Abstract
[Purpose] To report on the reduction of a double lumbar spine spondylolisthesis by use of Chiropractic BioPhysics® technique. [Participant and Methods] A 57 year-old male presented with severe chronic low back pains and sciatica. After playing hockey for 50 years, he was unable to continue and was forced to retire. Lumbar radiography showed an L3 retrolisthesis of −5.3 mm and an L4 anterolisthesis of 5.4 mm. Chiropractic BioPhysics technique including mirror image lumbar spine drop-table adjustments, corrective exercises and a unique pelvic extension traction was performed 50 times over 7-months. [Results] A radiograph after 3-months showed full reduction of the L3 retrolisthesis. A radiograph after 7-months showed full reduction of the L4 anterolisthesis. The patient reported full resolution of chronic back pains and was able to return to play hockey; a 1.75 year follow-up showed maintenance of the corrections and the patient remained injury-free while returning to play hockey. [Conclusion] A customized treatment program including Chiropractic BioPhysics lumbar spine traction, corrective exercises and drop-table spine manipulation resolved chronic back pains and fully reduced an L3 and L4 retro- and antero-listhesis, respectively. Further research may substantiate this treatment approach for reducing translational displacements in the lumbar spine. Routine upright radiography is required to diagnose spondylolisthesis.
Key words: Lumbar spine, Spondylolisthesis, Subluxation
INTRODUCTION
Spondylolisthesis is the displacement of a vertebral body relative to the segment below it1). This condition is most commonly caused by spondylolysis, a structural defect in the pars interarticularis causing forward translation of the vertebra (i.e. isthmic spondylolisthesis)2). This forward translation of the vertebra breaks the appearance of a smooth lumbar curve at the level of the ‘slippage’ (George’s line) when visualized on the lateral radiograph and causes instability of the lumbar spine2).
The traditional classification system for grading the severity of the translation of a vertebra is the Meyerding system3). The superior endplate of the inferior vertebra is divided into four equal divisions, the division which the posterior vertebral body margin of the superior vertebra lays within is the grading, i.e. 0–25%=Grade I, 26–50%=Grade II, etc. Although a low-grade spondylolisthesis (Grade I or II) does not always correlate with low back pain (LBP)4), a systematic review and meta-analysis by Raastad et al. determined that spondylolisthesis can definitively be a causative factor for LBP5).
When an adult presents with symptomatic low-grade spondylolisthesis it is usually reported as pain radiating into the legs1). Typically, treatment of spondylolisthesis varies based on presentation. Patients tend to respond very well to conservative treatment for low-grade spondylolisthesis which can include spinal bracing, physiotherapy and chiropractic treatment6,7,8). Despite ‘successful’ treatment outcomes for conservative treatment for spondylolisthesis, this more often relates to the symptoms and not the reduction of the translational vertebral off-set. In the non-surgical management of low-grade spondylolisthesis, there is little evidence of actual reduction of translational offset. Fedorchuk et al. reported on the reduction of a Grade II, 13.3 mm L4 anterolisthesis being reduced to 2.4 mm after 60 treatments utilizing mirror image® spinal exercises, adjustments, and a unique application of lumbar traction over a 45-week duration9). The authors concluded “This case provides the first documented evidence of a non-surgical or chiropractic treatment, specifically Chiropractic BioPhysics®, protocols of lumbar spondylolisthesis where spinal alignment was corrected”.
This purpose of this case is to report on the successful reduction of an L3 retrolisthesis and L4 anterolisthesis in the lumbar spine of an older hockey player who was forced to retire from the sport due to chronic low back pain and sciatica.
PARTICIPANT AND METHODS
A 57 year-old male, avid hockey player, presented to the first two authors spine clinic reporting severe LBP that radiated down both legs as well as chronic neck pains. The patient had sustained various injuries every hockey season for the last 10 years but over the past year, the pain had become so severe he was forced to retire from the sport after having played for 50 years. Comorbidities included high blood pressure, leg cramping, and ringing in the ears. The patient reported being in three previous motor vehicle collisions. Previous treatments included years of massage therapy, medication and physical therapy which at times, provided temporary relief however, long-term did not improve his condition.
Physical examination showed limited flexibility of the lumbar spine in all directions, while extension elicited pain. Muscle testing showed the L3 nerve to be affected on the left and upon palpation there was severe pain and spasms along the paraspinal muscles bilaterally throughout the levels of L1–S2. On the short form-36 quality of life questionnaire (SF-36) the patient scored below normal on all indices; notably, he scored a 0/100 on energy and 35/100 on the pain categories (Table 1).
Table 1. SF-36 quality of life scores.
| Date | Health | Physical | Role- | Role- | Social | Mental | Bodily | Energy/ | Change in |
| perception | functioning | physical | emotional | functioning | health | pain | Fatigue | health | |
| Normal | 72 | 84 | 81 | 81 | 83 | 75 | 75 | 61 | n/a |
| 5-4-15 | 45 | 45 | 0 | 66.7 | 50 | 60 | 35 | 30 | 25 |
| 8-6-15 | 55 | 75 | 0 | 33.3 | 87.5 | 68 | 77.5 | 60 | 50 |
| 12-11-15 | 75 | 95 | 100 | 100 | 87.5 | 84 | 77.5 | 70 | 75 |
| 12-1-16 | 80 | 95 | 100 | 100 | 75 | 88 | 90 | 75 | 100 |
Lumbar radiographs were performed and analyzed using the PostureRay EMR software (PostureCo Inc., Trinity, FL, USA). This program allows for easy digitization of the biomechanical alignment of lumbopelvic parameters using the Harrison posterior tangent method10). Lines are drawn contiguous with the posterior margins of the vertebrae so that adjacent intersegmental vertebral angles and distances as well as a global lordosis alignment (L1–L5) can easily be reported. This method is highly accurate and has a standard error of measurement of about 2° and 2 mm10, 11). The initial lateral lumbar X-ray (Fig. 1) showed a segmental posterior translation (posterolisthesis) of L3 on L4 of −5.3 mm (Grade I spondylolisthesis) and a segmental anterior translation (anterolisthesis) of L4 on L5 of 5.4 mm (Grade I spondylolisthesis).
Fig. 1.
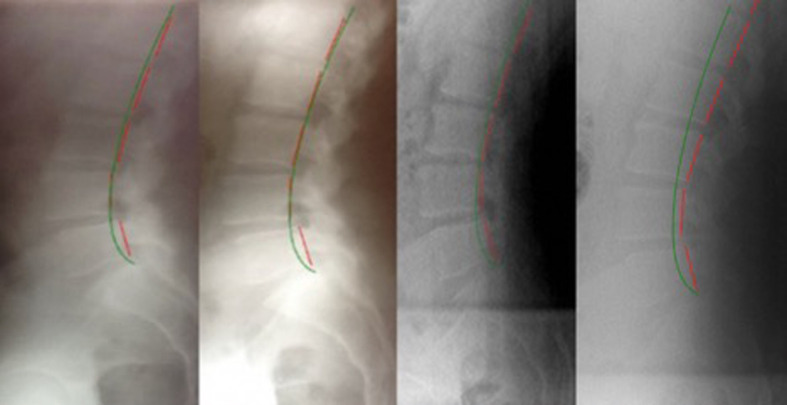
Lateral lumbar views. Left: Initial radiograph showing an L3 posterolisthesis of −5.3 mm and an L4 anterolisthesis of +5.4 mm; Second: 10-week follow-up radiograph showing an L3 posterolisthesis of −1.7 mm and an L4 anterolisthesis of +4.7 mm; Third: 20-week follow-up radiograph showing an L3 posterolisthesis of −1.5 mm and an L4 anterolisthesis of +1.0 mm. Right: 1 year follow-up radiograph showing maintenance of correction. The green line represents a normal lumbar curve, while the red line represents the patient’s posterior vertebral body margins.
The patient underwent treatment including spinal manipulation as well as traction methods based on Chiropractic BioPhysics protocols12,13,14) for an initial 7-month period, totaling 50 treatment sessions. The treatment for each visit consisted of mirror image® corrective adjusting, lumbar spine traction and exercises. A mirror-image adjustment is a specialized chiropractic adjustment in which the patient is placed in the exact opposite position of what their abnormal presenting posture is, all while high-velocity and low-amplitude spinal manipulations are being delivered. The patient was treated approximately two times per week for the initial 7.25-month period with follow up X-rays being taken after the 3-months, and again after another 4.25-months (7.25-months overall). After this the patient remained on a wellness care plan that involved 18 more treatments over a 1 year duration (1.7 year overall treatment). X-rays are also reported for the 1 year post-treatment follow-up.
The patient received mirror image adjustments using a chiropractic drop table to adjust the lumbar spine. This involved the patient to be in a supine position on the drop table keeping the hips in a flexed position by raising the knees to the chest to flatten out the lumbar lordosis. The table was then cocked and dropped five times while the patient remained in this position. The treating doctor’s contact hand, or the hand placed under the patient during the delivery of the drop was on the posterior aspect of the L5 paravertebral area.
Corrective exercises included movements in which the patient actively tilted his pelvis posteriorly by bringing the knees to the chest in order to traction the lordosis by flattening out the lumbar spine. These exercises were performed for seven minutes at a time, three times per week.
Spinal traction was performed with the patient in a supine position, placing a strap across the anterior-superior iliac spine of the pelvis, where it was tightened down to flatten the lumbar spine. A second strap was placed underneath the ischial tuberosities with traction applied with a cephalad tilt, or an extension tilt of the pelvis. The traction sessions were applied for twenty minutes at a time, approximately two times per week throughout the initial ‘corrective care’ course of treatment (first 7.25-months) and approximately 1.5 times per month during ‘maintenance care’ treatment for a subsequent year. The patient gave verbal and written consent for the publication of this case.
RESULTS
An assessment after the first 3-months (29 treatments) showed a 4.6 mm, or total reduction of the L3 retrolisthesis (−1.7 mm vs. −5.3mm), the L4 anterolisthesis was still present (+4.7 mm vs. +5.4 mm) (Fig. 1; Table 2). The L1–5 lordosis increased 5.6° (36.3° vs. 30.7°). Two of eight SF-36 health indices scored normal, including bodily pain (Table 1). The LBP and leg pains were substantially improved. The lumbar range of motion also improved, being only slightly painful upon extension.
Table 2. Spinal parameter values.
| Parameter | Normal | Initial | 1st f/u | 2nd f/u | 1-yr f/u |
| L1–2 Tz (mm) | 0 | −2.4 | −1.7 | −0.8 | −1.3 |
| L2–3 Tz (mm) | 0 | −2.6 | −1.9 | −1.1 | −0.5 |
| L3–4 Tz (mm) | 0 | −5.3* | −1.7 | −1.5 | −2.6 |
| L4–5 Tz (mm) | 0 | +5.4* | +4.7* | +1.0 | +1.6 |
| L5–S1 Tz (mm) | 0 | −1.5 | −1.3 | −1.3 | −1.4 |
| L1–5 ARA | −40° | −30.7° | −36.3° | −37.7° | −37.6° |
| Tz (T12–S1) (mm) | 0 | 6.1 | 5.0 | −4.0 | −17.7 |
| SBA | 40° | 39.3° | 37.4° | 37.4° | 38.2° |
*Spondylolisthesis. ARA: absolute rotation angle from posterior tangents; f/u: follow-up; SBA: sacral base angle; Tz: anterior-posterior translation.
Assessment after 7.25-months (50 total treatments) showed a normalization of the lumbar alignment (Fig. 1; Table 2). The L3 initial retrolisthesis remained reduced at −1.5 mm (vs. −5.3 mm), and the L4 anterolisthesis was now completely reduced (1.0 mm vs. 5.4 mm). All eight SF-36 indices scored within normal limits (Table 1). The LBP and leg pains were now not bothering the patient. After the 7.25-months of treatment, the patient was able to begin playing hockey again, as the activity did not aggravate his low back.
A 1 year follow-up (1.6 years after initial presentation), showed the maintenance of the L3 retrolisthesis reduction (−2.6 mm vs. −5.3 mm), L4 anterolisthesis reduction (1.6 mm vs. 5.4 mm), and the L1–5 lumbar lordosis (−37.6° vs. −30.7°) (Fig. 1; Table 2). All SF-36 scores remained within normal limits (Table 1) and the patient reported to be very well and to have experienced the first injury-free hockey season in 10 years.
DISCUSSION
This case reports on the successful reduction of a double Grade I spondylolisthesis, an L3 retrolisthesis and an L4 anterolisthesis, after performing specific spinal adjusting, corrective exercises and traction methods. There was a complete reduction of translational offset of both vertebrae over a 7.25-month period and 50 treatment sessions. The patient reported the resolution of severe LBP and bilateral sciatic pains and the patient was able to return to play hockey. A follow-up assessment 1 year after the initial reduction (1.6 years total), determined the lumbar spine corrections were maintained, the patient remained well and reported having their first injury-free hockey season in 10 years.
This case is important as it shows that non-surgical, non-invasive manual therapy approaches may be proven to reliably reduce low-grade lumbar spondylolisthesis and represents only the second case reported in the literature showing the reduction of a lumbar spondylolisthesis; the first showing reduction of a double spondylolisthesis. As mentioned, the first case was reported by Fedorchuk et al. who reported the successful reduction of an L4 anterolisthesis from 13.3 mm to 2.4 mm, a 10.9 mm total reduction9).
The 2017 Fedorchuk case9) as well as the current case used a similar type of lumbar spine traction. Spinal traction is unique as it is thought to provide forces that exert a visco-elastic creep onto the spinal soft tissues, particularly the intervertebral disc and longitudinal ligaments15,16,17,18). Thus, traction sustained for 10–20 minutes, over time can change the biomechanical structure of the spine, including the reduction of spondylolisthesis, through repeated sessions much like the literature has shown that increasing the lumbar lordosis is possible by ‘extension traction’ methods15, 16).
Limitations to this case are that multiple procedures were used to treat the patient; thus, technically it is impossible to determine which of the procedures reduced the deformity. It is known, however, that manual spinal manipulation does not change spinal curves19,20,21). Further, in carefully planned randomized controlled trials, it was definitively proven that the specific traction methods caused the structural change in spinal position in multimodal spinal rehabilitation programs for increasing the lordosis in the low back22, 23) and the neck24, 25). Therefore, even though one study on spinal manipulation reported a 34% reduction of spondylolisthesis, this was only an average of a 1.1° reduction in 45 patients; a negligible change in comparison to the error of measurement (<2°)11, 12). This case showed a 3.8° (L3) and a 4.4° (L4) reduction, well beyond the error of measurement.
It must be mentioned that the primary screening method for spondylolisthesis is upright X-ray26, 27). As discussed, the Grading system for categorizing the magnitude of the translational offset is by the Meyerding system3). Although within the medical management of LBP, routine X-rays are not recommended as it does not usually change the course of treatment (e.g. pain, anti-inflammatory, and/or muscle relaxant medications)28, 29), routine X-rays for LBP are recommended for manual therapy providers who specialized in methods that require biomechanical analysis for methods that are radiographically-guided much like spinal surgeons30, 31).
Conflict of interest
Dr. Paul Oakley (PAO) is a paid consultant for CBP NonProfit, Inc.; Dr. Deed Harrison (DEH) teaches chiropractic rehabilitation methods and sells products to physicians for patient care as used in this manuscript.
REFERENCES
- 1.Hu SS, Tribus CB, Diab M, et al. : Spondylolisthesis and spondylolysis. J Bone Joint Surg Am, 2008, 90: 656–671. [PubMed] [Google Scholar]
- 2.Marchiori DM: Clinical imaging with skeletal, chest, and abdominal pattern differentials. St. Louis: Mosby, 1999. pp 581–587. [Google Scholar]
- 3.Meyerding HW: Spondyloptosis. Surg Gynecol Obstet, 1932, 54: 371–377. [Google Scholar]
- 4.Beutler WJ, Fredrickson BE, Murtland A, et al. : The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine, 2003, 28: 1027–1035, discussion 1035. [DOI] [PubMed] [Google Scholar]
- 5.Raastad J, Reiman M, Coeytaux R, et al. : The association between lumbar spine radiographic features and low back pain: a systematic review and meta-analysis. Semin Arthritis Rheum, 2015, 44: 571–585. [DOI] [PubMed] [Google Scholar]
- 6.Pizzutillo PD, Hummer CD, 3rd: Nonoperative treatment for painful adolescent spondylolysis or spondylolisthesis. J Pediatr Orthop, 1989, 9: 538–540. [DOI] [PubMed] [Google Scholar]
- 7.Excoffon SG, Wallace H: Chiropractic and rehabilitative management of a patient with progressive lumbar disk injury, spondylolisthesis, and spondyloptosis. J Manipulative Physiol Ther, 2006, 29: 66–71. [DOI] [PubMed] [Google Scholar]
- 8.Wong LC: Rehabilitation of a patient with a rare multi-level isthmic spondylolisthesis: a case report. J Can Chiropr Assoc, 2004, 48: 142–151. [PMC free article] [PubMed] [Google Scholar]
- 9.Fedorchuk C, Lightstone DF, McRae C, et al. : Correction of grade 2 spondylolisthesis following a non-surgical structural spinal rehabilitation protocol using lumbar traction: a case study and selective review of literature. J Radiol Case Rep, 2017, 11: 13–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison DE, Harrison DD, Cailliet R, et al. : Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine, 2001, 26: E235–E242. [DOI] [PubMed] [Google Scholar]
- 11.Hwang JH, Modi HN, Suh SW, et al. : Reliability of lumbar lordosis measurement in patients with spondylolisthesis: a case-control study comparing the Cobb, centroid, and posterior tangent methods. Spine, 2010, 35: 1691–1700. [DOI] [PubMed] [Google Scholar]
- 12.Harrison DD, Janik TJ, Harrison GR, et al. : Chiropractic biophysics technique: a linear algebra approach to posture in chiropractic. J Manipulative Physiol Ther, 1996, 19: 525–535. [PubMed] [Google Scholar]
- 13.Oakley PA, Harrison DD, Harrison DE, et al. : Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc, 2005, 49: 270–296. [PMC free article] [PubMed] [Google Scholar]
- 14.Harrison DE, Betz JW, Harrison DD, et al. : CBP structural rehabilitation of the lumbar spine. Harrison Chiropractic Biophysics Seminars, 2007.
- 15.Harrison DE, Oakley PA: Non-operative correction of flat back syndrome using lumbar extension traction: a CBP® case series of two. J Phys Ther Sci, 2018, 30: 1131–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oakley PA, Moustafa IM, Harrison DE: Restoration of cervical and lumbar lordosis: CBP® methods overview. In: Spinal deformities in adolescents, adults and older adults. IntechOpen, 2019. [Google Scholar]
- 17.Oliver MJ, Twomey LT: Extension creep in the lumbar spine. Clin Biomech (Bristol, Avon), 1995, 10: 363–368. [DOI] [PubMed] [Google Scholar]
- 18.Hukins DW, Kirby MC, Sikoryn TA, et al. : Comparison of structure, mechanical properties, and functions of lumbar spinal ligaments. Spine, 1990, 15: 787–795. [PubMed] [Google Scholar]
- 19.Plaugher G, Cremata EE, Phillips RB: A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments. J Manipulative Physiol Ther, 1990, 13: 498–506. [PubMed] [Google Scholar]
- 20.Harrison DD, Jackson BL, Troyanovich S, et al. : The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. J Manipulative Physiol Ther, 1994, 17: 454–464. [PubMed] [Google Scholar]
- 21.Harrison DE, Harrison DD, Betz JJ, et al. : Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther, 2003, 26: 139–151. [DOI] [PubMed] [Google Scholar]
- 22.Moustafa IM, Diab AA: Extension traction treatment for patients with discogenic lumbosacral radiculopathy: a randomized controlled trial. Clin Rehabil, 2013, 27: 51–62. [DOI] [PubMed] [Google Scholar]
- 23.Diab AA, Moustafa IM: The efficacy of lumbar extension traction for sagittal alignment in mechanical low back pain: a randomized trial. J Back Musculoskeletal Rehabil, 2013, 26: 213–220. [DOI] [PubMed] [Google Scholar]
- 24.Moustafa IM, Diab AA, Taha S, et al. : Addition of a sagittal cervical posture corrective orthotic device to a multimodal rehabilitation program improves short- and long-term outcomes in patients with discogenic cervical radiculopathy. Arch Phys Med Rehabil, 2016, 97: 2034–2044. [DOI] [PubMed] [Google Scholar]
- 25.Moustafa IM, Diab AA, Harrison DE: The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. Eur J Phys Rehabil Med, 2017, 53: 57–71. [DOI] [PubMed] [Google Scholar]
- 26.Bendo JA, Ong B: Importance of correlating static and dynamic imaging studies in diagnosing degenerative lumbar spondylolisthesis. Am J Orthop, 2001, 30: 247–250. [PubMed] [Google Scholar]
- 27.Segebarth B, Kurd MF, Haug PH, et al. : Routine upright imaging for evaluating degenerative lumbar stenosis: incidence of degenerative spondylolisthesis missed on supine MRI. J Spinal Disord Tech, 2015, 28: 394–397. [DOI] [PubMed] [Google Scholar]
- 28.Oakley PA, Harrison DE: Are restrictive medical radiation imaging campaigns misguided? It seems so: a case example of the American Chiropractic Association’s adoption of “choosing wisely”. Dose Response, 2020, 18: 1559325820919321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oakley PA, Cuttler JM, Harrison DE: Response to letters from Anderson and Kawchuk et al: x-ray imaging is essential for contemporary chiropractic and manual therapy spinal rehabilitation: radiography increases benefits and reduces risks. Dose Response, 2018, 16: 1559325818809584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oakley PA, Ehsani NN, Harrison DE: Repeat radiography in monitoring structural changes in the treatment of spinal disorders in chiropractic and manual medicine practice: evidence and safety. Dose Response, 2019, 17: 1559325819891043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oakley PA, Harrison DE: Radiogenic cancer risks from chiropractic x-rays are zero: 10 reasons to take routine radiographs in clinical practice. Ann Vert Sublux Res, 2018, March 10: 48–56. [Google Scholar]


