Abstract
Purpose
To compare the specificity and sensitivity of preoperative D-dimer and age-adjusted D-dimer value for predicting the incidence of the DVT preoperatively in total joint arthroplasty (TJA) patients.
Methods
We enrolled 406 patients finally above 50 years old. Everyone had done ultrasonography bedside, and D-dimer concentrations were collected before surgery. The D-dimer and age-adjusted D-dimer cut-off was calculated by multiple logistic regression and receiver operating curve (ROC) analyses.
Results
A total of 39 patients had found asymptomatic deep vein thrombosis (DVT) by ultrasonography. The age (odds ratio [OR] 1.067; p = 0.003) and D-dimer (OR 1.331; p = 0.025) were related to the existence of DVT. For conventional D-dimer and age-adjusted D-dimer value, the area under the curves (AUCs) were 0.685 (0.499–0.696) and 0.795 (0.611–0.881), respectively.
Conclusion
Compared to traditional D-dimer, age-adjusted D-dimer showed better performance in screening DVT, which was useful clinically.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-020-02172-w.
Introduction
As is known to all, the total hip arthroplasty (THA) and total knee arthroplasty (TKA) are the effective methods to treat osteoarthritis, but it also can bring some complications, such as infection, pain, and deep vein thrombosis (DVT), which was the most common complication. The incidence of DVT is about 11.9% in THA and 20.8% in TKA after surgery [1]. DVT can lead to Pulmonary thromboembolism (PTE), which is the most serious complication after arthrosurgery. There are many researches that focus on the incidence of DVT postoperatively; few studies about preoperative DVT were reported [2]. In clinical work, the removal of thrombus preoperatively may need the help of imaging examination such as ultrasound and contrast radiography. However, there are inadequacies in all the above examinations, such as time-consuming, expensive, and labor-consuming, so they are not suitable for large-scale use before operation. If patients have asymptomatic DVT preoperatively, it might cause severe consequence. Thus, a valuable method in detection of DVT or PTE before surgery is necessary.
In clinical work, the prompt diagnosis for thrombosis is the D-dimer test, which can give references to the surgeon [3]. D-dimer is produced by fibrin degradation [4]. The monitoring value of D-dimer is identified according to different methods. The cut-off value of D-dimer is 0.5 μg/ml by latex agglutination turbidimetry (LATEX) in our hospital; however, in the elderly patients, the D-dimer concentrations are higher than the upper limit of normal age [5]. Thus, the value of D-dimer is discounted in the elderly patients [6]. Moreover, the pregnancy, infection, inflammation, and cancer also can lead to high D-dimer value. As a result, the only use of D-dimer to predict DVT is not appropriate.
Some studies showed that the use of age-adjusted D-dimer cut-off in the diagnostic strategy for the specificity and sensitivity of deep vein thrombosis is more valuable over 50 years old [7, 8]. Nybo and Hvas argued that the use of an age-adjusted D-dimer in patients above 50 years of age for ruling out DVT seems as safe as using a standard D-dimer cut-off [9]. Schouten et al. also described that the application of age-adjusted cut-off values to the D-dimer value (0.01 × age [years]) considerably elevates specificity without altering sensitivity in patients aged > 50 years with suspected PTE [10].
Therefore, the use of D-dimer concentrations for predicting deep vein thrombosis is controversial [11]. However, the application of age-adjusted cut-off values to the D-dimer value is relatively rare in orthopedics. So, it is valuable for us to research. The method of this study is to compare the specificity and sensitivity of preoperative D-dimer and age-adjusted D-dimer value for predicting the incidence of the DVT preoperatively. Our aim is to explore the feasibility and effectiveness of this method in the field of joint replacement.
Materials and methods
We enrolled 834 patients, whose age was over 50 years old, who underwent THA or TKA at Affiliate Drum Tower Hospital, Medical School of Nanjing University from September 1, 2015, to April 1, 2017. All patients signed the informed consent. The patients who underwent the pregnancy, infection, and cancer were excluded. In addition, patients were excluded if they had a femoral neck fracture, whose concentration of D-dimer was above normal level. Also, patients with cardiovascular disease and a previous history of thromboembolism were excluded. We removed the patients who had taken anticoagulant or antiplatelet agents previously. In the end, we included 406 patients in our study. All the patients drew blood for collecting the plasma D-dimer level when they were admitted to hospital. The cut-off value of D-dimer was 0.5 μg/ml by latex agglutination turbidimetry (LATEX). We divided patients aged > 50 into 10-year age groups. Renee A Douma made three large cohorts to find the age-adjusted D-dimer value. They plotted the D-dimer cut-off level against age group and performed linear regression analysis to obtain the regression coefficient. They finally proved the multiplication factor for age in the new age-adjusted cut-off value was 0.01. Thus, the age-adjusted D-dimer value was calculated as age (years) × 0.01 μg/mL. The plasma D-dimer level, diagnosis, age, sex, and body mass index (BMI) of the patients were recorded preoperatively. All the patients did not take anticoagulant or antiplatelet agents. The surgeries were done by four skilled orthopedic surgeons. The patients accepted the same program of rehabilitation and postoperative management. We observed vein thrombosis 1 day preoperatively. The skilled radiologists performed thrombosis examinations for all patients. The double lower limbs were observed with bedside ultrasound machine with two mode (B-mode and color Doppler ultrasound examination) for the common femoral, popliteal, superficial, and calf veins bilaterally. DVT was diagnosed if (1) the vein could not be compressed and (2) there were abnormal vascular signals in Doppler color ultrasound. Plasma D-dimer normal value was defined as 0.5 μg/ml. We wanted to analyze the age-adjusted D-dimer cut-off to predict the DVT event. At the same time, we also analyzed the risk factors for preoperative deep venous thrombosis. We predicted that the age-adjusted D-dimer was a more valuable index for monitoring the DVT before the TKA and THA.
All statistical analyses were from SPSS (version 25; SPSS Inc., Chicago, IL, USA). The qualitative data such as the number of females or males was analyzed by Fisher’s exact test. The quantitative data such as body height, body weight, age, body mass index, and D-dimer value was analyzed by unpaired Student’s t test. Multiple logistic regression analysis was used to discover the following risk factors related to the presence of DVT: body height, body weight, body mass index (BMI), age, sex, and D-dimer value. Receiver operating characteristic (ROC) curves were produced for age-adjusted D-dimer value and conventional D-dimer value. Also, the area under the curve (AUC) was calculated by ROC curves. In addition, we used the Youden index [12] to determine the cut-off value. We considered p < 0.05 to be statistically significant.
Results
In the end, we included 406 patients. There were 118 males and 288 females. The average BMI of all patients was 25.3 ± 3.9 kg/m2. The mean age was 65.4 ± 8.4 years old. The patients’ detailed preoperative basic data and related blood tests are shown in Table 1.
Table 1.
Patients’ characteristics
| Total patients | Patients with DVT | Patients without DVT | p value | |
|---|---|---|---|---|
| Patient (n) | 406 | 39 | 367 | - |
| Sex (male/female) | 118/288 | 9/30 | 109/258 | 0.386 |
| Age (years) | 65.4 ± 8.4 | 69.8 ± 6.9 | 65.0 ± 8.5 | < 0.001 |
| Body weight (kg) | 66.0 ± 10.8 | 67.5 ± 11.6 | 65.7 ± 10.7 | 0.316 |
| Body height (cm) | 161.4 ± 7.0 | 160.5 ± 6.3 | 161.5 ± 7.0 | 0.307 |
| BMI (kg/m2) | 25.3 ± 3.9 | 27.2 ± 3.2 | 25.0 ± 3.9 | 0.201 |
| Preoperative D-dimer (μg/ml) | 0.45(0.25,0.84) | 0.91(0.61,1.12) | 0.66(0.32,0.98) | 0.045 |
| APTT (s) | 28.1 ± 3.8 | 28.1 ± 4.6 | 28.1 ± 3.7 | 0.968 |
| PT (s) | 12.0 ± 0.9 | 12.0 ± 0.8 | 12.0 ± 0.9 | 0.865 |
| INR | 1.04 ± 0.08 | 1.04 ± 0.07 | 1.04 ± 0.08 | 0.927 |
| Platelet count (109/L) | 206.9 ± 61.7 | 194.8 ± 55.8 | 208.2 ± 62.2 | 0.193 |
| Hb (g/L) | 128.7 ± 18.4 | 126.1 ± 12.0 | 129.0 ± 18.9 | 0.091 |
DVT deep vein thrombosis, BMI body mass index, APTT activated partial thromboplastin time, PT prothrombin time, INR international normalized ratio, Hb hemoglobin
We divided patients aged > 50 into 10-year age groups. We found that the incidence of thrombosis in the group older than 80 years old was higher than that in the other groups, and the difference was statistically significant. In addition, we compared conventional D-dimer and age-adjusted D-dimer cut-off by age group; more patients below cutoff values could be found in all age groups using age-adjusted D-dimer cut-off values. The specific information is shown in Table 2.
Table 2.
Comparison of different cut-off values stratified by age group
| Age range (years) | |||||
|---|---|---|---|---|---|
| Total patients | 50–59 | 60–69 | 70–79 | > 80 | |
| No (%) of patients | 406 | 103 (25.4) | 182 (44.8) | 99 (24.4) | 22 (5.4) |
| Median age (years) | 63.3 | 54.7 | 64.9 | 73.5 | 83.3 |
| No (%) of patients with DVT | 39 | 3 (2.9) | 16 (8.8) | 16 (16.2) | 4 (18.2) |
| Conventional cut-off value | |||||
| No (%) of patients below cut-off value | 226 (55.7) | 73 (70.9) | 99 (54.4) | 46 (46.5) | 8 (36.4) |
| Age-adjusted cut-off value | |||||
| No (%) of patients below cut-off value | 269 | 78 (75.7) | 118 (64.8) | 6 0(60.6) | 12 (54.5) |
A total of 39 patients had found deep vein thrombosis of the lower extremities, all of which were asymptomatic. The incidence of thrombosis was 9.6%. Two of them were iliac vein thrombosis, and the rest were intramuscular venous thrombosis. The mean age of patients with thrombosis was 69.8 ± 6.9 years, and the mean age of patients without thrombosis was 65.0 ± 8.5 years, with a statistically significant difference (p < 0.001). For preoperative D-dimer levels, patients with thrombosis had an average of 0.91 (0.61, 1.12) mg/mL, compared with 0.66 (0.32, 0.98) mg/mL for patients without thrombosis, and there was a statistically significant difference (p = 0.045).
By multivariate logistic regression analysis, when age, gender, BMI, body weight, and preoperative D-dimer levels were independent variables, we found that only age and D-dimer levels were associated with the development of deep vein thrombosis (Table 3).
Table 3.
Multiple logistic regression analysis for preoperative deep vein thrombosis
| OR | 95% CI | p value | |
|---|---|---|---|
| Age (year) | 1.067 | 1.023–1.113 | 0.003 |
| Sex (female) | 0.615 | 0.208–1.814 | 0.378 |
| Body height (cm) | 0.977 | 0.910–1.049 | 0.52 |
| Body weight (kg) | 1.022 | 0.988–1.057 | 0.209 |
| D-dimer (μg/ml) | 1.331 | 1.032–1.716 | 0.027 |
CI confidence interval, OR odds ratio
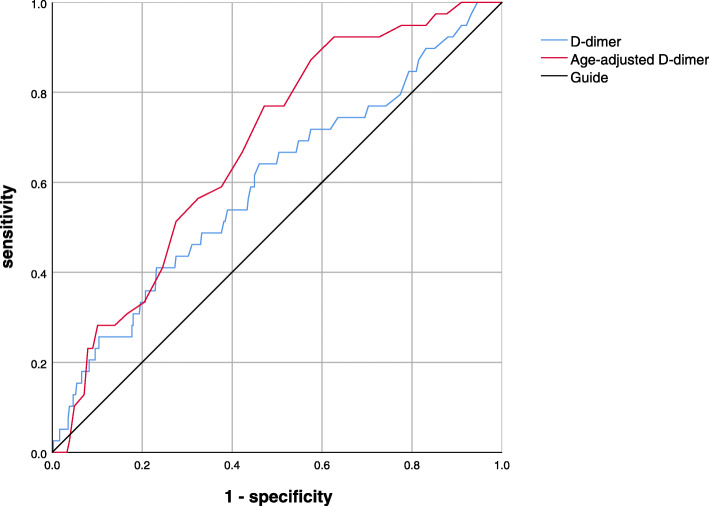
With regard to preoperative D-dimer, a total of 180 patients had a D-dimer concentration greater than 0.5 μg/mL, of which only 18 had thrombosis. With the use of age-adjusted D-dimer, there were only 33 patients’ D-dimer concentration above the age-adjusted D-dimer reference value. In addition, we plotted the ROC curve for the age-adjusted D-dimer and the traditional D-dimer (Fig. 1). The area under the curve was 0.795 and 0.685, respectively (Table 4). For DVT observations, the traditional D-dimer had a cut-off value of 0.845 with a sensitivity of 41% and a specificity of 0.658 (Table 4). The cut-off value of age-adjusted D-dimer cut-off value was 0.655, which caused a sensitivity of 0.769 and a specificity of 0.768 (Table 4).
Fig. 1.
The ROC curve for the age-adjusted D-dimer and the traditional D-dimer
Table 4.
AUC and cut-off
| Cut-off value | Sensitivity | Specificity | AUC | 95% CI | p value | |
|---|---|---|---|---|---|---|
| Age-adjusted D-dimer | 0.655 | 0.769 | 0.768 | 0.795 | 0.611–0.881 | < 0.001 |
| D-dimer | 0.845 | 0.41 | 0.658 | 0.685 | 0.499–0.696 | 0.045 |
AUC area under the curve, CI confidence interval
Discussion
Patients with joint replacement were generally older. If the traditional D-dimer value was used as a preoperative diagnosis method, the false positive patient would be greatly increased [5].
We used both age-adjusted D-dimer and traditional D-dimer values to detect the effectiveness of deep vein thrombosis. The area under the ROC curve was 0.795 and 0.685, respectively, and the age-adjusted D-dimer had a better predictive value in predicting deep vein thrombosis. In addition, we found that the sensitivity of the age-adjusted D-dimer cut-off value (76.8%) was significantly improved compared to the traditional method (41%), while the specificity, age-adjusted D-dimer cut-off value (76.9%) was also slightly better than the traditional D-dimer (65.8%).
The basic D-dimer value increased with age. Harper et al. found that D-dimer concentration increased with age reducing the clinical value of the D-dimer assay in the elderly [5].
Through the age-stratification study, we found that the elderly had higher incidence of thrombosis, which is consistent with the conclusion of our risk factor analysis, and by the age-adjusted D-dimer cut-off value in all age groups, it can be found that more samples are lower than the cut-off value, which improved the sensitivity of the model.
In our study, the age-adjusted D-dimer value was defined as age × 0.01 (μg/mL), which was considered safe. Nybo and Hvas had found that the age-adjusted D-dimer cut-off was safe to recommend the use of an age-adjusted D-dimer in a DVT setting as well as for PE from a systematic review [9]. In this study, we also made multivariate logistic regression analysis to find that age is the risk factor of DVT.
In previous reports, Imai et al. demonstrated that age and D-dimer index can be useful in screening patients for DVTs before THA [13]. The conclusion was similar to us. Moreover, age-adjusted D-dimer value was calculated as patients’ age times 0.01(μg/mL) by Schouten et al. [10]. They drew conclusions that age-adjusted D-dimer value can increase specificity, whereas sensitivity was not. The sensitivity was 97%, but the specificity was below 60%. The results did not coincide with our research. In addition, some studies focused on the performance of age-adjusted D-dimer cut-off values for reducing the use of ultrasounds [3, 14, 15]. Broen et al. inclined the view that age-adjusted D-dimer cut-off values can lead to less duplex ultrasounds performed to find patients that suffer from DVT [16].
In our study, the age-adjusted D-dimer value cut-off increased sensitivity, which was important to find patients with DVT. DVT was the most critical complication. Once we did not observe the asymptomatic DVT patients, it might cause serious consequences, such as pulmonary embolism (PE). Thus, the age-adjusted D-dimer could help us find more asymptomatic DVT patients. Actually, that was what we cared about more.
As far as we know, it was the first study to focus on the performance of age-adjusted D-dimer cut-off values for the screening of deep vein thrombosis in both TKA and THA. We gave the lower extremity venous color ultrasound bedside to all patients admitted to the hospital. Thus, we had enough samples for observation.
However, there were several limitations in our study. First, we did not use Wills score to assess the sensitivity and specificity of age-adjusted D-dimer cut-off value. Wills score could help us predict DVT better [17]. Second, our hospital used latex agglutination turbidimetry (LATEX) to measure the concentrations of D-dimer. Compared to enzyme-linked fluorescent assays (ELISA), LATEX may lead to lower sensitivity and specificity in our study. Finally, we did not group patients to several levels by age, which may get a better result in this study.
In conclusion, compared to traditional D-dimer, age-adjusted D-dimer showed better performance in screening DVT, which was useful clinically. Meanwhile, more clinical observations were needed to verify our ideas.
Supplementary Information
Additional file 1. Supplementary Material.
Acknowledgements
This work was supported by Key Program of NSFC (81730067), Jiangsu Provincial Key Medical Center Foundation, Jiangsu Provincial Medical Outstanding Talent Foundation, Jiangsu Provincial Medical Youth Talent Foundation, Jiangsu Provincial Key Medical Talent Foundation, National Natural Science Foundation of China (81972124), and Basic Research Program of Jiangsu Province (20170123). We thank the patients and their families who donated their blood samples for this study.
Abbreviations
- DVT
Deep vein thrombosis
- TKA
The knee arthroplasty
- THA
The hip arthroplasty
- TJA
The joint arthroplasty
- PTE
Pulmonary thromboembolism
- BMI
Body mass index
- ROC
Receiver operating characteristic
- AUC
Area under the curve
- APTT
Activated partial thromboplastin time
- PT
Prothrombin time
- INR
International normalized ratio
- Hb
Hemoglobin
- CI
Confidence interval
- OR
Odds ratio
- PE
Pulmonary embolism
- ELISA
Enzyme-linked fluorescent assays
- LATEX
Latex agglutination turbidimetry
Authors’ contributions
Qing Jiang contributed substantially to the conception and design of the study. Jian Xiang Wu, Jiang Hui Qing, Yao Yao, and Dong Yang Chen collected and analyzed the data. Jian Xiang Wu wrote the manuscript with support from Yao Yao. All authors read and approved the final manuscript.
Funding
This work was supported by Key Program of NSFC (81730067), Jiangsu Provincial Key Medical Center Foundation, Jiangsu Provincial Medical Outstanding Talent Foundation, Jiangsu Provincial Medical Youth Talent Foundation, Jiangsu Provincial Key Medical Talent Foundation, National Natural Science Foundation of China (81972124), and Basic Research Program of Jiangsu Province (20170123).
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Ethics approval and consent to participate
This study was approved by the institutional review board (IRB) of Nanjing Drum Tower Hospital (No. 2012029).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yamaguchi T, et al. Incidence and time course of asymptomatic deep vein thrombosis with fondaparinux in patients undergoing total joint arthroplasty. Thromb Res. 2010;126(4):e323–e326. doi: 10.1016/j.thromres.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 2.Dai X, et al. Associations of serum lipids and deep venous thrombosis risk after total knee arthroplasty in patients with primary knee osteoarthritis. Int J Low Extrem Wounds. 2019:1534734619868123. [DOI] [PubMed]
- 3.Sartori M, et al. D-dimer for the diagnosis of upper extremity deep and superficial venous thrombosis. Thromb Res. 2015;135(4):673–678. doi: 10.1016/j.thromres.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Gimenez N, et al. Rapid D-dimer test combined a clinical model for deep vein thrombosis. Validation with ultrasonography and clinical follow-up in 383 patients. Thromb Haemost. 2004;91(6):1237–1246. doi: 10.1160/TH03-02-0080. [DOI] [PubMed] [Google Scholar]
- 5.Harper PL, et al. D-dimer concentration increases with age reducing the clinical value of the D-dimer assay in the elderly. Intern Med J. 2007;37(9):607–613. doi: 10.1111/j.1445-5994.2007.01388.x. [DOI] [PubMed] [Google Scholar]
- 6.Cini M, et al. D-dimer use for deep venous thrombosis exclusion in elderly patients: a comparative analysis of three different approaches to establish cut-off values for an assay with results expressed in D-dimer units. Int J Lab Hematol. 2014;36(5):541–547. doi: 10.1111/ijlh.12184. [DOI] [PubMed] [Google Scholar]
- 7.Farm M, et al. Age-adjusted D-dimer cut-off leads to more efficient diagnosis of venous thromboembolism in the emergency department: a comparison of four assays. J Thromb Haemost. 2018;16(5):866–875. doi: 10.1111/jth.13994. [DOI] [PubMed] [Google Scholar]
- 8.Li J, et al. The diagnostic efficacy of age-adjusted D-dimer cutoff value and pretest probability scores for deep venous thrombosis. Clin Appl Thromb Hemost. 2019;25:1076029619826317. doi: 10.1177/1076029619826317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nybo M, Hvas AM. Age-adjusted D-dimer cut-off in the diagnostic strategy for deep vein thrombosis: a systematic review. Scand J Clin Lab Invest. 2017;77(8):568–573. doi: 10.1080/00365513.2017.1390783. [DOI] [PubMed] [Google Scholar]
- 10.Schouten HJ, et al. Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta-analysis. BMJ. 2013;346:f2492. doi: 10.1136/bmj.f2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haenssle HA, et al. Limited diagnostic value of Wells-score and D-dimer testing in hospitalized dermatologic patients with symptoms of deep vein thrombosis. Eur J Dermatol. 2013;23(6):830–6. doi: 10.1684/ejd.2013.2188. [DOI] [PubMed] [Google Scholar]
- 12.Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J. 2005;474(4):458–72. [DOI] [PubMed]
- 13.Imai N, et al. Usefulness of a novel method for the screening of deep vein thrombosis by using a combined D-dimer- and age-based index before total hip arthroplasty. PLoS One. 2017;12(2):e0172849. doi: 10.1371/journal.pone.0172849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riva N, et al. Age-adjusted D-dimer to rule out deep vein thrombosis: findings from the PALLADIO algorithm. J Thromb Haemost. 2018;16(2):271–278. doi: 10.1111/jth.13905. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JH, et al. Age-related diagnostic value of D-dimer testing and the role of inflammation in patients with suspected deep vein thrombosis. Sci Rep. 2017;7(1):4591. doi: 10.1038/s41598-017-04843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broen K, Scholtes B, Vossen R. Predicting the need for further thrombosis diagnostics in suspected DVT is increased by using age adjusted D-dimer values. Thromb Res. 2016;145:107–108. doi: 10.1016/j.thromres.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Sartori M, et al. The Wells rule and D-dimer for the diagnosis of isolated distal deep vein thrombosis. J Thromb Haemost. 2012;10(11):2264–2269. doi: 10.1111/j.1538-7836.2012.04895.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Material.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.