1 |. INTRODUCTION
On 26 March 2020, the South African government imposed a national lockdown that prohibited citizens from leaving a strict quarantine except for food, medicine, and essential work. President Cyril Ramaphosa also banned in-country travel and the sale of alcohol and cigarettes. South Africa was praised by the World Health Organization for its swift and assertive efforts to slow the transmission of the 2019 coronavirus disease (COVID-19; WHO, 2020). Yet others, including the United Nations, criticized the government for its harsh sanctions against non-adherent communities. Police brutality, militarization, and demolition of informal settlements brutalized households across the country, especially in already marginalized communities that lack adequate resources to properly adhere to quarantine laws. Amidst ongoing conditions of racialized inequality, South Africa’s harsh administration of its national lockdown has introduced serious threats to public mental health in a society where one in three individuals develop a psychiatric disorder during their life (Herman et al., 2009; Kim et al., 2020; Reddy et al., 2020).
Data from past coronavirus epidemics (eg, SARS, MERS) poignantly illustrate the psychosocial impacts of quarantine and foreshadow the possible psychological consequences of South Africa’s lockdown. Numerous aspects of life under quarantine, including emotional distress, social isolation, and for some, extreme threats to survival, may substantially increase psychiatric risk (Brooks et al., 2020; Jung & Jun, 2020). Emerging epidemiological data on COVID-19 worldwide corroborate these findings and report greater psychiatric morbidity and barriers to accessing mental healthcare (Brooks et al., 2020; Jung & Jun, 2020). Additionally, early evidence on hospitalized cases of COVID-19 reports novel psychopathological presentations among COVID-19 patients, including anxiety, psychosis, and mood disorders (Subramaney et al., 2019). In South Africa, pre-existing societal conditions including rampant poverty, unemployment, and infectious and non-communicable disease burden foregrounded by the ongoing legacies of the apartheid regime and its racial capitalist logics, place many individuals at elevated risk for COVID-19 (StatsSA, 2019).
In this commentary, I describe the potential mental health consequences of the ongoing COVID-19 pandemic in Soweto, South Africa and offer potential strategies for promoting mental health in research and community settings during the pandemic. I provide ethnographic accounts of COVID-19 in Soweto, a major township of Johannesburg, through the lens of my fieldwork on trauma and mental health and discuss new steps put in place to safeguard mental health of research staff, study participants, and their communities. As human biologists frequently work in settings with considerable psychological morbidity and limited healthcare access, I offer these reflections not as a prescriptive model for researchers but to create a space to share effective strategies, discuss problems, and initiate a broader dialogue on this underappreciated aspect of fieldwork. As human biologists and biological anthropologists, we are well aware of the biological and health consequences of stress, infectious disease, social inequality, and other adversities precipitated by ongoing structural violence and now the compounding effects of the COVID-19 pandemic, and we must not be complicit in perpetuating these conditions. Given this knowledge, access to resources, and collaboration with research communities, we face an ethical imperative to promote and safeguard the mental health of the societies with which we work.
2 |. ETHNOGRAPHIC PERSPECTIVES OF COVID-19 FROM URBAN SOUTH AFRICA
In the days leading up to South Africa’s national lockdown, my ongoing study on trauma and mental health in Soweto was well on its way. My study team and I had just completed our 200th participant interview and we were filled with joy and accomplishment, even though we knew that we still had thousands of salivary cortisol samples that we needed to organize. Discussions of the elusive coronavirus disease were only made in jest, since the total number of active cases of COVID-19 in the country was quite low relative to those in other countries in Europe, Asia, and North America. And given the demographic distribution of COVID-19 infections at the time and existing public perceptions—that only rich, white travelers from Europe living in the bourgeois northern suburbs of Johannesburg were susceptible—many of my colleagues at my research site in Soweto, nearly all black South Africans living in southwest of the city, were unbothered. I share a series of two brief but telling encounters I had with my coworkers to illustrate their sentiments, taken from my field notes.
2.1 |. 20 MARCH 2020
I walk into a friend’s house after hearing news that the first bout of COVID-19 cases hit Gauteng, the province in which Soweto is located. Fully expecting to be met with anxiety and fear from my colleagues, many of whom reside in Soweto, a dense, urban township that is a potential hotbed for community transmission, I prepared myself to have several difficult conversations and help contain peoples’ fears. I enter room, where two of my friends are chatting, just like any other, pandemic-free day. After some conversation about our weekends and family, I ask:
A: So what do you guys think about this coronavirus? How are you feeling about it?
N: (in a soft, calm voice) We are not afraid.
T: Black people will not get it. It will not affect us.
I’m overwhelmed with disbelief. Trying hard to contain my shock, I walk to the room across the hall and see that one of their siblings is dressed in her Sunday best—a black and grey tweed vest over a smooth blouse with jewels and a freshly-ironed skirt over dark stockings. “Why are you dressed so nicely to watch TV?” I asked jokingly. She responded, “No, I am going somewhere after work. We have church service.” My eyes respond for me. They clearly expressed fear and disbelief as large social gatherings had been banned a few days prior. “No Andy, ay, this disease, it’s only for white people. The blood of Jesus will save us!”
During the very early days of COVID-19 in late March, many rejected the risk and reality of the novel coronavirus in Soweto. COVID-19 appeared to be “only a white people’s virus” that did not affect the overwhelmingly black South African township. Several explanations for the origin, etiology, purpose of the disease accompanied these perspectives—that COVID-19 was a tool for bioterrorism created by China, “a conspiracy theory to bring back population regulation from apartheid,” and that the virus spread due to its invisible nature and pandemic potential. Given the wide variation in perceptions of the new disease, we worried about the well-being of our participants and their families as we knew that the unforgiving conditions of the strict stay-at-home order could possibly exacerbate already difficult home situations. Nearly every week since the beginning of our study in January 2020, our team attended to some form of acute psychological distress, relapse, or suicidality among our participants.
The South African public only had a brief period of time to integrate the new expectations and social realities of work and life during a pandemic since the government did not announce clear public health guidelines, like social distancing or voluntary quarantine, until shortly before the announcement of the national lockdown on 23 March, three days before the lockdown. We stopped all in-person data collection on 13 March. To prepare for our transition to remote work, we cancelled upcoming in-person interviews, distributed study equipment (eg, tablets, laptops) and duties (eg, data entry and cleaning, telephonic interviews for surveys and obtaining missing data, general administration, etc.), reviewed safety protocols for COVID-19 prevention, and scheduled frequent group calls to check in and maintain social contact.
Immediately after the lockdown commenced, we began noting an uptick in distress and fear over the virus, possibly due to the new, drastic reality of forced quarantine. Early data from telephonic surveys in Soweto during the first six weeks of the lockdown showed that nearly half of participants expressed fear over the possibility of infection and death: “People in the community are scared, especially the older people, because we see the number of cases going up every day. This virus kills.” Another person said, “People in the community are worried. When we see the number of cases on TV, it’s scary. They said that people like me who have chronic diseases are in trouble.” Other common concerns included anxiety, fear, and excessive rumination due to unemployment, health of their loved ones, greater susceptibility due to comorbidities, lack of knowledge of COVID-19, and the invisible nature of the virus. By mid-April, COVID-19 began to emerge in Soweto, but quickly. Painful accounts of distress, financial insecurity, and fear were palpable through our calls and occurred much more frequently. I first noted the effects of vicarious trauma wear my research staff at this time.
2.2 |. 14 April 2020
A: How are people coping with the lockdown?
E: The reality of corona has hit homes… (spoken softly).
O: People are depressed, worried, may not get paid, jobs are not contacting them… (pause) It’s sad.
W: …Some people are sad about not being able to go out, window shopping, see other people. No one is coping, especially people who are alone and people who don’t have family. It hurts me to see.
COVID-19 emerged South Africa at a time of high prevalence of mental illness and low healthcare access: over a quarter of all cases are considered severe (Herman et al., 2009), yet only 27% of patients with severe mental illnesses receiving treatment and 16% of citizens enrolled in health insurance (Docrat, Besada, Cleary, Daviaud, & Lund, 2019). Amidst these conditions, rates of new COVID-19 cases continue to rise in South Africa—epidemiological models estimate the pandemic will peak between July and September 2020 (SACMC, 2020). As the total prevalence and rate of COVID-19 infections approaches an all-time high, a growing psychological burden due to socioeconomic, medical, and political adversities is expected. Human biologists must be adequately prepared to safeguard the health and well-being of the communities in and with which they work. I share the following strategies implemented in my study to encourage greater practice of mental health promotion and safety in biological anthropology field settings.
3 |. STRATEGIES FOR PROMOTING MENTAL HEALTH IN COMMUNITY AND RESEARCH SETTINGS
3.1 |. Assessing the psychiatric epidemiology of COVID-19—ethically and judiciously
Motivated by our qualitative research and further ethnographic work, we quickly obtained a research ethics amendment and began refocused our study to explore the perceptions, experiences, and social dynamics of COVID-19 among families in Soweto and assess the mental health impacts of the national lockdown. The current study collaborates with an existing project to reach over a thousand adults living in Soweto with an eye towards understanding key risk and protective factors as well as strategies to mitigate mental illness risk and enrich psychological well-being in the coming months. Our recent findings show greater perceived risk of COVID-19 infection predicts greater depression risk, particularly among adults with histories of childhood trauma (Figures 1 and 2; Kim et al., 2020). Over 70% of individuals, however, reported that the pandemic does not impact their mental health, a discrepancy which may lead individuals to disregard their psychological needs (Kim et al., 2020). We plan to work closely in conjunction with local mental health NGOs, university partners, and public health institutions to disseminate these findings. Providing accurate data on the course and impacts of the pandemic, particularly among stigmatized conditions like mental illnesses, can help the planning and targets of public health initiatives.
FIGURE 1.
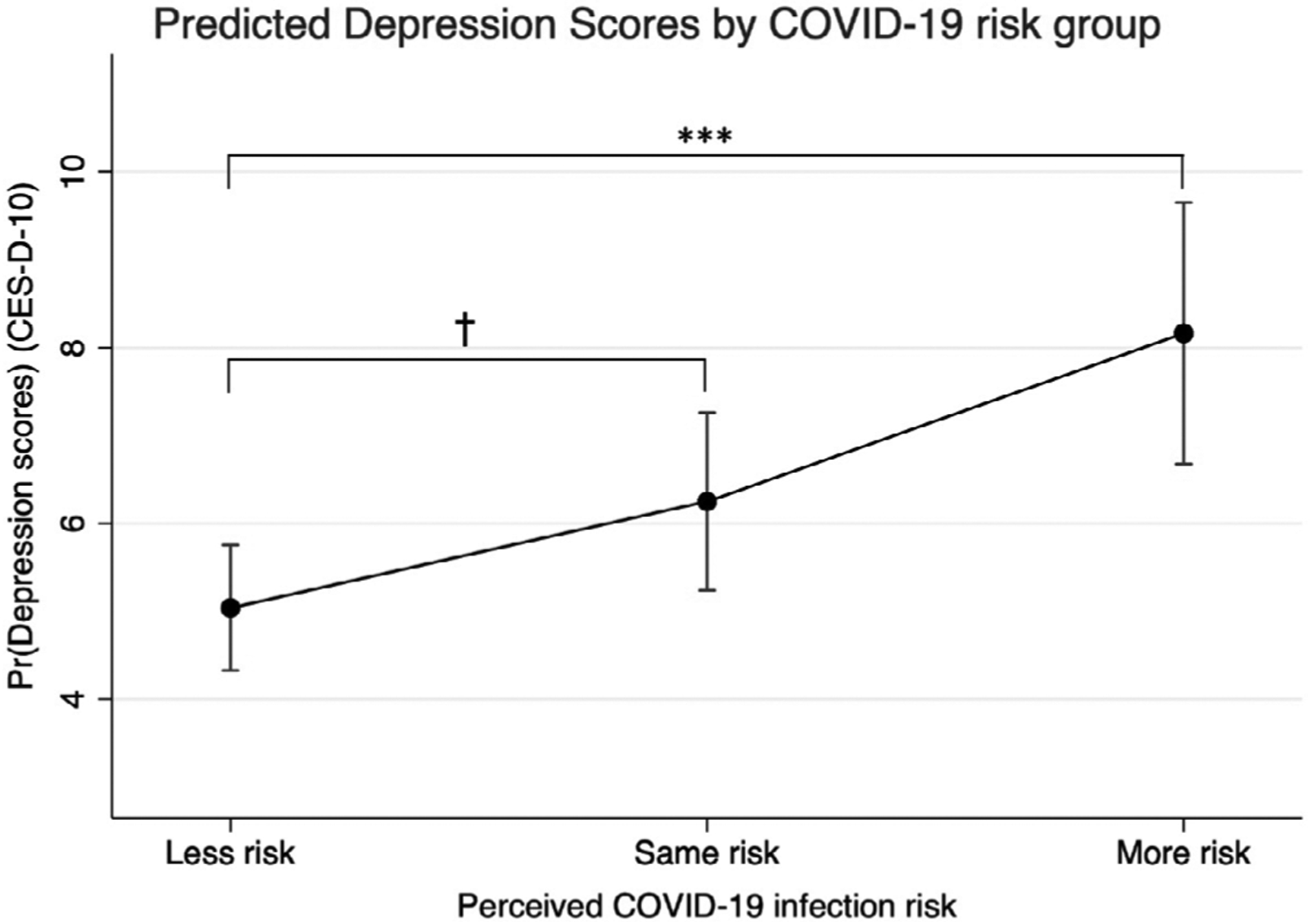
Perceived COVID-19 infection risk and Depression symptomatology. Note: Greater perceived risk of COVID-19 infection corresponds with greater depression symptomatology in adults living in Soweto. The effect of being in the “More risk” group is highly significant (P < .001) relative to being at “Less risk”, while the effect of perceiving that one is at the “Same risk” of COVID-19 infection relative to other individuals living in Soweto on depression symptoms is marginally significant (P = .088) (Kim et al., 2020)
FIGURE 2.
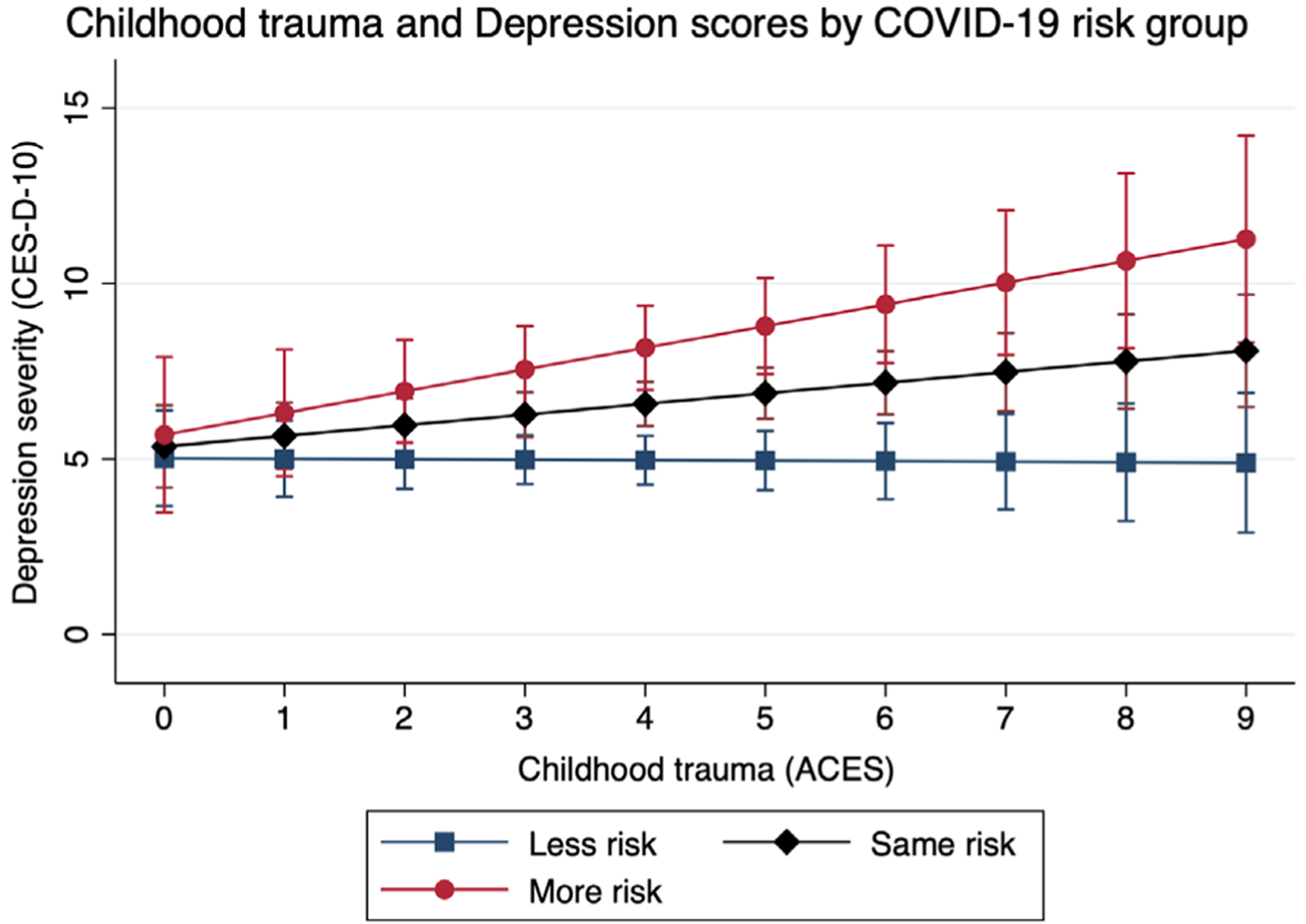
Relationship between childhood trauma and depression risk vary by perceived risk of COVID-19 infection. Note: Greater childhood trauma (ACES) potentiates the positive relationship between greater perceived COVID-19 risk and the severity of depressive symptomatology. The effect of the interaction between childhood trauma and perceived COVID-19 risk on depression is marginally significant (F[1, 208] = 3.51, P = .0625; Kim, Nyengerai, & Mendenhall, 2020)
Epidemiology alone, however, will not stop the pandemic or future health emergencies. As human biologists, we are perceptive to the limits and politics of epidemiological data, particularly during a pandemic. These include the difficulty of surveying marginalized and hard-to-reach communities, the representativeness and generalizability of data, and the politics of scientific research (Ford et al., 2008; Kim, 2020; LaVeaux & Christopher, 2009; Sisk & DuBois, 2020; Yonas et al., 2006). As anthropologists have previously argued, numbers and global health metrics can flatten the complexity of lived experience and sociopolitical realities (Adams, 2016; Sangaramoorthy & Benton, 2012), particularly during pandemic conditions. Numbers can also simply be false. We have already seen the intentional doctoring of national COVID-19 statistics in China (Verma 2020) and the United States (Rocco, 2020).
Finally, a deep examination of the ethics of data collection during the ever-changing times of COVID-19 is also crucial. The social conditions of the pandemic, the potential strain on research ethics review board and administration, and lack of guidance for research studies may obfuscate ethical guidelines for research studies (Sisk & DuBois, 2020; Townsend, Nielsen, Allister, & Cassidy, 2020). Scientists have also identified a growing belief of “research exceptionalism,” that the high standards of scientific practice may be compromised during a pandemic in order to expedite translational research (London & Kimmelman, 2020). As findings on the novel pandemic reproduce at unprecedented rates, upholding high ethical and scientific standards during a pandemic will allow researchers to better serve public health, maximize resources, and advance science (London & Kimmelman, 2020).
3.2 |. Developing a surveillance and referral system
We have also reformatted our remote data collection procedures to incorporate an impromptu surveillance system to identify immediate mental health and other household needs and to connect participants and their families with appropriate resources and telephonic counseling. Through our daily discussions, we have identified individuals with pressing concerns such as those who are seeking medical attention, food, and psychological distress, and provided direct referrals. For those seeking further psychosocial support or experiencing mental distress or any other matter concerning their mental well-being, we direct all patients to a free, 24/7 crisis hotline through a collaboration with the South African Depression and Anxiety Group (SADAG; http://www.sadag.org/), which houses a call center fully staffed with trained multicultural and multilingual counselors. The research team then conducts follow-up calls to monitor individuals with high psychiatric risk and morbidity and refers them back to the counseling service when needed. The collaboration precipitated from a series of conversations about the participant’s needs, the study’s goals, and SADAG’s services. Taking advantage of this existing resource allowed us to provide additional psychological resources at no cost. While numerous researchers provide psychological first aid (PFA) or clinical referrals to participants in their studies, there is a dearth of literature, both formal and informal, on best practice methods for PFA and clinical referrals practices in research studies. Creating a standard operation procedure can be beneficial for formalizing the referral protocol, future trainings, and developing a safe work environment.1
Additionally, researchers should also be mindful of overloading already strained healthcare systems, especially during the COVID-19 pandemic and in resource-limited settings, and identify alternative resources. Despite being situated on the campus of a major tertiary hospital, we are not able to refer participants to the psychiatric ward due to high patient loads, limited beds, and long queues in the emergency room (Docrat et al., 2019). Instead, we direct all patients to the aforementioned crisis hotline at South African Depression and Anxiety Group, who also provides containment-based multilingual counseling and referrals for mental healthcare, social workers, basic needs assistance, and community support groups. Importantly, free counseling resources and other accessible psychological services may not be readily available in certain settings, which raises larger questions around the roles, responsibility, and limitations of researchers in mitigating risk and safeguarding mental health for all involved in fieldwork and warrants future discussion. Fieldwork in human biology and biological anthropology often takes place in settings with limited mental health resources, social services, and other structural inequalities. Bearing witness to these realities and potentially placing participants at risk, whether intentionally or unintentionally, further necessitates researchers to identify relevant resources for study staff and participants and a greater consideration around the responsibilities, limitations, and ethics of the research team in facilitating usage and access of mental healthcare.
3.3 |. Safeguarding mental well-being of research staff—an underappreciated set of “frontline” workers
The psychological toll from daily conversation about fears of infection, experiences of depression and suicide during quarantine, and food insecurity is considerable. Exposures to secondary trauma and various forms of violence is a familiar but underappreciated burden that many research assistants across the world (Powell & Lloyd, 2001; Shannonhouse, Barden, Jones, Gonzalez, & Murphy, 2016), particularly in low-resource contexts, face when gathering data for population health research (Ng et al., 2016). Even evidence of secondary trauma among tran-scriptionists is known (Kiyimba & O’Reilly, 2016). Before we launched the COVID-19 and mental health study, we developed an informal emotional debriefing program to provide basic psychoeducation and mental health resources for my research staff given the heavy nature of our data collection. After transitioning to home-based work, we all faced the difficult psychological burden of quarantine and isolation in addition to holding daily discussions about stress, trauma, mental health, and the pandemic. Research staff are also provided free confidential counseling with a trained psychologist when needed and should be budgeted as a line item when preparing grant proposals. Formalizing and implementing our pre-existing emotional debriefing program continue to be essential for our team, which we hope to share in the near future.
We also know that the relationship between researcher and participant is experienced differently and can a range of impacts on one’s mental health. Social dynamics and relationships between researchers and interlocutors are shaped by race, class, age, gender, and other intersectional realities. For instance, a researcher can face aggression from participant, trauma from an unfamiliar fieldwork situation, or intersectional violence at multiple scales, particularly against women2 (Clancy, Nelson, Rutherford, & Hinde, 2014; Nelson, Rutherford, Hinde, & Clancy, 2017). Researchers involved in trauma related research can also experience a range of physical and emotional symptoms (Etherington, 2007). Additionally, the presence of researchers may actively harm the people being researched. In one retracted article3 published by a group of white researchers at Stellenbosch University, an institution complicit in the rise and formulation of apartheid ideology, researchers attempted to make conclusive assertions about “cognitive functioning” among Colored women living in the Western Cape province of South Africa in their 66 person, cross-sectional study. The study’s racist ideologies, flawed methodology, and problematic use of “Colored” as a social category led to its widespread criticism and ultimate retraction. As Aluwihare-Samaranayake (2012:76) states, “The risk involved to the researcher and/or the participant can vary from being trivial to profound, physical to psychological, individual or social.” As the global pandemic continues, we must continue to uphold critical and ethical anthropological practice while promoting the mental health and well-being of our research communities.
Funding information
Fogarty International Center, Grant/Award Number: D43 TW010543; National Science Foundation; Social Science Research Council; Wenner Gren Foundation
Footnotes
Readers of this piece can contact the author to receive a copy of the standard operation procedure used for this study.
No data reported on non-binary and gender non-conforming individuals.
The citation for this study is: Nieuwoudt, Dickie, Coetsee, Engelbrecht, and Terblanche (2020). To avoid giving any intellectual credit or academic recognition for this research, I do not include the citation in the bibliography.
REFERENCES
- Adams V (2016). Metrics: What counts in global health. Durham, North Carolina, United States: Duke University Press. [Google Scholar]
- Aluwihare-Samaranayake D (2012). Ethics in qualitative research: A view of the participants’ and researchers’ world from a critical standpoint. International Journal of Qualitative Methods, 11(2), 64–81. [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clancy KB, Nelson RG, Rutherford JN, & Hinde K (2014). Survey of academic field experiences (SAFE): Trainees report harassment and assault. PLoS One, 9(7), e102172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docrat S, Besada D, Cleary S, Daviaud E, & Lund C (2019). Mental health system costs, resources and constraints in Southh Africa: A national survey. Health Policy and Planning, 34(9), 706–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etherington K (2007). Working with traumatic stories: From transcriber to witness. International Journal of Social Research Methodology, 10(2), 85–97. [Google Scholar]
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, … Powe NR (2008). Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer: Interdisciplinary International Journal of the American Cancer Society, 112(2), 228–242. [DOI] [PubMed] [Google Scholar]
- Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, & Williams DR (2009). The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. South African Medical Journal, 99(5), 339–344. [PMC free article] [PubMed] [Google Scholar]
- Jung SJ, & Jun JY (2020). Mental health and psychological intervention amid COVID-19 outbreak: Perspectives from South Korea. Yonsei Medical Journal, 61(4), 271–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AW (2020). How should we study intergenerational trauma? Reflections on a 30-year birth cohort study in Soweto, South Africa. Somatosphere. http://somatosphere.net/2020/intergenerational-trauma-birth-cohort-study-south-africa.html/ [Google Scholar]
- Kim AW, Burgess R, Kwinda Z, Chiwandire N, & Mendenhall E (2020). Perceptions, understandings, and impacts of COVID-19 pandemic in urban South Africa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AW, Nyengerai T, & Mendenhall E (2020). Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: Perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. Psychological Medicine, 1–24. 10.1101/2020.06.13.20130120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiyimba N, & O’Reilly M (2016). An exploration of the possibility for secondary traumatic stress among transcriptionists: A grounded theory approach. Qualitative Research in Psychology, 13(1), 92–108. [Google Scholar]
- LaVeaux D, & Christopher S (2009). Contextualizing CBPR: Key principles of CBPR meet the indigenous research context. Pimatisiwin, 7(1), 1. [PMC free article] [PubMed] [Google Scholar]
- London AJ, & Kimmelman J (2020). Against pandemic research exceptionalism. Science, 368(6490), 476–477. [DOI] [PubMed] [Google Scholar]
- Nelson RG, Rutherford JN, Hinde K, & Clancy KB (2017). Signaling safety: Characterizing fieldwork experiences and their implications for career trajectories. American Anthropologist, 119(4), 710–722. [Google Scholar]
- Ng LC, Magidson JF, Hock RS, Joska JA, Fekadu A, Hanlon C, … Henderson DC (2016). Proposed training areas for global mental health researchers. Academic Psychiatry, 40(4), 679–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell RA, & Lloyd KR (2001). A national survey of violence experienced by community mental health researchers. Social Psychiatry and Psychiatric Epidemiology, 36(3), 158–163. [DOI] [PubMed] [Google Scholar]
- Reddy SP, Sewpaul R, Mabaso M, Parker S, Naidoo I, Jooste S, … Zuma K South Africans’ understanding of and response to the COVID-19 Outbreak: An online survey. Available at SSRN 3576939. 2020. [PubMed] [Google Scholar]
- Rocco P (2020). Trump’s fight over Covid-19 numbers shows how the hollowing out of expertise can be dangerous for American democracy. London, United Kingdom: USApp-American Politics and Policy Blog. [Google Scholar]
- Sangaramoorthy T, & Benton A (2012). Enumeration, identity, and health. Medical Anthropology, 31(4), 287–291. 10.1080/01459740.2011.638684 [DOI] [PubMed] [Google Scholar]
- Shannonhouse L, Barden S, Jones E, Gonzalez L, & Murphy A (2016). Secondary traumatic stress for trauma researchers: A mixed methods research design. Journal of Mental Health Counseling, 38(3), 201–216. [Google Scholar]
- Sisk BA, & DuBois J (2020). Research ethics during a pandemic: A call for normative and empirical analysis. The American Journal of Bioethics, 20(7), 82–84. [DOI] [PubMed] [Google Scholar]
- South African COVID-19 Modelling Consortium. (2020). Estimating cases for COVID-19 in South Africa long-term provincial projections.
- StatsSA. (2019). Five facts about poverty in South Africa. Retrieved from http://www.statssa.gov.za/?p=12075 [Google Scholar]
- Subramaney U, Kim AW, Chetty I, Chetty S, Jayrajh P, Govender M, … Pak E (2019). Coronavirus disease 2019 (COVID-19) and psychopathology in South Africa: Beyond anxiety disorders. Wits Journal of Clinical Medicine, 2(2), 115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend E, Nielsen E, Allister R, & Cassidy SA (2020). Key ethical questions for research during the COVID-19 pandemic. The Lancet Psychiatry, 7(5), 381–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Media briefing on COVID-19.
- Yonas MA, Jones N, Eng E, Vines AI, Aronson R, Griffith DM, … DuBose M (2006). The art and science of integrating undoing racism with CBPR: Challenges of pursuing NIH funding to investigate cancer care and racial equity. Journal of Urban Health, 83(6), 1004–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]


