures for social science research. Beverly Hills: Sage Publications; 1984. [Google Scholar]
- *Rotondi, A. J., Haas, G. L., Anderson, C. M., Newhill, C. E., Spring, M. B., Ganguli, R., et al. (2005). A clinical trial to test the feasibility of a telehealth psychoeducational intervention for persons with schizophrenia and their families: Intervention and 3-month findings. Rehabilitation Psychology, 50, 325–336. 10.1037/0090-5550.50.4.325 [DOI] [PMC free article] [PubMed]
- *Sibley, M. H., Comer, J. S., & Gonzalez, J. (2017). Delivering parent-teen therapy for ADHD through videoconferencing: A preliminary investigation. Journal of Psychopathology and Behavioral Assessment, 39, 467–485. 10.1007/s10862-017-9598-6 [DOI] [PMC free article] [PubMed]
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. Australian and New Zealand Journal of Surgery. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- *Stormshak, E. A., Seeley, J. R., Caruthers, A. S., Cardenas, L., Moore, K. J., Tyler, M. S., et al. (2019). Evaluating the efficacy of the Family Check-Up Online: A school-based, eHealth model for the prevention of problem behavior during the middle school years. Development and Psychopathology, 31, 1873–1886. 10.1017/s0954579419000907 [DOI] [PMC free article] [PubMed]
- Stuttard L, Clarke S, Thomas M, Beresford B. Replacing home visits with telephone calls to support parents implementing a sleep management intervention: Findings from a pilot study and implications for future research. Child: Care Health and Development. 2015;41:1074–1081. doi: 10.1111/cch.12250. [DOI] [PubMed] [Google Scholar]
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: Transportation barriers to health care access. Journal of Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran-Lien, A. (2020). Telehealth FAQs for therapists during the COVID-19 coronavirus pandemic. Retrieved from https://www.camft.org/Resources/Legal-Articles/Legal-Department-Staff-Articles/Telehealth-FAQS-for-Therapists-During-COVID-19.
- *Vander Stoep, A., McCarty, C. A., Zhou, C., Rockhill, C. M., Schoenfelder, E. N., & Myers, K. (2017). The Children's Attention-Deficit Hyperactivity Disorder Telemental Health Treatment Study: Caregiver outcomes. Journal of Abnormal Child Psychology, 45, 27–43. 10.1007/s10802-016-0155-7 [DOI] [PMC free article] [PubMed]
- *Wade, S. L., Carey, J., & Wolfe, C. R. (2006). The efficacy of an online cognitive-behavioral family intervention in improving child behavior and social competence following pediatric brain injury. Rehabilitation Psychology, 51, 179. 10.1037/0090-5550.51.3.179
- Wade SL, Cassedy AE, McNally KA, Kurowski BG, Kirkwood MW, Stancin T, Taylor HG. A randomized comparative effectiveness trial of family-problem-solving treatment for adolescent brain injury: Parent outcomes from the Coping with Head Injury through Problem Solving (CHIPS) study. Journal of Head Trauma Rehabilitation. 2019;34:E1–E9. doi: 10.1097/htr.0000000000000487. [DOI] [PubMed] [Google Scholar]
- *Wade, S. L., Kurowski, B. G., Kirkwood, M. W., Zhang, N., Cassedy, A., Brown, T. M., et al. (2015). Online problem-solving therapy after traumatic brain injury: A randomized controlled trial. Pediatrics, 135, E487–E495. 10.1542/peds.2014-1386 [DOI] [PMC free article] [PubMed]
- *Wade, S. L., Taylor, H. G., Yeates, K. O., Kirkwood, M., Zang, H., McNally, K., et al. (2018). Online problem solving for adolescent brain injury: A randomized trial of 2 approaches. Journal of Developmental and Behavioral Pediatrics, 39, 154–162. 10.1097/DBP.0000000000000519 [DOI] [PubMed]
- *Williams, L. K., McCarthy, M. C., Burke, K., Anderson, V., & Rinehart, N. (2016). Addressing behavioral impacts of childhood leukemia: A feasibility pilot randomized controlled trial of a group videoconferencing parenting intervention. European Journal of Oncology Nursing, 24, 61–69. 10.1016/j.ejon.2016.08.008 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of Study 3 are not publicly available due to privacy and ethical approval restrictions. Data were not collected for Study 1 or Study 2.