Abstract
Background
There is evidence that the COVID-19 pandemic is having adverse effects on mental health. It is vital to understand what is causing this: worries over potential adversities due to the pandemic, or the toll of experiencing adverse events.
Methods
We used panel data from 41 909 UK adults in the COVID-19 Social Study assessed weekly from 1 April 2020 to 12 May 2020 to study the association between adversities and anxiety and depressive symptoms. We studied six categories of adversity including both worries and experiences of: illness with COVID-19, financial difficulty, loss of paid work, difficulties acquiring medication, difficulties accessing food, and threats to personal safety. Anxiety and depression were measured using the 7-item Generalised Anxiety Disorder Assessment and the 9-item Patient Health Questionnaire. We used fixed-effect regression models to account for time-invariant confounders.
Results
Cumulative number of worries and experience of adversities were both related to higher levels of anxiety and depression. A number of worries were associated more with anxiety than depression, but number of experiences were equally related to anxiety and depression. There were clear associations between specific worries and poorer mental health. There was weak evidence that individuals of lower socio-economic position were more negatively affected psychologically by the adverse experiences.
Conclusion
Measures over the first few weeks of lockdown in the UK appear to have been insufficient at reassuring people given that we see clear associations with mental health and cumulative worries. Interventions are required that seek to prevent adverse events (eg, redundancies) and reassure individuals and support adaptive coping strategies.
Keywords: mental health, depression, stress
Introduction
The global pandemic of COVID-19 is leading to increasing experience of adversities, from infection and serious illness due to the virus, to financial shocks such as loss of employment and income, to challenges in accessing food, medication or accommodation, to adverse domestic experiences such as abuse.1 2 These experiences echo those reported during previous epidemics.3 However, their effects are causing even greater concern than in epidemics previously due to the global spread of the virus, the scale of lockdown measures that are proving necessary to contain the spread (which are having major effects on economies), and the long time scale being projected for the pandemic.1 4
In particular, there are concerns that COVID-19 will have substantial and lasting effects on mental health.5 Already, reports are emerging of a parallel epidemic of fear, anxiety and depression.6 But at present, it remains unclear what is triggering these adverse psychological effects: worries over potential adversities due to the virus, or the toll of actually experiencing adverse events. Literature suggests that experiencing adversities such as ill health, financial problems and challenges meeting basic needs is associated with poor psychological outcomes including anxiety, depression, post-traumatic stress and broader distress.7 8 This has been found to apply to situations in epidemics too.9 However, it is not just experiencing adversities that can have such effects; even worries about experiencing adverse effects can negatively impact on mental health. For example, experiencing daily worries is associated with depressive symptoms both in the short term and over several years.10 11 This has been shown for a range of worries, including those relating to health and finances.12 13 In fact, worries and other negative reactions to an event have in some instances been found to be more important in predicting mental health and well-being than experiencing the event itself.14 It is vital to ascertain whether it is worries of adversity or experiences of adversity that are most strongly linked to declines in mental health as each require different types of support or interventions to prevent or mitigate their effects. For example, if worries are most strongly associated with poor mental health, then provision of greater public reassurance or individual interventions such as online cognitive behavioural therapy programmes could be made more available to people. In contrast, if experience of adversity shows greater associations with poor mental health, then interventions that provide more tangible and material support (such as further financial relief measures) may be key.
Additionally, there are worries that adversities will exacerbate existing inequalities within societies by disproportionally affecting individuals of lower socioeconomic position (SEP).1 2 These individuals are more likely to experience adverse events during the pandemic, as well as more likely to have poorer mental health in the first place.3 15 Low SEP individuals may also have fewer material and psychosocial resources available to deal with adversity,16 and studies specifically looking at the effect of adversity on mental health have shown that there is socio-economic variation in the consequences of adversity.17
Therefore, this study used a large, longitudinal dataset of weekly experiences during the early weeks of the lockdown due to COVID-19 in the UK to explore the time-varying longitudinal relationship between (1) worries about adversity and (2) experience of adversity, and both anxiety and depression. Further, it sought to ascertain whether the relationship between adversity and mental health was moderated by SEP.
Methods
Participants
We use data from the COVID-19 Social Study; a large panel study of the psychological and social experiences of over 70 000 adults (aged 18+) in the UK during the COVID-19 pandemic. The study commenced on 21 March 2020 and involves online weekly data collection from participants for the duration of the pandemic in the UK. The study is not random but does contain a well-stratified sample with good representation across all sociodemographic groups (see online supplemental material for further information on recruitment). All participants gave informed consent. Full details of the study, recruitment, retention, protocol and user guide are available at https://github.com/UCL-BSH/CSSUserGuide.
jech-2020-215598supp001.pdf (517.7KB, pdf)
As questions asked about experiences of adversity in the last week, we focused on data from 1 April 2020 (1 week after lockdown commenced) to 12 May 2020. We limited our analysis to participants with two or more waves of data during this period (n=48 723, observations=2 08 057, 71.6% of sample who joined the survey by 12 May). Note, recruitment was ongoing across the study period, so not all participants were able to complete multiple waves. We used complete case data in our analysis. This necessitated excluding participants with complete data in fewer than two waves in order to meet inclusion criteria (n=6814; 14.0% of eligible participants). This provided a final analytical sample of 41 909 participants (178 430 observations).
Measures
Depression
Depression during the past week was measured using the Patient Health Questionnaire (PHQ-9); a standard 9-item instrument for diagnosing depression in primary care, with 4-point responses ranging from ‘not at all’ to ‘nearly every day’ (range 0–27; higher scores indicate more depressive symptoms).18 19
Anxiety
Anxiety during the past week was measured using the Generalised Anxiety Disorder assessment (GAD-7); a well-validated 7-item tool used to screen and diagnose GAD-7 in clinical practice and research, with 4-point responses ranging from ‘not at all’ to ‘nearly every day’ (range 0–21; higher scores indicate more symptoms of anxiety).20
Adversities
We study six categories of adversity, each measured weekly (see table 1). We constructed weekly total adversity worries and total adversity experiences measures by summing the number of adversities present in a given week (range 0–6). We considered worries to be one-off events and counted them only in the weeks they were reported. For adversities that are likely to be continuing (ie, once experienced in 1 week, their effects would likely last into future weeks), we counted them on subsequent waves after they had first occurred. This applied to experiencing suspected/diagnosed COVID-19, loss of paid work, major cut in household income and abuse victimisation.
Table 1.
Questions on adversities
| Type of adversity | Adversity worries | Adversity experiences |
| COVID-19 illness | Worried about catching COVID-19 | Currently have or previously had suspected or diagnosed COVID-19 |
| Financial difficulty | Worried about finances | Experienced a major cut in household income |
| Loss of paid work | Worried about losing your job/unemployment | Lost one’s job or been unable to do paid work |
| Difficulties accessing food | Worried about getting food | Unable to access sufficient food |
| Difficulties acquiring medication | Worried about getting medication | Unable to access required medication |
| Threats to personal safety | Worried about personal safety/security | Experienced being physically harmed or hurt by somebody else or being bullied, controlled, intimidate or psychologically hurt by someone else |
Socioeconomic position
We measured SEP using five variables collected at participant’s first round of data collection: annual household income (<£16 000, £16 000–£30 000, £30 000–£60 000, £60 000–£90 000, £90 000+), highest qualification (GCSE or lower, A levels or vocational training, undergraduate degree, postgraduate degree), employment status (employed, inactive and unemployed), housing tenure (own outright, own with mortgage, rent/live rent free) and household overcrowding (binary: >1 persons per room). From these variables, we constructed a low SEP index measure by counting indications of low SEP (income <£16 000, educational qualifications of GCSE or lower, unemployed, living in rented or rent free accommodation, and living in overcrowded accommodation), collapsing into 0, 1 and 2+ indications of low SEP to attain adequate sample sizes for each category.
Analysis
We used fixed-effects regression, which differs from other regression techniques as it explores within-person variation with individuals serving as their own reference point, comparing themselves over time. So all time-invariant (stable) covariates are accounted for, even if unobserved.21 This approach is advantageous as individual stable characteristics such as socioeconomic status, genetics, personality, history of mental illness and threshold for worries could confound associations between adversities and mental health. As individuals are compared with themselves, such bias cannot affect results. Nevertheless, having experiences and worries varies over time, as does mental health and both can be affected by time-varying confounders.
In model 1, we regressed each mental health measure on the total number of adversity experiences and total number of adversity worries, both (a) separately and (b) jointly, using the fixed effects estimator to account for time-invariant heterogeneity across participants. In model 2, we regressed each measure of mental health on adversity experiences and adversity worries separately for each category of adversity in turn. In model 3, we repeated model 1a including interactions between adversity measures and the low SEP index, in order to estimate differences in associations by SEP. We adjusted for day of week (categorical) and days since lockdown commenced (continuous) in each regression, and we standardised GAD-7 and PHQ-9 scores to aid comparison across the two measures. Other time-constant confounders were automatically adjusted for due to the analytical approach. To account for the non-random nature of the sample, all data were weighted to the proportions of gender, age, ethnicity, education and country of living obtained from the Office for National Statistics.22 All graphs show standardised coefficients (predicted change in standardised Likert scores). Analyses were carried out in Stata V.16.0 (StataCorp) and R V.3.6.3.
Results
Table 2 provides detail on the demographic composition of our sample. Descriptive statistics for our exposures and outcomes are shown in online supplemental table S1. There was within-variation in each of the measures, suggesting fixed effects was a valid approach. Online supplemental table S2 displays descriptive statistics for PHQ-9 and GAD-7 scores by SEP group. Our sample showed clear social gradients in anxiety and depression symptoms. There were small correlations between the (within-person demeaned) adversity worries and experience measures, showing that these are separable phenomena (online supplemental figure S1).
Table 2.
Descriptive statistics
| Variable | Overall mean | Overall SD |
Between SD |
Within SD |
| Outcome | ||||
| PHQ-9 Likert | 6.26 | 5.99 | 5.65 | 1.99 |
| GAD-7 Likert | 4.67 | 5.24 | 4.93 | 1.79 |
| Experiences | ||||
| Adversity experiences | 0.60 | 0.84 | 0.80 | 0.28 |
| Lost work | 0.10 | 0.30 | 0.29 | 0.08 |
| Cut in income | 0.20 | 0.40 | 0.38 | 0.13 |
| Unable to access sufficient food | 0.04 | 0.20 | 0.15 | 0.13 |
| Unable to access required medication | 0.03 | 0.16 | 0.12 | 0.11 |
| Suspected or diagnosed COVID-19 | 0.14 | 0.34 | 0.33 | 0.08 |
| Physically or psychologically harmed | 0.09 | 0.29 | 0.27 | 0.11 |
| Worries | ||||
| Adversity worries | 1.30 | 1.32 | 1.14 | 0.65 |
| Losing job/unemployment | 0.13 | 0.34 | 0.28 | 0.19 |
| Finances | 0.31 | 0.46 | 0.39 | 0.24 |
| Getting food | 0.19 | 0.40 | 0.30 | 0.26 |
| Getting medication | 0.11 | 0.32 | 0.24 | 0.20 |
| Catching COVID-19 | 0.42 | 0.49 | 0.40 | 0.29 |
| Personal safety | 0.13 | 0.34 | 0.25 | 0.22 |
Main study variables.
GAD-7, Generalised Anxiety Disorder Assessment; PHQ-9, Patient Health Questionnaire.
The average number of follow-ups was 4.29. The average time between follow-ups was 7.69 days (SD=1.35). Online supplemental figure S2, tables S3 and S4 show sample demographics according to whether the participant met inclusion criteria and by number of follow-ups. Individuals who completed more waves of data collection have better mental health, experience fewer adversities, are older and are less likely to live in rented or overcrowded accommodation, on average.
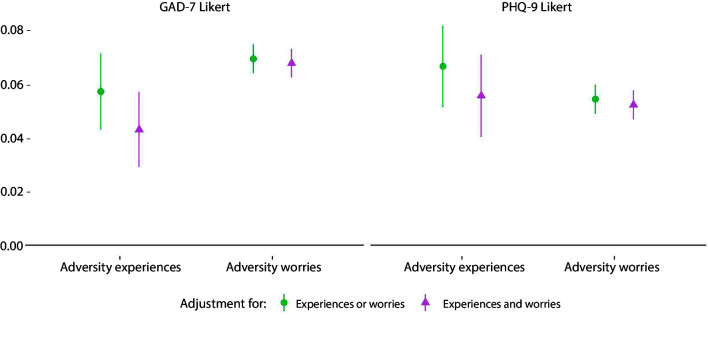
Both the total adversities and total worries indices were associated with increases in GAD-7 and PHQ-9 scores (figure 1). The inclusion of worries in the same model as experiences slightly reduced the effect size of experiences, although the inclusion of experiences in the model had little effect on the effect size of worries. Effect sizes for number of experienced adversities were similar across depression and anxiety measures, but adversity worries were more highly related to anxiety symptoms than depression symptoms.
Figure 1.
Associations between (1) total number of adversity experiences and (2) total number of adversity worries and change over time in GAD-7 and PHQ-9 Likert scores derived from fixed effects models. ‘Experiences or worries’ meant that experiences and worries were entered into separate models. ‘Experiences and worries’ meant that experiences and worries were entered simultaneously into the same model, so were mutually adjusted for one another. Analyses were further adjusted for day of the week and time since lockdown began and automatically account for all time-constant confounders. Graphs show standardised coefficients. GAD-7, Generalised Anxiety Disorder Assessment; PHQ-9, Patient Health Questionnaire.
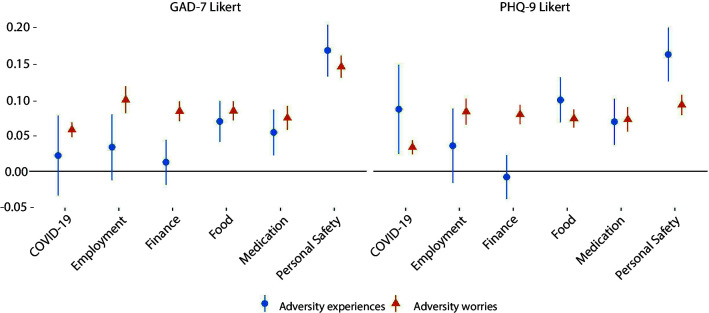
Worries about all types of adversities showed associations with higher levels of GAD-7 and PHQ-9 scores (figure 2). Experiences of adversities relating to accessing food, accessing medication and personal safety were also associated with higher GAD-7 and PHQ-9 scores. However, experience of adversities relating to employment and finance were not associated with changes in mental health, and experience of COVID-19 symptoms was only related to higher depression scores. Experience of harm was more strongly related to mental health than worry about personal safety.
Figure 2.
Associations between (1) experience of specific types of adversities or (2) worries about specific types of adversities and change over time in GAD-7 and PHQ-9 Likert scores derived from fixed effects models. Experiences and worries were entered simultaneously into the same model, so were mutually adjusted for one another. Analyses were further adjusted for day of the week and time since lockdown began and automatically account for all time-constant confounders. Graphs show standardised coefficients. GAD-7, Generalised Anxiety Disorder Assessment; PHQ-9, Patient Health Questionnaire.
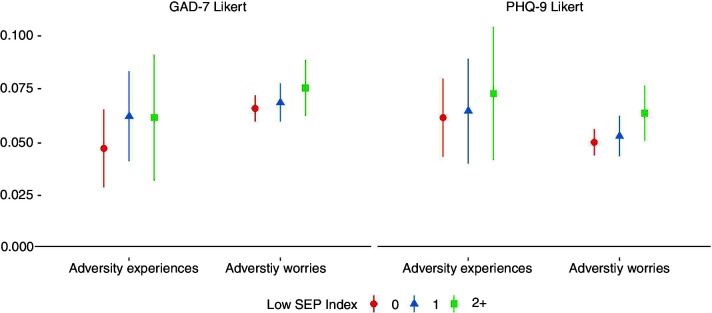
There was some evidence of a social gradient in the association between adversity experiences and adversity worries and mental health outcomes, with stronger associations generally found in more disadvantaged groups (figure 3). However, individual estimates showed substantial variability, especially for experiences.
Figure 3.
Associations between (1) total number of adversity experiences and (2) total number of adversity worries and change over time in GAD-7 and PHQ-9 Likert scores derived from fixed effects models, by SEP index. Experiences and worries were entered simultaneously into the same model, so were mutually adjusted for one another. Analyses were further adjusted for day of the week and time since lockdown began and automatically account for all time-constant confounders. Graphs show standardised coefficients. GAD-7, Generalised Anxiety Disorder Assessment; PHQ-9, Patient Health Questionnaire; SEP, socioeconomic position.
Sensitivity analyses
We carried out several sensitivity analyses to test the robustness of our results. When re-estimating models 1 and 2 using inability to pay bills, rather than major cut in household income, as our measure of experienced financial adversity, the point estimates were more highly related to depression and anxiety symptoms (online supplemental figure S3 and S4). When repeating models 1–3 using only reports of ‘significant stress’ as opposed to minor stress to define the worries variables, effect sizes were predictably larger (online supplemental figures S5 and S6), and there was evidence of a reverse social gradient for the relationship between adversity worries and anxiety symptoms, with largest associations found among the least disadvantaged groups (online supplemental figure S7). To assess whether our findings were just an artefact of our categorisation of SEP, we re-estimated model 3 using quintiles of a continuous measure of SEP derived from a confirmatory factor analysis of the five SEP indicator variables (see online supplemental material methods). There was still some weak indication of a social gradient in the association between adversity experiences and mental health, and some indication of a reverse social gradient in adversity worries and anxiety symptoms, with smaller associations found in more disadvantaged groups (online supplemental figure S8 and table S5).
Discussion
In this study, we explored the relationship between worries and experience of adversities and mental health during the first few weeks of the lockdown due to COVID-19 in the UK. Cumulative number of worries and experience of adversities were both related to higher levels of anxiety and depression. Number of worries were associated more strongly with anxiety than depression, but number of experiences were equally related to anxiety and depression. When considering specific types of adversities, there was greater variability in the relationship between experiences and mental health than worries and mental health. Worries were more strongly related to mental health than experiences for employment and finances, but less for personal safety and catching COVID-19. Individuals of lower SEP were more negatively affected psychologically by adverse experiences, but the relationship between worries, SEP and mental health was unclear.
Our findings show that number of worries were more closely related to anxiety than to depression echoes previous research.23 Indeed, worrying is an integral component of many kinds of anxiety disorders,24 with substantial worrying or ‘rumination’ associated with poor mental health.25 The finding that number of worries about adversities and number of experiences of adversity were equally related to anxiety echoes previous work highlighting how the impact worries about events can be equal to or even greater than experiences of events.14 The results on worries may indicate a bidirectional process between experiencing worries during COVID-19 and becoming more anxious. However, for depression there is less evidence of a bidirectional relationship in previous literature. Instead, reactivity to worries has been found to be a vulnerability factor for depression, but depression has not been found to predict higher negative reactivity.10 26
In relation to experience of adversities, the fact that cumulative experiences was associated with poorer mental health but only certain specific experiences showed the same association suggests that it is the toll of cumulating events that is particularly challenging, perhaps as individual capabilities to manage challenging situations become exhausted.11 However, lack of immediate response to an adversity does not necessarily imply that mental health is not affected, as for certain worries, adverse consequences for mental health may take time to arise. For instance, there is a reported delayed response time in mental health responses to unemployment,27 with rejections during job searches or cuts in income starting to impact on living standards appearing to be bigger triggers than the loss of work itself.28 In line with this, it is notable that we found higher associations for the relationship between inability to pay bills and mental health than loss of income and mental health. Indeed, while loss of income could occur across the wealth spectrum, inability to pay bills is likely concentrated at those with lower levels of household income, so could be regarded as a more significant experience. Financial adversities may also have been anticipated, which may have decreased mental health in the lead up to the event, leading to a floor effect by the time the event occurred.27 But it is also possible that the fear of potential adversity, in particular given the low levels of control experienced in worrying, is psychologically more demanding than the adjustment after an adverse event has occurred.29 The exception to this theory on psychological demand is experiences of adversities relating to personal safety. These were much more strongly linked with mental health than worries about personal safety, and had the strongest link with mental health out of all adversities assessed, which echoes research on the strong negative mental health impact of domestic abuse and violence.30
In relation to catching COVID-19, there was a relationship between worries about catching the virus and anxiety, but there was much greater variability in the relationship between actually catching the virus and mental health. It is possible that there was selection bias in the study, with only individuals who caught and recovered from COVID-19 continuing to take part. But it is also possible that in terms of anxiety, the experience of the virus was less bad than some people had been fearing, leading to relief that individuals had not experienced serious health consequences. Nevertheless, although the CIs were wide, there was still evidence to suggest that catching COVID-19 was associated with increases in depression. This is interesting given evidence suggesting that COVID-19 leads to the release of proinflammatory cytokines associated with depressive disorders,31 and remains to be explored further in future research.
There was some slight evidence of a stronger relationship between adverse experiences and both anxiety and depression among people of low SEP. This echoes previous research suggesting that higher SEP can be a buffer against the effects of adversity, with individuals of lower SEP more vulnerable especially to economic shocks.17 But it is also of note that there was some evidence of a reverse social gradient for adversity worries (especially for more significant worries), with individuals of higher SEP more affected. This could suggest that people who usually face fewer adversities in day to day life, the experience of new worries relating to adversity may have more profound effects.32 Or it could reflect the already higher levels of anxiety and depression found among individuals of lower SEP, suggesting a ceiling effect in reactivity to stressful situations.3 15
This study had a number of strengths including its large, well-stratified sample, which was weighted to population proportions for core sociodemographic characteristics. Further, the study collected data covering the entire period from the start of lockdown in the UK on a weekly basis, providing an extremely rich dataset with longitudinal data. Our statistical approach (fixed effects regression) also allowed the comparison of individuals against themselves (within rather than between-subjects comparisons), so changes over time in the experience of worries and mental health were relative to each individual. As such, our measurement of worries was relative to each individual’s own perspectives, circumstances and coping threshold, allowing us to assess changes in an individual’s perception of their worries over time. Although, it should be noted that there were much wider confidence intervals measurements of association between experiences and mental health compared with worries and mental health, which may suggest that people’s responses to experiences are much more variable, presumably due to differences in coping styles and wider circumstances. However, the study had several limitations. Our sampling was not random, so although we deliberately sampled from groups such as individuals of low SEP and individuals with existing mental illness, it is possible that more extreme experiences were not adequately captured in the study. It is also possible that individuals experiencing particularly extreme situations during the lockdown withdrew from the study. While our statistical method means their survey data is still used, we would lack longitudinal follow-up on their changing experiences. Individuals with poorer mental health and those who experienced greater adversity experiences completed fewer waves of data collection, on average.
We also focused on just six types of adversities, including those relating to health, safety, finances and basic needs. However, many other types of adversity were not included in the study, including those relating to interpersonal relationships, displacement and bereavement. Finally, our study only followed individuals up for a few weeks looking at the immediate associations with mental health. As such, it remains for future studies to assess how experience of adversities during the COVID-19 pandemic relates to long-term mental health consequences.
Overall, the finding that mental health was associated both with experiences and worries about adversities suggests that interventions are required that both seek to prevent adverse events (such as loss of jobs) but also that reassure individuals and support adaptive coping strategies. This appears to be particularly important for managing anxiety, where provision of online cognitive–behavioural training may help support individuals in the management of uncertainty. These results suggest that measures over the first few weeks of lockdown in the UK have been insufficient at reassuring people given we are still seeing clear associations with poor mental health both for cumulative worries and also for a range of specific worries relating to finance, access to essentials, personal safety and COVID-19. Given the challenges in providing mental health support to individuals during the lockdown, these findings highlight the importance of developing online and remote interventions that could provide such support, both as COVID-19 continues and in preparation for future pandemics.
What is already known on this subject.
The pandemic of COVID-19 has led to increased experiences of adversity across the population, and there is evidence that mental health and well-being has declined as a result of COVID-19. There is limited research on whether adversity experiences—and worries about future adversities—have contributed to this decline.
What this study adds.
We find evidence that both adversity experiences and adversity worries have contributed to worsened mental health. Our results suggest that policy measures to reassure citizens and to prevent adversities occurring may have protective effects for mental health.
Acknowledgments
The researchers are grateful for the support of a number of organisations with their recruitment efforts including: the UKRI Mental Health Networks, Find Out Now, UCL BioResource, HealthWise Wales, SEO Works, FieldworkHub and Optimal Workshop.
Footnotes
Contributors: LW, AS and DF conceived and designed the study. LW analysed the data and DF wrote the first draft. All authors provided critical revisions. All authors read and approved the submitted manuscript.
Funding: This Covid-19 Social Study was funded by the Nuffield Foundation (WEL/FR-000022583). The study was also supported by the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by UK Research and Innovation (ES/S002588/1), and by the Wellcome Trust (221400/Z/20/Z). DF was funded by the Wellcome Trust (205407/Z/16/Z). LW is funded by the Economic and Social Research Council through the UCL, Bloomsbury and East London Doctoral Training Partnership (ES/P000592/1). The study was also supported by HealthWise Wales, the Health and Car Research Wales initiative, which is led by Cardiff University in collaboration with SAIL, Swansea University.
Disclaimer: The funders had no final role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All researchers listed as authors are independent from the funders and all final decisions about the research were taken by the investigators and were unrestricted.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. Data used in this study will be made publicly available once the pandemic is over. The code used to run the analysis is available at https://osf.io/6mevr/.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the UCL Research Ethics Committee (12467/005).
References
- 1.Nassif-Pires L, Xavier LdeL, Masterson T, Nikiforos M, Rios-Avila F. Pandemic of inequality Levy Economics Institute; 2020. https://ideas.repec.org/p/lev/levppb/ppb_149.html [Accessed 22 Apr 2020]. [Google Scholar]
- 2.Redefining vulnerability in the era of COVID-19. Lancet 2020;395:1089. 10.1016/S0140-6736(20)30757-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 2020;395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson RM, Heesterbeek H, Klinkenberg D, et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020;395:931–4. 10.1016/S0140-6736(20)30567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020;7:e21. 10.1016/S2215-0366(20)30090-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int Arch Occup Environ Health 2016;89:561–73. 10.1007/s00420-015-1107-1 [DOI] [PubMed] [Google Scholar]
- 8.Pourmotabbed A, Moradi S, Babaei A, et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutrition 2020;23:1778–90. 10.1017/S136898001900435X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawryluck L, Gold WL, Robinson S, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004;10:1206–12. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parrish BP, Cohen LH, Laurenceau J-P. Prospective relationship between negative affective reactivity to daily stress and depressive symptoms. J Soc Clin Psychol 2011;30:270–96. 10.1521/jscp.2011.30.3.270 [DOI] [Google Scholar]
- 11.Charles ST, Piazza JR, Mogle J, et al. The wear and tear of daily stressors on mental health. Psychol Sci 2013;24:733–41. 10.1177/0956797612462222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deimling GT, Bowman KF, Sterns S, et al. Cancer-Related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology 2006;15:306–20. 10.1002/pon.955 [DOI] [PubMed] [Google Scholar]
- 13.Kinnunen P, Laukkanen E, Pölkki P, et al. Are worries, satisfaction with Oneself and outlook in secondary school students associated with mental health in early adulthood? International Journal of Mental Health Promotion 2010;12:4–10. 10.1080/14623730.2010.9721808 [DOI] [Google Scholar]
- 14.Beck AT. Cognitive therapy of depression. Guilford Press, 1979. [Google Scholar]
- 15.Lorant V, Deliège D, Eaton W, et al. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 2003;157:98–112. 10.1093/aje/kwf182 [DOI] [PubMed] [Google Scholar]
- 16.Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol 2011;62:501–30. 10.1146/annurev.psych.031809.130711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valtorta NK, Hanratty B. Socioeconomic variation in the financial consequences of ill health for older people with chronic diseases: a systematic review. Maturitas 2013;74:313–33. 10.1016/j.maturitas.2013.01.015 [DOI] [PubMed] [Google Scholar]
- 18.Löwe B, Kroenke K, Herzog W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (PHQ-9). J Affect Disord 2004;81:61–6. 10.1016/S0165-0327(03)00198-8 [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32:509–15. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 21.Allison PD. Fixed effects regression models. SAGE publications, 2009. [Google Scholar]
- 22.Office for National Statistics . Overview of the UK population: November 2018, 2018. Available: https://www.ons.gov.uk/releases/overviewoftheukpopulationnovember2018 [Accessed 7 May 2020].
- 23.Boehnke K, Schwartz S, Stromberg C, et al. The structure and dynamics of worry: theory, measurement, and cross-national replications. J Pers 1998;66:745–82. 10.1111/1467-6494.00031 [DOI] [PubMed] [Google Scholar]
- 24.Andrews G, Hobbs MJ, Borkovec TD, et al. Generalized worry disorder: a review of DSM-IV generalized anxiety disorder and options for DSM-V. Depress Anxiety 2010;27:134–47. 10.1002/da.20658 [DOI] [PubMed] [Google Scholar]
- 25.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev 2010;30:217–37. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- 26.Wichers M, Geschwind N, Jacobs N, et al. Transition from stress sensitivity to a depressive state: longitudinal twin study. Br J Psychiatry 2009;195:498–503. 10.1192/bjp.bp.108.056853 [DOI] [PubMed] [Google Scholar]
- 27.von Scheve C, Esche F, Schupp J. The emotional Timeline of unemployment: anticipation, reaction, and adaptation. J Happiness Stud 2017;18:1231–54. 10.1007/s10902-016-9773-6 [DOI] [Google Scholar]
- 28.Wanberg CR, Zhu J, Kanfer R, et al. After the pink slip: applying dynamic motivation frameworks to the job search experience. Acad Manage J 2012;55:261–84. 10.5465/amj.2010.0157 [DOI] [Google Scholar]
- 29.Ferrie JE, Shipley MJ, Marmot MG, et al. Health effects of anticipation of job change and non-employment: longitudinal data from the Whitehall II study. BMJ 1995;311:1264–9. 10.1136/bmj.311.7015.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watson CG, Barnett M, Nikunen L, et al. Lifetime prevalences of nine common psychiatric/personality disorders in female domestic abuse survivors. J Nerv Ment Dis 1997;185:645–7. 10.1097/00005053-199710000-00011 [DOI] [PubMed] [Google Scholar]
- 31.Conti P, Ronconi G, Caraffa A, et al. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents 2020;34:327–31. 10.23812/CONTI-E [DOI] [PubMed] [Google Scholar]
- 32.Seery MD, Holman EA, Silver RC. Whatever does not kill us: cumulative lifetime adversity, vulnerability, and resilience. J Pers Soc Psychol 2010;99:1025–41. 10.1037/a0021344 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2020-215598supp001.pdf (517.7KB, pdf)
Data Availability Statement
No data are available. Data used in this study will be made publicly available once the pandemic is over. The code used to run the analysis is available at https://osf.io/6mevr/.