Abstract
Air travel during the COVID-19 pandemic is challenging for travellers, airlines, airports, health authorities, and governments. We reviewed multiple aspects of COVID peri-pandemic air travel, including data on traveller numbers, peri-flight prevention, and testing recommendations and in-flight SARS-CoV-2 transmission, photo-epidemiology of mask use, the pausing of air travel to mass gathering events, and quarantine measures and their effectiveness.
Flights are reduced by 43% compared to 2019. Hygiene measures, mask use, and distancing are effective, while temperature screening has been shown to be unreliable. Although the risk of in-flight transmission is considered to be very low, estimated at one case per 27 million travellers, confirmed in-flight cases have been published. Some models exist and predict minimal risk but fail to consider human behavior and airline procedures variations. Despite aircraft high-efficiency filtering, there is some evidence that passengers within two rows of an index case are at higher risk. Air travel to mass gatherings should be avoided. Antigen testing is useful but impaired by time lag to results. Widespread application of solutions such as saliva-based, rapid testing or even detection with the help of “sniffer dogs” might be the way forward. The “traffic light system” for traveling, recently introduced by the Council of the European Union is a first step towards normalization of air travel. Quarantine of travellers may delay introduction or re-introduction of the virus, or may delay the peak of transmission, but the effect is small and there is limited evidence. New protocols detailing on-arrival, rapid testing and tracing are indicated to ensure that restricted movement is pragmatically implemented. Guidelines from airlines are non-transparent. Most airlines disinfect their flights and enforce wearing masks and social distancing to a certain degree. A layered approach of non-pharmaceutical interventions, screening and testing procedures, implementation and adherence to distancing, hygiene measures and mask use at airports, in-flight and throughout the entire journey together with pragmatic post-flight testing and tracing are all effective measures that can be implemented.
Ongoing research and systematic review are indicated to provide evidence on the utility of preventive measures and to help answer the question “is it safe to fly?“.
Keywords: COVID19, Inflight transmission, Flying, Safety measures
1. Introduction
COVID-19 has changed traveller numbers, destinations and flight patterns and the situation remains in constant flux. Travellers must comply with protective measures as considered appropriate by the country of departure, the country of arrival and the transporter, in particular airlines. There is confusion with regard to the risk of transmission of SARS-CoV-2. On one hand there is the risk of infection in-flight or at airports, which airlines address with measures such as the use of filters, monitoring and testing of passengers. On the other hand, governments try to limit the risk of transporting infectious passengers from abroad or within a country with measures such as travel bans and quarantines.
Despite large numbers of studies, there is still only scant evidence evaluating protective measures for air travel or indeed for everyday life. How useful are masks, hand sanitisers, thermo screening, pre-flight testing, seat distancing and air filtration systems respectively? Which measures are scientifically proven to have a benefit, and which are merely there to show that an effort is being made? There is a lack of unanimity throughout the world with respect to the definition of risk areas and thresholds for restricted travel as well as to the necessity, effectiveness, duration and implementation of quarantine measures. Airlines are struggling to be compliant with COVID-19 prevention guidelines while somehow retaining at least partial flight services. Travellers are struggling with the decision “Should I stay, or should I go?“. This narrative review aims to assess the status quo of air travel measures in the context of COVID-19 as of October 2020 and to examine their scientific basis if appropriate.
2. Methods
As a group, we divided up topics related to air-travel in the pandemic period and did a rapid narrative review on each of the assigned sub-topics. For identification of relevant publications, a standardized search strategy was used. The PubMed, Scopus and Web of Sciences databases were searched by using the search terms “In-flight”, “flight”, “transmission”; “SARS-CoV-2″, “airborne”, “respiratory”, “aviation”, “COVID”, “COVID-19”, “Corona”, “aircraft” in various combinations with the terms “cabin”, “transmission”, “social distancing”, “quarantine” and testing”. Additionally, cited publications in the original hits were screened and included if relevant, with no restrictions on language and years. IATA, flightradar24 and Forwardkeys were sources of information on air transport volumes. We checked official websites, did an airline survey by email or contacted airlines via social media to evaluate pre-flight and in-flight measures/precautions/recommendations adapted by airlines.
3. Results
3.1. Travel numbers
Air travel numbers have significantly declined. The International Air Transport Association (IATA) reported worldwide passenger departures totalling 4.5 billion on 39 million scheduled flights in 2019 (117 per flight on average). Revenue Passenger Kilometers (RPKs) flown were 8.7 trillion in 2019 (with 1911 km per departure on average).
For 2020 IATA foresees a substantial reduction in numbers, with passenger departures projected at 2.2 billion (−51.6%), flights at 23 million (−40.6%) and RPKs at 3.9 trillion (−54.7%) (with 1749 km per passenger on average) [1], [Table 1 ]. Data refers to international flights (between countries and territories) as well as domestic flights (within countries and territories). Based on mode of transport, 58% of international overnight visitors reached their destination by air in 2018 according to the World Tourism Organization (UNWTO) [2]. As for international travel, the vast majority of flights are within the same world region, rather than flights between regions.
Table 1.
IATA, worldwide airline industry.
| unit |
2019 |
2020 |
% change | |
|---|---|---|---|---|
| real | projection | |||
| Aircraft fleet | 29,697 | 20,261 | −31.8 | |
| Scheduled flights | million | 38.9 | 23.1 | −40.6 |
| - flights per aircraft | 598 | 355 | −40.6 | |
| Passenger departures* | billion | 4.5 | 2.2 | −50.6 |
| - passengers per flight | 117 | 97 | −16.7 | |
| Revenue Passenger Kilometers (RPKs) | billion km | 8680 | 3929 | −54.7 |
| - average distance per passenger | km | 1911 | 1749 | −8.4 |
| Unique city pairs | 21,187 | 16,102 | −24.0 | |
| Passenger load factor | % | 82.5 | 62.7 | −19.8 |
Source: compiled from International Air Transport Association (IATA) Airline Industry Economic Performance - June 2020 – Report & Data tables https://www.iata.org/en/publications/economics/?Search=&EconomicsL1=149&EconomicsL2=150 * Departures refer to legs flown, so # of round trips is half for direct flights, and a third or less for indirect flights.
Domestic air travel is rather concentrated in the large populous countries such as the US, China, India, Indonesia, Japan and Russian Federation Brazil.
Commercial flights (including cargo, but excluding private flights, some business jet flights, most helicopter, ambulance, military and drone flights) are tracked flights in virtual real-time by Flightradar24 and offer insight in flight evolution over time. The year 2020 started with growth in January in commercial flights. In February there was a moderate decrease because of the disruption of traffic within and to/from China. With the lockdowns increasingly being installed in many countries, flights were 55% down in the final week of March 2020 compared to the same period of 2019 [3]. In April 2020, flights were 74% below the same month in 2019, but showed early signs of a turning point at the very end of the month [4]. This slow recovery continued with flights down 71% in May [5], 62% in June [6], 50% in July [7], 45% in August [8], 43% in September and 42% in October 2020 [9]. At the height of the pandemic, a majority of countries closed borders for inbound and/or outbound travel with traffic limited to repatriation of travellers and essential travel, or sometimes for all travel. In some cases, mandatory quarantine was ordered. Rising numbers at the end of August and throughout September have seen European countries adapt recommendations and restrictions with changes being implemented at short notice. At the start of October, at the time of writing, a second wave of COVID-19 is moving through Europe necessitating multiple travel restrictions.
Domestic travel has been overall less restricted. The travel analytics company, Forwardkeys, based on its latest analysis, expects domestic air travel in China to have fully recovered by the start of September 2020. This is highly significant, because it is the first time, since the start of the COVID-19 outbreak, that a major segment of the aviation market, anywhere in the world, has returned to pre-pandemic levels [10].
The most resilient travel flows and the projected quickest to recover include the following [10]:
-
•
Nearby destinations, domestic or neighboring countries
-
•
Late bookings and private transport
-
•
Visiting family, friends and relatives (VFR)
-
•
Essential business travel, such as visiting clients, and providers. Meetings on the other hand are predicted to be held virtually when at all possible.
3.2. Quarantine measures and travel bans
COVID-19 has changed how we travel; travel advisories and travel bans as well as quarantine or self-isolation when entering a country are now commonplace. For the international traveller, the variable and broad border measures now mean that they not only need to consider disease risk, but also need to take into account the need for quarantine at their destination, on their return, or both. Travel restrictions and quarantine are often the first response against emerging infectious disease threats [11]. They are used as public health tools to combat the international spread of COVID-19, although their utility is yet to be determined. The rationale for the implementation of quarantine is complex, based on a combination of factors such as economy, political agenda, and changing knowledge and epidemiology. Differing national and international guidance, evolving evidence, and the potential for recommendations to change rapidly make travel a lot more complex [Table 2 ].
Table 2.
Some Factors that may be considered when making quarantine decisions.
| 1.Disease specific factors |
|---|
| Incubation period, reproduction number, extent of asymptomatic and pre-symptomatic transmission, severity of illness, population level immunity |
| Knowledge of key characteristics of infection |
| Availability of vaccine or effective treatment |
| 2.Epidemiology |
| Worldwide epidemiology |
| Rates of infection in receiving country |
| 3.Travel patterns |
| 4. Healthcare factors |
| Effectiveness of non-pharmaceutical control measures |
| Resilience during a crisis |
| Availability of prompt and efficient testing and contact tracing |
| Capacity of healthcare systems |
| 5.Legal and ethical considerations, likelihood of compliance |
| 6.Economic and logistic factors |
3.3. Travel advisories and bans
International travel advisories have been introduced, but where is the evidence that such bans are effective? While the direct effect of such advisories is difficult to quantify, travel advisories during the SARS epidemic in 2003 did result in a significant reduction in travel, but these were considered to be too late and too small to influence the global spread of SARS had there not been such effective control of the epidemics within affected areas [12].
Similarly, travel bans have been introduced in response to other emerging infectious disease threats, but the evidence relating to their impact has been inconsistent [13]. An analysis of the 2009 H1N1 pandemic showed that the decline in air travel to and from Mexico was too small to have an impact, and stricter restrictions would have led to delays of about two weeks even with early intervention [14]. Border closure were, however, shown to be effective in controlling the 1918–19 influenza pandemic in various Pacific islands [15], and theoretically might be helpful in small island nations with low traveller numbers [16], but a systematic review of the effectiveness of travel restrictions in containing the spread of influenza showed that in general, travel restrictions had only limited effect, and the degree of impact was dependant on multiple factors ranging from the extent and timing of the restrictions, the epidemic size, to virus transmissibility and travel patterns.
The review concluded that only extensive travel restrictions had any meaningful effect on reducing the magnitude of epidemics, and on their own, might delay the spread and peak of pandemics by a few weeks or months but the evidence for containment of influenza within a defined geographical area was lacking [17].
In the case of COVID-19, the evidence reveals a similar picture; some research has indicated a negligible effect of travel bans [18], and other studies have suggested a delay in disease spread and case numbers, albeit with a recognition that complete travel bans are unlikely to be sustainable in the longer term [19,20]. Yet, the current situation and patchwork of bans and quarantine measures is unprecedented in scale.
3.4. Quarantine recommendations, their usefulness and risks
Quarantine (the restriction of asymptomatic healthy people who may have had exposure to an infectious disease) after travel is one of the oldest, public health tools known. Adopted widely in the fourteenth century to stop the spread of plague, quarantine has subsequently been used with varying degrees of success following international travel.
Following the 2003 SARS outbreak, an assortment of quarantine approaches was used in five severely affected countries/regions. While measures were highly effective in reducing onward transmission of SARS by containment of imported cases on arrival, implementation of quarantine was resource intensive, involved coordination of multiple sectors of society, frequently required new legislative actions or authorities, and was highly dependent on effective communication [21,22].
In the context of COVID-19, a Cochrane review found that quarantine is important in reducing incidence and mortality, and early implementation combined with other public health measures is important to ensure effectiveness. They also concluded that the quarantine of travellers from a country with a declared outbreak may delay its introduction or re-introduction, or may delay the peak of transmission, or both, but the effect was small, and their confidence in the results was low or very low due to the limitations in the evidence available [23].
As of 3rd September, an estimated 156 countries or territories have introduced some form of traveller quarantine measures [24], and in the absence of any international consensus this means that approaches to quarantine and how it is implemented (voluntary/mandated, home/government facility, individual/group etc) will vary from country to country; likely based on a combination of factors, including epidemiology, culture, local context, economic imperatives and political factors. However, any decision to introduce quarantine measures is not without risk, requires adequate resourcing, and needs to account for the potential negative effects, which are increasingly being reported [25].
As of October 9th, the Council of the European Union introduced a “traffic light system” based on infection rate per 100′000 people. The European Centre for Disease Prevention and Control (ECDC) will publish a map weekly categorizing EU regions into different zones for which different rules will apply. This is being complicated by countries being able to additionally set their own rules. A common testing regime has still not been set out making the framework difficult to work and further adding uncertainty to travel as nations are only required to provide information on new restrictions 24 h before enforcement [26].
3.5. Pre-flight passenger screening
COVID-19 has led to unprecedented lockdowns and reduction of air travel globally, fuelled by fear of trans-border introduction of the virus and onboard transmissions. The fear is not ungrounded as past instances with SARS-COV have shown that superspreader events can lead to hundreds of new infections. Transmission mainly occurs in the symptomatic phase of the illness [27,28]. However, many infections in SARS-CoV-2 are also associated with contact to asymptomatic or presymptomatic patients [29,30].
In essence, flying will be safer and superspreading events diminished by optimizing screening procedures, minimizing the risk of allowing pre- or asymptomatic patients to board, and consequent implementation and adherence to simple hygiene measures that prevent the spread of diseases.
Various strategies have been introduced to detect SARS-CoV-2 carriers including temperature screening, which is currently advised by IATA [31]. A recent paper has shown the lack of utility of temperature screening in the identification of young infected persons. Another option is demanding negative PCR tests before letting passengers board, a strategy Swiss Airlines is partly pursuing by allowing mask free travel with a medical certificate and a negative PCR test [32]. Certain destination countries also require a negative PCR test at point of entry [33].
Simple measures, such as allowing only passengers to enter airports, regular disinfection of surfaces, and mandatory PPE for staff and handing out packs containing disinfectants and masks, have been introduced at various airports around the world [34].
3.6. Temperature screening
Temperature screenings have been introduced worldwide in an effort to reduce transmissions. The installation of thermoscanners can be quite costly. During the SARS pandemic, Canada spent around 5.7 million dollars on the installation of such scanners, yet failed to detect a single case [35,36]. Initial data speculated that only around 45% of travelers would be detected by temperature screenings [37], recent data suggests that number is much lower, as amongst young people a vast majority never develops fever [38], suggesting that fever measurements are not an adequate screening method for airports.
3.7. COVID-19 tests
There are three main ways to establish infection with SARS-CoV-2; nucleic acid tests to detect the presence of RNA, either via RT-PCR or LAMP. Antigen testing for the presence of a viral antigen, usually a surface protein. Antibody tests to detect prior infection using ELISA or LFA assays.
For diagnostic testing the gold standard currently is naso-/oropharyngeal swabbing with subsequent RT-qPCR analysis. The sensitivity varies greatly based on who performs the test and how it is being performed (only NP, OP + NP, only OP) in addition to viral RNA concentrations varying across the respiratory tract. A previous study in which both OP and NP specimen were collected in previously SARS-CoV-2 positively confirmed patients showed discordant results in 38% of the cases [39]. Due to the invasive nature of the test, prolonged positivity post recovery and variability of the results based on who performs them this makes it a poor tool for screening.
The immune response against SARS-CoV-2 does not reflect infectivity of the individual, especially since in most cases the immediate IgM response is absent or not measurable [40]., In addition commercial ELISA kits are costly and LFA assays lack the required sensitivity making them poor candidates for screening purposes.
The most promising candidates are thus antigen based testing and saliva tests.
Saliva tests have a similar sensitivity to PCR tests of 91% [41], and most importantly are non-invasive and can be considered for self-testing. Colorimetric tests such as New England Biolabs tests seem especially promising as they allow testing with minimal amounts of equipment and results can be obtained within half an hour. Antigen tests such as Abbotts Rapid test are another option, as they provide immediate results and have a very high specificity. However, they still rely on nasopharyngeal swabbing [42] and have faced scrutiny in the past over low sensitivity of their tests [43].
Recently, Finland and other countries are training dogs to detect SARS-CoV-2 positive patients. In a pilot study by Jendrny et al. tracheobronchial secretions and saliva were collected from positive hospitalized patients. The study was double blinded (dog, handler and observer) and the dogs were able to find positive samples with a sensitivity of 82% and specificity of 96.5% - most notably there was no significant difference between saliva and tracheal secretions (85% vs 87% hitrates). While the specificity of rapid COVID-19 Antigen tests is higher (99.5%), the sensitivity of dogs is much superior to those of antigen based tests (56.2%) [44,45]. A limitation of the study is that only samples from hospitalized patients were used. A follow up study with samples from different time points of a patient is needed since especially pre-/asymptomatic patients’ samples are of interest. Nonetheless certain airports, such as the one in Helsinki [46] have already started using dogs to detect SARS-CoV-2 in travelers with satisfying results and a “sensitivity of almost 100%“.
As of October 10th, more than 90 countries require arriving air passengers to be in possession of a negative COVID-19 PCR result from a test taken within a prescribed number of days prior to arriving in the respective country. The usefulness of this measure needs evaluation. More than 30 additional countries require a negative COVID-19 PCR test result to be exempt from quarantine or other restrictions. Although antigen testing may be more readily available, only PCR test results are accepted by these countries. More than 60 countries require COVID-19 testing upon arrival in the respective country, some regardless of whether the traveller already had a negative COVID-19 test result prior to arrival [47].
3.8. Physical distancing on planes, use of masks, hand sanitisation and air filtration systems
In recent time, transmission of COVID-19 during airplane travel has gained enormous importance for re-establishing worldwide travel activities. Since air travellers spend extended periods in enclosed spaces where physical distancing is difficult or impossible, there is a theoretical risk of spread of infectious diseases during the flight. Although there is sparse knowledge on COVID-19, recent evidence is available for other (SARS-like) viruses and their dissemination during airplane travel. However, comparisons are difficult to make since the kinetics of viruses are different due to their size, aerosol-linked movement in the aircraft cabin as well as their infectivity. Recent studies in previous years have focused on other infectious diseases such as the Zika virus [48], yellow fever [49], the influenza virus [50,51], Ebola [52], SARS [27,53], and others [54] but differences with COVID-19 precludes firm conclusions.
3.9. Aircraft cabin
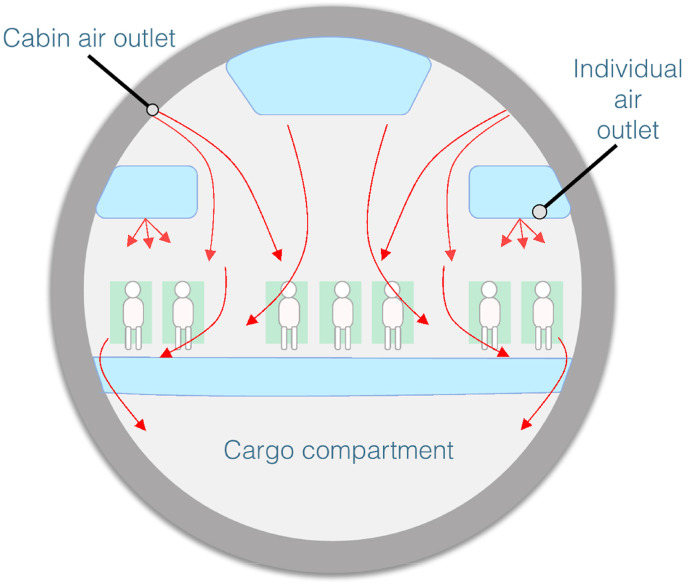
The cabin of a typical aircrafts [Fig. 1 ] is usually provided with a high airflow of many cubic meters per minute, which replaces the air onboard the cabin every two to 3 minutes. Air filtration in various implementations has become a critical intervention in managing the spread of COVID-19. Recent evidence has shown that severe acute respiratory syndrome (SARS-CoV-2) can remain airborne longer and travel farther than anticipated earlier in the COVID-19 pandemic, and high-efficiency particulate Air/Arrestance (HEPA) filters have been recommended [55]. In a typical aircraft, the recirculated air is passed through HEPA filters, which are required to remove over 99.97% of particles characterized by aero-diameter of 0.3 μm or larger [56]. In practice, however, they were found just as efficient at 0.01 μm, which is much smaller than the 0.125 μm size of the virus that causes COVID-19 [56,57]. Altogether, high airflow and use of HEPA filters onboard planes make it unlikely to catch the virus from someone who is not in the immediate vicinity.
Fig. 1.
Sample airflow, A320.
3.10. Social distancing, hygienic procedures and inflight transmission
Social distancing during the whole time at an airport as well as during boarding, sitting and de-boarding of the aircraft is of utmost importance to prevent the spread of SARS-CoV-2. Whereas the in-flight transmission of symptomatic COVID-19 patients is comparatively easy to identify due to clinical symptoms and is an established screening procedure [58,59], the evidence for the transmission of the virus from asymptomatic passengers on an aircraft is inconclusive. Only sparse data are available yet [60].
In-flight transmission has been long-standing described for multiple infectious agents, especially bacterial and viral respiratory pathogens [61], such as tuberculosis [[62], [63], [64]], influenza [65,66], measles [67], and coronaviruses, such as the Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) [27,61,[68], [69], [70], [71], [72]].
During a flight from Singapore to Hangzhou International Airport in Zhejiang, China, in January 2020, a commercial aircraft carrying 335 passengers and crew members, 16 patients, not using face masks, were exposed and infected with SARS-CoV-2. The median age of those infected was 37 years, and no fatal outcomes were reported in these series, although 10 of these cases were symptomatic [73].
Two more instances of inflight transmissions were reported. One during a domestic flight between Sydney and Perth with 11 infectious cases during the flight. 6 were seated mid cabin and 5 aft cabin. They noticed a significantly greater risk of transmission in secondary infections in mid cabin vs aft cabin seats (11/112 vs 0/101 passengers) as well as window seats 7/28 vs non-window seats (4/83) [74].
The second flight was a long haul flight between London Heathrow, and Hanoi during which one primary case seated in business class led to 15 secondary infections. 12/15 passengers were seated in business class, 3/15 in economy class. The authors concluded that seating proximity (<2 seats away) was associated with the highest risk of transmission [75].
Preliminary data from the U.S. Department of Defense using Boeing 777–200 and 767–300 air frames was released to shed light on aerosol behavior and virus reduction during a flight using mannequins. The study showed a minimum 99.7% reduction of virus aerosols. The authors concluded that the infection risk is thus 1 infection per 54 h of flight and zero infections during a 12-h flight. This contrasts the cases we described in this article in which several instances of inflight transmissions are reported. While the risk of transmission is probably low, such models are based on sitting mannequins and do not take into account human interactions, differences in airflow throughout the flight, possible infections during boarding or deboarding or even differences in seating arrangements during which infection risk also seems to differ. Further studies are necessary to evaluate elements in human behavior and heightened infection risk, as well as particularities and differences in airline safety protocols which could account for the differences in infection observed between flights [Table 3 ].
Table 3.
Published cases of inflight transmission of COVID-19 with known index cases.
| Scientifically confirmed cases of inflight transmission of COVID-19 | Infectious passengers | Secondary cases | From - > To | Date | Flight length | Article | Comment |
|---|---|---|---|---|---|---|---|
| 1 | 11 | 11 | Perth - > Sydney | March 2020 | 4 h 10 min | Speake et al. [74] | |
| 2 | 1 | 15 | London - > Hanoi | March 2020 | 12 h | Khanh et al. [75] | |
| 3 | 2 | 0 | China - > Greece | January 2020 | 10 h | Schwartz et al. [94] | |
| 4 | 6 (asymptomatic) | 1 | Italy - > South Korea | March 2020 | 10 h | Hwan be et al. [79] | Was wearing mask, transmission most likely in toilet |
| 5 | 7 | 2 | Tel Aviv - > Frankfurt | March 2020 | 4 h 40 min | Hoehl et al. [68] | |
| 6 | 2 | 5 | Israel - > Athens | March 2020 | 2 h | Pavli et al. [95] | |
| 7 | 3 | 6 | Wuhan - > Singapore | January 2020 | 10 h | Zhang et al. [96] | |
| 8 | ? | 2 | Bangui - > Paris | March 2020 | 7 h | Eldin et al. [97] |
As a consequence of the risk, the recommendation of face masks on board has been extended internationally during this period of transition from the pandemic to the peri-pandemic era. In a study of the repatriation of Israeli citizens from Japan, who had been passengers on the Diamond Princess cruise ship, no case of in-flight transmission of SARS-CoV-2 in the 14-h flight was shown, likely due to use of face masks on board [76].
The risk of transmission of droplet-mediated infections on an aircraft depends on proximity to an index case and on other factors, such as movement of passengers and crew, fomites, and contact among passengers in the departure gate [68,77].
Considering the difficulty of airborne infection transmission in-flight because of HEPA filters used in aircraft ventilation systems, contact with contaminated surfaces or infected persons when boarding, moving, or disembarking from the aircraft may play a critical role in inflight transmission of infectious diseases [27,61]. Whilst seated, Hoehl et al. characterized high risk only passengers seated within two rows of an index case [68].
Real-world data bodes well for flying too. Worldwide, there have been a few reports of individual transmissions linked to flights, but no superspreading-type events. Australia, through its exhaustive contact tracing system, did not identify any case of on-board transmission, even for people who travelled whilst contagious [78]. Bae and colleagues analysed 310 passengers who boarded an evacuation flight from Milan, Italy, to South Korea. N95 respirators were provided, and passengers were kept 2 m apart for physical/social distancing before boarding. After an 11-h flight, 299 asymptomatic passengers arrived in South Korea and were immediately quarantined for 2 weeks [79]. Only one passenger became infected after the flight [79].
Barnett estimated the risk of catching the virus during a full 2-h flight to be around 1 in 4300. The risk drops to 1 in 7700 if airlines leave the middle seat empty [80]. This is further confirmed by recent data suggesting that following strict measures with the risk of infection with SARS-CoV-2 on flights remains extremely low (44 transmissions in 1.2 billion travellers). Even when taking underreporting into account, those figures are very promising.
The International Air Transport Association (IATA) supported wearing of face coverings for passengers and crew while on board aircraft, but did not support mandating social distancing measures that would leave ‘middle seats’ empty, based mainly on an economical argument. Airlines for Europe (A4E) stated that „leaving middle seats free (…) is not viable for the air transport industry given it would reduce the maximum number of passengers onboard to between 50 and 66% of aircraft capacity. Due to high operating and other fixed costs, airlines require planes to be at least 77% full in order to “break even.“
The odds of dying of a case contracted in flight are estimated at between 1 in 400,000 to 1 in 600,000 depending on age and risk factors, which is comparable to the risk for a standard 2-hour exposure on the ground [80]. Finally, the risk of infection is also increased during travel to and from the airport, as public transportation and ridesharing can increase the risk of getting exposed to the virus [81].
3.11. Mass gatherings
Mass gatherings (MGs) are watched cautiously by public health experts because of its three important public health implications [82]. First, MG related adverse health events and medical emergencies can compromise the public health response capacity of the host country. Second, MGs can accelerate disease outbreaks to epidemic levels in the host country. Third, MG related travel can accelerate the global seeding of pathogens with epidemic potential and may cause silent or explosive outbreaks globally. Air travel is particularly implied as a risk factor for the 2nd and 3rd outcome, and most notably for the 3rd.
Increasing access to air travel is the most critical enabler of international mass gatherings such as the Hajj and the Olympics Games. However, air travel is also becoming increasingly relevant for other mostly domestic or regional MGs such as the Khumb Mela in India, Arbaeen in Iraq, and the Shiite pilgrimage to Qom in Iran. About three quarters of Olympics participants and Hajj pilgrims use air travel to reach their MG destination [82,83]. It was in light of this fact that following the World Health Organization declaration of a public health emergency of international significance (PHEIC) on COVID-19, the authors advocated for the suspension of the of the year-around Umrah pilgrimage in Saudi Arabia, the trend setter for future MG cancellations [82]. Subsequent declaration of COVID-19 as a pandemic strengthened the call for the cancellation of MGs. MGs including the annual international Hajj pilgrimage, the Olympics Games 2020 in Japan, the Miami Beach Arts Fair, California's spring Coachella Valley Music and Arts Festival, and Canada's national music awards (the Junos) have been cancelled or postponed.
Due to airborne routes of disease transmission, respiratory diseases are the most common and consistent public health risk during mass gatherings [83]. When transmission occurs from innate surfaces and from human secretions, high density occupation in common spaces, high density crowding in event venues, and high frequency use of shared toilet facilities add to the complexity of transmission for both air travel and mass gatherings.
There is no known short-cut to hosting a true mass gathering amid a respiratory disease pandemic of high transmission potential, mortality, and poorly understood natural history such as COVID-19. During such uncertainties, the overwhelming public health recommendation have been to cancel the event [84,85].
Communities that held MG events prior to COVID-19 PHEIC such as the Qom pilgrimage in Iran and a conference in Boston have resulted in extensive COVID-19 transmission [86,87].
Cases also increased to epidemic levels in areas that hosted multiple events as in the State of South Dakota in the USA. The scaled down Hajj 2020 [88] with 1000 domestic pilgrims in Mecca (1200 square kms) do not meet the definition of a mass gathering (an event that strains the planning and response resources of the health system in the community where it takes place) as the downsizing afforded nearly 27 square meters of personal space to each pilgrim in the most potentially crowded pilgrim ritual area, the Grand Mosque.
As mitigation fatigue increases among the population, providers of travel health services will be faced with interest from their patients about participation in fly-in mass gatherings.
Attendance in religious MGs are highly sensitive events to many people and lifelong wishes of many, and interest in religious MGs may be amplified at times of uncertainty such as a pandemic.
However, in the absence of a vaccine or specific pharmaceutical intervention, participation in mass gathering during an active pandemic (with a respiratory virus that sustains among asymptomatic carriers) may not be encouraged. By providing a full list of implications of participation in MGs during respiratory disease pandemics (such as lock down for an extended period of time if exposed, challenges with medical evacuations if ill, the cost of evacuation for a pandemic disease acquired at a mass gathering), providers of travel health services can play an important role to help their patients to make informed decisions about MG attendance.
3.12. Measuring mitigation compliance: photo-epidemiology to measure face covering use
The success of modified air-travel amid a pandemic requires review of traveller compliance with prevention interventions, and ultimately of the utility of such interventions in reducing air-travel related risk of transmission. Participation compliance in individualized surveys or assessments is likely to be suboptimal in travel settings due to privacy issues, time factors, and crowded settings. One innovative epidemiologic surveillance approach has been the use of photo-epidemiology methods were systematically obtained sequential photographs of the crowd and analysed manually or using face recognition systems. Photo-epidemiology has its origins in wildlife surveillance, but Elachola & Ebrahim studied its utility to monitor face mask use for prevention of respiratory viruses and umbrella use for sun protection during the 2009 and 2013 Hajj mass gathering [89,90]. Those reports remain as the first ever reported estimates of face mask and umbrella use during mass gatherings. Elachola and Ebrahim applied this method at airports for the first time early during the COVID-19 outbreak and reported face mask use among travellers observed at airports in Asia, Europe and USA [91]. At the height of COVID -19 lockdowns photo-epidemiology methods were also applied to monitor population face covering use in most frequented venues such as supermarkets [92]. The findings from these two studies generally corresponded to the disparities observed in implementation of face covering advisories, historic population exposure to face covering advisories.
The above experiences underscore the utility of photo-epidemiology to monitor face covering use among travellers. Photo-epidemiology studies can be tailored to specific flights as it can be conducted at departure lounges, arrival gates, and inside the cabin. Thus, photos taken at multiple points of a flight can also ascertain pre-boarding and post embarkation variation in face covering use, all of which affect airborne transmission of SARS-COV-2. While photo-epidemiology helps to address self-report bias of individualized surveys, this method may not be suitable for stratified analysis by age, gender and other characteristics of the surveyed population. Yet, photo-epidemiology remains the only available tool to measure population level prevalence of compliance of face coverings.
3.13. Preparedness for compounding transmission risk and uncertainties to air travellers due to emergencies during pandemic
The crash of the Air India COVID-19 related repatriation flight carrying Indian emigrant workers from Dubai to Kozhikode airport on August 7, 2020 underscores how disease transmission risk from air travel could be compounded during pandemics. The 199 persons on board this flight had pre-flight COVID-19 negative tests but were exposed to rescue workers, security and government officials, and volunteers who rushed to the scene at the crash site. Given the COVID-19 status of the formal and informal responders were unknown and the airport was located in a high transmission area designated as ‘hotspot’, all rescued passengers and responders were quarantined and subjected to COVID-19 testing. The entire District Government Office, and airport emergency staff were quarantined, compromising the capacity of government and airport function in addition to adding to the COVID-19 response burden in the airport vicinity.
While the full extent of accident-attributable transmission primary and secondary transmission of SARS-COVI-2 is still being studied, the incident underscores the fragilities of risk aversion during air travel with implications for international assistance. Both airlines and airport management systems should have protocols in place that anticipate and prepare the ground staff for emergencies during pandemics. Plans should assure COVID-19 free status of all airport and responder staff, triage plans, a maintenance pool of vetted volunteers from the community oriented to disease mitigation concepts who could improve emergency response capacity, and surplus personal protection equipment in place. Advisories to travellers should include mention of emergencies including potential quarantine of survivors and such advance warning can help improve travellers’ coping capabilities during an unanticipated crisis.
3.14. Pre- and in-flight measures by airline
The International Air Transport Association sets forth rules for safe flying [93]. The implementation of said rules varies greatly based on the airline. While all airlines enforce masks on the flight, there are many differences in pre-flight and in-flight measures (Table 4 ).
Table 4.
Preflight-Measures of the 20 biggest airlines by size as of October 15th.
| Mask | Negative Testing PCR certificate | Thermoscanners | Hygiene kit | Health Screening for staff | Personnel PPE | Social Distancing when boarding | Systematic Boarding | Rapid tests before boarding | |
|---|---|---|---|---|---|---|---|---|---|
| Swiss Airlines | x | (x) | ? | ? | ? | x | ? | ? | – |
| Emirates | x | – | x | x | ? | X | ? | x | x |
| Turkish Airlines | x | – | x | – | (−) (+) (just temperature) | x | ? | ? | – |
| Air Canada | x | – | x | – | ? | x | x | x | – |
| Lufthansa | x | (x) | x | – | – | - (plexiglass) | x | x | x |
| American Airlines | x | – | ? - | – | – | x | x | – | – |
| British airways | x | – | – | – | – | ? | x | x | – |
| ANA | x | – | x | x | – | x | x | x | – |
| Air France | x | (x) possibility | x | – | – | x | x | x | – |
| Southwest Airlines | x | – | x | (x) wipes | – | x | x | x | – |
| Alaska Airlines | x | (x) possibility | – | – | – | x | x | x | – |
| Ryanair | x | – | self | – | – | (x) limited | (x) encouraged | ? | – |
| Easyjet | x | – | (x) varies | – | – | x | x | x | – |
| Aeroflot | x + gloves + change mask every 3 h | – | x 37° | x | ? | x | x | x | – |
| United | x | – | x | – | – | x | x | x | – |
| Delta Airlines | x | – | x | x | ? | x | x | x | – |
| China Southern Airlines | x | – | x (also during flight) | x | x | x | x | x | – |
| China Eastern Airlines | x | – | x | x | ? | ? | ? | ? | – |
| Air China | x | – | x | x | ? | x | x | x | – |
| IndiGo | x | – | x + health declaration app | x | x | x | x | x | – |
| LATAM Airlines | x | – | – | – | ? | x | x | x | – |
| Avianca | x | – | x | – | – | x | x | x | – |
| Inflight measures of the 20 biggest airlines by size | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mask | Systematic boarding | Social Distancing enforced (empty seats) | Eating allowed? | Drinking allowed? | HEPA Filters? | Inflight disinfection of sanitary facilities? | Pre/Post flight disinfection | Passenger locator card? | Special disembarking? | Reserved isolation seats | |
| Swiss Airlines | x | x | – | x | x | x | – | x | ? | ? | – |
| Emirates | x | x | – | (x) | (x) | x | x | x | ? | ? | – |
| Turkish Airlines | x | x | – | (x) - not at same time | x | x | ? | x | x | x (waiting period) | x |
| Air Canada | x | x | – | (x) prepacked | (x) limited | x | x | x | ? | ? | ? |
| Lufthansa | x | x | – | x | x | x | – | x | – | – | – |
| American Airlines | (x) | – | – | x | x | x | – | x | – | – | – |
| British Airways | x | – | – | x | x | x | – | x | – | x | – |
| ANA | x | x | – | (x) limited | x | x | – | x | ? | ? | – |
| Air France | x | x | x | (x) limited | (x) | x | – | x | ? | ? | – |
| Southwest | x | x | x | (x) limited | x | x | – | x | – | x | – |
| Alaska | x | x | x | (x) limited | x | x | x | x (+ATP testing + cleaning certificates) | ? | x | x |
| Ryanair | x | ? | – | (x) limited | x | x | – | - (once daily) | ? - | ? | – |
| Easyjet | x | x | – | (x) limited | x | x | – | - (once daily) | x | x | – |
| Aeroflot | x + gloves | x | – | (x) limited | x | x + air renewal | x | x | x | x | – |
| United | x | x | – | (x) limited | x | x | – | x | – | x | – |
| Delta | x | x | x | - (own food ok) | – | x | x | x | ? - | x | – |
| China Southern Airlines | x | x | – | (x) prepackaged | x | x | x | x | ? | x | x |
| China Eastern Airlines | x | ? | – | (x) limited | ? | x | x | x | ? | ? | – |
| Air China | x | x | ? | (x) limited | x | x | x (different risk levels, up to hourly) | x | ? | ? | ? |
| IndiGo | x | x | – | x | x | x | – | x | x | x | – |
| LATAM Airlines | x | x | – | x | x | x | – | – | – | x | – |
| Avianca | x | x | – | x prepackaged | x | x | ? | – | – | – | – |
Information on measures taken by airlines can be very difficult to find. With some airlines such as Emirates or Air China, all information is transparently visible on their webpage making it easy for the traveller to comprehend what is awaiting him at the airport or during the flight. Others, unfortunately display the information in a very chaotic way, or are very vague about the measures they are taking, or do not display the measures at all and are also reluctant to provide concise answers when contacted.
There are significant differences in pre-flight measures of airlines. Some, like the Lufthansa group or Emirates encourage or enforce pre-flight testing for their passengers. GoIndiGo on the other hand created an app that requires passengers to complete e questionnaires on their health status multiple times before the flight, which is essentially a telemedicine application.
Most airlines disinfect their plane before and after every flight. Some, like Aeroflot or the Emirates also disinfect sanitary facilities inflight during long flights. Air China varies the frequency based on an internal risk evaluation. Others, like Easyjet or Ryanair only seem to disinfect their flights once a day, claiming that this suffices for a full 24 h.
A vast majority of airlines have reduced the food they are serving to prepackaged food or own food only. Turkish Airlines has a shift-based eating system only allowing certain groups of passengers to eat at once. All airlines seem to allow drinking during the flight, and all airlines enforce wearing a mask, or in the case of Aeroflot also gloves inflight.
All airlines we looked at are using HEPA filters. Some, like Turkish Airlines have especially designated isolation seats in case someone becomes symptomatic inflight.
There was little information available on which airlines use passenger locater forms, with some airlines such as Lufthansa stating openly that it is a data protection issue, and others such as Goindigo making it mandartory via their app.
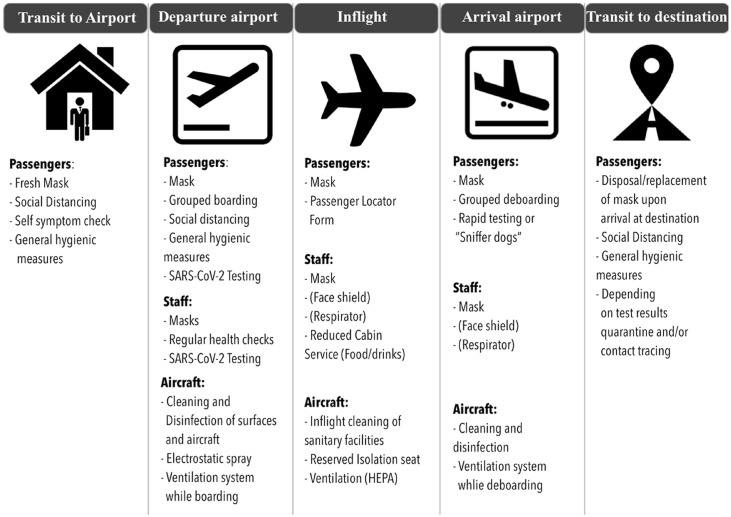
A report [98] report published by Faculty and Scientists at the Harvard T.H. Chan School of Public Health provides a comprehensive and thorough summary on common practices and recommendations concerning SARS-CoV-2 transmission during travel. They propose a layered approach for reduction of SARS-CoV-2 transmission (Education and Awareness; Screening; Physical and Engineering Controls; Process Management, and PPE) by means of NPIs (Non-Pharmaceutical Interventions) and suggests a reduction of risk to minimal levels can be achieved by utilizing standard control measures (social distancing, wearing masks, disinfecting of surfaces, screenings, testing and a strict enforcement of those measures) that are effective in other circumstances. Such an approach can mitigate the transmission risk of SARS-CoV-2 to passengers and crew members. We summarized those findings along with our recommendations in Fig. 2.
Fig. 2.
Mitigation measures × for prevention of SARS-CoV-2 transmission while traveling from home to the end destination.
Also including NPIs: Non-Pharmaceutical Intervention Layering Non-Pharmaceutical Interventions (NPIs) can mitigate risk of SARS-CoV-2 transmission for Passengers and crew members during air travel (figure derived from the report “Assessment of Risks of SARS-CoV-2 Transmission During Air Travel and Non-Pharmaceutical Interventions to Reduce Risk Phase One Report: Gate-to-Gate Travel Onboard Aircraft Prepared by Faculty and Scientists at the Harvard T.H. Chan School of Public Health).
4. Limitations
Our paper is a rapid, narrative review of the status quo (as of October 2020) of air-travel in the pandemic and peri-pandemic period. It is limited because it is not a systematic review and also because of the rapidly evolving numbers of publications that may have an impact on precautions related to air travel and SARS-CoV-2 transmission.
5. Conclusions
In the pandemic and peri-pandemic periods, a substantial reduction in air travel numbers is apparent with a decrease (−51.6%) in passenger departures. Trends show that the most resilient and fastest travel flows for recovery are domestic flights and neighboring country travel, last minute travel, visiting friends and relatives and essential business travel.
Systematic reviews show that in general, travel restrictions have only limited effect in containing infection, and the degree of impact depends on multiple factors ranging from the extent and timing of the restrictions, the epidemic size, to virus transmissibility and travel patterns. Quarantine of travellers from a country with a declared outbreak may delay introduction or re-introduction of the virus, or may delay the peak of transmission, or both, but the effect is small and there are limitations to the evidence available.
Temperature screening is ineffective. A combined approach of telemedicine (i.e. patients have to fill out self-assessment form prior to flight) and facilities at airports performing both systematic rapid tests, possibly a combination of saliva and antigen could be a viable future strategy at airports. Going forward, on arrival based saliva testing might thus be the best way to reduce the number of persons who have to quarantine after arrival. Hand hygiene and physical distancing from the point of entering an airport until leaving an airport as well as continuous face coverings are key elements of preventing SARS-CoV-2 transmission. Despite high air turnaround and high efficiency filtering used in aircrafts, there is some evidence that passengers within two rows of an index case are at higher risk. A retrospective analysis shows, however, that when stringent hygiene measures are enforced inflight, transmission rates of SARS-CoV-2 are likely to be very low, as little as one case per 27 million travellers, even with positive cases aboard. Guidelines from airlines are difficult to research. Most airlines disinfect their flights and enforce wearing masks and social distancing to a certain degree. Information on other precautions are lacking, not transparent and confusing to interpret. A layered approach of non-pharmaceutical interventions (including masks and sanitisers) for the entire journey (, home to airport to final destination) is indicated. While the guidelines set out by IATA are straight forward, a common platform for contact tracing, telemedicine approaches by preflight questionnaires and COVID-19 test results is lacking. What is necessary is a unified front with all stakeholders, further validation of existing rapid tests and an expert committee to systematically evaluate preventive strategies so that recommendations for safe air-travel are evidence based.
Author contributions
PS: concept and design. MB: figures and tables and airline survey. All authors contributed to evidence building and paper writing, review and revisions.
Declaration of competing interest
MB is involved in a start-up that 3-D prints components for virus tests including tests for SARS-CoV-2.
All other authors declare no conflicts of interest.
Footnotes
This article is a reprint of a previously published article. For citation purposes, please use the original publication details; Travel Medicine and Infectious Disease, Volume 39, January–February 2021, 101915.
References
- 1.IATA Economics https://www.iata.org/en/publications/economics/?Search=&EconomicsL1=149&EconomicsL2=150 [cited 6 Sep 2020]. Available.
- 2.International tourism highlights. 2019. https://www.e-unwto.org/doi/epdf/10.18111/9789284421152 Edition. [cited 6 Sep 2020]. Available.
- 3.Petchenik I. Charting the decline in air traffic caused by COVID-19. https://www.flightradar24.com/blog/charting-the-decline-in-air-traffic-caused-by-covid-19/ [cited 6 Sep 2020]. Available.
- 4.Petchenik I. Scraping along the bottom: april air traffic statistics. https://www.flightradar24.com/blog/scraping-along-the-bottom-april-air-traffic-statistics/ [cited 6 Sep 2020]. Available.
- 5.Petchenik I. Aviation's slow recovery: may air traffic statistics. https://www.flightradar24.com/blog/aviations-slow-recovery-may-air-traffic-statistics/ [cited 4 Nov 2020]. Available.
- 6.Petchenik I. Flight activity rises in June, still far below 2019 levels. https://www.flightradar24.com/blog/flight-activity-rises-in-june-still-far-below-2019-levels/ [cited 6 Sep 2020]. Available.
- 7.Petchenik I. Pause or plateau: July marks inflection point in flight traffic recovery. https://www.flightradar24.com/blog/pause-or-plateau-july-marks-inflection-point-in-flight-traffic-recovery/ [cited 4 Nov 2020]. Available.
- 8.Petchenik I. Commercial flight growth slows in August. https://www.flightradar24.com/blog/commercial-flight-growth-slows-in-august/ [cited 4 Nov 2020]. Available.
- 9.Petchenik I. Bumping along: charting October's flight activity. https://www.flightradar24.com/blog/bumping-along-charting-octobers-flight-activity/ [cited 4 Nov 2020]. Available.
- 10.Gonzalez L. Full recovery of domestic air travel in China by September. https://forwardkeys.com/full-recovery-of-domestic-air-travel-in-china-by-september/ 26 Aug 2020 [cited 6 Sep 2020]. Available.
- 11.Worsnop C.Z. Domestic politics and the WHO's International Health Regulations: explaining the use of trade and travel barriers during disease outbreaks. The Review of International Organizations. 2017;12:365–395. doi: 10.1007/s11558-016-9260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hollingsworth T.D., Ferguson N.M., Anderson R.M. Will travel restrictions control the international spread of pandemic influenza? Nat Med. 2006;12:497–499. doi: 10.1038/nm0506-497. [DOI] [PubMed] [Google Scholar]
- 13.Errett PhD N., Lauren M., Sauer M.S., Phd Lainie Rutkow. An integrative review of the limited evidence on international travel bans as an emerging infectious disease disaster control measure. Journal of Emergency Management. 2020;18:7–14. doi: 10.5055/jem.2020.0446. [DOI] [PubMed] [Google Scholar]
- 14.Bajardi P., Poletto C., Ramasco J.J., Tizzoni M., Colizza V., Vespignani A. Human mobility networks, travel restrictions, and the global spread of 2009 H1N1 pandemic. PloS One. 2011;6 doi: 10.1371/journal.pone.0016591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McLeod M.A., Baker M., Wilson N., Kelly H., Kiedrzynski T., Kool J.L. Protective effect of maritime quarantine in South Pacific jurisdictions, 1918-19 influenza pandemic. Emerg Infect Dis. 2008;14:468–470. doi: 10.3201/eid1403.07-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eichner M., Schwehm M., Wilson N., Baker M.G. Small islands and pandemic influenza: potential benefits and limitations of travel volume reduction as a border control measure. BMC Infect Dis. 2009;9:160. doi: 10.1186/1471-2334-9-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mateus A.L.P., Otete H.E., Beck C.R., Dolan G.P., Nguyen-Van-Tam J.S. Effectiveness of travel restrictions in the rapid containment of human influenza: a systematic review. Bull World Health Organ. 2014;92:868–880D. doi: 10.2471/BLT.14.135590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Costantino V., Heslop D.J., MacIntyre C.R. The effectiveness of full and partial travel bans against COVID-19 spread in Australia for travellers from China. medRxiv. 2020;2020 doi: 10.1093/jtm/taaa081. 03.09.20032045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee K., Worsnop C.Z., Grépin K.A., Kamradt-Scott A. Global coordination on cross-border travel and trade measures crucial to COVID-19 response. Lancet. 2020;395:1593–1595. doi: 10.1016/S0140-6736(20)31032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cetron M., Simone P. Battling 21st-century scourges with a 14th-century toolbox. Emerg Infect Dis. 2004;10:2053–2054. doi: 10.3201/eid1011.040797_12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nussbaumer-Streit B., Mayr V., Dobrescu A.I., Chapman A., Persad E., Klerings I. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4:CD013574. doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.COVID-19 government public health mitigation measures. https://www.iata.org/en/programs/covid-19-resources-guidelines/covid-gov-mitigation/ [cited 6 Sep 2020]. Available.
- 25.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European concil flying. https://data.consilium.europa.eu/doc/document/ST-11689-2020-INIT/en/pdf Available.
- 27.Olsen S.J., Chang H.-L., Cheung T.Y.-Y., Tang A.F.-Y., Fisk T.L., Ooi S.P.-L. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349:2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 28.Al-Tawfiq J.A., Rodriguez-Morales A.J. Super-spreading events and contribution to transmission of MERS, SARS, and SARS-CoV-2 (COVID-19) J Hosp Infect. 2020;105:111–112. doi: 10.1016/j.jhin.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bielecki M., Züst R., Siegrist D., Meyerhofer D., Crameri G.A.G., Stanga Z.G. Social distancing alters the clinical course of COVID-19 in young adults: a comparative cohort study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buitrago-Garcia D., Egli-Gany D., Counotte M.J., Hossmann S., Imeri H., Ipekci A.M. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guidance E. Temperature screening: a public health responsibility. https://www.iata.org/contentassets/67e015cf3db1410392cd5b5bb5961a16/iata-temperature-screening-public-health-responsibility.pdf Available.
- 32.SWISS travel briefing. https://www.swiss.com/de/EN/various/travel-briefing [cited 31 Aug 2020]. Available.
- 33.Covid-19 PCR test. https://privateharleystreetclinic.com/pages/current-requirements-to-travel-to-certain-countries [cited 20 Oct 2020]. Available.
- 34.Air travel remains a safe way to travel during COVID-19; advanced HEPA filters constantly clean the air onboard, limiting the risk of virus transmission and providing a safe environment – airlines for Europe. https://a4e.eu/publications/air-travel-remains-a-safe-way-to-travel-during-covid-19-advanced-hepa-filters-constantly-clean-the-air-onboard-limiting-the-risk-of-virus-transmission-and-providing-a-safe-environment/ [cited 15 Oct 2020]. Available.
- 35.Why airport screening won't stop the spread of coronavirus. 6 Mar 2020. https://www.sciencemag.org/news/2020/03/why-airport-screening-wont-stop-spread-coronavirus [cited 1 Sep 2020]. Available.
- 36.Mouchtouri V.A., Christoforidou E.P., An der Heiden M., Menel Lemos C., Fanos M., Rexroth U. Exit and entry screening practices for infectious diseases among travelers at points of entry: looking for evidence on public health impact. Int J Environ Res Publ Health. 2019;16 doi: 10.3390/ijerph16234638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quilty B.J., Clifford S., Flasche S., Eggo R.M., CMMID nCoV working group Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV) Euro Surveill. 2020:25. doi: 10.2807/1560-7917.ES.2020.25.5.2000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bielecki M., Crameri G.A.G., Schlagenhauf P., Buehrer T.W., Deuel J.W. Body temperature screening to identify SARS-CoV-2 infected young adult travellers is ineffective. Trav Med Infect Dis. 2020;37:101832. doi: 10.1016/j.tmaid.2020.101832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.COVID-19 Investigation Team Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. 2020;26:861–868. doi: 10.1038/s41591-020-0877-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Immune responses and immunity to SARS-CoV-2. https://www.ecdc.europa.eu/en/covid-19/latest-evidence/immune-responses [cited 2 Sep 2020]. Available.
- 41.Diagnostic testing and screening for SARS-CoV-2. In: European Centre for disease prevention and control. https://www.ecdc.europa.eu/en/covid-19/latest-evidence/diagnostic-testing [Internet]. [cited 22 Jul 2020]. Available.
- 42.CDC Interim guidance for rapid antigen testing for SARS-CoV-2. https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html 29 Aug 2020 [cited 2 Sep 2020]. Available.
- 43.Mahase E. Covid-19: two antibody tests are “highly specific” but vary in sensitivity, evaluations find. BMJ. 2020;369:m2066. doi: 10.1136/bmj.m2066. [DOI] [PubMed] [Google Scholar]
- 44.How accurate are rapid tests, performed during a health-care visit (point-of-care), for diagnosing COVID-19? [cited 20 Oct 2020]. doi:10.1002/14651858.CD013705.
- 45.Grandjean D., Sarkis R., Tourtier J.-P., Julien-Lecocq C., Benard A., Roger V. 2020. Detection dogs as a help in the detection of COVID-19 Can the dog alert on COVID-19 positive persons by sniffing axillary sweat samples ? Proof-of-concept study. 2020.06.03.132134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.This airport is using dogs to detect passengers infected with coronavirus. https://www.weforum.org/agenda/2020/09/dogs-coronavirus-covid-19-aviation-flying-finland-helsinki-airport/ [cited 20 Oct 2020]. Available.
- 47.COVID-19 country specific information. https://travel.state.gov/content/travel/en/traveladvisories/COVID-19-Country-Specific-Information.html [cited 20 Oct 2020]. Available.
- 48.Luo X.S., Imai N., Dorigatti I. Quantifying the risk of Zika virus spread in Asia during the 2015-16 epidemic in Latin America and the Caribbean: a modeling study. Trav Med Infect Dis. 2020;33:101562. doi: 10.1016/j.tmaid.2020.101562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shearer F.M., Longbottom J., Browne A.J., Pigott D.M., Brady O.J., Kraemer M.U.G. Existing and potential infection risk zones of yellow fever worldwide: a modelling analysis. Lancet Glob Health. 2018;6:e270–e278. doi: 10.1016/S2214-109X(18)30024-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Balcan D., Hu H., Goncalves B., Bajardi P., Poletto C., Ramasco J.J. Seasonal transmission potential and activity peaks of the new influenza A(H1N1): a Monte Carlo likelihood analysis based on human mobility. BMC Med. 2009;7:45. doi: 10.1186/1741-7015-7-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee J., Choi B.Y., Jung E. Metapopulation model using commuting flow for national spread of the 2009 H1N1 influenza virus in the Republic of Korea. J Theor Biol. 2018;454:320–329. doi: 10.1016/j.jtbi.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 52.Marston B.J., Dokubo E.K., van Steelandt A., Martel L., Williams D., Hersey S. Ebola response impact on public health programs, west africa, 2014-2017. Emerg Infect Dis. 2017;23 doi: 10.3201/eid2313.170727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Drake J.M., Chew S.K., Ma S. Societal learning in epidemics: intervention effectiveness during the 2003 SARS outbreak in Singapore. PloS One. 2006;1 doi: 10.1371/journal.pone.0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Leta S., Beyene T.J., De Clercq E.M., Amenu K., Kraemer M.U.G., Revie C.W. Global risk mapping for major diseases transmitted by Aedes aegypti and Aedes albopictus. Int J Infect Dis. 2018;67:25–35. doi: 10.1016/j.ijid.2017.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nazarenko Y. Air filtration and SARS-CoV-2. Epidemiol Health. 2020;42 doi: 10.4178/epih.e2020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jayaweera M., Perera H., Gunawardana B., Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res. 2020;188:109819. doi: 10.1016/j.envres.2020.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.NASA Technical Reports Server (NTRS) https://ntrs.nasa.gov/citations/20170005166 [cited 6 Sep 2020]. Available.
- 58.Yang N., Shen Y., Shi C., Ma A.H.Y., Zhang X., Jian X. In-flight transmission cluster of COVID-19: a retrospective case series. medRxiv. 2020;2020 doi: 10.1080/23744235.2020.1800814. 03.28.20040097. [DOI] [PubMed] [Google Scholar]
- 59.Ng O.-T., Marimuthu K., Chia P.-Y., Koh V., Chiew C.J., De Wang L. SARS-CoV-2 infection among travelers returning from wuhan, China. N Engl J Med. 2020;382:1476–1478. doi: 10.1056/NEJMc2003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Operational considerations for managing COVID-19 cases/outbreak on board ships. https://www.who.int/publications/i/item/operational-considerations-for-managing-covid-19-cases-outbreak-on-board-ships [cited 6 Sep 2020]. Available.
- 61.Mangili A., Gendreau M.A. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kenyon T.A., Valway S.E., Ihle W.W., Onorato I.M., Castro K.G. Transmission of multidrug-resistant Mycobacterium tuberculosis during a long airplane flight. N Engl J Med. 1996;334:933–938. doi: 10.1056/NEJM199604113341501. [DOI] [PubMed] [Google Scholar]
- 63.Marienau K.J., Cramer E.H., Coleman M.S., Marano N., Cetron M.S. Flight related tuberculosis contact investigations in the United States: comparative risk and economic analysis of alternate protocols. Trav Med Infect Dis. 2014;12:54–62. doi: 10.1016/j.tmaid.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 64.Miller M.A., Valway S., Onorato I.M. Tuberculosis risk after exposure on airplanes. Tuber Lung Dis. 1996;77:414–419. doi: 10.1016/s0962-8479(96)90113-6. [DOI] [PubMed] [Google Scholar]
- 65.Kim J.H., Lee D.-H., Shin S.-S., Kang C., Kim J.S., BY Jun. In-flight transmission of novel influenza A (H1N1) Epidemiol Health. 2010;32 doi: 10.4178/epih/e2010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lei H., Tang J.W., Li Y. Transmission routes of influenza A(H1N1)pdm09: analyses of inflight outbreaks. Epidemiol Infect. 2018;146:1731–1739. doi: 10.1017/S0950268818001772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Beard F., Franklin L., Donohue S., Moran R., Lambert S., Maloney M. Contact tracing of in-flight measles exposures: lessons from an outbreak investigation and case series, Australia. Western Pac Surveill Response J. 2010;2:25–33. doi: 10.5365/WPSAR.2011.2.2.010. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoehl S., Karaca O., Kohmer N., Westhaus S., Graf J., Goetsch U. Assessment of SARS-CoV-2 transmission on an international flight and among a tourist group. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.18044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Flint J., Burton S., Macey J.F., Deeks S.L., Tam T.W., King A. Assessment of in-flight transmission of SARS--results of contact tracing, Canada. Can Comm Dis Rep. 2003;29:105–110. [PubMed] [Google Scholar]
- 70.Lei H., Li Y., Xiao S., Lin C.-H., Norris S.L., Wei D. Routes of transmission of influenza A H1N1, SARS CoV, and norovirus in air cabin: comparative analyses. Indoor Air. 2018;28:394–403. doi: 10.1111/ina.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wilder-Smith A., Leong H.N. A case of in-flight transmission of severe acute respiratory syndrome (SARS): SARS serology positive. J Trav Med. 2004:130. doi: 10.2310/7060.2004.17091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wilder-Smith A., Leong H.N., Villacian J.S. In-flight transmission of severe acute respiratory syndrome (SARS): a case report. J Trav Med. 2003;10:299–300. doi: 10.2310/7060.2003.2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen J., He H., Cheng W., Liu Y., Sun Z., Chai C. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hanghzou, China: an epidemiological investigation. Trav Med Infect Dis. 2020:101816. doi: 10.1016/j.tmaid.2020.101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Speake H., Phillips A., Chong T., Sikazwe C., Levy A., Lang J. Flight-associated transmission of severe acute respiratory syndrome coronavirus 2 corroborated by whole-genome sequencing. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2612.203910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Khanh N.C., Thai P.Q., Quach H.-L., Thi N.-A.H., Dinh P.C., Duong T.N. Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis. 2020;26:2617–2624. doi: 10.3201/eid2611.203299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nir-Paz R., Grotto I., Strolov I., Salmon A., Mandelboim M., Mendelson E. Absence of in-flight transmission of SARS-CoV-2 likely due to use of face masks on board. J Trav Med. 2020 doi: 10.1093/jtm/taaa117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hertzberg V.S., Weiss H., Elon L., Si W., Norris S.L., FlyHealthy Research Team Behaviors, movements, and transmission of droplet-mediated respiratory diseases during transcontinental airline flights. Proc Natl Acad Sci U S A. 2018;115:3623–3627. doi: 10.1073/pnas.1711611115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Other known flights with confirmed cases of COVID-19 - COVID-19 (Coronavirus) https://www.health.nsw.gov.au/Infectious/covid-19/Pages/flights-archive.aspx [cited 6 Sep 2020]. Available.
- 79.Bae S.H., Shin H., Koo H.-Y., Lee S.W., Yang J.M., Yon D.K. Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2611.203353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barnett A. Covid-19 risk among airline passengers: should the middle seat stay empty? medRxiv. 2020 doi: 10.1101/2020.07.02.20143826. [DOI] [Google Scholar]
- 81.CDC Travel during the COVID-19 pandemic. 26 Aug 2020. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html [cited 6 Sep 2020]. Available.
- 82.Ebrahim S.H., Memish Z.A. COVID-19: preparing for superspreader potential among Umrah pilgrims to Saudi Arabia. Lancet. 2020;395:e48. doi: 10.1016/S0140-6736(20)30466-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.London Olympics visitor spending by mode of travel 2012. https://www.statista.com/statistics/290512/london-olympics-overseas-visitor-spending-by-mode-of-travel/ [cited 6 Sep 2020]. Available.
- 84.Memish Z.A., Ahmed Q.A., Schlagenhauf P., Doumbia S., Khan A. No time for dilemma: mass gatherings must be suspended. Lancet. 2020:1191–1192. doi: 10.1016/S0140-6736(20)30754-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ebrahim S.H., Zhuo J., Gozzer E., Ahmed Q.A., Imtiaz R., Ahmed Y. All Hands on Deck: a synchronized whole-of-world approach for COVID-19 mitigation. Int J Infect Dis. 2020;98:208–215. doi: 10.1016/j.ijid.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Arab-Mazar Z., Sah R., Rabaan A.A., Dhama K., Rodriguez-Morales A.J. Mapping the incidence of the COVID-19 hotspot in Iran - implications for travellers. Trav Med Infect Dis. 2020;34:101630. doi: 10.1016/j.tmaid.2020.101630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lemieux J., Siddle K.J., Shaw B.M., Loreth C., Schaffner S., Gladden-Young A. Phylogenetic analysis of SARS-CoV-2 in the Boston area highlights the role of recurrent importation and superspreading events. medRxiv. 2020 doi: 10.1101/2020.08.23.20178236. [DOI] [Google Scholar]
- 88.Memish Z.A., Ahmed Y., Alqahtani S.A., Ebrahim S.H. Pausing super spreader events for COVID-19 mitigation: international Hajj pilgrimage cancellation. Trav Med Infect Dis. 2020:101817. doi: 10.1016/j.tmaid.2020.101817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Elachola H., Assiri A.M., Memish Z.A. 2014. Sun protection during the Hajj mass-gathering--2013. Travel medicine and infectious disease; pp. 783–784. [DOI] [PubMed] [Google Scholar]
- 90.Elachola H., Assiri A.M., Memish Z.A. Mass gathering-related mask use during 2009 pandemic influenza A (H1N1) and Middle East respiratory syndrome coronavirus. Int J Infect Dis. 2014;20:77–78. doi: 10.1016/j.ijid.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Elachola H., Ebrahim S.H., Gozzer E. 2020. COVID-19: facemask use prevalence in international airports in Asia, Europe and the Americas, March 2020. Travel medicine and infectious disease; p. 101637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Elachola H., Gozzer E., Rahman N.M.M., Ditekemena J., Pando-Robles V., Pa K. Photo-epidemiology to estimate face covering use in select areas in Asia versus the Americas and Africa during the COVID-19 pandemic. J Trav Med. 2020 doi: 10.1093/jtm/taaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.IATA air travel and COVID-19. https://www.iata.org/en/youandiata/travelers/health/ [cited 15 Oct 2020]. Available.
- 94.Schwartz K.L., Murti M., Finkelstein M., Leis J.A., Fitzgerald-Husek A., Bourns L. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2020. Lack of COVID-19 transmission on an international flight; p. E410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pavli A., Smeti P., Hadjianastasiou S., Theodoridou K., Spilioti A., Papadima K. In-flight transmission of COVID-19 on flights to Greece: an epidemiological analysis. Trav Med Infect Dis. 2020;38:101882. doi: 10.1016/j.tmaid.2020.101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang X.-A., Fan H., Qi R.-Z., Zheng W., Zheng K., Gong J.-H. Importing coronavirus disease 2019 (COVID-19) into China after international air travel. Trav Med Infect Dis. 2020:101620. doi: 10.1016/j.tmaid.2020.101620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Eldin C., Lagier J.-C., Mailhe M., Gautret P. Probable aircraft transmission of Covid-19 in-flight from the Central African Republic to France. Trav Med Infect Dis. 2020:101643. doi: 10.1016/j.tmaid.2020.101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Assessment of risks of SARS-CoV-2 transmission during air travel and non-pharmaceutical interventions to reduce risk phase one report: gate-to-gate travel onboard aircraft prepared by faculty and Scientists at the harvard T.H. Chan School of Public Health.