Letter:
We read with great interest the article by Jayakumar et al,1 “Neurosurgical referral patterns during the COVID-19 pandemic: a United Kingdom experience.” This article provides a relevant insight into the effects of the coronavirus disease 2019 (COVID-19) pandemic on the pattern of neurosurgical referrals at the authors’ institution, a level I trauma center in the northeast of England, which serves a population of >3 million people. The United Kingdom was under a nationwide lockdown from March 23 to May 13, 2020. The authors evaluated all electronic referrals from their database from January to May 2020 and used January 2020 as the baseline because the first COVID-19 case in the United Kingdom was diagnosed on January 31, 2020. They observed that the monthly referrals had decreased from January (n = 572) to April (n = 352) before increasing again in May (n = 441). A statistically significant reduction was observed in the volume of referrals for degenerative spine cases and traumatic brain injuries (P < 0.001). Similarly, the number of patients presenting with stroke syndromes, subarachnoid hemorrhage, tumors, and shunts decreased during the pandemic months in their study.
The whole world has been affected by the ongoing COVID-19 pandemic. India reported its first case of COVID-19 on January 30, 2020,2 and the first case in the Himalayan state of Uttarkhand was reported on March 15, 2020.3 With the early implementation of a nationwide lockdown, India was able to delay the increase in the number of COVID-19 cases to a certain extent compared with the United Kingdom and Europe. The administration and hospitals used this time to prepare for the incoming patients. The government advised patients against crowding hospitals for minor ailments to prevent the hospitals from becoming “hotspots” for the spread of COVID-19. The All India Institute of Medical Sciences, Rishikesh, is a 960-bed institute catering to the Himalayan state of Uttarkahand with a population of ~11 million. Since the onset of the COVID-19 pandemic in India, we have largely restricted the use of physical outpatient department (OPD) procedures and have been attending mainly to emergent patients. This protocol was instituted as a part of institute policy to divert most of the available resources in preparation of the incoming tsunami of patients with COVID-19 and remain able to treat emergent cases. Gradually, as the lockdown was eased starting June 1, 2020, we have gradually increased our intake of OPD patients, although the volume has remained curtailed compared with that before the COVID-19 pandemic.
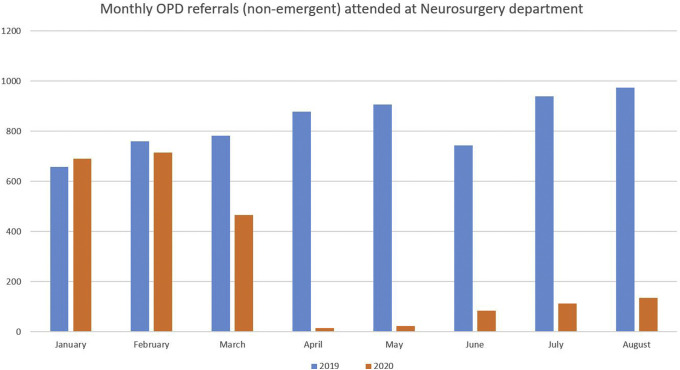
We evaluated the number of nonemergent patients attending our neurosurgery OPD during the months of the ongoing pandemic (ie, January to August) and compared these numbers with the data from the same months in 2019. We compared the data specifically by month to remove any seasonal variation in the patient profile, which can be a confounding factor in our hilly state. In January and February 2020, the number of patients attending the neurosurgery OPD at our institute was similar to that in the same months in 2019. With the arrival of COVID-19 and vigorous mass education by the government, the OPD volumes declined substantially in March and were the lowest in April and May 2020. As the lockdown was eased starting June 1, 2020, the OPD volumes again started to gradually increase (Figure 1 ). Our operative workload reflected this change in nonemergent OPD volumes.4 5 During the lockdown period in 2020 (March 25 to May 31, 2020), 53 surgeries (47 emergency and 6 routine) had been performed compared with 111 (47 emergency, 64 routine) during the same period in 2019. Furthermore, the number of surgeries performed per week had declined steadily as the number of COVID-19 cases increased in the state [rs(8) = −0.914; P = 0.000]. A similar decrease in OPD patients had occurred in the whole country as depicted by a nationwide survey of 201 Indian neurosurgeons from May 7 to May 23, 2020, conducted by us, in which a decrease in the OPD patient volume of 76.25% was observed (P = 0.000).6 , 7 Various investigators have documented similar declines in the number of OPD patients across the world.8, 9, 10, 11, 12 , 13
Figure 1.
Vertical bar graph depicting the number of “nonemergent” outpatient department patients from January to August in 2019 and 2020. Compared with the same period in 2019, the outpatient department referrals in 2020 were comparable in January and February, started decreasing in March, were the lowest in April and May, and started increasing gradually with the easing of the lockdown in June.
On analyzing our operative workload by specialty, a decrease in the number of cases was noted across all specialties compared with before the COVID-19 pandemic4 in concordance with the findings reported by Jayakumar et al.1 The number of neuro-trauma cases had decreased owing to the decreased number of road traffic accidents, which had resulted from the reduced vehicle movement during the lockdown. No patients with degenerative spine had undergone surgery during the pandemic in our study, probably because such cases could easily be managed conservatively at home. The number of neuro-oncology cases and ruptured aneurysms also decreased, similar to the findings reported by Jayakumar et al.1 The number of cerebrospinal fluid diversion procedures in our study had been the least affected by the COVID-19 pandemic.
We appreciate and share the concern of Jayakumar et al.1 for patients unable to receive the necessary hospital care because of the pandemic. A risk exists of these patients presenting at a later stage with disease progression, resulting in a worse prognosis for these patients and more difficult cases to manage later for neurosurgeons.1 , 4, 6, 7 , 14 Jayakumar et al.1 have advised neurosurgical centers across the world to be ready for an increased demand on resources as referrals and operative volumes begin to increase once the COVID-19 pandemic has slowed. With the easing of the lockdown in India and establishment of evidence-based protocols for COVID-19 testing, we were able to increase our nonemergent operative workflow. However, this process of recovery was again halted by an increasing number of COVID-19 cases and depleted workforce because many healthcare workers had contracted COVID-19. Thus, we were again forced to decrease our nonemergent cases to be able to deploy more healthcare workers to caring for patients with COVID-19. We must rise above the challenge and again attempt to resume work with the necessary precautions.15 Proper evidence-based protocols, creation of adequate COVID-19 testing facilities, and the provision of ample personal protective equipment have been instrumental in restarting nonemergent surgeries in our experience.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Jayakumar N., Kennion O., Villabona A.R., Paranathala M., Holliman D. Neurosurgical referral patterns during the COVID-19 pandemic: a United Kingdom experience. World Neurosurg. 2020;144:e414–e420. doi: 10.1016/j.wneu.2020.08.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reid D. India confirms its first coronavirus case. CNBC. January 30, 2020. https://www.cnbc.com/2020/01/30/india-confirms-first-case-of-the-coronavirus.html Available at:
- 3.DehradunMarch 15 PT of I, March 15 2020UPDATED: Ist 2020 23:04. Uttarakhand reports first coronavirus case. India Today. https://www.indiatoday.in/india/story/uttarakhand-reports-first-coronavirus-case-1655825-2020-03-15 Available at: Accessed September 2, 2020. [DOI]
- 4.Goyal N., Venkataram T., Singh V., Chaturvedi J. Collateral damage caused by COVID-19: change in volume and spectrum of neurosurgery patients. J Clin Neurosci. 2020;80:156–161. doi: 10.1016/j.jocn.2020.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goyal N., Gupta K. Letter to the Editor Regarding- COVID-19 impact on neurosurgical practice: lockdown attitude and experience of a European academic center. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.09.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venkataram T., Goyal N., Dash C. Impact of the COVID-19 pandemic on neurosurgical practice in India: results of an anonymized national survey. Neurol India. 2020;68:595. doi: 10.4103/0028-3886.289004. [DOI] [PubMed] [Google Scholar]
- 7.Goyal N., Venkataram T., Dash C., Chandra P. Letter to the editor regarding “impact of COVID-19 on an academic neurosurgery department: The Johns Hopkins experience”. World Neurosurg. 2020;143:599–600. doi: 10.1016/j.wneu.2020.07.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khalafallah A.M., Jimenez A.E., Lee R.P. Impact of COVID-19 on an academic neurosurgery department: The Johns Hopkins experience. World Neurosurg. 2020;139:e877–e884. doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deora H., Mishra S., Tripathi M. Adapting neurosurgery practice during the COVID-19 pandemic in the Indian subcontinent. World Neurosurg. 2020;142:e396–e406. doi: 10.1016/j.wneu.2020.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernucci C., Brembilla C., Veiceschi P. Effects of the COVID-19 outbreak in northern Italy: perspectives from the Bergamo neurosurgery department. World Neurosurg. 2020;137:465–468.e1. doi: 10.1016/j.wneu.2020.03.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antony J., James W.T., Neriamparambil A.J., Barot D.D., Withers T. An Australian response to the COVID-19 pandemic and its implications on the practice of neurosurgery. World Neurosurg. 2020;139:e864–e871. doi: 10.1016/j.wneu.2020.05.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilligan J., Gologorsky Y. Collateral damage during the coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;140:413–414. doi: 10.1016/j.wneu.2020.05.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal N., Venkataram T., Dash C., Chandra P.P. Letter to the Editor regarding “COVID-19’s Impact on Neurosurgical Training in Southeast Asia”. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.08.190. [DOI] [PubMed] [Google Scholar]
- 14.Venkataram T., Goyal N., Kalita D. Deployment of neurosurgeons at the warfront against COVID-19. World Neurosurg. 2020;144:e561–e567. doi: 10.1016/j.wneu.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dash C., Venkataram T., Goyal N. Neurosurgery training in India during COVID-19 pandemic: Straight from the horse’s mouth. Neurosurg Focus. 2020 doi: 10.3171/2020.9.FOCUS20537. [DOI] [PubMed] [Google Scholar]