Abstract
Lung transplantation from a donor previously infected with SARS-CoV-2
In late 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its resulting respiratory disease, COVID-19, emerged.1 As the pandemic continues, with more than 62 million people with documented SARS-CoV-2 infection, a growing number of potential organ donors will have been infected. Since SARS-CoV-2 resides primarily in the respiratory tract, lung transplantation has the highest concern in terms of donor-derived viral transmission and impaired graft quality. Therefore, graft acceptance for lung transplantation should carefully be balanced against the longer waiting time for the recipient.2, 3 So far, to our knowledge, there have been no published reports of lung transplantation from a donor with previous COVID-19. We describe a successful double-lung transplantation from a donor who recovered from SARS-CoV-2 infection with screening of different specimens for SARS-CoV-2 during procurement and transplantation (figure 1 ; video). Approval for reporting was granted by the ethics committee of the University Hospitals Leuven (S52174).
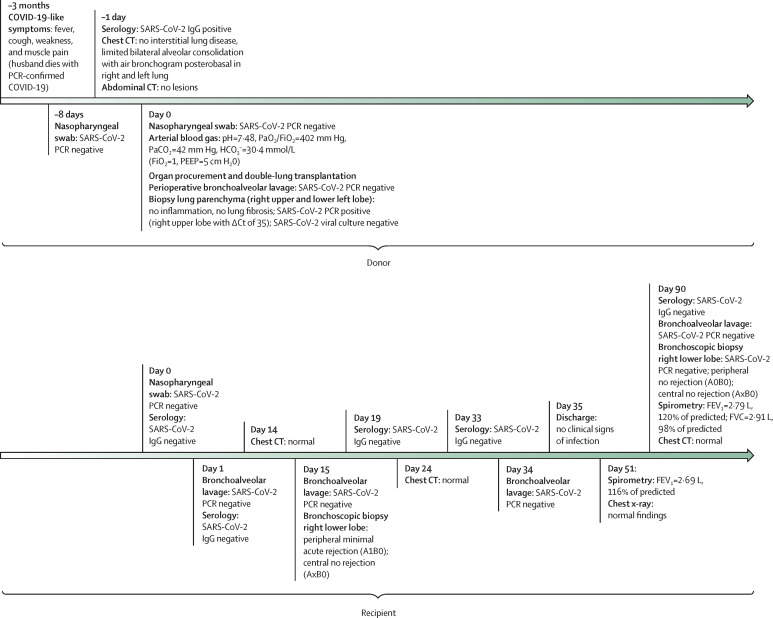
Figure 1.
Chronological overview of transplant specimen analyses
In-house multiplex real-time PCR was used for detection of respiratory bacteria, viruses, and fungi. Normal on chest CT is defined as normal postoperative changes, excluding any signs of fibrosis or infection. FVC=forced vital capacity. HCO3–=bicarbonate. PaCO2=partial pressure of arterial carbon dioxide. PaO2/FiO2=ratio of partial pressure of arterial oxygen to fractional concentration of oxygen in inspired air. PEEP=positive end-expiratory pressure. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
A 61-year-old woman with end-stage chronic obstructive pulmonary disease, not treated with chronic corticosteroids, received a donor offer 7 months after listing for double-lung transplantation. The donor was a 72-year-old woman with a hypertensive intracerebral haemorrhage who was eligible for donation after circulatory determination of death. In our lung transplantation programme, median donor age is 55 years and 30% of donations are from patients with circulatory death.4, 5
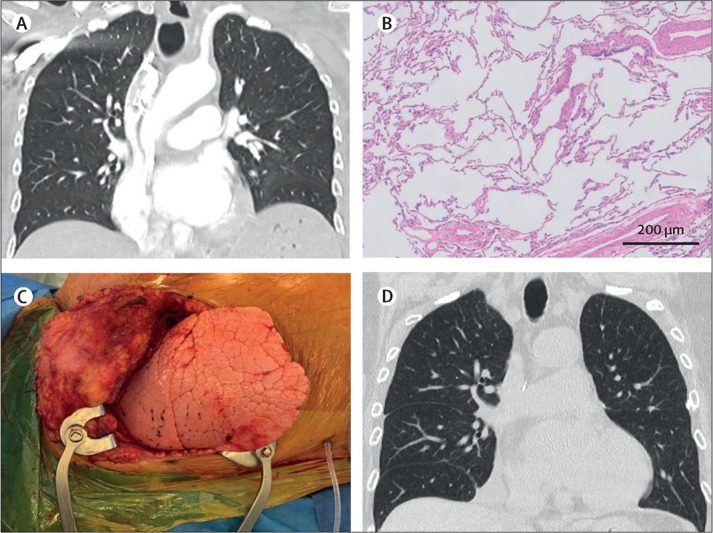
The donor had no medical history and had never smoked. In April, 2020, 3 weeks after the start of the COVID-19 epidemic in Belgium, she developed COVID-19-like symptoms, including fever, cough, weakness, and muscle pain, which lasted for 2 weeks (appendix p 1). She was not screened for SARS-CoV-2 because of low testing capacity. She was asked to isolate for 2 weeks, during which time her husband with whom she was isolating was admitted to hospital and died from PCR-confirmed COVID-19. 3 months later, in July, when she was admitted to hospital with intracranial bleeding, nasopharyngeal swab SARS-CoV-2 PCR was negative, but serology showed positive SARS-CoV-2 IgG antibodies (Abbott Architect SARS-CoV-2 IgG-assay; Lake Forest, IL, USA), indicating previous exposure to the virus (appendix p 1). Liver and kidney function were normal (appendix p 2). A donation after circulatory death III procedure was engaged 8 days later. SARS-CoV-2 PCR on nasopharyngeal swab was repeated (8 h before donation) and remained negative. Lower lobe bronchoalveolar lavage was negative for (myco)bacterial and fungal cultures as well as for SARS-CoV-2 PCR. No pulmonary infiltrates or signs of interstitial lung disease were seen on chest CT scan (figure 2A ). Partial pressure of arterial oxygen was 402 mm Hg (fractional concentration of oxygen in inspired air was 100% and positive end-expiratory pressure was 5 cm H2O; appendix p 3).
Figure 2.
Imaging of the donor lungs
(A) Chest CT scan of lung allografts before donation excluding inflammation or lung fibrosis (coronal plane). (B) Histology of the peripheral lung biopsy sample revealing normally preserved lung parenchyma without inflammation or fibrotic changes. Arteries are normal, without vasculopathy or thrombi (haematoxylin and eosin). (C) Macroscopic picture of the right donor lung after implantation. (D) Chest CT at 3-month follow-up excluding ground glass opacities, reticular changes, inflammation, or lung fibrosis (coronal plane).
The donor lungs were accepted after multidisciplinary agreement and according to the International Society for Heart and Lung Transplantation (ISHLT) guidelines on COVID-19.6 Following our national legislation (appendix p 4), the recipient consents before listing to allow physicians to accept or decline an organ on the basis of their clinical judgment. No specific consent is required for extended-criteria donors, including those with previous COVID-19. The liver was allocated for a high-urgency transplantation elsewhere. Ventilator switch-off resulted in circulatory arrest 23 min later. 5 min after circulatory arrest, an incision was made and perfusion with low-potassium dextran solution started. Macroscopic analysis showed good compliance and minor emphysema. Ex-vivo lung perfusion was not required. Because of two parenchymal tears related to lung extraction, two peripheral donor lung biopsy samples (right upper and left lower lobes) could be analysed histologically, demonstrating mild subpleural emphysema, but no signs of COVID-19-induced injury, nor fibrotic sequelae (figure 2B). The right lung biopsy sample had low levels of PCR-amplified SARS-CoV-2 RNA (DCt was 35), but a negative viral culture (appendix p 5).
Pretransplant recipient assessment showed negative SARS-CoV-2 PCR on nasopharyngeal swab and negative serology. Bilateral sequential lung transplantation was done via anterolateral thoracotomy without extracorporeal life support. The right lung was reperfused after 357 min of ischaemia (figure 2C) and the left lung after 518 min (appendix p 6). Standard immunosuppression was administered: antithymocyte globulin (3 days), tacrolimus, mycophenolate mofetil, and methylprednisolone (appendix p 7). Standard treatment consisted of nystatin, azithromycin, acyclovir, sulfamethoxazole–trimethoprim, and amphotericin-B aerosols.
The patient was extubated after 2 days. Primary graft dysfunction scores were 0 at 0 h, 1 at 24 h, and 0 at 48 h and 72 h after transplantation.7 6 days after lung transplantation, the patient was discharged from the intensive care unit. Postoperative complications were minimal acute rejection (A1B0) 15 days after transplantation, requiring methylprednisolone, and left-side pneumothorax due to a dislocated chest tube, requiring CT-guided drainage at day 24. The patient was discharged 35 days after surgery.
SARS-CoV-2 PCR and viral culture of bronchoalveolar lavage samples collected 15 days, 34 days, and 90 days after lung transplantation were negative. Also, SARS-CoV-2 IgG remained negative at 3 months. Routine chest CT on days 14, 24, and 90 (figure 2D) showed normal post-transplant changes without lung injury. At day 90, spirometry was normal (FEV1 of 2·79 L, 120% of predicted; forced vital capacity of 2·91 L, 98% of predicted) and a peripheral lung biopsy sample was negative for SARS-CoV-2 PCR. The liver transplant recipient tested negative after transplantation for SARS-CoV-2 on bronchoalveolar lavage.
In contrast to several viral disease outbreaks in the past, such as Ebola, the 2003 SARS-CoV, West Nile virus, or pandemic influenza H1N1, which remained manageable and mostly limited geographically, the ongoing COVID-19 pandemic is unprecedented in modern times.2 In the future, more donors will have a history of SARS-CoV-2. It is generally accepted that lungs from a donor with ongoing SARS-CoV-2 infection should not be transplanted. In the case of a donor with former COVID-19, ISHLT guidelines stipulate that lungs can be assessed and considered for donation in the case of clinical recovery from COVID-19 at least 28 days from symptom onset if two PCR tests (24 h apart) give negative results and no permanent organ damage is detected, as in our case.6
Two unintended transplantations have been described from asymptomatic donors with a SARS-CoV-2 infection in the days following donation.8 The first report described a patient with aplastic anaemia under immunosuppression receiving a platelet transfusion from an asymptomatic donor who was positive for SARS-CoV-2 2 days later. No donor-derived transmission occured.9 The second involved a living related liver donor with SARS-CoV-2 confirmed 3 days after donation.10 SARS-CoV-2 PCR from a liver biopsy sample was negative. Donor-derived transmission was not diagnosed; however, the recipient was prophylactically treated with lopinavir–ritonavir and hydroxychloroquine.
Notably, in our case, a history of SARS-CoV-2 exposure was known before donation, as confirmed by positive serology. Although SARS-CoV-2 PCR analysis on nasopharyngeal swab was repeatedly negative, a weakly positive signal was detected in the lung biopsy sample. This result could be a false positive or might have resulted from residual viral fragments in lung parenchyma. Although rare, prolonged viral shedding (up to 63 days) has been reported from nasopharyngeal and throat swabs, even after seroconversion, but not up to 3 months and from lung tissue, as in our case.11, 12, 13 Therefore, the precise meaning and implication of a high Ct value in lung tissue from an individual exposed to SARS-CoV-2 should be further studied, using orthogonal complementary virus detection methods. In our case, a high Ct value of 35 supports the notion that the risk of infectivity was very low. Bullard and colleagues14 have shown that no positive viral cultures could be obtained with a Ct greater than 24 and the odds of a positive culture were decreased by 32% for each unit increase in Ct.14 In agreement, viral culture on our lung biopsy sample was negative.
If recommendations are followed, the risk of donor-derived transmission for SARS-CoV-2 is very low.2, 6 Therefore, in coming years, the systematic use of rapid and highly sensitive SARS-CoV-2 detection methods will be indispensable for every donation.
One of the outstanding questions about SARS-CoV-2 is its long-term effect on lung health. SARS-CoV-2 might cause lung damage through viral cytotoxicity, acute respiratory distress syndrome (ARDS), capillary thrombosis, drug-induced toxicity, and ventilator-associated injury.15, 16 Although this injury might resolve, it does not preclude alveolar damage, followed by dysregulated repair, irreversible interstitial changes or interstitial lung disease, and respiratory impairment.16, 17, 18, 19 A study of the 2003 SARS-CoV outbreak (8096 cases worldwide) showed that 29 (53%) of 55 patients who recovered had a significant diffusion capacity restriction at 24 months of follow-up, with limited exercise capacity.20 This finding was consistent with CT images demonstrating persistent ground glass or reticular opacities and bronchiectasis suggesting fibrosis. Similar CT images are observed in SARS-CoV-2 survivors. Early interstitial changes were also seen in Middle East respiratory syndrome coronavirus, with evidence of lung fibrosis on CT scans months after recovery.21, 22 A 15-year follow-up of patients who recovered from 2003 SARS-CoV showed that the initial functional decrease mostly recovered over time, but 4–6% of patients had signs of persisting interstitial lung disease.23
During the COVID-19 pandemic, donor history, chest CT, blood-gas analysis, and macroscopic lung compliance should be carefully appraised to exclude early interstitial lung disease stages related to previous SARS-CoV-2 infection. Donors with a mild symptomatic history of COVID-19 should be differentiated from donors with previous ARDS or fibrotic changes on CT, who are at increased risk for development of interstitial lung disease. In the case described here, the CT scan excluded severe lung damage and the oxygenation capacity was excellent. However, long-term follow-up with chest CT in a large group of patients is needed.
In conclusion, we report a successful double-lung transplantation from a donor exposed to SARS-CoV-2 who had mild COVID-19-like symptoms 3 months earlier. Before donation, repeated nasopharyngeal swab was negative for SARS-CoV-2 and chest CT showed no residual signs of lung injury. The lungs were successfully transplanted without viral transmission to the recipient, as shown by repetitive bronchoalveolar lavage and serology after transplantation. Initial recovery up to day 90 after lung transplantation has been excellent, but long-term results are awaited. We encourage other transplantation centres to report their experience of donors with previous SARS-CoV-2 infection to better inform the transplant community and general population.
Acknowledgments
Acknowledgments
We thank all members of the the Department of Thoracic Surgery, Laboratory of Respiratory Diseases and Thoracic Surgery (BREATHE), transplant coordinators, anaesthesiologists, and pulmonologists involved in the Lung Transplant Program at the University Hospitals Leuven, Belgium, for their contributions. We thank Herman Nys (Interfaculty Centre for Biomedical Ethics and Law at the KU Leuven, Leuven, Belgium) for his contribution.
Contributors
LJC, JVS, EVW, GMV, DEVR, and RV were involved in the conception and design of the work. All authors were involved in acquisition, analysis, and interpretation of data, and all assisted in writing and approving the final draft of the manuscript. LJC, JVS, and RV accessed and verified the data. All authors had access to all the data reported.
Declaration of interests
LJC is supported by a KU Leuven University Chair funded by Medtronic and a postdoctoral grant from University Hospitals Leuven (KOOR-UZ Leuven). AV is supported by a fundamental research grant from the research foundation Flanders (FWO). GMV and DEVR are supported by a grant from the Broere Charitable Foundation. RV is supported as a senior clinical research fellow by FWO. All other authors declare no competing interests.
Supplementary Material
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar D, Manuel O, Natori Y, et al. COVID-19: A global transplant perspective on successfully navigating a pandemic. Am J Transplant. 2020;20:1773–1779. doi: 10.1111/ajt.15876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kates OS, Fisher CE, Rakita RM, Reyes JD, Limaye AP. Use of SARS-CoV-2-infected deceased organ donors: should we always “just say no?”. Am J Transplant. 2020;20:1787–1794. doi: 10.1111/ajt.16000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Somers J, Ruttens D, Verleden SE, et al. A decade of extended-criteria lung donors in a single center: was it justified? Transpl Int. 2015;28:170–179. doi: 10.1111/tri.12470. [DOI] [PubMed] [Google Scholar]
- 5.Ruttens D, Martens A, Ordies S, et al. Short- and long-term outcomes after lung transplantation from circulatory-dead donors: a single-center experience. Transplantation. 2017;101:2691–2694. doi: 10.1097/TP.0000000000001678. [DOI] [PubMed] [Google Scholar]
- 6.Aslam S, Danziger-Isakov L, Luong M, et al. Guidance from the International Society of Heart and Lung Transplantation regarding the SARS CoV-2 pandemic. Aug 19, 2020. https://ishlt.org/ishlt/media/documents/SARS-CoV-2_-Guidance-for-Cardiothoracic-Transplant-and-VAD-centers.pdf
- 7.Snell GI, Yusen RD, Weill D, et al. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction, part I: definition and grading-a 2016 consensus group statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2017;36:1097–1103. doi: 10.1016/j.healun.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Kates OS, Fisher CE, Rakita RM, Reyes JD, Limaye AP. Emerging evidence to support not always ”just saying no” to SARS-CoV-2 positive donors. Am J Transplant. 2020 doi: 10.1111/ajt.16119. published online June 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho HJ, Koo JW, Roh SK, et al. COVID-19 transmission and blood transfusion: a case report. J Infect Public Health. 2020;13:1678–1679. doi: 10.1016/j.jiph.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong HL, Kim SH, Choi DL, Kwon HH. A case of coronavirus disease 2019-infected liver transplant donor. Am J Transplant. 2020;20:2938–2941. doi: 10.1111/ajt.15997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 12.Widders A, Broom A, Broom J. SARS-CoV-2: The viral shedding vs infectivity dilemma. Infect Dis Health. 2020;25:210–215. doi: 10.1016/j.idh.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu WD, Chang SY, Wang JT, et al. Prolonged virus shedding even after seroconversion in a patient with COVID-19. J Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bullard J, Dust K, Funk D, et al. Predicting infectious SARS-CoV-2 from diagnostic samples. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa638. published online May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spagnolo P, Balestro E, Aliberti S, et al. Pulmonary fibrosis secondary to COVID-19: a call to arms? Lancet Respir Med. 2020;8:750–752. doi: 10.1016/S2213-2600(20)30222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naik PK, Moore BB. Viral infection and aging as cofactors for the development of pulmonary fibrosis. Expert Rev Respir Med. 2010;4:759–771. doi: 10.1586/ers.10.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grillo F, Barisione E, Ball L, Mastracci L, Fiocca R. Lung fibrosis: an undervalued finding in COVID-19 pathological series. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30582-X. published online July 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu J, Xu X, Jiang L, Dua K, Hansbro PM, Liu G. SARS-CoV-2 induces transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respir Res. 2020;21:182. doi: 10.1186/s12931-020-01445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15:543–550. doi: 10.1111/j.1440-1843.2010.01720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Franquet T, Jeong YJ, Lam HYS, et al. Imaging findings in coronavirus infections: SARS-CoV, MERS-CoV, and SARS-CoV-2. Br J Radiol. 2020;93 doi: 10.1259/bjr.20200515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Das KM, Lee EY, Singh R, et al. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J Radiol Imaging. 2017;27:342–349. doi: 10.4103/ijri.IJRI_469_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang P, Li J, Liu H, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020;8:8. doi: 10.1038/s41413-020-0084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lung transplantation from a donor previously infected with SARS-CoV-2