Corresponding Author

Key Words: COVID-19, heart failure, hospitalization, mortality, risk
The coronavirus disease-2019 (COVID-19) pandemic continues to stress the capacity of health care systems worldwide with an influx of patients hospitalized with severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Along with the exponential growth of infected individuals has come a supply−demand mismatch of the U.S. health care system, which has resulted in a never-before witnessed emphasis on clinical triage and medical resource rationing in a wartime-like environment (1). Recognizing risk factors and identifying high-risk patients will allow appropriate triage and resource allocation.
Several large registries have demonstrated a high degree of morbidity and mortality in patients with pre-existing cardiovascular disease and other chronic comorbidities who are infected with COVID-19 (2,3). Seemingly overnight, almost all Americans have become versed in the phrase “pre-existing conditions.”
In this issue of the Journal, Alvarez-Garcia et al. (4) report on the outcomes of patients with heart failure hospitalized with COVID-19 across the Mount Sinai Healthcare System. A strength of this study is the large number of ethnically diverse patients with laboratory-confirmed COVID-19 (n = 6,439), with 422 patients having a history of heart failure before admission. This analysis is the largest reported COVID-19 cohort with heart failure to date, with a smaller Italian-based population identifying <100 patients with antecedent heart failure (5).
The overall mortality rate of 25% is consistent with that seen in other large registries, whereas a humbling 40% of those with heart failure died during hospitalization (6,7). The heart failure cohort witnessed a near doubling in the mortality risk and a substantially increased risk of intubation and mechanical ventilation that was independent of left ventricular ejection fraction, and surprisingly, race. The highest risk cohort was, not surprisingly, those patients with New York Heart Association functional class III and/or IV heart failure and/or moderate or severe mitral regurgitation at baseline. Although significant attention has been paid to biomarkers of late, the current study suggests that antecedent heart failure remains a powerful predictor of outcomes, regardless of D-dimer and troponin levels. Brain natriuretic peptide is not a predictor of mortality (8). Furthermore, use of renin-angiotensin-aldosterone inhibitors was not associated with adverse cardiovascular outcomes, underscoring the importance of continued drug adherence.
The high mortality associated with COVID-19 in heart failure cannot be overemphasized because this population represents a unique and high-risk substrate, with recent data demonstrating a direct infection of cardiac myocytes with SARS-CoV-2 on autopsy (9). In this light, heart failure is perhaps the most significant pre-existing condition that should be recognized. Although much emphasis has been placed on pathophysiological mechanisms in COVID-19, exact mechanism and degree of injury to the myocardium still needs to be understood. Myocardial inflammation and injury have been described, although the nature of worsening function among pre-existing heart failure needs to be documented. Whether this pattern of worsened outcomes among patients with heart failure is unique to COVID-19 or similar to that seen in any other systemic inflammatory state is not clear. Unfortunately, in the current study, only 19% of the patients with heart failure underwent an echocardiogram. In a recent paper, up to three-quarters of the population had abnormalities on cardiac magnetic resonance imaging, independent of pre-existing conditions, severity and overall course of the acute illness, and time from the original diagnosis.
As the recognition of high-risk populations continues to emerge and attempts to understand the mechanism of injury are underway, efforts need to be made on the safe and timely delivery of care to the high-risk groups. Prevention should be the initial step to minimize exposure and provide timely care to patients with heart failure. That there is a delay in getting treatment and fewer clinic visits, which further affects outcomes, is already known (10,11). To this regard, greater use of telemedicine may be useful and has transformed the delivery of care paradigm in the evolving health care environment (12). However, wide adoption would require overcoming barriers to equitable access to basic technology, education, and remote monitoring tools among at-risk communities.
Surprisingly, in the current report, race did not appear to be a factor associated with prognosis among the patients with heart failure. This is in contrast to several other reports, albeit in a general population with a predisposition for infection and worse outcomes among African Americans (7,13). Whether this reflects cardioprotection from high use of guideline-driven medical therapy in the current cohort compared with the general population with variable degree or poor control of other chronic risk factors is not yet known and begs more investigation. In the interim, safety of angiotensin-converting enzyme inhibitors use among patients with heart failure is confirmed and should not be discontinued. Further investigation on in-hospital care settings, team structures (specialist vs. hospitalist) and relationship to outcomes are needed for better understanding of optimal resource and health care staffing, capacity building, and preparation for ongoing pandemic and future scenarios.
The pandemic has rightfully placed significant emphasis on treatment of all patients with SARS-CoV-2, but we need to remind ourselves of another harsh reality: >6 million U.S. adults have heart failure; they represent among the highest risk subset of potential COVID-19 infections and worse outcomes, including a 2-fold risk of death, need for prolonged length of stay, and mechanical intubation (4,14).
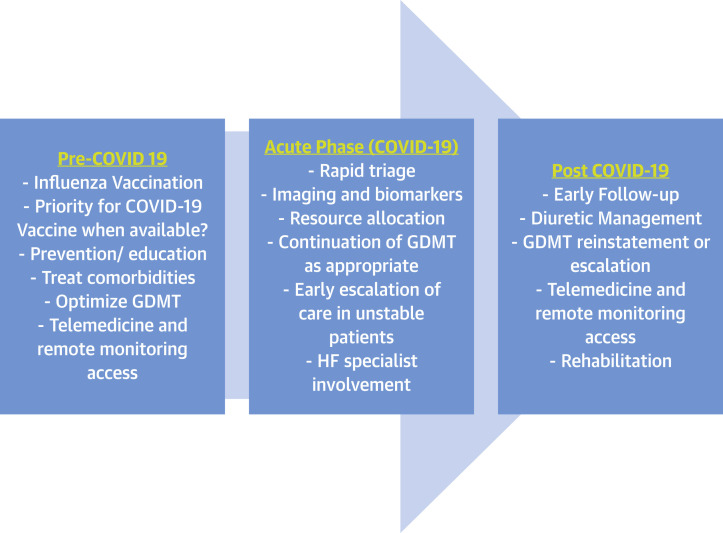
Future efforts need to be made toward further elucidating the mechanism and durability of injury by COVID-19 among patients with antecedent heart failure, instituting widespread prevention, and appropriating triage of suspected infections and resource allocation. This includes timely access to vaccines when available, widespread use of influenza vaccine, and continuation or reinstatement of appropriate guideline-driven medical therapy, as well as timely follow-up and access to telemedicine to reduce the risk of worsened prognosis and to facilitate recovery (Figure 1 ). As the pandemic continues to ravage communities, pathways for care specific to heart failure care need to be created, keeping in mind pre-existing conditions, and tailored to resources available in the health care systems and the communities they serve.
Figure 1.
Framework for the Care of Patients With HF Pre-COVID-19, During Acute Phase, and Post-COVID-19
Care of heart failure patient with COVID-19. COVID-19 = coronavirus disease-2019; HF = heart failure; GDMT = guideline-driven medical treatment.
Author Relationship With Industry
Drs. Panjrath and Krepp have received personal fees from Pfizer Inc.
Footnotes
Lisa A. Mendes, MD, served as Guest Associate Editor for this paper. Athena Poppas, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 2.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Alvarez-Garcia J., Lee S., Gupta A. Prognostic impact of prior heart failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76:2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lombardi C.M., Carubelli V., Iorio A. Association of troponin levels with mortality in Italian patients hospitalized with coronavirus disease 2019: results of a multicenter study. JAMA Cardiol. 2020;26 doi: 10.1001/jamacardio.2020.3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta S., Hayek S.S., Wang W. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020:e203596. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandoval Y., Januzzi J.L., Jr., Jaffe A.S. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020;76:1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindner D., Fitzek A., Brauninger H. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhatt A.S., Moscone A., McElrath E.E. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall M.E., Vaduganathan M., Khan M.S. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail. 2020;26:462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorodeski E.Z., Goyal P., Cox Z.L. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26:448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yehia B.R., Winegar A., Fogel R. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 US hospitals. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.18039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Virani S.S., Alonso A., Benjamin E.J. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]