Abstract
Phenytoin is an antiepileptic drug with a narrow therapeutic index and large inter-patient pharmacokinetic variability, partly due to genetic variation in CYP2C9. Furthermore, the variant allele HLA-B*15:02 is associated with an increased risk of Stevens-Johnson syndrome and toxic epidermal necrolysis in response to phenytoin treatment. We summarize evidence from the published literature supporting these associations and provide therapeutic recommendations for the use of phenytoin based on CYP2C9 and/or HLA-B genotypes (updates on cpicpgx.org).
Keywords: Phenytoin, HLA-B, CPIC, CYP2C9, pharmacogenetics, fosphenytoin, Stevens-Johnson syndrome, toxic epidermal necrolysis
Introduction
The purpose of this guideline is to provide information for the interpretation of human leukocyte antigen B (HLA-B) and/or cytochrome P450 2C9 (CYP2C9) genotype test results to guide use and/or dosing of phenytoin. Guidelines for phenytoin use and cost effectiveness of genetic testing are outside the scope of this report. This guideline updates the 2014 Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C9 and HLA-B Genotypes and Phenytoin Dosing (1). CPIC guidelines are periodically updated at www.cpicpgx.org.
Focused Literature Review
We reviewed literature focused on CYP2C9 and HLA variation and phenytoin use (details in Supplemental Material). Evidence is summarized in Tables S1 and S2.
Genes: HLA-B and CYP2C9
Background
This guideline discusses HLA-B and the risk of Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) with phenytoin and CYP2C9 as it relates to phenytoin metabolism and dosing. Updated CYP2C9 allele function assignments are provided using the activity score system.
HLA-B.
HLA-B is part of a gene cluster designated as the human major histocompatibility complex (MHC) located on the short arm of chromosome 6. The cluster contains three classes (I, II and III). MHC class I contains three genes: HLA-A, HLA-B and HLA-C. These genes encode a cell surface protein that binds peptides generated by proteolysis and extruded from proteasomes. The presentation of these cell surface peptides enables the immune system to distinguish self-proteins from foreign proteins (see Supplement for further discussion).
HLA genes, specifically HLA-B, are among the most highly polymorphic genes in the human genome. HLA polymorphisms were previously ascertained serologically, but DNA sequencing methods have identified genetic variability in the HLA region with greater precision. More than 7,000 HLA-B alleles, many of which differ by more than one nucleotide from each other, were deposited to the World Health Organization Nomenclature Committee for Factors of the HLA System (http://hla.alleles.org). Each allele is designated by the gene name followed by an asterisk and up to an eight-digit (four pairs) identifier, which gives information about the allele type (designated by the first two digits) followed by the specific protein subtypes (second set of up to 6 digits). The first four digits typically differ in at least one amino acid substitution and give the most important functional information. For more information on the description of the current HLA allele nomenclature see http://hla.alleles.org/nomenclature/naming.html and a previous CPIC guideline (2). This guideline discusses only the HLA-B*15:02 allele as it relates to the phenytoin-induced cutaneous adverse drug reactions, including SJS and TEN.
CYP2C9.
The hepatic CYP2C9 enzyme system metabolizes many clinically relevant drugs, including phenytoin (http://www.pharmgkb.org/pathway/PA145011115). The CYP2C9 gene is highly polymorphic, with at least 61 variant alleles and multiple suballeles (see CYP2C9 Allele Definition Table in references (3, 4); https://www.pharmvar.org/gene/CYP2C9 (5)). Each CYP2C9 star (*) allele is defined by one or more single nucleotide polymorphisms (SNPs) or nucleotide deletions that may alter enzyme activity. The two most common variants with decreased enzyme activity are CYP2C9*2 (rs1799853) and CYP2C9*3 (rs1057910) (6). CYP2C9 allele and diplotype frequencies differ between racial/ethnic groups ((7); CYP2C9 Frequency Table (3, 4)). In vitro and clinical studies suggest that CYP2C9 decreased function and no function alleles generate variant enzymes with activities that are substrate-dependent (CYP2C9 Allele Functionality Table (3, 4)). Therefore, assigning function to CYP2C9 alleles requires careful evaluation of individual drugs.
Genetic Test Interpretation
HLA-B.
Clinical genotyping test results for HLA-B*15:02 are interpreted as “positive” if one or two copies of HLA-B*15:02 are present or “negative” if no copies of HLA-B*15:02 are found. HLA-B alleles do not affect the pharmacokinetics or pharmacodynamics of phenytoin. Phenotype assignments for HLA-B*15:02 genotypes are summarized in Table 1. HLA-B*15:02 is most prevalent in East Asian and Central/South Asian populations with allele frequency ranging from 1% to over 20%. HLA-B*15:02 is less frequent in European populations (0–1%) and was not detected in several sub-Saharan African populations (HLA-B Frequency Table (3, 4, 8)).
Table 1.
Assignment of likely HLA-B phenotypes based on genotypes
| HLA Phenotype | Genotype | Examples of diplotypes |
|---|---|---|
| HLA-B*15:02 negative | Homozygous for an allele other than HLA-B*15:02 |
*X/*X Where *X = any HLA-B allele other than HLA-B*15:02. |
| HLA-B*15:02 positive | Heterozygous or homozygous variant |
*15:02/*X, *15:02/*15:02 Where *X = any HLA-B allele other than HLA-B*15:02. |
CYP2C9.
Most clinical laboratories reporting CYP2C9 genotype use the star (*) allele nomenclature and may interpret the patient’s predicted metabolizer phenotype based on the combination of CYP2C9 alleles (diplotype) (Table 2; CYP2C9 Diplotype to Phenotype Table (3, 4)). Not all CYP2C9 allelic variants may be tested, and this influences the accuracy of the genotype-based dose prediction. Misclassification occurs primarily in individuals of Asian or African ancestry who carry decreased function CYP2C9 alleles other than *2 or *3 (CYP2C9 Frequency Table (3, 4)). An activity value is assigned to each CYP2C9 allele ranging from 0 to 1 (i.e. 0 for no function, 0.5 for decreased function, and 1.0 for normal function). Activity values are summed to calculate the activity score (AS) of a diplotype (3, 4). The CYP2C9 AS is translated into phenotypes as follows: individuals with an AS of 0 or 0.5 are poor metabolizers (PMs), those with a score of 1 or 1.5 are intermediate metabolizers (IMs), and those with a score of 2 are normal metabolizers (NMs) (Table 2; CYP2C9 Diplotype to Phenotype Table (3, 4)). Of note, as there are no known increased function alleles for CYP2C9, no ultrarapid or rapid CYP2C9 metabolizer phenotypes currently exist. Reference laboratories providing clinical CYP2C9 genotyping may use various methods to assign phenotypes. Thus, before making phenytoin therapeutic decisions, we strongly advise referring to the online CYP2C9 Diplotype to Phenotype Table (3, 4) that lists of all possible CYP2C9 diplotypes and phenotype assignments.
Table 2.
Assignment of likely CYP2C9 phenotypes based on genotypes
| CYP2C9 Phenotypea,b | Activity Score | Genotypes | Examples of Diplotypes |
|---|---|---|---|
| Normal Metabolizer | 2 | An individual carrying two normal function alleles | *1/*1 |
| Intermediate Metabolizer | 1.5 1 |
An individual carrying one normal function allele plus one decreased function allele; OR one normal function allele plus one no function allele OR two decreased function alleles |
*1/*2 *1/*3, *2/*2 |
| Poor Metabolizer | 0.5 0 |
An individual carrying one no function allele plus one decreased function allele; OR two no function alleles |
*2/*3 *3/*3 |
Assignment of allele function and associated citations can be found at https://www.pharmgkb.org/page/cyp2c9RefMaterials (see CYP2C9 Allele Definition Table and CYP2C9 Allele Functionality Table in references (3, 4)). For a complete list of CYP2C9 diplotypes and resulting phenotypes, see the CYP2C9 Diplotype to Phenotype Table in references (3, 4).
Of note, Table 2 denotes a change to the previous (2014) genotype to phenotype translation tables for diplotypes containing CYP2C9*2 and other decreased function alleles (see Supplement for details). The CYP2C9*2/*2 diplotype (AS=1) is now translated into the IM phenotype group (originally translated to PM). This change is based on data for multiple substrates (flurbiprofen, celecoxib, phenytoin, and warfarin) showing a similar effect of CYP2C9*1/*3 (AS=1) and CYP2C9*2/*2 on metabolic ratio and dose requirements (warfarin) (9–11). Furthermore, CYP2C9*3 and alleles with a similar clinical effect and function are classified as ‘no function’ alleles with a value of 0 for AS calculation. This is based on CYP2C9*3/*3, which represents the diplotype with the lowest metabolic activity and slowest pharmacokinetic clearance. Other alleles with similarly low function have also been classified as ‘no function’(see CYP2C9 Allele Functionality Table (3, 4)).
Available Genetic Test Options
See Supplement and the Genetic Testing Registry (https://www.ncbi.nlm.nih.gov/gtr/) for more information on commercially available clinical testing options.
Incidental findings
While multiple autoimmune diseases are associated with HLA-B alleles, HLA-B*15:02 has not been reproducibly associated with these or other non-drug induced diseases (12). No diseases have been linked to genetic variations in CYP2C9, except for a small study that associated CYP2C9*2 and *3 variants and phenytoin with a higher frequency of cerebellar atrophy (13).
Other Considerations
Not applicable
Drugs: Phenytoin and Fosphenytoin
Phenytoin and its prodrug fosphenytoin are commonly used treatments for both focal and generalized convulsive status epilepticus. Phenytoin is indicated for control of generalized tonic-clonic (grand mal) and complex partial (psychomotor, temporal lobe) seizures and prevention and treatment of seizures occurring during or following neurosurgery (14). Once a mainstay of treatment, phenytoin’s complex dosing and propensity for side effects and drug-drug interactions have led to a decline in its use.
Phenytoin dosing is complex owing to its nonlinear dose accumulation pharmacokinetics and requirements for adjustments based on patient weight, sex, and age (see Supplementary Material and Figures S1 and S2). Outpatient therapy is generally initiated at 5–7 mg/kg/day in adults (slightly higher in children) and may be given once daily (or twice daily in children). The starting dose must be lower in the setting of hepatic impairment. Careful dose adjustments must then be made to stabilize drug concentrations within the targeted therapeutic range (typically 10–20 mcg/mL). In urgent situations such as status epilepticus, intravenous loading doses of 15–20 mg/kg are given over 1–3 mg/kg/min or 50 mg/min, whichever is slower, with cardiac monitoring (14), followed by intravenous or oral maintenance doses, as above. Acute dose-related side effects include sedation, ataxia, dizziness, nystagmus, nausea, and cognitive impairment. The drug is highly allergenic, and rashes ranging from mild eruptions to life-threatening hypersensitivity reactions may be seen. HLA-B*15:02 is associated with phenytoin-induced SJS and TEN. Sub-acutely, hematologic and hepatic toxicity can occur. Hepatic toxicity is likely a hypersensitivity reaction and is usually accompanied by rash (15), while the hematologic toxicity may reflect leukopenia or pancytopenia. Suicide ideation/behavior has also been linked to phenytoin (two-fold greater risk than placebo), as described in the Food and Drug Administration (FDA) label (14).
Because of the narrow therapeutic index of the drug, initial maintenance dose selection is important. Higher plasma concentrations increase the probability of toxicity (16). However, nonlinear saturable pharmacokinetics, CYP2C9 autoinduction and CYP2C9 pharmacogenetics complicate dose-selection. The CYP2C9 PM phenotype and CYP2C9 drug interactions, such as concomitant use with voriconazole, can significantly increase phenytoin exposure (17). Variability in protein binding, primarily related to changes in albumin concentrations, can confound the relationship of therapeutic drug monitoring, unless unbound drug concentrations are assayed (18). Use of phenytoin for outpatient therapy has declined in the last decade owing to its potential for drug interactions, chronic metabolic effects including bone loss, and the aforementioned pharmacokinetic difficulties that make phenytoin dose adjustments challenging (see Supplement for further discussion).
Linking genetic variability to variability in drug-related phenotypes
Substantial evidence links CYP2C9 and HLA-B*15:02 genotypes with phenotypic variability (see Tables S1 and S2). Application of a grading system that evaluates the relationship between genetic variation and phenotypic variability produces consistent, high quality evidence. The evidence presented in the Supplement text and in Tables S1 and S2 provides the basis for the dosing recommendations in Table 3. In this guideline, all clinical recommendations were based on evidence graded at either High (Evidence includes consistent results from well-designed, well-conducted studies) or Moderate (Evidence is sufficient to determine effects, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies; generalizability to routine practice; or indirect nature of the evidence).
Table 3.
Recommended dosing of phenytoin/fosphenytoin based on HLA-B*15:02 and CYP2C9 phenotype/genotype
| HLA-B*15:02 Phenotype | CYP2C9 Phenotype | Implication | Therapeutic Recommendation | Classification of Recommendation | Considerations |
|---|---|---|---|---|---|
| HLA-B*15:02 positive | Any CYP2C9 phenotype | Increased risk of phenytoin-induced SJS/TEN | If patient is phenytoin-naïve, do not use phenytoin/fosphenytoin. Avoid carbamazepine and oxcarbazepine. | Strong | Other aromatic anticonvulsants, including eslicarbazepine, lamotrigine, and phenobarbital, have weaker evidence linking SJS/TEN with the HLA-B*15:02 allele; however, caution should still be used in choosing an alternative agent. |
| If the patient has previously used phenytoin continuously for longer than three months without incidence of cutaneous adverse reactions, cautiously consider use of phenytoin in the future. The latency period for drug-induced SJS/TEN is short with continuous dosing and adherence to therapy (4–28 days), and cases usually occur within three months of dosing. | Optional | Previous tolerance of phenytoin is not indicative of tolerance to other aromatic anticonvulsants. | |||
| HLA-B*15:02 negative | CYP2C9 NM | Normal phenytoin metabolism | No adjustments needed from typical dosing strategies. Subsequent doses should be adjusted according to therapeutic drug monitoring, response, and side effects. An HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN, and patients should be carefully monitored according to standard practice. | Strong | |
| HLA-B*15:02 negative | CYP2C9 IM AS 1.5 | Slightly reduced phenytoin metabolism; however, this does not appear to translate into increased side effects. | No adjustments needed from typical dosing strategies. Subsequent doses should be adjusted according to therapeutic drug monitoring, response and side effects. An HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN, and patients should be carefully monitored according to standard practice. | Moderate | |
| HLA-B*15:02 negative | CYP2C9 IM AS 1.0 | Reduced phenytoin metabolism; Higher plasma concentrations will increase probability of toxicities. |
For first dose, use typical initial or loading dose. For subsequent doses, use approximately 25% less than typical maintenance dose. Subsequent doses should be adjusted according to therapeutic drug monitoring, response and side effects. An HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN, and patients should be carefully monitored according to standard practice. | Moderate | |
| HLA-B*15:02 negative | CYP2C9 PM | Reduced phenytoin metabolism; Higher plasma concentrations will increase probability of toxicities. |
For first dose, use typical initial or loading dose. For subsequent doses use approximately 50% less than typical maintenance dose. Subsequent doses should be adjusted according to therapeutic drug monitoring, response, and side effects. An HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN, and patients should be carefully monitored according to standard practice. | Strong | |
| HLA-B*15:02 negative | Indeterminate | n/a (not applicable) | n/a | No recommendation | n/a |
Therapeutic Recommendations
HLA-B*15:02 and CYP2C9 dosing recommendations.
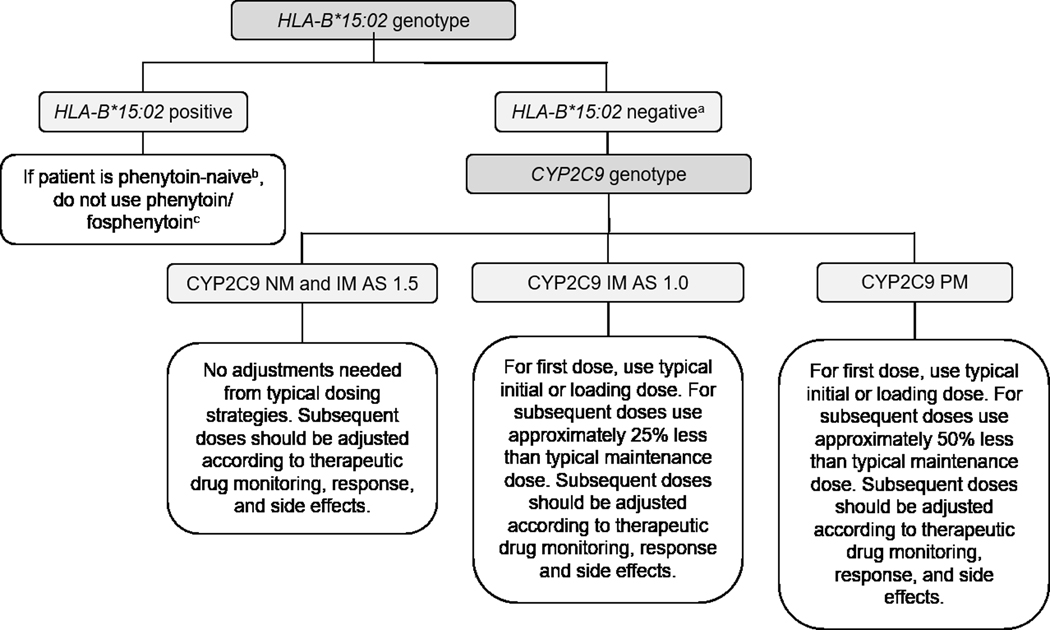
Table 3 summarizes the dosing recommendations for phenytoin based on genotype-derived HLA-B*15:02 and CYP2C9 phenotypes. If both HLA-B*15:02 and CYP2C9 genotypes are known, consider the HLA-B*15:02 genotype first, then CYP2C9 genotype (Figure 1; Table 3).
Figure 1. Algorithm for suggested clinical actions based on HLA-B*15:02 and CYP2C9 genotype.
NM, normal metabolizer; IM, intermediate metabolizer; PM, poor metabolizer; AS, Activity Score
aAn HLA-B*15:02 negative test does not completely eliminate the risk of phenytoin-induced SJS/TEN, and patients should be carefully monitored according to standard practice.
bIf the patient has previously used phenytoin continuously for longer than three months without incidence of cutaneous adverse reactions, cautiously consider use of phenytoin in the future. The latency period for drug-induced SJS/TEN is short with continuous dosing and adherence to therapy (4–28 days), and cases usually occur within three months of dosing.
cOther aromatic anticonvulsants, including eslicarbazepine, lamotrigine, and phenobarbital, have weaker evidence linking SJS/TEN with the HLA-B*15:02 allele; however, caution should still be used in choosing an alternative agent.
HLA-B*15:02 recommendations.
If a patient is phenytoin-naïve and HLA-B*15:02 positive, the patient has an increased risk of SJS/TEN and the recommendation is to consider using an anticonvulsant other than phenytoin unless the benefits of treating the underlying disease clearly outweigh the risks (see Table 3). Carbamazepine and oxcarbazepine should also be avoided if a patient is HLA-B*15:02 positive (19). Alternative medications such as eslicarbazepine acetate and lamotrigine have limited evidence linking SJS/TEN with the HLA-B*15:02 allele. These alternatives to phenytoin should be chosen with caution (see Supplement for details). With standard dosing, phenytoin-induced SJS/TEN usually develops within the first 4–28 days of therapy (20–22). Therefore, patients who have evidence of adherence and continuous dosing of phenytoin or fosphenytoin for longer than 3 months without the development of cutaneous reactions are at low risk of hypersensitivity events related to phenytoin in the future, regardless of HLA-B*15:02 status (Figure 1; Table 3). The FDA warning for phenytoin states “Consideration should be given to avoiding phenytoin as an alternative for carbamazepine in patients positive for HLA-B*15:02 due to the increased risk of SJS/TEN in patients of Asian ancestry (14)”. The evidence linking HLA-B*15:02 to phenytoin-induced SJS/TEN was generated primarily in individuals of Asian ancestry as the frequency of HLA-B*15:02 is very low in other populations (see HLA-B Frequency Table (3, 4)). However, this allele may also occur in other populations throughout the world that have yet to be studied, and patients may be unaware of, or fail to disclose, Asian ancestry in their families (23, 24).
If a patient is phenytoin-naïve and HLA-B*15:02 negative, the patient has a normal risk of phenytoin-induced SJS/TEN and the recommendation is to use phenytoin with dosage adjustments based on CYP2C9 genotype (if known) or standard dosing guidelines (if CYP2C9 genotype is unknown). However, an HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN (see Supplement for additional guidance).
CYP2C9 recommendations.
Phenytoin and fosphenytoin dose should first be adjusted according to a patient’s clinical characteristics. The recommended phenytoin initial or loading and maintenance doses do not need adjustments based on genotype for CYP2C9 NMs and IMs with an AS of ≥1.5. Available evidence does not clearly indicate the extent of dose reduction needed to prevent phenytoin-related toxicities in CYP2C9 IMs with an AS of 1.0 and PMs with an AS of 0 or 0.5. Furthermore, multiple case studies have observed that CYP2C9 PMs are at increased risk for exposure-related phenytoin toxicities, and multiple studies have observed an association between the CYP2C9*3 allele and SJS/TEN (25–27). Although carriage of the CYP2C9*3 allele is insufficient to predict phenytoin-induced SJS/TEN, these and other data suggest that the risk of SJS/TEN is dose-related and provide an additional rationale for reducing phenytoin dose in CYP2C9 PMs (28). Thus, our recommendations are conservative given the variability surrounding phenytoin dosing. Based on the doses reported in the pharmacokinetic and pharmacogenetic studies mentioned above (29–31) and in Table S2, a typical initial or loading dose followed by at least a 25% reduction in the recommended starting maintenance dose may be considered for CYP2C9 IMs with AS of 1.0. Subsequent maintenance doses should be adjusted based on therapeutic drug monitoring and response. For CYP2C9 PMs, use a typical initial or loading dose then consider at least a 50% reduction of starting maintenance dose with subsequent maintenance doses adjusted based on therapeutic drug monitoring and response.
Pediatrics.
Much of the evidence (summarized in Table S1) linking HLA-B*15:02 to phenytoin-induced SJS/TEN was generated in both children and adults. Therefore, the above recommendation is made regardless of CYP2C9 genotype, individual age, race or ancestry. For pediatric patients who are CYP2C9 IMs or PMs, dose adjustment as described in Table 3 with therapeutic drug monitoring is recommended. While limited data are available for effects of CYP2C9 alleles on phenytoin metabolism in pediatric patient populations, there is no compelling data to indicate that CYP2C9 polymorphisms will affect phenytoin metabolism differently in children compared to adults. As such, the pediatric recommendation is extrapolated using adult data. Special considerations in neonates and older pediatric patients, including a high degree of dose variability and dosage forms, and evidence from pediatric populations is included in the supplement (see Pediatrics section of the Supplement for details).
Other considerations
HLA.
HLA-B*15:02 is linked to SJS and TEN but not to a predisposition for other phenytoin-induced cutaneous ADRs such as mild maculopapular eruptions (MPE) or drug hypersensitivity syndrome (HSS) (32). Other HLA-B alleles have also been associated with phenytoin-induced drug reactions with eosinophilia and systemic symptoms (DRESS) and are associated with hypersensitivity reactions to other drugs (26, 33). CPIC guidelines are available for HLA-B*15:02 and HLA-A*31:01 and carbamazepine- and oxcarbazepine-induced SJS and TEN (2, 19). Although the structural similarity between phenytoin and carbamazepine and the shared association of the HLA-B*15:02 allele with SJS and TEN might suggest cross-reactivity with HLA-A*31:01, no association between HLA-A*31:01 and phenytoin-induced SJS and TEN has been presently found. CPIC guidelines are also available for HLA-B*57:01 and abacavir-induced hypersensitivity reactions and HLA-B*58:01 and allopurinol-induced severe cutaneous adverse reactions (2, 19, 34).
CYP2C9.
Because of its potent CYP-inducing properties, phenytoin can contribute to a large number of drug interactions, especially involving increased metabolism of other agents with subsequent decrease in their plasma concentrations (35). A full discussion of these is beyond the scope of this guideline, but agents prominently and significantly affected include antineoplastic and immunosuppressive agents, lipid-lowering agents, psychotropics, oral contraceptives, antifungals and warfarin. Furthermore, inhibitors of CYP2C9 can cause phenytoin overexposure and toxicity. Although there are several potent CYP2C9 enzyme inhibitors such as fluconazole and amiodarone, other less potent drugs can produce significant elevations in phenytoin plasma concentrations. Therefore, it is important to interpret the results of pharmacogenetic testing in the context of other co-administered drugs.
CYP2C9 genetic variation does not account for all observed pharmacokinetic variability in phenytoin metabolism. Some studies suggest that variants in other genes also contribute to altered phenytoin metabolism (e.g., CYP2C19, CYP1A1, and EPHX1; see (36) for a review) and combined genetic analysis might improve the prediction of phenytoin metabolism (29, 30). However, these studies evaluating the effect of multiple gene variation and phenytoin dose requirements are limited and have not been replicated. Consequently, this guideline on genotype-directed phenytoin dosing is limited to CYP2C9.
Implementation of this Guideline:
The guideline supplement and CPIC website (https://cpicpgx.org/guidelines/guideline-for-phenytoin-and-cyp2c9-and-hla-b/) contains resources that can be used within electronic health records (EHRs) to assist clinicians in applying genetic information to patient care for the purpose of drug therapy optimization (see Resources to incorporate pharmacogenetics into an electronic health record with clinical decision support in the Supplemental Material).
Recommendations for Incidental Findings
Case reports have identified cross-reactions to lamotrigine and other anti-epileptic drugs in the presence of HLA-B*15:02 (see Supplemental Material for further discussion). However, larger replication studies are warranted.
CYP2C9 metabolizes substrates from several drug classes, including nonsteroidal anti-inflammatory drugs (NSAIDs) and oral hypoglycemics. Patients with enhanced sensitivity to warfarin may have a decreased capacity to metabolize phenytoin owing to the presence of one or more CYP2C9 variant alleles (37).
Potential Benefits and Risks for the Patient
The potential benefit for patients with existing CYP2C9 and/or HLA-B*15:02 genotype information is avoidance of adverse effects in patients who are CYP2C9 IMs (AS of 1.0) and CYP2C9 PMs by making significant reductions in their initial maintenance dose or by selecting alternative agents for patients who carry HLA-B*15:02. A potential risk is that phenytoin therapy may have been needlessly avoided in patients who may not have developed SJS/TEN; however, this risk is mitigated because alternatives to phenytoin with comparable effectiveness exist. Another potential risk would be an error in genotyping. Also, many commercially available genotyping tests do not detect all known alleles or de novo variants (for example HLA-B alleles in the same B75 serotype family as HLA-B*15:02). Other HLA alleles are not well characterized, resulting in uncertainty when predicting the phenotype for some genetic test results. Since an HLA-B*15:02 negative test does not eliminate the risk of phenytoin-induced SJS/TEN and since genetic tests may not detect rare CYP2C9 variants, a patient with a high ADR risk could be prescribed phenytoin or a patient with reduced CYP2C9 activity could be prescribed a higher than needed phenytoin dose. Moreover, because not all phenytoin-induced adverse events are attributed to HLA-B*15:02 or CYP2C9 metabolizer status, particularly in non-East and Central/South Asian populations, clinicians should carefully monitor all patients according to standard practices.
Caveats: Appropriate Use and/or Potential Misuse of Genetic Tests
The application of genotype-based dosing is most appropriate when initiating phenytoin maintenance therapy. Obtaining genetic information after months of drug therapy is less informative, given that the drug dose may have already been adjusted based on therapeutic drug monitoring. As with all diagnostic tests, genetic tests are only one of several pieces of clinical information that should be considered before initiating and maintaining drug therapy.
Disclaimer
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines reflect expert consensus based on clinical evidence and peer-reviewed literature available at the time they are written and are intended only to assist clinicians in decision-making, as well as to identify questions for further research. New evidence may have emerged since the time a guideline was submitted for publication. Guidelines are limited in scope and are not applicable to interventions or diseases not specifically identified. Guidelines do not account for all individual variation among patients and cannot be considered inclusive of all proper methods of care or exclusive of other treatments. It remains the responsibility of the health care provider to determine the best course of treatment for the patient. Adherence to any guideline is voluntary, with the ultimate determination regarding its application to be solely made by the clinician and the patient. CPIC assumes no responsibility for any injury to persons or damage to property related to any use of CPIC’s guidelines, or for any errors or omissions.
Supplementary Material
Acknowledgements
We acknowledge the critical input of members of CPIC of the Pharmacogenomics Research Network (PGRN), particularly Dr. Mary V. Relling (St Jude Children’s Research Hospital).
Funding
This work is funded by National Institutes of Health (NIH) grants CPIC (R24GM115264 and U24HG010135) and PharmGKB (R24 GM61374), R24GM123930 (AG), GM092666 (CEH), GM32165 (AER), UO1 GM092676, and U01 HL0105918. JHK is supported by grants from the NIH’s National Heart Lung and Blood Institute (NHLBI) under award number K01HL143137, the American College of Clinical Pharmacy, and the Flinn Foundation. AAS is supported by grant APP108798 by the National Health and Medical Research Council of Australia. EJP receives funding from the NIH (R01 HG010863–01, 1P50GM115305–01, R21AI139021 and R34AI136815) and NHMRC (APP1123499).
Footnotes
Conflicts of Interest
EJP is a consultant for Biocryst. She is section editor for drug allergy (uptodate) and is co-director of IIID, Pty Ltd that holds a patent for HLA-B*57:01 testing for abacavir hypersensitivity. She holds a provisional patent for HLA-A*32:01 testing for vancomycin-induced DRESS. All other authors declared no competing interests for this work.
References
- (1).Caudle KE et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin Pharmacol Ther 96, 542–48 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Martin MA, Klein TE, Dong BJ, Pirmohamed M, Haas DW & Kroetz DL Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing. Clin Pharmacol Ther 91, 734–8 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).CPIC. CPIC® Guideline for Phenytoin and CYP2C9 and HLA-B. <https://cpicpgx.org/guidelines/guideline-for-phenytoin-and-cyp2c9-and-hla-b/>. [Google Scholar]
- (4).PharmGKB. Gene-specific Information Tables for CYP2C9. <https://www.pharmgkb.org/page/cyp2c9RefMaterials>. [Google Scholar]
- (5).Gaedigk A. et al. The Pharmacogene Variation (PharmVar) Consortium: Incorporation of the Human Cytochrome P450 (CYP) Allele Nomenclature Database. Clin Pharmacol Ther 103, 399–401 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Lee CR, Goldstein JA & Pieper JA Cytochrome P450 2C9 polymorphisms: a comprehensive review of the in-vitro and human data. Pharmacogenetics 12, 251–63 (2002). [DOI] [PubMed] [Google Scholar]
- (7).Cespedes-Garro C. et al. Worldwide interethnic variability and geographical distribution of CYP2C9 genotypes and phenotypes. Expert Opin Drug Metab Toxicol 11, 1893–905 (2015). [DOI] [PubMed] [Google Scholar]
- (8).Gonzalez-Galarza FF et al. Allele frequency net database (AFND) 2020 update: gold-standard data classification, open access genotype data and new query tools. Nucleic Acids Res 48, D783–D788 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Vogl S, Lutz RW, Schonfelder G. & Lutz WK CYP2C9 genotype vs. metabolic phenotype for individual drug dosing--a correlation analysis using flurbiprofen as probe drug. PLoS One 10, e0120403 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Kusama M, Maeda K, Chiba K, Aoyama A. & Sugiyama Y. Prediction of the effects of genetic polymorphism on the pharmacokinetics of CYP2C9 substrates from in vitro data. Pharm Res 26, 822–35 (2009). [DOI] [PubMed] [Google Scholar]
- (11).Lindh JD, Holm L, Andersson ML & Rane A. Influence of CYP2C9 genotype on warfarin dose requirements--a systematic review and meta-analysis. Eur J Clin Pharmacol 65, 365–75 (2009). [DOI] [PubMed] [Google Scholar]
- (12).Karnes JH et al. Phenome-wide scanning identifies multiple diseases and disease severity phenotypes associated with HLA variants. Sci Transl Med 9, (389):eaai8708 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Twardowschy CA, Werneck LC, Scola RH, Borgio JG, De Paola L. & Silvado C. The role of CYP2C9 polymorphisms in phenytoin-related cerebellar atrophy. Seizure 22, 194–97 (2013). [DOI] [PubMed] [Google Scholar]
- (14).FDA. Phenytoin drug label. <https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&varApplNo=010151>. Accessed 1/10 2020. [Google Scholar]
- (15).Parker WA & Shearer CA Phenytoin hepatotoxicity: a case report and review. Neurology 29, 175–78 (1979). [DOI] [PubMed] [Google Scholar]
- (16).Greenberg RG et al. Therapeutic Index Estimation of Antiepileptic Drugs: A Systematic Literature Review Approach. Clin Neuropharmacol 39, 232–40 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Purkins L, Wood N, Ghahramani P, Love ER, Eve MD & Fielding A. Coadministration of voriconazole and phenytoin: pharmacokinetic interaction, safety, and toleration. Br J Clin Pharmacol 56 Suppl 1, 37–44 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Ter Heine R, Kane SP, Huitema ADR, Krasowski MD & van Maarseveen EM Nonlinear protein binding of phenytoin in clinical practice: Development and validation of a mechanistic prediction model. Br J Clin Pharmacol 85, 2360–68 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Phillips EJ et al. Clinical Pharmacogenetics Implementation Consortium Guideline for HLA Genotype and Use of Carbamazepine and Oxcarbazepine: 2017 Update. Clin Pharmacol Ther 103, 574–81 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Tennis P. & Stern RS Risk of serious cutaneous disorders after initiation of use of phenytoin, carbamazepine, or sodium valproate: a record linkage study. Neurology 49, 542–46 (1997). [DOI] [PubMed] [Google Scholar]
- (21).Roujeau JC et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med 333, 1600–07 (1995). [DOI] [PubMed] [Google Scholar]
- (22).Sassolas B. et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther 88, 60–8 (2010). [DOI] [PubMed] [Google Scholar]
- (23).Fang H. et al. A Screening Test for HLA-B( *)15:02 in a Large United States Patient Cohort Identifies Broader Risk of Carbamazepine-Induced Adverse Events. Front Pharmacol 10, 149 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Lonjou C. et al. A European study of HLA-B in Stevens-Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharmacogenet Genomics 18, 99–107 (2008). [DOI] [PubMed] [Google Scholar]
- (25).Yampayon K. et al. Influence of genetic and non-genetic factors on phenytoin-induced severe cutaneous adverse drug reactions. Eur J Clin Pharmacol 73, 855–65 (2017). [DOI] [PubMed] [Google Scholar]
- (26).Tassaneeyakul W. et al. Associations between HLA class I and cytochrome P450 2C9 genetic polymorphisms and phenytoin-related severe cutaneous adverse reactions in a Thai population. Pharmacogenet Genomics 26, 225–34 (2016). [DOI] [PubMed] [Google Scholar]
- (27).Chung WH et al. Genetic variants associated with phenytoin-related severe cutaneous adverse reactions. JAMA 312, 525–34 (2014). [DOI] [PubMed] [Google Scholar]
- (28).Karnes JH et al. Applications of Immunopharmacogenomics: Predicting, Preventing, and Understanding Immune-Mediated Adverse Drug Reactions. Annu Rev Pharmacol Toxicol 59, 463–86 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Hung CC et al. Effects of polymorphisms in six candidate genes on phenytoin maintenance therapy in Han Chinese patients. Pharmacogenomics 13, 1339–49 (2012). [DOI] [PubMed] [Google Scholar]
- (30).Hung CC, Lin CJ, Chen CC, Chang CJ & Liou HH Dosage recommendation of phenytoin for patients with epilepsy with different CYP2C9/CYP2C19 polymorphisms. Ther Drug Monit 26, 534–40 (2004). [DOI] [PubMed] [Google Scholar]
- (31).van der Weide J, Steijns LS, van Weelden MJ & de Haan K. The effect of genetic polymorphism of cytochrome P450 CYP2C9 on phenytoin dose requirement. Pharmacogenetics 11, 287–91 (2001). [DOI] [PubMed] [Google Scholar]
- (32).Yip VL, Marson AG, Jorgensen AL, Pirmohamed M. & Alfirevic A. HLA Genotype and Carbamazepine-Induced Cutaneous Adverse Drug Reactions: A Systematic Review. Clin Pharmacol Ther 92, 757–65 (2012). [DOI] [PubMed] [Google Scholar]
- (33).Ihtisham K. et al. Association of cutaneous adverse drug reactions due to antiepileptic drugs with HLA alleles in a North Indian population. Seizure 66, 99–103 (2019). [DOI] [PubMed] [Google Scholar]
- (34).Hershfield MS et al. Clinical Pharmacogenetics Implementation Consortium Guidelines for Human Leukocyte Antigen-B Genotype and Allopurinol Dosing. Clin Pharmacol Ther 93, 153–58 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Mintzer S. et al. Effects of antiepileptic drugs on lipids, homocysteine, and C-reactive protein. Ann Neurol 65, 448–56 (2009). [DOI] [PubMed] [Google Scholar]
- (36).Thorn CF, Whirl-Carrillo M, Leeder JS, Klein TE & Altman RB PharmGKB summary: phenytoin pathway. Pharmacogenet Genomics 22, 466–70 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Bochner F, Hooper WD, Eadie MJ & Tyrer JH Decreased capacity to metabolize diphenylhydantoin in a patient with hypersensitivity to warfarin. Aust N Z J Med 5, 462–6 (1975). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.