Abstract
Pharmacies have been practicing innovative infection control measures during COVID-19. This article seeks to explore the current activities undertaken across various community pharmacy settings in relation to the safety of the workplace environment for staff and patients.
Methods
An online cross-sectional survey was conducted in Australia during the COVID-19 outbreak from 1st to 30th April 2020, addressing community pharmacist's awareness and response to infection and sanitation control.
Results
A total of 137 pharmacists took part in the survey. Regular cleaning took place in the pharmacy, but the use of gloves while cleaning was not regularly practice (48.18%). In addition, only 46.72% of respondents reported observing script baskets being cleaned and disinfected. About one-third (37.96%) of pharmacists were aware of the two-step cleaning and disinfecting process, with only 18.98% of pharmacist practicing such cleaning procedures. More than half of surveyed pharmacists reported having difficulty keeping up with pharmacy practice and infection control guidelines during the pandemic.
Conclusion
This study demonstrates that the majority of pharmacists are not fully aware of the proper infection control measures needed in a community pharmacy setting. Pharmacists must play a bigger role in infection control measures to ensure staff and public health safety.
Keywords: Pharmacy practice, Infection control, Sanitation, Hygiene, COVID-19, SARS-CoV-2, Pharmacists, Public health, Workplace safety, OHS
Introduction
The first case of the novel coronavirus was first reported in Wuhan, in the Hubei Province of China in December 2019, with links to a source from a seafood wholesale market in Huanan, Wuhan.1 The spread of the novel coronavirus was uncontainable and spreading rapidly, leading to the Chinese central government imposing a lockdown in Wuhan and other cities in Hubei province as of 23 January 2, 020.2 This was done in effort to quarantine the epicentre of the outbreak, which on the day prior the lockdown 444 positive cases were reported3 with 25 deaths within the Hubei province.4
On 13 January 2020 saw the first coronavirus case outside of China in Thailand. A few weeks later, the first death outside of China was reported in the Philippines.5 On 11 February 2020, the World Health Organization (WHO) changed the name of the novel coronavirus from the 2019 novel coronavirus (2019-nCoV) to coronavirus disease 2019 (COVID-19).6 On March 11, 2020, the World Health Organization labeled COVID-19 to be a pandemic.7 As of 1 April 2020, WHO officially reported more than 823,626 confirmed cases with 40,598 deaths globally.8
The source and etiology of COVID-19 is still unknown. As of current evidence, COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus that is spread via droplet transmission of between 5 and 10 μm.9 Such transmission can occur via an infected person's sneeze or cough that results in expulsion of infectious respiratory droplets into the air and surfaces.10 Transmission can occur via two different modes: 1) direct, and 2) indirect contact.11 In direct contact, an infectious individual can transfer the virus to susceptible host via actions such as a handshake from a contaminated hand or inhalation of a droplet from an infected person's sneeze. On the other hand, indirect contact consist of an infectious individual transferring viral content on a fomite such as a frequently touched surface in the form of door handles, elevator buttons and via money transactions. Both contact methods can lead to COVID-19 infection when susceptible individuals unknowingly come in contact with viral contents on their oral, nasal, or eye mucous membranes, or touching these areas with their contaminated hands.12 As it is not known definitely if COVID-19 is an airborne virus, America's Centres for Disease Control and Prevention (CDC) has recommended that healthcare workers and teams ensure adequate environmental sanitation, sound infection prevention practices and routine droplet barrier precautions.13
The virus that causes COVID-19 disease is the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).6 A recent study has shown that SARS-CoV-2 virus can remain viable on various surfaces for different lengths of time, and can be a factor in human-to-human transmission via indirect contact.14 The study published in the New England Journal of Medicine demonstrated that aerosols (<5 μm) of SARS-CoV-2 strain was detectable in the air for up to 3 h, 4 h on copper, 24 h on cardboard and up to two to three days on plastic and stainless steel surfaces.14 SARS-CoV-2 also has a longer half-life on cardboard than SARS-CoV-1 (the virus strain that causes SARS in 2003). With that, SARS-CoV-2 has a higher propensity for both community transmissions in the public and healthcare setting due to the handling of external cardboard packaging as compared to SARS-CoV-1. This places community pharmacies at an increased risk due to its unique overlap as a primary healthcare facility and placement in the community encountering high foot traffic (i.e. shopping centres, medical clinics, hospitals).
Pharmacist can play wide-ranging roles in disaster management across four key phases in 1) prevention, 2) preparedness, 3) response, and 4) recovery.15 In community pharmacies, the provision of accurate public health education and knowledge on infection control and disease transmission are important across these four phases during an infectious diseases outbreak.16
As highly assessable healthcare professionals,17 the community pharmacist will often be the first point of contact within the Australian health system for individuals who require advice on COVID-19-related information, health advice and medication access during the current pandemic.18 With physicians cancelling non-urgent consultations and Australian government ceasing non-essential elective surgery to free up human and capital resources to manage COVID-19,19 the community pharmacist is now one of the sole point of contact in the primary healthcare system. To respond to the crisis, pharmacies extended their opening hours and services, and is supported by the Australian Government in delivering medicines to vulnerable populations to ensure continuity of medicine supply and treatments.20 Early accounts from Chinese community pharmacist showed that pharmacists played significant roles in educating the public on personal and environmental hygiene during COVID-19.21 Therefore it is imperative that community pharmacist possess the right knowledge needed to help limit the impacts of COVID-19 in the community.22
The total positive COVID-19 cases vary across Australian states and territories.23 Community pharmacies are in an environment where staff are not advised to routinely wear masks and personal protective equipment (PPE). A mixture of clinical staff (pharmacist), non-clinical staff (pharmacy assistants and dispensary technicians) and patients utilize common areas and devices such as communal pens, blood pressure monitors, script counters, product shelves, furniture and keyboards. As community pharmacies do not commonly have dedicated environmental service workers in cleaning its premises, the responsibilities of cleaning and disinfecting frequently touched surfaces rests on individual pharmacies and their management team. Good infection prevention and control practices can reduce direct virus transmission between people, and indirectly through contact with frequently touched items in the pharmacy. It is therefore important that pharmacy staff are practicing meticulous hand hygiene with readily available hand hygiene products,24 and keeping workspaces clean and disinfected regularly to eliminate potential source of infection.25 Providing a set of measures in decontamination not only minimizes the spread of COVID-19, but also provides extra assurance to stressed and concerned pharmacy staff and their patients during the pandemic.26
Community pharmacists in Australia are in a unique position where they are neither classified front-line health workers in the COVID-19 pandemic but may be considered to be at medium risk of exposure to the SARS-CoV-2 virus.18 Given that community pharmacies are categorized as retail workplaces, pharmacist and their employers must use their professional judgment to determine their pharmacy's risk exposure, and provide staff with the necessary PPE such as masks, goggles, gowns and gloves.27
With community pharmacy an essential healthcare service in Australia, the health and safety of the pharmacy workforce is of high priority. While some pharmacies have reported providing novel and extra measures on top of professional infection control guidance,28 leaders in each community pharmacy must ensure adequate hygiene measures are practiced as per their situation. Professional oversight and leadership are essential to preserve the health and safety of pharmacy staff and ensure continuity in supply of essential health services to the public.29 In addition, leaders in the workplace should be made aware of individual worker's pre-existing health conditions that may put them at a higher risk of severe infections and complications should they contract COVID-19, and redeploying these susceptible workers to non-patient facing roles where the risk of contracting COVID-19 is lower.
Published research has been focusing on the extent of pharmaceutical care being provided by pharmacists in all clinical settings.27 , 28 No previous study has looked into pharmacist and/or pharmacy's response to their role in sanitation implementation management in the COVID-19 pandemic.
Pharmacists are one of the most highly trusted profession in Australia,30 and it is of utmost importance that they provide sound public health recommendations21 and implement adequate sanitation and infection control measures that can support the ever-evolving levels of an infectious disease outbreak emergency.31
The aim of this study was to investigate pharmacies and pharmacists’ preparedness level and their awareness of important information regarding the occupational health and safety of their workplaces in infection control during this emergent situation.
Methods
Study period
Australia's positive COVID-19 case numbers started to increase at the start of March 2020 and peaked towards the end of March 2020. On 1 April 2020, Australia has a total of 4707 COVID-19 confirmed cases and 20 deaths from COVID-19.8 The month of April 2020 was the start of strict restrictions in public gatherings to curb the spread of the virus.32 A survey conducted during this period of highest social restrictions will demonstrate community pharmacy's response to the pandemic.
Study design
A quantitative cross-sectional survey was undertaken during the month of April 2020. An online survey was directed at Australian registered pharmacist practicing in the community setting or in a pharmacy that includes a retail section. The survey consists of 23 multiple choice questions formulated based on guidance from the International Pharmaceutical Federation (FIP) health advisory,18 New South Wales (NSW) health advice for community pharmacies on COVID-19,33 websites from non-Australian pharmacy society and medical society, media networks, and observations of the rapid changes taking place around retail companies in infection control measures. Questions included steps taken for staff and patient safety, understanding of sanitation requirements, and steps taken by each individual pharmacies in maintaining hygiene standards.
Questionnaire administration
Pharmacists were invited to participate via informal pharmacist-only groups on social media website Facebook. These informal groups are a mix of employed pharmacist working either as full time, part-time, locums, managers, and employer pharmacist proprietors. The survey was provided via an online link onto a Survey Monkey website. Pharmacists were informed prior participation in the survey that their participation is made anonymous, voluntary, and their inputs will be treated as confidential. The names of pharmacists and their professional registration numbers were not recorded in any part of the survey. Consent was obtained from participants’ prior the start of the survey. The survey was opened from 1 April 2020 to 31 April 2020.
Data analysis
The data from the online survey were exported into Microsoft Office Excel and into IBM SPSS Statistic 25. Frequency analysis was performed to create a demographic profile of our participants.
Results
In this section, a pharmacist's response is assumed to be synonymous to their own actions or the actions taken at their primary workplace.
Participant's demographics
A total of 137 pharmacists took part in the survey, with 71.53% females and 28.47% males. Almost half (45.26%) of pharmacist surveyed belonged to the age group of 25–34 years. Community pharmacy represented 89.05% of participant's primary place of practice, with 9.49% practicing at private hospitals with a retail section, and 1.46% at public hospitals with retail sections.
In Australia, community pharmacies are categorized into three main groups. Discount chains, non-discount chains, and independent pharmacies. Half of our study's participants belong to non-discount chains (47.45%), followed by independents (34.31%), then discount chains (18.25%).
Full/part-time employed pharmacist formed half of our study's participants (55.47%), with pharmacist manager at 18.25%, pharmacist proprietor at 15.33%, and locum/casual pharmacist at 10.95% (see Table 1 ).
Table 1.
Participant's demographics.
| Demographic | Type | Percentage (%) |
|---|---|---|
| Sex | Male | 28.47 |
| Female | 71.53 | |
| Age | 18–24 | 6.57 |
| 25–34 | 45.26 | |
| 35–44 | 16.79 | |
| 45–54 | 18.98 | |
| 55–64 | 12.41 | |
| 65+ | 0.00 | |
| Primary Place of Practice | Community pharmacy | 89.05 |
| Private hospital pharmacy with community retail section | 9.49 | |
| Public hospital pharmacy with community retail section | 1.46 | |
| Pharmacy Groups | Discount chains | 18.25 |
| Non-discount chains | 47.45 | |
| Independents | 34.31 | |
| Pharmacist Roles | Full/Part-time | 55.47 |
| Pharmacist Manager | 18.25 | |
| Pharmacist Proprietor | 15.33 | |
| Locum/Casual | 10.95 |
Overall health & safety activities
When surveyed on whether they are asked to wear face masks at work, 82.48% of pharmacist were not asked to wear face masks, while the remaining 17.52% of pharmacist chose or were asked to wear face masks during work periods.
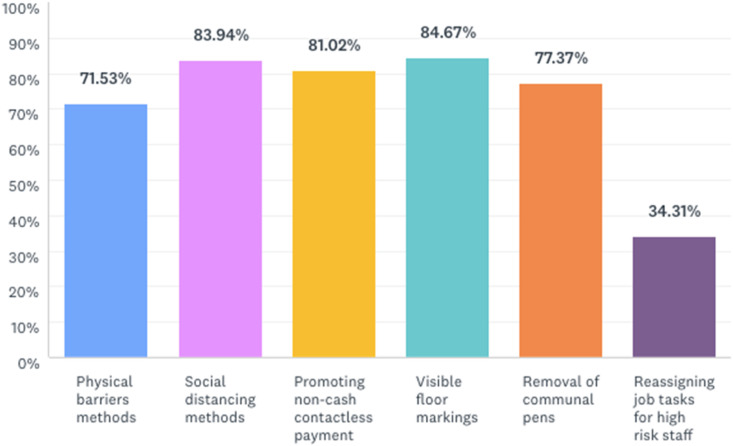
In terms of staff safety precaution, there were more than 70% uptake of social distancing and hygiene measures in the areas of employing clear physical Plexiglas shields, social distancing at cash registers, encouragement of contactless payment, visible floor markings for safe distancing in high traffic areas, and removing of communal pens. However reassigning of job task for immunocompromised or high health risks staff (such as moving away from patient-facing roles) was least practiced in pharmacies, with only an uptake of 34.31% of total respondents (see Fig. 1 ). In addition, temperature checks prior starting work was not heavily practiced, with only 42 out of 137 participants being involved in such measures.
Fig. 1.
The uptake of activities undertaken by pharmacists and their pharmacies in ensuring staff and workplace safety.
A small number of pharmacies (35.04%) provided restricted sections of the pharmacy for COVID-19 suspected patients, while 65.69% of pharmacies were actively involved in limiting the amount of patients in the pharmacy premises at any one time according to the 4 square meters per person guidelines.34
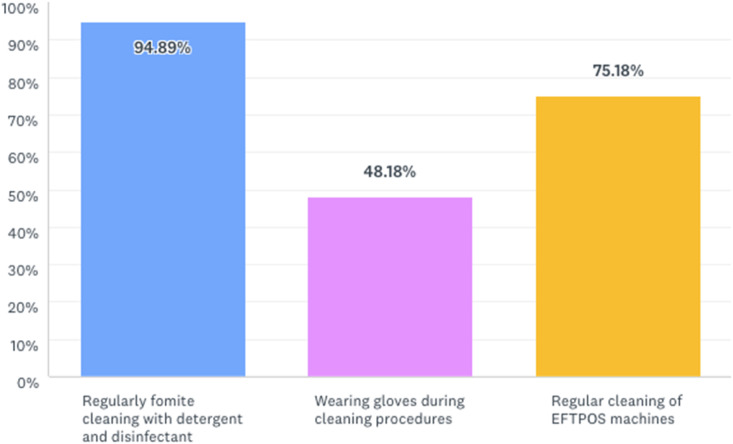
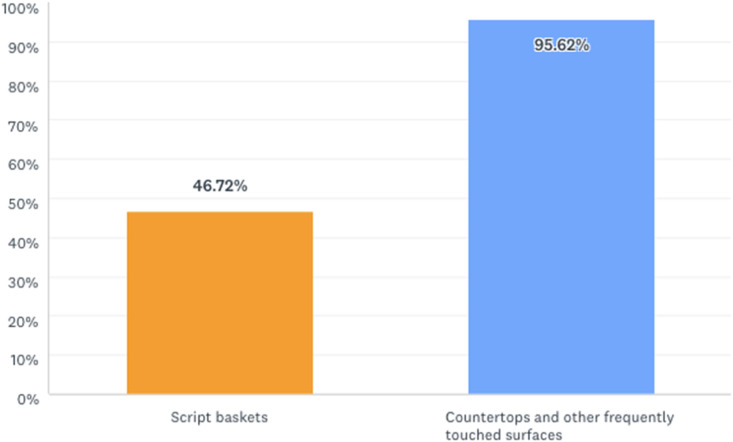
When assessing the awareness and status of sanitation and infection control in the workplace, 94.89% of pharmacists observed regular cleaning occurring in their workplace. However only 48.18% of cleaning was performed using gloves (see Fig. 2 ). Frequently touched surfaces such as countertops were cleaned regularly as reported by 95.62% of respondents, but only 46.72% of respondents reported observing script baskets (a frequently touched item) being cleaned and disinfected (see Fig. 3 ).
Fig. 2.
Awareness and status of sanitation and infection control practices undertaken by pharmacists and their pharmacies.
Fig. 3.
Types of fomites cleaned and disinfected by pharmacists and their pharmacies.
Out of the 137 pharmacists surveyed, only 49 pharmacists (35.77%) worked in pharmacies that provided hand sanitizer for patient use as a pre-requisite before entry into the premises. Only 44.53% of pharmacies provided hand sanitizers around the pharmacy premises for public use.
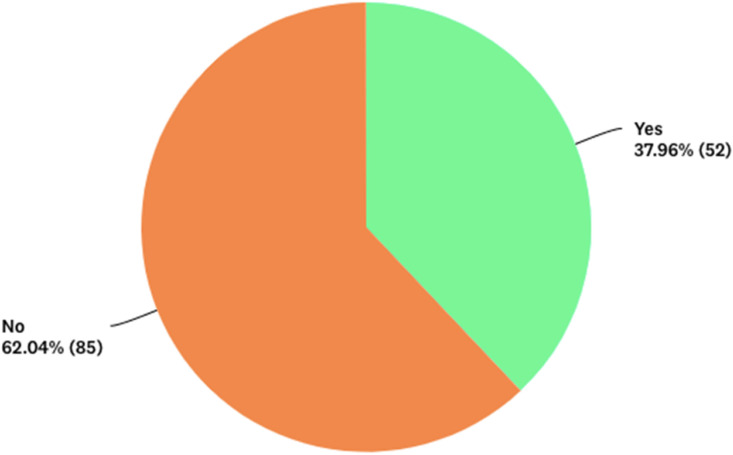
About one-third (37.96%) of pharmacists were aware of the two-step cleaning and disinfecting process of using detergent and water followed by a chemical disinfectant (see Fig. 4 ). When surveyed, a majority of pharmacist (34.31%) observed that their workplace only used a chemical disinfectant as a cleaning process on frequently touched surfaces, while 24.09% observed the usage of a combination of chemical disinfectant and natural disinfectant such as eucalyptus oil and tea tree oil (see Table 2 ). Only 18.98% of pharmacies were practicing the correct two-step cleaning and disinfecting process.
Fig. 4.
Pharmacist's awareness of two-step cleaning and disinfecting process in Australian healthcare setting.
Table 2.
Cleaning and disinfection practice in the pharmacy.
| Types of method(s) | Percentage (%) |
|---|---|
| A: Detergent with warm water | 2.92 |
| B: Chemical disinfectant | 34.31 |
| C: Natural disinfectant | 5.11 |
| A and B | 18.98 |
| A and C | 2.19 |
| B and C | 24.09 |
| A, B and C | 12.41 |
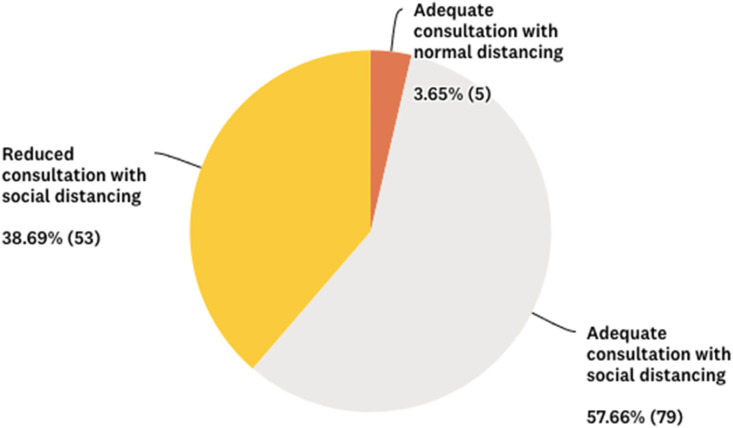
With the need to practice physical distancing, more than half of all pharmacists responded that medication advice and clinical services could be achieved. However 38.69% of pharmacist found the provision of clinical services and medication counseling to be challenging due to distancing measures (see Fig. 5 ).
Fig. 5.
Pharmacist's response to social/physical distancing and medication counseling ability.
More than half of surveyed pharmacists reported difficulty in keeping up with evolving changes in pharmacy practice guidelines during this period of time. Only 9.49% of pharmacist found it easy to keep up-to-date to new guidelines.
Discussion
The majority of pharmacists surveyed did not observe or practice wearing face mask at work. This was in line with the guidance provided by the Australian Department of Health.35 Unless pharmacists are in direct contact with confirmed cases of COVID-19 patients, they will then be required to put on full Personal Protective Equipment (PPE) including P2/N95 respirators, disposable gowns, aprons, goggles, visors and gloves.35 The split decision to wear surgical mask despite guidance is similar to pharmacist in the United Kingdom.36 In Australia, local primary health networks have provided community pharmacies with surgical mask and some PPE, only to be used in situations where pharmacist are in direct contact with a confirmed COVID-19 case or to be given to a suspected patient.37
The death of a community pharmacist in the United Kingdom made certain that community pharmacies are susceptible to COVID-19 despite their position as a retailer.38 Community pharmacies are a mix of primary healthcare service with a retail section, and therefore may come in contact with patients who are asymptomatic or are displaying cold and flu-like symptoms similar to that of COVID-19. Pharmacists play an important role in triaging these patients and directing suspected patients to COVID-19 testing centres. Therefore the risk of close contact with a true positive COVID-19 case is still probable. Hence stringent measures must be taken to ensure staff safety is of utmost importance in community pharmacies.
The data obtained in this survey showed that pharmacies are not practicing reassigning at-risk staff members to non-patient facing roles. In addition, temperature checks prior commencement of the days work was not regularly conducted. This poses a risk for staff and patients, as precautions are not put in place to ensure the safety of both pharmacy teams and their patients. Stricter compliance to guidance provided by local professional pharmacy organization and government documents could mitigate the risks of community transmission of COVID-19 in the compounds of the community pharmacy.29
The nature of community pharmacy premise is the absence of infrastructure requirements to isolate and monitor patients with highly contagious infectious diseases.39 Due to limited floor space requirements; the provision of an isolated area is least likely to occur in a community pharmacy. A snapshot survey performed in the United Kingdom showed that 94% and 40% of pharmacist were unable to maintain a physical distance of 2 m from their colleagues, and patients respectively.40
Only half of pharmacist respondents reported the use of hand gloves worn by themselves or staff during the cleaning and disinfecting process in the pharmacy. Gloves are meant to protect the individual performing the sanitation process. It preserves hand skin integrity by forming a physical barrier against the irritant and hazardous nature of some cleaning chemicals, and also provides protection against cuts and punctures to skin membranes when cleaning contaminated sharp objects.41 As community pharmacies do not regularly employ professional environmental cleaning professionals to maintain hygiene standards in the pharmacy, further education on the importance of wearing gloves during cleaning should be disseminated to pharmacy staff to ensure safe sanitation and hygiene procedures.
The stability of SARS-CoV-2 is greater in plastics and stainless than in copper and cardboard materials.14 Prescription or script baskets made up of plastic are a norm in the pharmacy profession as a way to segregate different patient's medications to reduce medication errors (such as receiving someone else's medication).42 These script baskets could be the most highly touched objects in the pharmacy and will be the medium of possible SARS-CoV-2 transmission between staff and patients. With less than half of all surveyed pharmacists responding to the observation in cleaning and disinfecting procedures of script baskets, it highlights the blind spot in pharmacy attention to the identification of highly touched objects meant for targeted cleaning and disinfection.
Only 52 out of 137 (37.96%) of pharmacists were aware of the recommended two-step mechanical cleaning and disinfecting procedure in a healthcare setting, with only half of that population (26 respondents) practicing it in their primary workplace. This lack of understanding of the correct cleaning procedure and implementation43 could reduce the safety and hygiene standards of the pharmacy during the COVID-19 pandemic. Similar results were obtained in non-healthcare workplaces around Australia where employees were reasonably knowledgeable about basic infection prevention measures (such as good hand hygiene and equipment cleaning), but were unaware of its true effectiveness and appropriateness in their specific workplaces.44
In contrast, pharmacists in China were heavily involved in ensuring public safety by ensuring high standards of infection control measures.45 Therefore more attention should be given to pharmacists around infection control measures to ensure the continuity of their role as an essential service provider.
Social and physical distancing may compromise the quality of medication counseling provided by a pharmacist, especially when community pharmacies do not regularly have a private room to conduct counseling of private and confidential health matters. However the safety of patients and staff are crucial during this period of time. Pharmacists who are unable to relay private health message across to a patient during a physical distancing consultation could utilize telehealth methods to deliver quality care as soon as practicable. A systematic review demonstrated positive patient satisfaction in receipt of telehealth consultations, but its effectiveness and efficiency are still debated.46 In Australia, general practitioners and accredited consultant pharmacists have been given the ability for reimbursement for telehealth during the COVID-19 pandemic as a means of ensuring the continuity of quality medical and healthcare.47 , 48 This provision offers incentives to accredited pharmacist to conduct telehealth for their patients, however non-accredited pharmacist are not able to get reimbursed for such telehealth consultations, and may hinder the quality of consultations that requires more privacy while trying to maintain physical and social distancing in a community and/or retail setting.
During the course of COVID-19 pandemic, the large influx of guidance changes to sanitation and hygiene protocols may create some confusion and anxiety among non-clinical pharmacy staff. As community health leaders, pharmacists must uphold sanitation measures so as to reduce anxiety among staff and the public. Carico Jr et al. discussed the possible benefits of pharmacists applying the Health Belief Model to reinforce COVID-19 limiting behaviours to patients,22 and this construct could be helpful for adopting better infection control practices amongst staff. It is crucial that continuous feedback sessions are conducted, including the dissemination of transparent information in a clear and concise manner so that teams can practice safely. As the only clinical member of a community pharmacy, pharmacists must continue to keep up-to-date with the ever-evolving changes to workplace health and safety requirements, including proper sanitation and infection protocols to ensure staff and patients feel safe. A recent media release showed that patient visits to their general practitioner have dropped due to fear of contracting COVID-19 in the clinic.49 Community pharmacists and pharmacies must aim to quell fear by setting high standards in hygiene management such that patients continue to visit their pharmacist and/or community pharmacy regularly thus not putting themselves at risk of not being able to access essential healthcare items.
Infection control management strategies are more likely to be developed in higher infection risk organizations (e.g. aged care facility and hospitals), where exposure of biohazard waste and bodily fluids to staff are higher as compared to those working in lower risk areas.50 Regardless, most non-healthcare business independent of size reported a lack of formalized policy plans in infection prevention strategies even for the annual influenza virus.51 In addition, infection control strategies adopted in workplaces were not backed by evidence, but rather based on assumption to be more effective than other infection control strategies.51
In the uncertainty of COVID-19, the maintenance of a hygienic and sanitary environment in community pharmacies must be prioritized. A systematic review on hand hygiene programs in the office setting showed increased staff morale and confidence at work when such programs are put in place.52 Despite the ever-evolving work health and safety requirements in different industry types may have influenced the results, pharmacy management teams must take initiatives and plan ahead to enact adequate evidence-based protection measures for the safety and morale of their staff and patients.53
Conclusions
During times of crisis, community pharmacists are required to adapt to and respond with new ideas to safeguard the profession and their community. Community pharmacists are given a huge responsibility of accurately informing their local community about ways to reduce community spread of the SARS-CoV-2 virus.
This article is not exhaustive, but serve to illustrate the range of activities undertaken by community pharmacists in infection control and environmental hygiene risk management measures in response to the public health crisis of COVID-19. These measures are currently implemented to varying extents across pharmacy settings; and show pharmacists commitments and response to protect their staff and the local community. Although most pharmacies were implementing an adequate range of infection control and prevention strategies, a majority was unaware of the efficacy and correct infection control guidelines for their particular business setting. Certain gaps in infection control around COVID-19 were identified and highlighted for improvement; and it is hoped that the future corrective action strategies can help pharmacists uphold public health roles and minimize the community spread of COVID-19. The last thing community pharmacies would want to become is a reservoir source of COVID-19 transmission.
This article demonstrated the varied response in pharmacists and pharmacies role in infection control as their public health response during COVID-19. In the future when the pandemic curtails and normality has settled; the collective infection control actions of pharmacists, pharmacy academics, educators, professional organizations, and allies must be reviewed and evaluated to guide awareness and future policy responses against the next infectious disease pandemic.
Author contributions
“Conceptualization, Z.S. and C.O.; methodology, Z.S. and C.O.; formal analysis, Z.S.; investigation, Z.S and C.O.; data curation, Z.S and C.O.; writing—original draft preparation, Z.S.; writing—review and editing, Z.S.; visualization, Z.S.; project administration, Z.S. and C.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
We would like to thank frontline pharmacists that played an important role in helping craft this area of research during COVID-19. Your ideas have been inspirational and contributed to the development of this vital research in pharmacists' health and safety in the community.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2020.06.014.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lockdowns Rise as China Tries to Control Virus. BBC News; 2020. https://www.bbc.com/news/world-asia-china-51217455 Published. [Google Scholar]
- 3.Jiang S. CNN; 2020. Death Toll in China Rises to 17.https://edition.cnn.com/asia/live-news/wuhan-coronavirus-china-intl-hnk/h_4298eb7dac659e02dfe712a4d0ae134e Published. [Google Scholar]
- 4.Jiang S. CNN; 2020. Death Toll Rises to 25.https://edition.cnn.com/asia/live-news/coronavirus-outbreak-intl-hnk/index.html Published. [Google Scholar]
- 5.The Straits Times . 2020. First Death outside China in Philippines.https://www.straitstimes.com/asia/se-asia/first-death-outside-china-in-philippines Published. [Google Scholar]
- 6.Naming the coronavirus disease (COVID-19) and the virus that causes it. Who. Int. 2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Published. [Google Scholar]
- 7.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Who.int. Published.
- 8.Coronavirus disease 2019 (COVID-19) situation report – 72. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?sfvrsn=3dd8971b_2 Who.int. Published.
- 9.World Health Organization . World Health Organization; Geneva: 2020. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations.https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations [Google Scholar]
- 10.Tellier R., Li Y., Cowling B., Tang J. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect Dis. 2019;19(1) doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asadi S., Bouvier N., Wexler A., Ristenpart W. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles? Aerosol Sci Technol. 2020:1–4. doi: 10.1080/02786826.2020.1749229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu C., Liu X., Jia Z. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/s0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coronavirus Disease 2019 (COVID-19) Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol-recommendations.html Published. [Google Scholar]
- 14.van Doremalen N., Bushmaker T., Morris D. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 doi: 10.1056/nejmc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rimmer A. Covid-19: GPs can stop health checks for over 75s and routine medicine reviews. BMJ. 2020:m1157. doi: 10.1136/bmj.m1157. [DOI] [PubMed] [Google Scholar]
- 16.Kaku M. Expect for the pharmacist in the management of infectious diseases. Yakugaku Zasshi. 2011;131(10):1403–1405. doi: 10.1248/yakushi.131.1403. [DOI] [PubMed] [Google Scholar]
- 17.Todd A., Copeland A., Husband A., Kasim A., Bambra C. The positive pharmacy care law: an area-level analysis of the relationship between community pharmacy distribution, urbanity and social deprivation in England. BMJ Open. 2014;4(8) doi: 10.1136/bmjopen-2014-005764. e005764-e005764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Pharmaceutical Federation . International Pharmaceutical Federation; The Netherlands: 2020. COVID-19: Guidelines for Pharmacists and the Pharmacy Workforce.https://www.fip.org/files/content/priority-areas/coronavirus/COVID-19-Guidelines-for-pharmacists-and-the-pharmacy-workforce.pdf [Google Scholar]
- 19.Prime Minister of Australia . 2020. Elective Surgery.https://www.pm.gov.au/media/elective-surgery [Google Scholar]
- 20.Department of Health . 2020. Ensuring Continued Access to Medicines during the COVID-19 Pandemic.https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/ensuring-continued-access-to-medicines-during-the-covid-19-pandemic [Google Scholar]
- 21.Ung C. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019-nCoV outbreak. Res Soc Adm Pharm. 2020;16(4):583–586. doi: 10.1016/j.sapharm.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carico R., Sheppard J., Thomas C. Community pharmacists and communication in the time of COVID-19: applying the health belief model. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMillan S., Wheeler A., Sav A. Community pharmacy in Australia: a health hub destination of the future. Res Soc Adm Pharm. 2013;9(6):863–875. doi: 10.1016/j.sapharm.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization . World Health Organization; Geneva: 2009. WHO Guidelines on Hand Hygiene in Health Care: A Summary.https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf [Google Scholar]
- 25.World Health Organization . World Health Organization; Geneva: 2009. Hand Hygiene: Why, How & when?https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf [Google Scholar]
- 26.Adams J., Walls R. Supporting the health care workforce during the COVID-19 global epidemic. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 27.Aruru M., Truong H., Clark S. Pharmacy Emergency Preparedness and Response (PEPR) framework for expanding pharmacy professionals' roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper R. Here's how community pharmacies are adapting to COVID-19 - Australian Pharmacist. 2020. https://www.australianpharmacist.com.au/heres-how-community-pharmacies-are-adapting-to-covid-19/ Australian Pharmacist. Published.
- 29.The Pharmacy Guild of Australia . The Pharmacy Guild of Australia; 2020. COVID-19 Pandemic Planning and Guidelines.https://www.guild.org.au/resources/business-operations/covid-19/covid-19-guide-for-community-pharmacy [Google Scholar]
- 30.Morgan Roy. Roy Morgan Research Ltd; Melbourne: 2017. Roy Morgan Image of Professions Survey 2017.http://file:///Users/zacharysum/Downloads/7244-Image-of-Professions-2017-May-2017.pdf [Google Scholar]
- 31.Mukhtar S. Research in Social and Administrative Pharmacy. 2020. Preparedness and proactive infection control measures of Pakistan during COVID-19 pandemic outbreak. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Victoria in Stage 3 Coronavirus Shutdown Restrictions as Cases Climb to 821 - ABC News. 2020. https://www.abc.net.au/news/2020-03-30/victoria-stage-3-coronavirus-restrictions-as-cases-rise/12101632 abc.net.au. Published. [Google Scholar]
- 33.Advice for community pharmacies on COVID-19. health.nsw.gov.au. 2020. https://www.health.nsw.gov.au/Infectious/diseases/Pages/covid-19-pharmacy.aspx Published.
- 34.Coronavirus (COVID-19) - new restrictions and closures. Dhhs.vic.gov.au. 2020. https://www.dhhs.vic.gov.au/coronavirus-covid-19-new-restrictions-and-closures Published.
- 35.Department of Health . Australian Government Department of Health; Canbera: 2020. Information on the Use of Surgical Masks.https://www.health.gov.au/sites/default/files/documents/2020/03/coronavirus-covid-19-information-on-the-use-of-surgical-masks.pdf [Google Scholar]
- 36.Are pharmacy teams being protected against COVID-19? Pharm J. 2020 doi: 10.1211/pj.2020.20207902. [DOI] [Google Scholar]
- 37.Personal Protective Equipment (PPE) for the Health Workforce during COVID-19. Australian Government Department of Health; 2020. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-advice-for-the-health-and-aged-care-sector/personal-protective-equipment-ppe-for-the-health-workforce-during-covid-19 Published. [Google Scholar]
- 38.Burrows T. The Sun. 2020. Dad-of-two pharmacist dies on coronavirus frontline as heartbroken wife and friends pay tribute.https://www.thesun.co.uk/news/11503303/dad-of-two-pharmacist-dies-coronavirus-family-friends-tribute/ Published. [Google Scholar]
- 39.The Pharmacy Guild of Australia . The Pharmacy Guild of Australia; 2020. COVID-19 Community Pharmacy Isolation Room/Area.https://www.guild.org.au/__data/assets/pdf_file/0030/90669/20200324-COVID-19-Community-Pharmacy-Isolation-Room-Area-Final.pdf [Google Scholar]
- 40.Royal Pharmaceutical Society | RPS. Rpharms.com; 2020. Pharmacists ‘unable to maintain social distancing’ at work and risk infection.https://www.rpharms.com/about-us/news/details/Pharmacists-unable-to-maintain-social-distancing-at-work-and-risk-infection Published. [Google Scholar]
- 41.South Australia Health . SA Health; 2015. Personal Protective Equipment (PPE) Selection.https://www.sahealth.sa.gov.au/wps/wcm/connect/8776f5804a4632a38e90cfb0cfc4074a/Guideline_Personal+Protective+Equipment+PPE+Selection_Policy_Oct2015.pdf?MOD=AJPERES&CACHEID=8776f5804a4632a38e90cfb0cfc4074a [Google Scholar]
- 42.Harvey J., Avery A., Ashcroft D., Boyd M., Phipps D., Barber N. Exploring safety systems for dispensing in community pharmacies: focusing on how staff relate to organizational components. Res Soc Adm Pharm. 2015;11(2):216–227. doi: 10.1016/j.sapharm.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Change Management and Community Pharmacy Project. 2004. http://6cpa.com.au/wp-content/uploads/Change-management-and-community-pharmacy-Fina-Report-Part-6.pdf 6cpa.com.au. Published. [Google Scholar]
- 44.Hansen S., Zimmerman P., van de Mortel T. Assessing workplace infectious illness management in Australian workplaces. Infect Dis Health. 2017;22(1):12–20. doi: 10.1016/j.idh.2016.12.005. [DOI] [Google Scholar]
- 45.Li H., Zheng S., Liu F., Liu W., Zhao R. Research in Social and Administrative Pharmacy. 2020. Fighting against COVID-19: innovative strategies for clinical pharmacists. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kruse C., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8) doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Expansion of Telehealth Services Australian government department of health. 2020. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/expansion-of-telehealth-services Published.
- 48.Cooper R. Telehealth medication reviews introduced. Australian Pharmacist. 2020 https://www.australianpharmacist.com.au/telehealth-medication-reviews-introduced/ Published. [Google Scholar]
- 49.Mason S. COVID-19 Fears lead to patients wrongly stopping GP visits and putting their health at risk. Aust Patients Assoc Aust Patients Assoc. 2020 https://www.patients.org.au/covid-19-fears-lead-to-patients-wrongly-stopping-gp-visits-and-putting-their-health-at-risk/ Published. [Google Scholar]
- 50.National Hazard Exposure Worker Surveillance – exposure to biological hazards and the provision of controls against biological hazards in Australian workplaces. Safeworkaustralia.gov.au. 2011. https://www.safeworkaustralia.gov.au/system/files/documents/1702/nhews_biologicalmaterials.pdf Published.
- 51.Huang C., Ma W., Stack S. The hygienic efficacy of different hand-drying methods: a review of the evidence. Mayo Clin Proc. 2012;87(8):791–798. doi: 10.1016/j.mayocp.2012.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zivich P., Gancz A., Aiello A. Effect of hand hygiene on infectious diseases in the office workplace: a systematic review. Am J Infect Contr. 2018;46(4):448–455. doi: 10.1016/j.ajic.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 53.Staying Alert and Safe (Social Distancing) GOV.UK; 2020. https://www.gov.uk/government/publications/staying-alert-and-safe-social-distancing/staying-alert-and-safe-social-distancing Published. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.