Abstract
Objective
In this randomized controlled study, we aimed to determine whether non-contact infrared thermometers (NCITs) are more time-efficient and create less patient distress than mercury axillary thermometers (MATs) and infrared tympanic thermometers (ITTs).
Methods
Forty-five rehabilitation inpatients were randomly assigned to one of three groups (NCIT, MAT, and ITT). Time required to measure body temperature with an NCIT, MAT, and ITT was recorded. We examined associations between time required to take patients’ temperature and measuring device used. Patient distress experienced during temperature measurement using the three thermometers was recorded.
Results
A significantly longer average time was required to measure temperatures using the MAT (mean 43.17, standard deviation [SD] 8.39) than the ITT (mean 13.74, SD 1.63) and NCIT (mean 12.13, SD 1.18). The thermometer used influenced the time required to measure body temperature (t = 33.99). There were significant differences among groups (NCIT vs. ITT, NCIT vs. MAT, and ITT vs. MAT) regarding patient distress among the different thermometers. Most distress arose owing to needing help from others, sleep disruption, and boredom.
Conclusion
The NCIT has clinically relevant advantages over the ITT and MAT in measuring body temperature among rehabilitation patients, including saving nurses’ time and avoiding unnecessary patient distress.
Clinical trial registration number (http://www.chictr.org.cn): ChiCTR1800019756.
Keywords: Non-contact infrared thermometer, infrared tympanic thermometer, mercury axillary thermometer, rehabilitation, body temperature measurement, randomized controlled study
Introduction
Inpatient rehabilitation care requires not only a focus on improving functional independence for patients with a wide range of neurologic injuries and illnesses1–3 but also the management and prevention of underlying diseases and infections. Measurement of body temperature, a fundamental vital sign, serves as a basic approach to clinical evaluation and diagnosis; however, there are a number of challenges to acquiring temperature measurements in the rehabilitation setting. Whereas the mercury axillary thermometer (MAT) is preferred for measuring body temperature in many clinical settings,4 the strict disinfection protocols, long measurement times, easily broken glass tubes, mercury leakage, and other operational drawbacks present safety hazards to nursing staff and patients and decrease time efficiency. The relative ease of use of an infrared tympanic thermometer (ITT) makes them appealing; however, the practical clinical use of ITT is limited by low measurement values and sensitivity, combined with the need to sterilize protective covers, store devices in a dust- and contaminant-free environment, overcome challenges posed by the presence of ear canal obstructions, and the possibility of inaccurate measurement arising from errors in probe placement.5–7
The non-contact infrared thermometer (NCIT) has been widely used in children, newborns, and other patients.8–10 However, rehabilitation inpatients often have motor, cognitive, and speech impairment and their clinical manifestations that differ from those of other patients. Therefore, prior to investing considerable resources into NCIT technology refinement and protocol development, there is a critical need to understand whether this technology offers substantial advantages over tools currently being used in the rehabilitation setting. This randomized controlled study was carried out to quantitatively compare use of the NCIT, ITT and MAT in a rehabilitation ward, to investigate whether the NCIT is a safe, comfortable, and efficient body temperature measurement tool for rehabilitation inpatients.
Methods
Study design
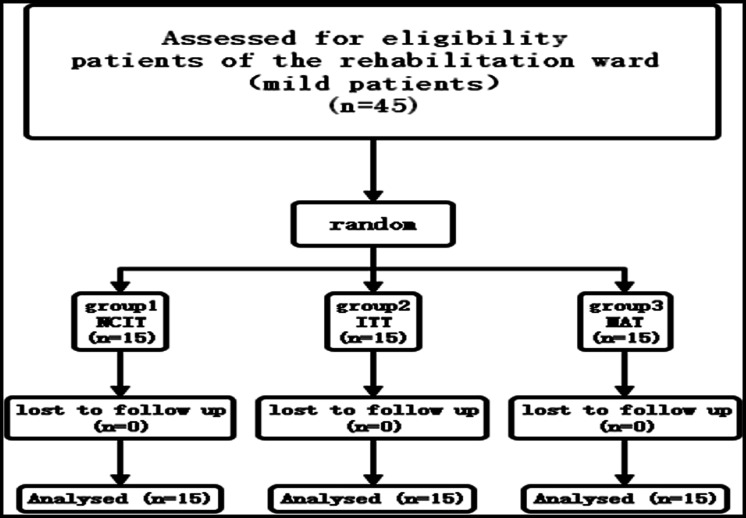
This randomized controlled study was approved by the Institutional Ethics Committee of the First Rehabilitation Hospital of Shanghai, China and was designed and carried out according to CONSORT guidelines. The study was registered in the Chinese Clinical Trial Registry with trial registration number ChiCTR1800019756. Informed consent was obtained from each patient or their family before the trial. The inclusion criteria for participation in the study were: 1) inpatient at a rehabilitation facility; 2) Barthel index score ≥40 (partially dependent to minimal assistance required in activities of daily living); 3) capable of granting consent/assent for study participation. Forty-five inpatients met the inclusion criteria and consented to participate in the study (Figure 1). Using a random number generator, the included participants were assigned to one of three groups (NCIT, ITT, and MAT), with each group consisting of 15 participants.
Figure 1.
Participant flow diagram.
Procedures
Before starting the study, two nurses in charge of temperature measurement and data collection were trained to use each thermometer (i.e., the NCIT, ITT, and MAT). Training procedures conformed to the manufacturers’ recommendations.
Each participant’s body temperature was recorded for 5 days using the thermometer corresponding to the participant’s group assignment. During the 5-day study, participants’ body temperature was measured twice daily (during the periods 6:00–7:00 and 15:00–16:00). During the temperature measurement period, the central air conditioning in the hospital was turned off so as to reduce the impact of ambient temperature on the accuracy of measurement, and the room temperature was maintained at 22°C to 25°C.
The time required for nurses to measure body temperature in each patient was recorded. During each measurement, the nurse also recorded whether the patient was distressed and the nature of distress was documented. Examples of distress included disrupted sleep and boredom.
Statistical analysis
The difference between nurses’ time requirements for measuring patients’ body temperatures was assessed in each group using repeated measures analysis of variance with a Tukey test for post-hoc comparison. Multivariate general linear regression analyses, with measurement time as the dependent variable, were performed to calculate correlation coefficients using the following independent variables: measuring device (NCIT, ITT, or MAT), age, sex, and time of the day when measurement was taken (morning/afternoon). Fisher’s exact test with Bonferroni correction was conducted to compare the frequency and types of distress. Statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set to a value of p < 0.05.
Results
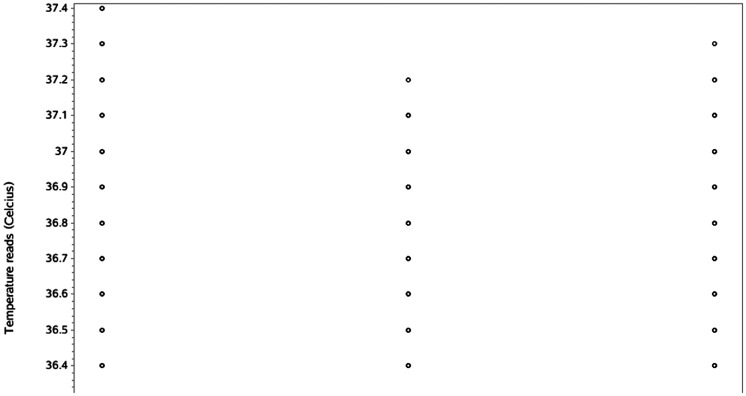
Table 1 describes the measurement procedures used with each type of thermometer. Table 2 shows the clinical characteristics of study participants. The average age of the 45 participants was 54.71 ± 17.73 years, and 62.22% were men. The cohort included participants who had experienced stroke, traumatic brain injury, spinal cord injury, brain tumor, or other diseases. Table 3 presents the types of injury or disease in each group. Although there were slight differences in disease types among the three groups, all patients had nervous system diseases, with stroke the main disease type. The mean temperature (average of 10 measurements) for each participant assigned to the NCIT, ITT, and MAT groups ranged from a low of 36.0°C recorded with an ITT to a high of 37.4°C measured with an NCIT (Figure 2).
Table 1.
Measurement procedures used with each thermometer.
| Thermometer | Procedure |
|---|---|
| Mercury axillary thermometer (MAT) | Before measurement, all MATs were shaken by a nurse until the mercury registered a temperature below 35°C. Then thermometers were placed in a 40°C water bath. MATs were removed from the water after 5 minutes and the temperature was read. Only thermometers reading 40°C ± 0.1°C were used for subsequent measurement. If patients had limb spasm, cognitive impairment, or severe wasting, nurses helped to place the mercury head in the patient’s axilla and assisted in holding the patient’s arms to their chest. Readings were recorded after 5 minutes. |
| Infrared tympanic thermometer (ITT) | Prior to measurement, the ear thermometer lens was checked and cleaned with 75% alcohol. After drying, the lens was covered with protective tape and clamped. After pressing the start button, the ear was pulled back to straighten and expose the external auditory canal and the thermometer was inserted into the canal and pressed down to ensure a good fit so that the device could detect infrared heat emitted by the eardrum and surrounding tissues. The temperature measurement button was again depressed, and following an auditory beep and display of the temperature, the measurement was recorded. |
| Non-contact infrared thermometer (NCIT) | After wiping away any perspiration and hair, the device was positioned perpendicularly, 3–5 cm from the middle portion of the patient’s forehead, centered horizontally between the eyebrows. After pressing the button, the temperature was displayed. This process was repeated three times and the most frequently displayed value was recorded consistent, with the manufacturer’s instructions. |
Table 2.
Basic information of patients (n = 45).
| n | (%) | |
|---|---|---|
| Sex | ||
| Male | 28 | 62.22 |
| Female | 17 | 37.78 |
| Diagnosis | ||
| Stroke | 28 | 62.22 |
| TBI | 6 | 13.33 |
| SCI | 7 | 15.56 |
| Brain tumor | 1 | 2.22 |
| Other | 3 | 6.67 |
| Age, years | ||
| 0–19 | 3 | 6.67 |
| 20–39 | 5 | 11.11 |
| 40–59 | 18 | 40 |
| 60–79 | 18 | 40 |
| 80–89 | 1 | 2.22 |
TBI: traumatic brain injury; SCI: spinal cord injury.
Table 3.
Proportion of diseases in each group, by thermometer type.
| Disease | All | Stroke | TBI | SCI | Brain tumor | Other |
|---|---|---|---|---|---|---|
| n (%) | 45 | 28 (62.22%) | 6 (13.33%) | 7 (15.56%) | 1 (2.22%) | 3 (6.67%) |
| NCIT | 15 | 13 (86.67%) | 1 (6.67%) | 1 (6.67%) | 0 | 0 |
| ITT | 15 | 7 (46.67%) | 3 (20%) | 3 (20%) | 1 (6.67%) | 1 (6.67%) |
| MAT | 15 | 8 (53.33%) | 2 (13.33%) | 3 (20%) | 0 | 2 (13.33%) |
TBI: traumatic brain injury; SCI: spinal cord injury; NCIT: non-contact infrared thermometer; MAT: mercury axillary thermometer; ITT: infrared tympanic thermometer.
Figure 2.
Patients’ temperature measured using three thermometers. Each circle represents mean temperature recorded across 10 measurements for a specific patient; some data points overlapped.
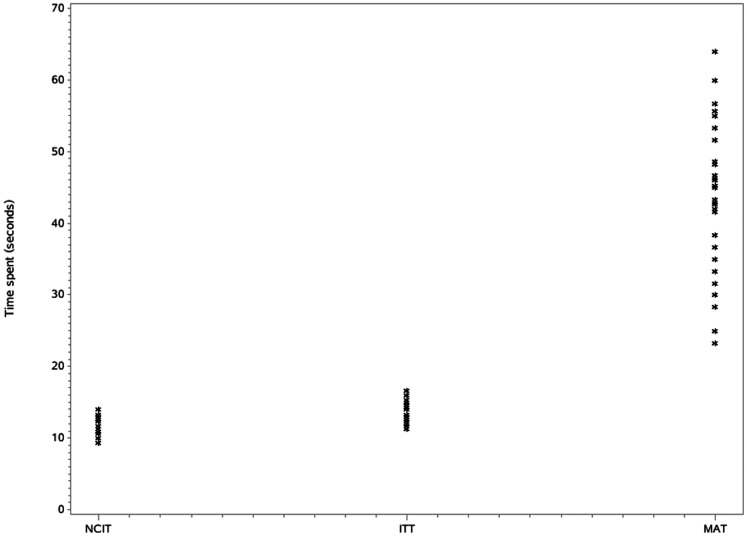
The mean time required for temperature measurement differed significantly across devices (p < 0.001; Table 4 and Figure 3). ITT measurement was related to the patient's body position. There was a large difference in ear temperature between the two sides in a patient lying laterally; however, there was no difference in the supine position. Therefore, nurses performing ear temperature measurement required patients to lie on their back. Moreover, the temperature cap had to be changed and hand disinfection carried out each time the ITT made contact with a patient, which increased the operation time. Body temperature measured using the NCIT did not present the above difficulties. A significantly longer time was required for temperature measurement using the MAT (43.17 s) than the ITT (13.74 s; p < 0.05) and NCIT (12.13 s; p < 0.05) and using the ITT compared with the NCIT (p < 0.05).
Table 4.
Time (in seconds) required by nurses to measure body temperature using different thermometers.
| n | Mean | SD | 95% LCI | 95% UCI | p | ||
|---|---|---|---|---|---|---|---|
| Thermometers | NCIT | 150 | 12.13 | 1.18 | 11.94 | 12.32 | <0.0001 |
| ITT | 150 | 13.74 | 1.63 | 13.48 | 14.00 | ||
| MAT | 150 | 43.17 | 8.39 | 41.81 | 44.52 |
Note: The analytical method is repeated measures analysis of variance. In post-hoc comparison using a Tukey test, the results showed significant differences between any two groups: p < 0.05.
SD: standard deviation; LCI: lower confidence interval; UCI: lower confidence interval; NCIT: non-contact infrared thermometer; MAT: mercury axillary thermometer; ITT: infrared tympanic thermometer.
Figure 3.
Time required to measure patients’ temperature using different thermometers. Each circle represents mean temperature recorded across 10 measurements for a specific patient; some data points overlapped.
Multivariate general linear regression analysis showed that the type of measurement device was a significant factor affecting the time required for nurses to measure body temperature in rehabilitation inpatients (t = 33.99; p < 0.0001, Table 4). The time of day (morning/afternoon) when body temperature was measured was not a significant factor affecting the required measurement time in rehabilitation inpatients (Table 5).
Table 5.
Effect of device and time of measurement (morning/afternoon) on time required for body temperature measurement.
| β | SE | t | p | |
|---|---|---|---|---|
| Measuring device | 15.73 | 0.46 | 33.99 | <0.0001 |
| Measurement time (morning/afternoon) | 0.32 | 0.75 | 0.43 | 0.6668 |
Note: The analytical method is multivariate generalized linear regression.
SE: standard error.
Using Fisher’s exact test with Bonferroni correction, we identified significant differences between each group in terms of patient distress experienced during body temperature measurement (p < 0.0001, Table 6). In particular, the MAT required the most additional help (41.33%) compared with the ITT (0%) and NCIT (0%). In contrast, use of the ITT contributed to significantly greater sleep disruption (21.33%) than use of either the MAT (17.33%) or NCIT (0%), and the MAT contributed to significantly greater sleep disruption than the NCIT (all p < 0.0001).
Table 6.
Frequency and types of distress experienced by rehabilitation inpatients and nurses using different body temperature measurement devices (NCIT, ITT, MAT).
| ND | NH | SD | Boredom | p | ||
|---|---|---|---|---|---|---|
| NCIT | n | 150 | 0 | 0 | 0 | <0.0001 |
| % | 100 | 0 | 0 | 0 | ||
| ITT | n | 118 | 0 | 32 | 0 | |
| % | 78.67 | 0 | 21.33 | 0 | ||
| MAT | n | 62 | 62 | 26 | 0 | |
| % | 41.33 | 41.33 | 17.33 | 0 |
Notes: The analysis method is Fisher’s exact test. There were significant differences between each two combinations among the three groups (NCIT vs. ITT, NCIT vs. MAT, ITT vs. MAT, with Bonferroni correction) (p < 0.05).
NI: No distress; NH: Needed help; SD: Sleep disruption; NCIT: non-contact infrared thermometer; MAT: mercury axillary thermometer; ITT: infrared tympanic thermometer.
Discussion
Use of the MAT, ITT, and NCIT has been studied across a variety of patient populations including newborns,9 children11 and adult patients in intensive care.12 However, to date, no study has focused on comparing the feasibility of using these devices in the inpatient rehabilitation setting. Past studies have investigated the accuracy of body temperature measurement using the three thermometers.13,14 However, our randomized controlled study is the first to examine the potential advantages to using the NCIT compared with the MAT and ITT to improve nurses’ work efficiency and patients’ satisfaction with nursing care.
Safe, efficient, and accurate alternatives to the MAT
At present, the MAT is the primary body temperature measurement tool used in clinical settings in China, partly owing to traditional clinical and educational approaches dating back over 100 years. However, it has been reported that more than 10 tons of mercury waste are treated in China every year owing to MAT breakage. This is concerning given the potentially deleterious impact of mercury on the environment and species, including humans and wildlife.15 For example, in a study of water, sediment, and fish samples, Karunasagar et al.16 identified higher levels of mercury pollution in a lake located in close proximity to a MAT factory than levels measured in two lakes located further away. Thus, in identifying the NCIT as a more time efficient and less burdensome approach to measuring body temperature than a MAT, our study is particularly relevant given the need for more environmentally friendly approaches to body temperature measurement.
Characteristics of the MAT, ITT, and NCIT
Use of the MAT requires patient contact, and although temperature measurement with a MAT is accurate, stable, and produces less error,17 our study findings showed that a longer time is required for nurses to measure patients’ temperature (43.17 s) using a MAT than an NCIT or ITT. Further, most patients in the rehabilitation ward have limb dysfunction, especially unilateral limb dysfunction, or require intensive rehabilitation,18 which make use of the MAT more challenging. Low conformity, insufficient measurement time, or insufficient contact between the thermometer and skin can lead to inaccurate measurements. Additionally, it may be difficult for nurses to read the results and MATs can break easily. Moreover, the steps required for MAT sterilization are complicated and use of these thermometers is prone to cross-infection.
ITT use requires nurses to have a good understanding of the correct location of temperature measurement, normal ear temperature values, applicable objects, contraindications, and other factors. Current studies have shown that body temperature measured using an ITT differs considerably from intravascular measures in that the former is always lower than body temperature measured via intravascular methods.9 Other studies suggest that ITT use increases the risk of tympanic membrane perforation.19 Use of an ITT has other limitations, such as disrupted sleep, ear injury, ear canal blockage, and infection, which can affect the measurement results. In contrast, the NCIT is a simple, quick, no-contact instrument for accurately measuring body temperature. Nurses can detect body temperature from a distance of 5 cm from the patient's forehead and within 2 s. Therefore, the NCIT is suitable for temperature monitoring in patients with different functional limitations in the rehabilitation ward.
Effect of thermometer type on rehabilitation nursing efficiency
Our findings indicated that use of the NCIT was significantly more time efficient for rehabilitation nurses and patients than the MAT or ITT (12.13 vs. 43.17 vs. 13.74 s, respectively; p < 0.0001; Table 4). When caring for only a single patient, this time difference may not be a cause for concern. However, stroke is associated with a greater number of disability-adjusted life-years lost than any other disease in China.20 Further, the burden of stroke is expected to increase in rehabilitation care units. Given the growing emphasis on cost containment and the need to deliver rehabilitation care more efficiently, use of the NCIT could lead to substantial cost savings and improved efficiency in care delivery. Beyond saving nurses time, the more efficient NCIT approach would also allow patients greater time to receive clinical care and to build stronger clinical relationships, which could lead to improved patient quality of care and outcomes.
Distress among patients and nurses using different measurement devices
Nurses did not need assistance when using the NCIT and patients did not report sleep disruption during measurement, two findings that contrast sharply with those documented for the MAT and ITT groups (Table 6). In particular, when using the MAT, nurses reported requiring assistance in 41.33% of measurements and patients reported sleep disruption in 17.33% of measurements. Most rehabilitation patients experience some level of limb dysfunction including limited mobility, spasticity, and uncontrolled movements. This dysfunction makes placement and stabilization of the MAT more challenging17 and can lead to an increased risk of breakage if the device is accidentally dropped or crushed. Thus, assistance from a second clinical staff member may be required to safely measure temperatures using the MAT. Whereas nurses did not require assistance using the ITT, patients did report experiencing sleep disruption in 21.33% of measurements. Because the ITT must be inserted into the ear, this approach may increase the risk of tympanic membrane perforation.19 To reduce the risk of injury, the ear must be manipulated, thus leading to a greater risk of disrupted sleep. Medical conditions such as ear injury, blockage, or infection can hinder accurate temperature recording. Additionally, whether a MAT or an ITT, when the patient has hemiplegia, only measuring temperature on one side of the body can effect accurate temperature readings whereas measuring temperature on both sides would disturb the patient and increases the workload of the nurse.21
Limitations
Owing to the design of this study, we could not compare the specific values of patients’ body temperature measured using the three thermometers in the same patient, because we felt that all readings from each device were accurate,9,13 as can be seen in our data (Figures 2 and 3). Furthermore, we primarily included rehabilitation inpatients with higher levels of functioning; however, different levels of functional independence may contribute to differences across clinical sites. Further investigation in needed to confirm our findings. Finally, this was a single-center study; a larger, randomized, controlled, double-blind clinical trial conducted at multiple centers is warranted to confirm the present results.
Conclusion
In the present study, we observed some challenges to patients during measurement as well as to nursing efficiency. Our study findings showed that the NCIT is efficient and safe and can improve patients’ satisfaction with medical care during rehabilitation. Given that the NCIT does not require skin contact to measure body temperature, use of this device can potentially reduce the risk of cross-infection among patients owing to instrument contact, especially in patients referred from the intensive care unit. In the global fight against infectious disease epidemics, use of the NICT can reduce the direct physical contact between patients and medical staff. Additionally, the NCIT does not use mercury, thereby reducing mercury pollution caused by MAT manufacture and breakage. In future research, consistency in the differences in clinical measurement among these three methods should be confirmed, to provide more robust evidence for recommending the NCIT as a replacement for the MAT in clinical practice. We believe that the use of non-contact electronic thermometers, which are accurate, safe, non-invasive, easy to use, and low cost, should be promoted in the future. This device is worth advocating in the rehabilitation ward as well as being actively promoted in clinical wards and outpatient clinics.
Acknowledgements
The authors thank Dr. Joseph Siu at the University of Nebraska Medical Center and Dr. Judy Burnfield at Madonna Rehabilitation Hospital for their valuable suggestions on the study.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received grants from Shanghai Medical Key Specialty (Project No. ZK2019B11) and Project of Shanghai Health Committee (Project No. 201740198, 20194Y0187).
ORCID iD: Zhen Chen https://orcid.org/0000-0002-3565-5707
References
- 1.Ajimsha MS, Kooven S, Al-Mudahka N. . Adherence of physical therapy with clinical practice guidelines for the rehabilitation of stroke in an active inpatient setting. Disabil Rehabil 2019: 41: 1855–1862. [DOI] [PubMed] [Google Scholar]
- 2.Deng G, Pooyania S. Addressing the Barriers Preventing Guideline Adherence for Blood Pressure Measurement on an Inpatient Stroke Rehabilitation Ward. Int J Stroke 2018; 13: 169. [Google Scholar]
- 3.Chen CM, Yang YH, Chang CH, et al. Effects of Transferring to the Rehabilitation Ward on Long-Term Mortality Rate of First-Time Stroke Survivors: A Population-Based Study. Arch Phys Med Rehabil 2017; 98: 2399–2407. [DOI] [PubMed] [Google Scholar]
- 4.Marui S, Misawa A, Tanaka Y, et al. Assessment of axillary temperature for the evaluation of normal body temperature of healthy young adults at rest in a thermoneutral environment. J Physiol Anthropol 2017; 36: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duru CO, Akinbami FO, Orimadegun AE. A comparison of tympanic and rectal temperatures in term Nigerian neonates. BMC Pediatr 2012; 12: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Apa H, Gozmen S, Bayram N, et al. Clinical accuracy of tympanic thermometer and noncontact infrared skin thermometer in pediatric practice: an alternative for axillary digital thermometer. Pediatr Emerg Care 2013; 29: 992–997. [DOI] [PubMed] [Google Scholar]
- 7.Gasim GI, Musa IR, Abdien MT, et al. Accuracy of tympanic temperature measurement using an infrared tympanic membrane thermometer. BMC Res Notes 2013; 6: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Apa H, Gozmen S, Keskin-Gozmen S, et al. Clinical accuracy of non-contact infrared thermometer from umbilical region in children: A new side. Turk J Pediatr 2016; 58: 180–186. [DOI] [PubMed] [Google Scholar]
- 9.Sollai S, Dani C, Berti E, et al. Performance of a non-contact infrared thermometer in healthy newborns. BMJ Open 2016; 6: e008695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basak T, Aciksoz S, Tosun B, et al. Comparison of three different thermometers in evaluating the body temperature of healthy young adult individuals. Int J Nurs Pract 2013; 19: 471–478. [DOI] [PubMed] [Google Scholar]
- 11.Wang K, Gill P, Wolstenholme J, et al. Non-contact infrared thermometers for measuring temperature in children: primary care diagnostic technology update. Br J Gen Pract 2014; 64: e681–e683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawson L, Bridges EJ, Ballou I, et al. Accuracy and precision of noninvasive temperature measurement in adult intensive care patients. Am J Crit Care 2007; 16: 485–496. [PubMed] [Google Scholar]
- 13.Teran CG, Torrez-Llanos J, Teran-Miranda TE, et al. Clinical accuracy of a non-contact infrared skin thermometer in paediatric practice. Child Care Hlth Dev 2012; 38: 471–476. [DOI] [PubMed] [Google Scholar]
- 14.Chiappini E, Sollai S, Longhi R, et al. Performance of non-contact infrared thermometer for detecting febrile children in hospital and ambulatory settings. J Clin Nurs 2011; 20: 1311–1318. [DOI] [PubMed] [Google Scholar]
- 15. The Madison declaration on mercury pollution. Ambio 2007; 36: 62–65. [PubMed] [Google Scholar]
- 16.Karunasagar D, Krishna MVB, Anjaneyulu Y, et al. Studies of mercury pollution in a lake due to a thermometer factory situated in a tourist resort: Kodaikkanal, India. Environ Pollut 2006; 143: 153–158. [DOI] [PubMed] [Google Scholar]
- 17.Franconi I, La Cerra C, Marucci AR, et al. Digital Axillary and Non-Contact Infrared Thermometers for Children. Clin Nurs Res 2018; 27: 180–190. [DOI] [PubMed] [Google Scholar]
- 18.Aadal L, Fog L, Pedersen AR. Tympanic ear thermometer assessment of body temperature among patients with cognitive disturbances. An acceptable and ethically desirable alternative? Scand J Caring Sci 2016; 30: 766–773. [DOI] [PubMed] [Google Scholar]
- 19.Yang WC, Kuo HT, Lin CH, et al . Tympanic temperature versus temporal temperature in patients with pyrexia and chills. Medicine (Baltimore) 2016; 95: e5267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol 2019; 18: 394–405. [DOI] [PubMed] [Google Scholar]
- 21.Alfieri FM, Massaro AR, Filippo TR, et al. Evaluation of body temperature in individuals with stroke. NeuroRehabilitation 2017; 40: 119–128. [DOI] [PubMed] [Google Scholar]