Abstract
Background:
Tibial tubercle osteotomy with concomitant distalization for the treatment of patellar instability remains controversial, as it may cause anterior knee pain and chondral degeneration.
Purpose:
To evaluate radiographic, clinical, and functional outcomes in patients who had patellar instability with patella alta and underwent tibial tubercle osteotomy with distalization (TTO-d) as well as medial patellofemoral ligament reconstruction.
Study Design:
Case series; Level of evidence, 4.
Methods:
Included in this study were 25 patients (31 cases) (mean age at surgery, 28.7 years; range, 14-33 years) with patellar instability and patella alta who underwent TTO-d with minimum 1-year follow-up. The Caton-Deschamps index (CDI), tibial tubercle–trochlear groove (TT-TG) distance, and amount of distalization were assessed. Clinical and functional variables included J-sign, anterior knee pain, apprehension test, Tegner activity level, and Kujala score.
Results:
The mean follow-up period was 2.62 years. The mean TT-TG was 16.15 mm (range, 7-24 mm); the mean CDI changed from 1.37 (1.25-1.7) preoperatively to 1.02 (0.9-1.12) postoperatively (P = .001); and the mean amount of tibial tubercle distalization was 8.80 mm (range, 4-16 mm). Lateral release (22 cases; 71.0%), medialization of tibial tubercle (17 cases; 54.8%), and autologous chondrocyte implantation (4 cases; 12.9%) were other associated procedures. The J-sign improved in 30 cases (96.8%; P = .001), and there was a complete resolution of anterior knee pain in 22 cases (71.0%; P = .001). An exploratory analysis showed that patellar cartilage defect severity was correlated with persistent pain (P = .005). The apprehension test became negative in all cases (P = .001). The median Kujala score increased from 52 to 77 (P = .001), and the median Tegner activity level improved from 3 to 4 (P = .001). No cases of osteotomy nonunion were reported. One case (3.2%) of patellar instability recurrence and 3 cases (6.5%) with painful hardware were observed.
Conclusion:
TTO-d resulted in good radiographic, clinical, and functional outcomes providing proper patellar stability to patients with patella alta. TTO-d appears to be a safe and efficient procedure with low complication rates, providing an additional tool for the personalized treatment of patellar instability.
Keywords: patellofemoral joint, knee surgery, osteotomy, joint instability
Patellar instability is a result of alterations of normal knee kinematics involving both static and dynamic stabilizers of the patella.22 Excessive tibial tuberosity lateralization measured by the tibial tuberosity–trochlear groove (TT-TG) distance, trochlear dysplasia, and patellar height are major factors associated with recurrent patellar instability.3,15,30 Moreover, patellar dislocation occurs in 2% to 3% of orthopaedic presentations related to the knee, occurring more frequently in younger and more active populations.4,15
Approximately a quarter of patients who experience patellar dislocation have patella alta,11 which is characterized by Caton-Deschamps index6 (CDI)>1.2.11,23 Different surgical options have been proposed to correct the anatomic abnormalities associated with patellar instability, and the combination of soft tissue and bone procedures is potentially beneficial.8,13 Regarding patella alta, tibial tubercle osteotomy (TTO) with concomitant distalization (TTO-d) is an effective technique to decrease patellar height, thus reducing the risk of dislocations. However, the indication for this procedure remains controversial among orthopaedic surgeons as it can increase patellofemoral contact pressure, leading to anterior knee pain and chondral degeneration21,23,29 in addition to loss of fixation, impairment of bone healing, and fractures.16,21,24
Treatment strategies for patella alta are still poorly explored, particularly TTO-d and its results.19 The present study aimed to evaluate radiographic, clinical, and functional outcomes in patients with patella alta who underwent TTO-d as an associated procedure to medial patellofemoral ligament (MPFL) reconstruction with a minimum follow-up of 1 year. We hypothesized that TTO-d, despite the potential complications, is a safe and effective associated procedure to treat patellar instability that accompanies patella alta.
Methods
This work was approved by the local ethics review board. This retrospective case series ultimately included 25 patients (31 knees) with patellar instability and patella alta who underwent TTO-d associated with MPFL reconstruction. The surgeries were performed between 2013 and 2019 at a tertiary care university hospital. Inclusion criteria were skeletal maturity; diagnosis of patellar instability by one of the senior authors (R.G.G.), based on history, physical examination findings, and imaging (with at least 1 episode of dislocation); and CDI >1.2. The study excluded patients who underwent additional procedures such as trochleoplasty or varus or valgus deformity osteotomy and patients with previous knee surgery or femoral and/or tibial torsion. Only lateral retinacular release (LRR) and chondral repair were accepted as combined procedures. LRR was performed in cases of excessive lateral retinaculum tightness, determined by a positive patellar tilt test or limitation of patellar medial passive translation. International Cartilage Regeneration and Joint Preservation Society5 (ICRS) grade 4 chondral lesions >1 cm2 of the patella or trochlea, assessed by preoperative magnetic resonance imaging (MRI), were treated by matrix-induced autologous chondrocyte implantation (MACI).
Surgical Procedure
The skin was incised in a longitudinal (paramedian) fashion directly over the tibial tubercle, initiating in the proximal edge and finishing 6 to 7 cm distal to the tibial tubercle. The medial and lateral borders of the patellar tendon were identified. The osteotomy was performed by completely detaching the tibial tubercle fragment, creating a bone fragment 6 cm long and 8 mm thick. The amount of distalization was calculated to ensure an intraoperative CDI between 1 and 1.2. Additionally, distalization was determined by positioning the inferior pole of the patella at the level of the anterior projection of the Blumensaat line, with knee in 30° to 45° of flexion. Bone was removed from the distal edge of the tibial tubercle fragment to allow distalization. In all cases, the center of the patellar tendon was aligned to the trochlear groove at 90° of knee flexion independent of TT-TG; this required medialization in some patients. Once satisfactory alignment was achieved after tibial tubercle transfer, final fixation was made with two 3.5-mm bicortical screws without washers.
We have recognized the following pearls of TTO-d from our experience:
Use a large bone fragment.
Employ 3.5-mm lag compression screws.
Avoid overcorrection (keep the inferior pole of the patella tangential to the anterior projection of the Blumensaat line).
Apply early rehabilitation without weightbearing restriction.
In all cases, MPFL reconstruction was performed using a gracilis autograft. The gracilis tendon was chosen because it is sufficient to replicate the native MPFL resistance of approximately 200 N.14,20 We have experience with this graft, and previous studies have shown satisfactory outcomes after MPFL reconstruction using gracilis autograft.9,27
The patellar insertion was identified at the transition between the middle and proximal third of the patellar medial border. The femoral insertion was determined under fluoroscopic guidance using Schöttle parameters.26 First, the femoral attachment was fixed with a 5.0-mm anchor or biotenodesis screw. Next, the graft was passed between the second and third layers of the retinaculum. The knee was placed at approximately 45° of flexion to guarantee patellotroclear engagement and stabilization to avoid medialization during graft fixation at the patella with a 3.5- or 5.0-mm anchor. During patellar fixation, the graft is pulled only enough to remove slackness, preventing overtensioning. Adequate tension was confirmed in extension with preservation of manual patellar lateralization of 1 quadrant.
All patients underwent the same rehabilitation protocol. Patients were maintained with an extended knee brace for walking from the first day until the sixth postoperative week. Physiotherapy was initiated on the first postoperative day with isometric exercises and passive exercises to improve range of motion (ROM), aiming to achieve 90° of flexion within 4 weeks and full range of motion at 6 to 8 weeks. Weightbearing was allowed with crutches as tolerated, and patients progressed to full weightbearing as soon as adequate muscular control was achieved. Extension resisted exercises were allowed only after bone consolidation. Open kinetic chain exercises were avoided for about 10 weeks. Return to full activity was recommended 4 to 6 months after surgery.
Data Collection
Patient demographic characteristics and clinical, radiographic, and functional assessments were collected before surgery and at the later follow-up. Radiographic analysis was based on CDI, the TT-TG distance, the amount of distalization represented by the TTO-d gap (Figure 1), and the Dejour classification for trochlear dysplasia.17 These analyses were assessed by standard lateral radiographs and computed tomography (CT) scans of these patients.
Figure 1.
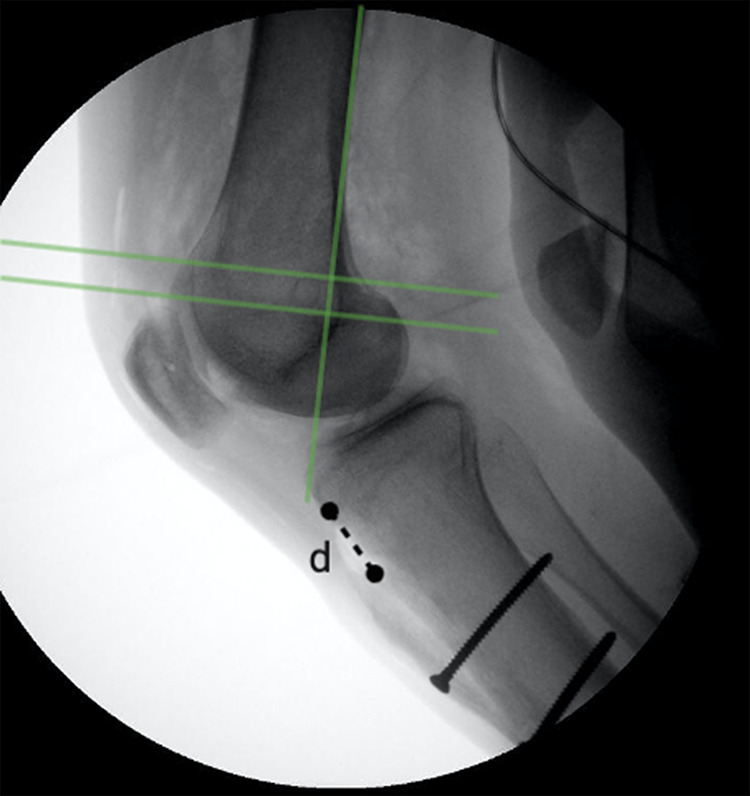
The tibial tubercle osteotomy with distalization (TTO-d) gap as an indirect measure for the amount of distalization (d).
Lateral radiographs were performed with the patient’s knee in 20° to 30° of flexion. Trochlear dysplasia was assessed through the Dejour classification.17 Two authors (C.B.G.L. and T.P.S.) assessed the CDI (preoperatively and at the final follow-up) and the amount of distalization represented by the TTO-d gap; the mean of both measurements was considered for analysis. The CT scans and MRI studies were assessed by the same authors. They evaluated the TT-TG distance (CT scan) and the presence of a knee chondral lesion (MRI) before surgery. Additionally, all patients had a full-length weightbearing radiograph performed preoperatively to assess lower limb alignment.
Clinical and functional evaluations relied on pre- and postoperative patient records, including ROM; anterior knee pain; the patellar apprehension test; the J-sign, classified into mild (<2 quadrants of lateralization) and severe (>2 quadrants of lateralization); the Tegner activity scale; and the Kujala score.
Statistical Analysis
Numerical variables were described as mean and standard deviation when the distribution was normal and as median and interquartile range when the distribution was nonnormal, according to Shapiro-Wilks test and histogram analysis. Categorical variables were described by absolute value and percentage.
According to data distribution, unpaired or paired t test for normal variables, as well as Mann-Whitney or Wilcoxon tests for nonnormal variables, were used to analyze the differences between or within groups, respectively. The Friedman test was used to compare >2 variables. For categorical variables, the Fisher exact test was used in the respective contingency tables. Additionally, a post hoc subgroup analysis was performed to assess how persistent postoperative pain was associated with patient or treatment variables. Spearman rank correlations were calculated to determine the relationship between patellar cartilage defect severity and persistent pain. Statistical significance was set at P < .05.
Results
A total of 41 medical records were reviewed for inclusion criteria. Of those, 8 were excluded due to additional procedures performed, and an additional 2 cases did not have adequate follow-up. As such, a total of 31 knees (25 patients) were included in the study. All included patients were assessed for a minimum of 1 year after surgery. The mean postoperative follow-up was 2.62 ± 1.49 years. Recurrent dislocation was the most common type of patellar dislocation (87.1%), followed by habitual dislocation (9.7%) and acute dislocation (3.2%). Baseline characteristics are reported in Table 1. It is noteworthy that the habitual dislocation cases did not present significant differences regarding demographic characteristics, imaging and clinical findings, and functional outcomes in comparison with the rest of the patients. Specific analysis of this subgroup of patients was not included due to the small number of cases and the exploratory nature of this analysis.
TABLE 1.
Characteristics of the Study Patientsa
| Characteristic | Value |
|---|---|
| No. of patients/knees | 25/31 |
| Sex | |
| Female | 22 (86.9) |
| Male | 3 (13.1) |
| Age, y, mean (range) | 28.7 (14-33) |
| Side | |
| Right knee | 15 (48.4) |
| Left knee | 16 (51.6) |
| Type of patellar dislocation | |
| Recurrent | 27 (87.1) |
| Habitual | 3 (9.7) |
| Acute | 1 (3.2) |
| Lower limb alignment | |
| Valgus | 15 (48.4) |
| Neutral | 13 (41.9) |
| Varus | 3 (9.7) |
aData are reported as n (%) unless otherwise indicated.
Imaging Examination
The results of the imaging examination are shown in Table 2. The mean preoperative CDI assessed by radiograph was 1.37 (range, 1.25-1.7). Trochlear dysplasia was found in all patients, with Dejour type C being the most common type (n = 12 patients; 38.7%). The mean TT-TG distance was 16.15 mm (range, 7-24 mm). Regarding the postoperative evaluation, the amount of distalization was 8.80 mm (range, 4-16 mm). At the immediate postoperative assessment, mean CDI was 1.02 (range, 0.9-1.12). At the later follow-up, it was 1.02 (range, 0.9-1.12) (Table 2). In addition, 15 cases (48.4%) had associated chondral lesion while 4 required specific surgical treatment (MACI). There were no cases of radiographic articular degeneration at the latest follow-up.
TABLE 2.
Results of Imaging Evaluationa
| Variable | Value | P Value |
|---|---|---|
| Caton-Deschamps index | <.001 b,c; .281d | |
| Preoperative | 1.37 (1.25-1.7) | |
| Postoperative | ||
| Immediate | 1.02 (0.90-1.12) | |
| Later follow-up | 1.02 (0.90-1.12) | |
| TT-TG, preoperative, mm | 16.15 (7-24) | |
| Amount of distalization, mm | 8.80 (4-16) | |
| Trochlear dysplasia (Dejour classification), n (%) | ||
| Type A | 7 (22.6) | |
| Type B | 2 (6.5) | |
| Type C | 12 (38.7) | |
| Type D | 10 (32.3) |
aMeasurements are expressed as mean (range) unless otherwise indicated. Bolded value indicates statistical significance (P < .05). TT-TG, tibial tubercle–trochlear groove distance.
bPaired t test between pre- and immediate postoperative assessments.
cPaired t test between pre- and late postoperative assessments.
dPaired t test between immediate postoperative and late postoperative assessments.
Surgical Procedures
All patients underwent TTO-d. MPFL reconstruction was performed in all cases. Lateral retinaculum release was combined in 22 cases (71.0%). In 17 cases (54.8%), medialization of tubercle tibial was also needed. Further, 4 cases (12.9%) required MACI to treat cartilage lesions.
Clinical and Functional Evaluation
The median Kujala score increased significantly from baseline (52; range, 28-70) to the later evaluation (77; range, 59-96). Similarly, the Tegner activity scale improved significantly over time (Table 3).
TABLE 3.
Functional Outcomes in the Pre- and Late Postoperative Assessmentsa
| Preoperative | Late Postoperative | P Valueb | |
|---|---|---|---|
| Tegner activity scale | 3 (1) | 4 (1) | <.001 |
| Kujala score | 52 (13) | 77 (12) | <.001 |
aData are reported as median (interquartile range). Bolded P values indicate statistically significant between-group difference (P < .05).
bWilcoxon test.
Table 4 summarizes the clinical findings. All cases initially had a positive patellar apprehension test, and all were resolved after surgery. The J-sign was present in all patients. Preoperatively, 29 cases (93.5%) had a severe J-sign and 2 cases (6.5%) had a mild J-sign. Normalization of the J-sign was not observed after the intervention. However, all but 1 case had an improvement compared with the preoperative assessment.
TABLE 4.
Clinical Signs of Patients in the Preoperative and Late Postoperative Assessmentsa
| Preoperative | Late Postoperative | P Valueb | |
|---|---|---|---|
| Apprehension test | <.001 | ||
| Normal | 1 (3.2) | 31 (100) | |
| Mild | 6 (14.9) | 0 | |
| Severe | 24 (77.4) | 0 | |
| J-sign | <.001 | ||
| Normal | 0 | 0 | |
| Mild | 2 (6.5) | 30 (96.8) | |
| Severe | 29 (93.5) | 1 (3.2) | |
| Anterior knee pain | <.001 | ||
| Absent | 2 (6.5) | 22 (71.0) | |
| Mild | 10 (32.2) | 8 (25.8) | |
| Severe | 20 (64.5) | 1 (3.2) |
aData are reported as n (%). Bolded P values indicate statistically significant between-group difference (P < .05).
bFisher exact test.
A total of 9 cases (29%) entailed persistent postoperative pain. We performed an exploratory post hoc subgroup analysis to assess how persistent postoperative pain was associated with patient or treatment variables. Cases were divided into 2 groups: “no persistent pain” and “persistent pain.” Group characteristics are displayed in Table 5. Patellar cartilage defect severity (by ICRS grades) was correlated with persistent pain (P = .005). The odds ratio for persistent pain in patients with or without high grade cartilage defects (ICRS grade 3 or 4) was 12.5 (P = .012).
TABLE 5.
Comparison Between Patients With and Without Persistent Postoperative Paina
| No Persistent Pain (n = 22; 71%) |
Persistent Pain (n = 9; 29%) |
P Value | |
|---|---|---|---|
| Age, y | 27.5 (14-39) | 31.9 (21-47) | .131b |
| Follow-up, y | 2.71 ± 1.57 | 2.41 ± 1.32 | .619b |
| Caton-Deschamps index, preoperative | 1.38 ± 0.11 | 1.35 ± 0.06 | .535b |
| Caton-Deschamps index, postoperative | 1.02 ± 0.04 | 1.01 ± 0.03 | .613b |
| TT-TG, preoperative, mm | 15.33 ± 5.19 | 16.71 ± 4.84 | .485b |
| Amount of distalization, mm | 9.02 ± 2.97 | 8.24 ± 1.96 | .778 |
| Chondral injury (ICRS grade) | .005 c | ||
| No injury | 15 (68.2) | 2 (22) | |
| Grade 1 | 3 (13.6) | 1 (11.1) | |
| Grade 2 | 2 (9.1) | 1 (11.1) | |
| Grade 3 | 1 (4.5) | 2 (22.2) | |
| Grade 4 | 1 (4.5) | 3 (33.3) | |
| Kujala score, preoperative | 52.5 (16.5) | 52 (8.5) | 0.334d |
| Kujala score, postoperative | 81 (13) | 74 (14) | 0.219d |
aValues are expressed as median (interquartile range), mean ± SD, or n (%). Bolded P value indicates statistically significant between-group difference (P < .05). ICRS, International Cartilage Repair Society; TT-TG, tibial tubercle–trochlear groove distance.
bUnpaired t test.
cSpearman correlation.
dMann-Whitney test.
Complications
There were no cases of bone consolidation disorders. All patients had complete osteotomy consolidation within a 3-month postoperative period. During the later follow-up, 1 case (3.2%) of patellar instability recurrence was reported. One case (3.2%) showed reduced ROM, with complete extension but 110° of maximum flexion, and 2 cases (6.5%) had hardware pain over the tibial tubercle screw. No additional surgical procedure was required in either situation. Only 1 major complication was found, a postoperative infection requiring surgical debridement and screw removal. Despite the complication, the case proceeded with good clinical and radiographic parameters.
Discussion
The most important finding of the present study was that TTO-d as an associated procedure in the treatment of patellar instability with patella alta had good radiographic, clinical, and functional outcomes. The only complication directly related to the osteotomy was hardware pain, which occurred in only 2 cases. The procedure did not negatively affect anterior knee pain, recurrence, or functional activity as assessed by the Kujala score and Tegner activity scale.
Patella alta is among the major risk factors associated with patellar instability.3,7,11,19 Dejour and Saggin10 noted the presence of patella alta in 24% of patients with recurrent patellar dislocation compared with 3% in a normal control group. Moreover, even in the absence of patellar instability, patella alta was correlated with cartilage lesions in the patellofemoral joint.2
In a case series, Feller et al12 demonstrated satisfactory results in isolated MPFL reconstruction for CDI >1.2. Those authors and others12,18,28 proposed in their reports that cutoff values as high as 1.4 should be used. Similarly, Sappey-Marinier et al25 considered a higher CDI (1.3) as the lower limit for TTO-d indication. They concluded that patella alta with CDI >1.3 (OR, 4.9; P = .02) and preoperative J-sign (OR, 3.9; P = .04) were the only risk factors for reconstruction failure. Exceptions should be considered in cases of trochlear dysplasia associated with patella alta, as these are the 2 major factors responsible for modifying patellar tracking. Therefore, lower CDI values may be used.18
The J-sign represents the lateral translation of the patella in the terminal extension of the knee. In our study, the J-sign was present in all patients and, despite the absence of normalization, all but 1 patient presented significant improvement. In this regard, we have shown that TTO-d with MPFL reconstruction was not enough to normalize the J-sign. Therefore, J-sign occurrence is probably associated with factors other than patella alta. In agreement with that, Sappey-Marinier et al25 found no significant association between the J-sign and patella alta with a CDI ≥1.3 (OR, 1.5; P = .30); however, those investigators observed a significant correlation between J-sign and types B and D trochlear dysplasia (OR, 16.9; P = .001). Interestingly, in our study, all patients had some degree of trochlear dysplasia, and approximately one-third had type D trochlea. None had a large bump or spur with boss height >5 mm, and therefore trochleoplasty was not indicated. Of note, we usually advocate trochleoplasty in cases of type B or D trochlea associated with a boss height >6 mm.10
TTO-d is an effective procedure to correct patellar height, preventing recurrent dislocation and resolving anterior knee pain. This procedure increases patellar stability, favoring the earlier engagement of the bone in the trochlea during knee flexion-extension movements.11 Thus, TTO-d has been appreciated as a therapeutic option for patellar instability. Indeed, a systematic review summarized the positive impact of TTO-d regarding patellofemoral stability.19
Among the complications related to TTO-d, osteotomy site nonunion, an increase in the patellofemoral pressure, and recurrent patellar dislocation are the most common. The overall risk of complications after TTO is relatively low.21 However, the risk is higher when the osteotomy involves complete detachment of the tibial tubercle, impairing the consolidation process. In this regard, Johnson et al16 compared complications after TTO (with or without distalization) and found that delayed union was the only significant negative event occurring in the distalization group. Aiming to decrease complications, Ambra et al3 described an alternative technique for Fulkerson-type anteromedialization TTO. By using a different proximal cut, this technique achieved distalization while preserving the proximal buttress, without leaving a proximal empty gap and leading to a mechanically more stable osteotomy. In our study, osteotomy was performed by total tibial tubercle detachment leading to a proximal gap. Nevertheless, there were no cases of fixation failure or bone consolidation disturbances. This can be explained by the generation of a large bone fragment associated with a good reduction, the interfragmentary compression, and stable lag cortical screw fixation. Additionally, 3.5-mm screws were used because small-diameter screws potentially result in fewer hardware complaints. Washers were not used, and screw heads were partially advanced inside the tendon and the bone, leaving no prominence. This hypothesis is corroborated by Johnson et al, who found 10 times more symptoms (pain or prominence) with 4.5-mm screws in comparison with 3.5-mm screws.
Regarding patellofemoral contact pressure, it was previously observed that after distalization, there was a 55% increase in contact pressure at 10° in relation to 0° of knee flexion,29 theoretically causing overload in the patellofemoral joint and persistence of anterior knee pain. However, a clinical study has shown that TTO-d, indicated for painful patella alta without dislocation, could improve both knee pain and function.1 Similar findings were observed in our study, as most cases (71%) evolved to complete improvement of anterior knee pain. In fact, at a minimum of 2 years postoperatively, 80% of cases had complete resolution of pain and there were no cases of worsening pain after distalization. Interestingly, our post hoc analysis suggested that persistent pain after TTO-d relates positively to patellar cartilage defect severity. Although these findings are interesting, they result from an exploratory analysis, and future studies should be performed to better understand this correlation.
In the current study, there were no cases of overcorrection or progressive distalization leading to patella baja (characterized by CDI <0.8). All patients had a CDI close to 1.0 (mean, 1.02; range, 0.90-1.12), with a mean distalization measure of 8.80 mm. Immediate postoperative CDI and CDI at the later evaluation remained practically unchanged. We believe that our technique of correcting the patellar height by leveling the inferior patellar pole with the Blumensaat line favors avoidance of overcorrection and patella baja, thus minimizing pain and overload.
A systematic review by Magnussen et al19 reported low risks for recurrent patellar dislocation after TTO-d. Moreover, this work identified a small amount of radiographic evidence of patellofemoral osteoarthritis in 5 to 10 years of follow-up. Those features were not observed in our study despite the short follow-up period.
This study has some limitations. Because it was a retrospective case series, there was no randomization or standardization of patients or surgical procedures performed in combination with TTO-d. In addition, a control group was not included. Even so, the main objective of this work is to demonstrate the safety and efficacy of TTO-d for patellar height correction. No gold standard treatment exists for patellofemoral instability, and a large spectrum of alterations related to the pathology have been observed. Therefore, case series studies with satisfactory results are important to the study of different techniques, justifying future comparative studies. An adequate number of patients were included, with a mean follow-up of >2 years. Postoperative MRI would allow a better evaluation of articular chondral conditions, but it was not performed at the postoperative assessments given the high cost of MRI examination and the absence of complaints. Thus, the lack of MRI results is also a limitation of the present study. Altogether, we present evidence that TTO-d is a safe and valuable procedure in patients with closed physis and CDI >1.2.
Conclusion
This study showed that TTO-d leads to good radiographic, clinical, and functional outcomes. It is an efficient and safe procedure with low complication rates, providing a good method to personalize treatment of patients with patellar instability and patella alta.
Footnotes
Final revision submitted July 30, 2020; accepted September 14, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (study ID: 13507419.6.0000.0068).
References
- 1. AL-Sayyad MJ, Cameron JC. Functional outcome after tibial tubercle transfer for the painful patella alta. Clin Orthop Relat Res. 2002;(396):152–162. [DOI] [PubMed] [Google Scholar]
- 2. Ambra LF, Hinckel BB, Arendt EA, Farr J, Gomoll AH. Anatomic risk factors for focal cartilage lesions in the patella and trochlea: a case-control study. Am J Sports Med. 2019;47(10):2444–2453. [DOI] [PubMed] [Google Scholar]
- 3. Ambra LF, Phan A, Gomoll AH. A new technique for distalization of the tibial tubercle that allows preservation of the proximal buttress. Orthop J Sports Med. 2018;6(9):2325967118798621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21(3):499–519. [DOI] [PubMed] [Google Scholar]
- 5. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85(suppl 2):58–69. [DOI] [PubMed] [Google Scholar]
- 6. Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera: apropos of 128 cases [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 7. Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2):305–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cerciello S, Corona K, Morris BJ, et al. Cross-cultural adaptation and validation of the Italian versions of the Kujala, Larsen, Lysholm and Fulkerson scores in patients with patellofemoral disorders. J Orthop Traumatol. 2018;19(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. [DOI] [PubMed] [Google Scholar]
- 10. Dejour D, Saggin P. The sulcus deepening trochleoplasty—the Lyon’s procedure. Int Orthop. 2010;34(2):311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Enea D, Canè PP, Fravisini M, Gigante A, Dei Giudici L. Distalization and medialization of tibial tuberosity for the treatment of potential patellar instability with patella alta. Joints. 2018;6(2):80–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470–2476. [DOI] [PubMed] [Google Scholar]
- 13. Franciozi CE, Ambra LF, Albertoni LJB, et al. Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy. 2019;35(2):566–574. [DOI] [PubMed] [Google Scholar]
- 14. Herbort M, Hoser C, Domnick C, et al. MPFL reconstruction using a quadriceps tendon graft: part 1, biomechanical properties of quadriceps tendon MPFL reconstruction in comparison to the intact MPFL: a human cadaveric study. Knee. 2014;21(6):1169–1174. [DOI] [PubMed] [Google Scholar]
- 15. Hevesi M, Heidenreich MJ, Camp CL, et al. The Recurrent Instability of the Patella (RIP) score: a statistically based model for prediction of long-term recurrence risk after first-time dislocation. Arthroscopy. 2019;35(2):P537–P543. [DOI] [PubMed] [Google Scholar]
- 16. Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ. Complications after tibial tuberosity osteotomy: association with screw size and concomitant distalization. Orthop J Sports Med. 2018;6(10):2325967118803614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lippacher S, Dejour D, Elsharkawi M, et al. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40(4):837–843. [DOI] [PubMed] [Google Scholar]
- 18. Magnussen RA. Patella alta sees you, do you see it? Am J Orthop. 2017;46(5):229–231. [PubMed] [Google Scholar]
- 19. Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2545–2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87(1):36–40. [PubMed] [Google Scholar]
- 21. Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The incidence of complications of tibial tubercle osteotomy: a systematic review. Arthroscopy. 2015;31(9):1819–1825. [DOI] [PubMed] [Google Scholar]
- 22. Prakash J, Seon J-K, Ahn H-W, Cho K-J, Im C-J, Song EK. Factors affecting tibial tuberosity-trochlear groove distance in recurrent patellar dislocation. Clin Orthop Surg. 2018;10(4):420–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Purohit N, Hancock N, Saifuddin A. Surgical management of patellofemoral instability, I: imaging considerations. Skeletal Radiol. 2019;48(6):859–869. [DOI] [PubMed] [Google Scholar]
- 24. Ridley TJ, Baer M, Macalena JA. Revisiting Fulkerson’s original technique for tibial tubercle transfer: easing technical demand and improving versatility. Arthrosc Tech. 2017;6(4):e1211–e1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, et al. Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47(6):1323–1330. [DOI] [PubMed] [Google Scholar]
- 26. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. [DOI] [PubMed] [Google Scholar]
- 27. Schöttle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129(3):305–309. [DOI] [PubMed] [Google Scholar]
- 28. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 29. Yang JS, Fulkerson JP, Obopilwe E, et al. Patellofemoral contact pressures after patellar distalization: a biomechanical study. Arthroscopy. 2017;33(11):2038–2044. [DOI] [PubMed] [Google Scholar]
- 30. Zilber S, Goutallier D. Preoperative planning of tibial tubercle medialisation according to the trochlear groove angle. Orthop Traumatol Surg Res. 2019;105(1):129–131. [DOI] [PubMed] [Google Scholar]


