Highlights
-
•
Perceived vulnerability to COVID-19 (PVC) was positively related to COVID-19-related worries, social isolation, and traumatic stress (TS).
-
•
Both COVID-19-related worries and social isolation were significant mediators of the relationship between PVC and TS.
-
•
The indirect effect of PVC on TS through COVID-19-related worries was stronger for participants who reported greater social isolation.
-
•
Social isolation and disease-related worries may be important variables that can be targeted in interventions to reduce pandemic-related TS.
Keywords: Coronavirus disease (COVID-19), Perceived vulnerability to COVID-19, COVID-19-related worries, Social isolation, Traumatic stress
Abstract
The purpose of the present study was to propose and test two models to understand the relationship between perceived vulnerability to COVID-19 (PVC) and COVID-19-related traumatic stress (TS), as well as the variables that may mediate and moderate this relationship among individuals who have not yet been infected with COVID-19. Using an online survey, data were collected between late March and early April 2020. Participants were recruited through Amazon Mechanical Turk and included 747 adults living in the United States. Supporting our hypotheses, results indicated that both COVID-19-related worries and social isolation were significant mediators of the relationship between PVC and TS (Model 1). In addition, the results of a moderated mediation analysis indicated that the indirect effect of PVC on TS through COVID-19-related worries was stronger for participants who reported greater social isolation (Model 2). Although future research is needed, these findings suggest that both social isolation and disease-related worries may be important variables that can be targeted in interventions to reduce pandemic-related TS.
1. Introduction
The Coronavirus Disease (COVID-19) pandemic, which initially started as an outbreak in China in late December of 2019, has spread globally and resulted in over 24 million infections and more than 838,000 deaths worldwide, as of August 30, 2020 (World Health Organization, 2020). In addition to its health consequences, the rapid spread of COVID-19 and the resulting disease containment efforts (e.g., border closures, travel restrictions, school and business closures, and quarantine) have brought about a multitude of challenges and stressors, such as disruptions in daily activities, loss of jobs, and increased social isolation worldwide. Given this broad range of consequences, the COVID-19 pandemic is not only a serious threat to physical health, but it also poses a critical threat to mental health worldwide.
Findings from earlier epidemics (e.g., the severe acute respiratory syndrome [SARS] epidemic, the Ebola epidemic; for reviews see Boyraz & Legros, 2020; Taylor, 2019) and recent COVID-19 literature (e.g., Casagrande, Favieri, Tambelli, & Forte, 2020; Wang et al., 2020) suggest that many people experience declines in their well-being and report anxiety and stress-related symptoms following infectious disease outbreaks. In light of this literature, Taylor and colleagues (Taylor et al., 2020a, 2020b) conceptualized the COVID-19-related distress (i.e., COVID stress syndrome) as a multifaceted construct that includes COVID-19-related fears (i.e., fears about contamination and economic consequences; fear of foreigners who may have COVID-19), compulsive checking, and traumatic stress (TS) symptoms (e.g., intrusive thoughts and nightmares about COVID-19). In the present study, we focused on the TS component of COVID-19-related distress and examined the factors that may contribute to TS among individuals who have not been infected COVID-19.
Recent evidence suggests that a substantial portion of the population has experienced at least moderate levels of TS following the COVID-19 outbreak (e.g., Casagrande et al., 2020; Forte, Favieri, Tambelli, & Casagrande, 2020; González-Sanguino et al., 2020; Jiang, Nan, Lv, & Yang, 2020; Sun et al., 2020). For example, in a study with a Chinese sample of adults, 6.1 % of the participants reported severe TS symptoms, and an additional 13.0 % reported moderate TS symptoms after the COVID-19 outbreak (Jiang et al., 2020). In another recent study with a sample of adults from Italy, 29.5 % of the participants reported COVID-19-related TS symptomatology (Forte et al., 2020).
The prevalence of TS symptomatology appears to be particularly high among individuals who had more direct exposure to COVID-19 (e.g., COVID-19 patients or individuals who are suspected to have COVID-19) (e.g., Bo et al., 2020; González-Sanguino et al., 2020; Sun et al., 2020); however, findings suggest that the COVID-19 pandemic can trigger TS reactions even among relatively low risk populations that are not directly affected by COVID-19 (Sun et al., 2020). Further, in a study with a Chinese sample, the level of COVID-19 exposure was a significant predictor of TS among participants who reported mild symptoms of TS, but not among those who reported moderate or severe TS symptomatology (Jiang et al., 2020). Therefore, TS reactions to COVID-19 may vary not only as a function of the level of COVID-19 exposure but also due to other factors, such as individuals’ beliefs and perceptions related to COVID-19.
For example, considering that COVID-19 can be fatal, individuals who perceive their likelihood of infection as high may experience this pandemic as more personally life-threatening and experience greater TS than those who perceive themselves as less vulnerable to COVID-19. Indeed, research suggests that perceived health threats can trigger TS reactions (e.g., Laubmeier & Zakowski, 2004; Meli, Kautz, Julian, Edmondson, & Sumner, 2018) and may have stronger effects on TS than objective health threats (Laubmeier & Zakowski, 2004). Drawing from these results and other relevant literature (e.g., Ahorsu et al., 2020; Ehlers & Clark, 2000; Ho, Kwong-Lo, Mak, & Wong, 2005; Park, Ju, Ohs, & Hinsley, 2020), we conceptualized and tested two models in the present study to examine the relationship between perceived vulnerability to COVID-19 (PVC; perceived likelihood of contracting COVID-19) and TS, as well as the variables that may mediate and moderate this relationship among individuals who have not been infected with COVID-19.
1.1. COVID-19-related worries and social isolation as mediators of the relationship between perceived vulnerability to COVID-19 and traumatic stress symptoms (Model 1)
People generally underestimate their vulnerability to infectious diseases or other illnesses (Weinstein, 1982, 1987); however, considering the rapid-spreading and life-threatening nature of COVID-19, as well as other factors related to COVID-19 (e.g., lack of approved vaccines for COVID-19, ongoing exposure to COVID-19-related content through the media and other sources), it is reasonable to assume that the current pandemic has generated a widespread sense of vulnerability. Indeed, a study that included national samples from ten countries in Europe, America, and Asia indicated that the COVID-19-related risk perception (i.e., perceived likelihood of oneself or family member/friend contracting COVID-19, perceived seriousness of the pandemic, and COVID-19-related worries) was high across all samples between March and April 2020 (Dryhurst et al., 2020).
Perceiving oneself vulnerable to COVID-19 may serve adaptive functions by motivating individuals to adopt self-protective behaviors (e.g., Park et al., 2020); however, a strong sense of vulnerability during this pandemic may undermine people’s sense of safety or control, which may increase COVID-19-related worries (e.g., fear of infection, feelings of insecurity and loss of control) and trigger TS reactions. Indeed, recent findings suggest that higher PVC is associated with increased fear and anxiety about COVID-19 (Ahorsu et al., 2020; Park et al., 2020). In addition, both recent COVID-19 literature (Taylor et al., 2020a) and past research (e.g., SARS literature, Ho et al., 2005) suggest that individuals who experience more disease-related worries (e.g., fear of infection, feeling unsafe about oneself) during infectious disease outbreaks report higher TS. Thus, we predicted that higher levels of PVC may increase COVID-19-related worries, which in turn may trigger TS reactions during this pandemic. This hypothesis is also consistent with the cognitive model of posttraumatic stress disorder (PTSD) (Ehlers & Clark, 2000) which posits that psychological reactions to a traumatic event vary as a function of how the event is appraised (e.g., appraisals of danger lead to fear) and that the development of PTSD is more likely when individuals’ appraisals create a “sense of serious current threat” (p. 320).
The effects of PVC and COVID-19-related worries on TS may be further mediated by social isolation. Experimental findings suggest that people rate themselves as less extraverted (Mortensen, Becker, Ackerman, Neuberg, & Kenrick, 2010) and show less need to belong after experimental activation of disease concerns (Sacco, Young, & Hugenberg, 2014). In addition, it has been reported that an increased sense of vulnerability to disease leads to heightened sensitivity to disease cues, interpersonal avoidance, and cognitive biases or extreme attitudes that may reduce affiliation with others, particularly when the potential threat of infection becomes salient (e.g., Duncan & Schaller, 2009; Miller & Maner, 2012; Mortensen et al., 2010; see Neuberg, Kenrick, & Schaller, 2011). For example, in a study conducted by Mortensen et al. (2010), participants with higher vulnerability to disease rated themselves lower on the openness and agreeableness domains of personality following an infectious disease prime (vs. a control prime). On the other hand, the effect of the disease prime on personality ratings was not significant among participants who perceive themselves less vulnerable to infectious disease (Mortensen et al., 2010). A second experiment conducted by these authors indicated that the disease prime (vs. the control prime) resulted in interpersonal avoidance behaviors (i.e., motor movements that facilitate interpersonal avoidance when participants were shown pictures of neutral faces) only among participants with higher perceived vulnerability to disease (Mortensen et al., 2010).
Taken together, higher levels of PVC and COVID-19-related worries may trigger cognitive biases or interpersonal avoidance behaviors that may reduce one’s social connectedness. While this may help protect oneself from COVID-19, it can also lead to an increased sense of social isolation during this pandemic. Social isolation or lack of social support increases the risk of PTSD following traumatic events (for a meta analysis, see Ozer, Best, Lipsey, & Weiss, 2003), including infectious disease outbreaks (see Boyraz & Legros, 2020). Therefore, we anticipated that, higher levels of PVC and the resulting COVID-19-related worries may increase perceived social isolation, which in turn, may contribute to TS. We hypothesized, specifically that a) PVC would be positively associated with COVID-19-related worries, social isolation, and TS, b) COVID-19-related worries would be positively associated with social isolation and TS, c) social isolation would be positively associated with TS, and d), the relationship between PVC and TS would be mediated by COVID-19-related worries and social isolation.
1.2. Social isolation as a moderator of the indirect relationship between perceived vulnerability to COVID-19 and traumatic stress symptoms (Model 2)
In light of theory and empirical findings, social isolation can also be construed as a moderator of the relationship between COVID-19-related worries and TS. The stress-buffering hypothesis and supporting empirical research (e.g., Cohen & Hoberman, 1983; Cohen & Wills, 1985) suggest that social support helps individuals better regulate their psychological and physiological reactions to stress in threatening situations and thereby modulates the effect of stress on pathological stress reactions. Social isolation, on the other hand, can lead to various mental and physical health problems (e.g., stress, anxiety, depressive symptoms, cardiovascular disease, and sleep problems), as well as impairments in self-regulation of behaviors, cognitions, and emotions (for a review, see Hawkley & Cacioppo, 2010). Individuals who perceive themselves as being socially isolated appraise daily stressors as more severe and engage in more passive coping mechanisms than those who perceive themselves as being socially connected (for a review, see Cacioppo & Hawkley, 2003). Thus, COVID-19-related worries may be more likely to escalate into maladaptive traumatic stress reactions among those who feel more socially isolated because these individuals may interpret and deal with their worries in a way that exacerbates rather than ameliorates their fears and perceptions of threat.
Further, social isolation is itself a significant stressor that activates psychological and physiological stress responses (e.g., neuroendocrine and cardiovascular responses) (see Cohen, 2004) and a significant predictor of TS in the face of life-threatening infectious disease outbreaks (see Boyraz & Legros, 2020). Accordingly, it is plausible to suggest that a combination of high levels of COVID-19-related worries and social isolation may carry a greater risk of triggering TS reactions than the presence of one of these risk factors alone. Consistent with this idea, we tested an alternative model in which social isolation served as a moderator, rather than a mediator of the relationship between COVID-19-related worries and TS. We hypothesized that social isolation would moderate the indirect effect (via COVID-19-related worries) of PVC on TS by strengthening the effect of COVID-19-related worries on TS.
We controlled for age, gender, pre-existing medical conditions (PEMC) and mental health conditions (PEMHC) as control variables in both hypothesized models due to potential effects of these variables on our outcome variables. Some of these variables have been identified as risk factors for PTSD. Specifically, it has been reported in trauma literature that women (for a review, see Tolin & Foa, 2006) and individuals with a history of mental health disorders (for a meta analysis, see Brewin, Andrews, & Valentine, 2000) are at heightened risk of developing PTSD following traumatic events. In addition, younger adults and women reported more distress and TS after the COVID-19 outbreak than older adults and men (see Boyraz & Legros, 2020). Although PEMC do not necessarily increase the risk of TS, we included it as a control variable in our analyses because individuals with certain medical conditions, such as diabetes and heart disease are more susceptible to COVID-19 (Centers for Disease Control & Prevention, 2020); thus, they may experience more COVID-19-related worries during this pandemic.
2. Method
2.1. Participants and procedures
Participants of this study included adults living in the United States who were recruited through Amazon Mechanical Turk (MTurk) to complete an online survey. The data collection took place between March 26 and April 6, 2020. All participants who completed the survey appropriately received a $3 payment. Although 799 adults participated in the study, 42 of these individuals were not included in the analyses either because they did not complete all study questionnaires, or they failed one or both of the attention check questions we included in the survey. In addition, three participants who tested positive for COVID-19 and seven participants who identified their gender as “non-binary” or “other” were not included in the final analyses due to insufficient sample size in these groups. The final sample included 747 adults whose ages ranged from 22 to 76 (Mage = 41.26, SD = 11.57). Approximately half of the participants were women (n = 366, 49.0 %) and 51.0 % (n = 381) were men. Descriptive information about participants’ other demographic characteristics and their exposure to COVID-19 is presented in Table 1 .
Table 1.
Demographic Characteristics of the Sample and COVID-19 Exposure.
| Variable | n | % |
|---|---|---|
| Ethnicity | ||
| American Indian/Alaskan Native | 5 | .70 |
| Black/African American | 52 | 7.0 |
| Asian/Asian American | 50 | 6.7 |
| Hispanic/Latinx | 26 | 3.5 |
| White/European American | 587 | 78.6 |
| Middle Eastern | 5 | .70 |
| Biracial/Multiracial | 19 | 2.5 |
| Other | 3 | .40 |
| Education | ||
| Less than high school | 2 | .30 |
| High school degree or equivalent (e.g., GED) | 104 | 13.9 |
| Some college but no degree | 152 | 20.3 |
| Associate degree | 91 | 12.2 |
| Bachelor’s degree | 319 | 42.7 |
| Master’s degree | 65 | 8.7 |
| Doctoral degree | 11 | 1.5 |
| Other | 3 | .40 |
| Employment Status | ||
| Employed for wages (part-time or full-time) | 500 | 66.9 |
| Self-employed | 155 | 20.7 |
| Unemployed and currently looking for work | 19 | 2.5 |
| Unemployed and not currently looking for work | 11 | 1.5 |
| Homemaker | 15 | 2.0 |
| Student | 7 | .90 |
| Retired | 28 | 3.7 |
| Unable to work | 7 | .90 |
| Other | 5 | .70 |
| Have you been in contact with an infected person? | ||
| Uncertain | 238 | 31.9 |
| No | 502 | 67.2 |
| Yes | 7 | .90 |
| Has a member of your family been infected with Coronavirus? | ||
| Uncertain | 91 | 12.2 |
| No | 648 | 86.7 |
| Yes | 8 | 1.1 |
| Do you live in the same household as a suspected or confirmed Coronavirus infected person? | ||
| Uncertain | 24 | 3.2 |
| No | 715 | 95.7 |
| Yes | 8 | 1.1 |
| Have you been tested for Coronavirus? | ||
| No | 740 | 99.1 |
| Yes | 7 | .90 |
| Do you personally know someone who has died of Coronavirus? | ||
| No | 725 | 97.1 |
| Yes | 22 | 2.9 |
2.2. Measures
2.2.1. Demographic questionnaire and COVID-19-exposure
Prior to completing the study questionnaires, participants completed a demographic questionnaire, as well as several questions related to their COVID-19-exposure (see Table 1).
2.2.2. Pre-existing medical conditions (PEMC)
PEMC were assessed with two questions. First, participants were provided with a list of medical conditions (e.g., diabetes, high blood pressure, cancer, a lung condition, a heart condition, HIV/AIDS, a weakened immune system) and asked to indicate whether a doctor, nurse, or other health professional ever said that they have any of these health condition(s). Participants who selected one or more of these conditions were asked to indicate whether they still have any of these conditions and if yes, to specify their current health condition(s). Based on participants’ responses, we created a categorical variable with two levels: 1) participants who currently have a medical condition that is considered a risk factor for COVID-19 (Centers for Disease Control & Prevention, 2020), and 2) participants with no current medical conditions that may increase susceptibility to COVID-19.
2.2.3. Pre-existing mental health conditions (PEMHC)
PEMHC were assessed using the following question: Prior to the Coronavirus outbreak, had you ever been told by a health professional that you had a mental health disorder, such as depression and/or anxiety disorders? The response options included: 1) uncertain, 2) no, and 3) yes. Participants who selected “yes” were asked to specify the mental health diagnosis they received.
2.2.4. Perceived vulnerability to COVID-19 (PVC)
Perceived vulnerability to COVID-19 was measured with five items. We adapted the following three items from the Perceived Vulnerability to Disease Questionnaire (PVD; Duncan, Schaller, & Park, 2009): 1) In general, I am very susceptible to infectious diseases, 2) I am more likely than the people around me to become infected with Coronavirus, and 3) I have a history of susceptibility to infectious disease. In addition, we added the following two items: 4) I am more likely than the people around my age to become infected with Coronavirus, and 5) I have pre-existing health conditions that increase my susceptibility to Coronavirus. Participants rated these items on a seven-point scale (1 = strongly disagree, 7 = strongly agree). The results of a principal component analysis indicated that these five items loaded on a single factor (factor loadings ranged from .771 to .902), which explained 74.4 % of the variance and demonstrated high internal consistency (α = .908).
2.2.5. COVID-19-related worries
We used eight items from the SARS Fear Scale (SFS; Ho et al., 2005) to assess COVID-19-related worries. The SFS was developed to measure SARS-related worries among health care workers and SARS survivors who work in hospitals (Ho et al., 2005). The original scale included 18 items, some of which measured work-related worries (e.g., “worry if I will be assigned to SARS ward” and “worry if my family or friends will keep a distance from me due to my job duties”), as well as fear of infecting others (Ho et al., 2005). In the present study, we used the following 8 items that focus on fear of infection, and feelings of insecurity and loss of control: 1) Fear that I will be infected, 2) suspect whether I have been infected or not, 3) feel that the virus is very close to me (and the virus may invade my body anytime), 4) feel very unsafe about myself, 5) feel that life is threatening, 6) feel that I have lost control of life, 7) think about death/dying, and 8) worry about other health problems regarding myself. Participants rated these items on a four-point scale (0 = definitely false, 3 = definitely true). The results of a principal component analysis revealed a single factor which explained 59.4 % of the variance. The factor loadings of the items ranged from .655 to .867. The Cronbach’s alpha coefficient for the eight items was .900.
2.2.6. Social isolation
We adapted the 3-item version of the UCLA Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004) to measure social isolation. The original version of this scale (i.e., the 3-item version) does not use a specific timeframe (e.g., “How often do you feel isolated from others?”); however, in the present study, we used the “past few weeks” timeframe to assess participants’ feelings of isolation during the COVID-19 outbreak (e.g., “During the past few weeks, how often did you feel isolated from others?”). Participants were instructed to rate each item on a four-point rating scale (1 = never, 4 = often). Hughes et al. (2004) provided support for the concurrent and discriminant validity of the three-item version of the UCLA Loneliness Scale. The Cronbach’s alpha coefficient for the three-item version was .72 and it had a strong correlation with the Revised UCLA Loneliness Scale (r = .82, p < .001) (Hughes et al., 2004). For the present study, the Cronbach’s alpha coefficient was .904.
2.2.7. Traumatic stress symptoms
The PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) was used in the present study to measure COVID-19-related TS. The instrument is comprised of 20 self-report items (e.g., “Having strong negative feelings such as fear, horror, anger, guilt, or shame.”) that map on to the diagnostic criteria for PTSD defined by the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2013). In the present study, we modified the instructions of the PCL-5 in order to measure COVID-19-related TS. Specifically, we instructed participants to think about how the Coronavirus outbreak affected them within the past month and then indicate the extent to which they experienced each symptom during the past month in relation to COVID-19. The items of the PCL-5 are rated on a five-point scale ranging from 0 (not at all) to 4 (extremely). Total scale scores of the PCL-5 range from 0 to 80 and represent overall posttraumatic symptom severity (Weathers et al., 2013). Recent studies provided support for the reliability and the validity of the PCL-5 among different samples, including college students (e.g., Blevins, Weathers, Davis, Witte, & Domino, 2015) and military service members (e.g., Wortmann et al., 2016). Our reliability analysis revealed a Cronbach’s alpha coefficient of .959 for the overall scale.
2.3. Data analysis overview
Prior to testing our hypothesized models, we conducted descriptive statistics and preliminary exploratory analyses to describe our data and to screen the data for potential problems (e.g., missing values, multicollinearity). In order to test our first hypothesized model, we conducted a mediation analysis using PROCESS macro (Model 6) for SPSS (Version 3; Hayes, 2018). This analysis included four control variables (age, gender, PEMC, and PEMHC), one predictor variable (PVC), two sequential mediators (COVID-19-related worries and social isolation), and an outcome variable (TS). The significance of the indirect effects of PVC on TS through our proposed mediators was determined using a bootstrap analysis with 5000 samples. The bootstrapping method is recommended for testing the significance of mediating effects due to its advantages (e.g., increased power and control over type I error rate) over other methods of testing mediation (e.g., MacKinnon, Lockwood, & Williams, 2004; Preacher & Hayes, 2008).
Our second hypothesized model was examined using a moderated mediation analysis. This analysis included four control variables (age, gender, PEMC, and PEMHC), one mediator (COVID-19-related worries), one moderator (social isolation), and an outcome variable (TS). All continuous variables except for TS were mean centered prior to testing the model. The moderated mediation analysis was conducted using PROCESS macro (Model 14) by Hayes (2018). This analysis provides an index of moderation mediation (Hayes, 2015) and a 95 % bootstrap confidence interval (CI) for this index, which was generated using 5000 samples in the present study. The moderated mediation effect is considered significant if the index of moderated mediation is significantly different from zero (i.e., the bootstrap CI associated with this index does not include zero). If a significant moderated mediation effect is detected, the conditional indirect effects are examined in order to further probe the moderated mediation effect.
3. Results
3.1. Preliminary analyses
Descriptive statistics and bivariate correlations among the study variables are provided in Table 2 . Preliminary analyses indicated that ten participants had one or two missing values on study questionnaires. We utilized the person mean substitution method to handle these missing values. The overall scale scores for PVC, COVID-19-related worries, social isolation, and TS were computed by taking the mean of the items measuring these constructs.
Table 2.
Means, Standard Deviations, and Bivariate Correlations among Study Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | .223*** | .325*** | −.018 | .117** | −.021 | −.050 | −.125** | 41.260 | 11.566 |
| 2. Gender | – | .103** | .185*** | .113** | .108** | −.072* | .004 | – | – | |
| 3. PEMC | – | .147*** | .422*** | .162*** | .043 | .072* | – | – | ||
| 4. PEMHC | – | .092* | .133*** | .151*** | .141*** | – | – | |||
| 5. PVC | – | .518*** | .212*** | .422*** | 2.600 | 1.449 | ||||
| 6. COVID-19-related worries | – | .285*** | .580*** | 1.163 | .752 | |||||
| 7. Social isolation | – | .511*** | 2.066 | .956 | ||||||
| 8. Traumatic stress | – | .737 | .795 |
Note. N = 747. PEMC = pre-existing medical conditions; PEMHC = pre-existing mental health conditions; PVC = perceived vulnerability to COVID-19. Gender is coded as 0 = man, 1 = woman. PEMC is coded as 0 = no, 1 = yes. PEMHC is coded as 0 = no, 1 = yes or uncertain. * p < .05. ** p < .01. *** p < .001.
Descriptive analyses indicated that 79.7 % of the participants (n = 595) did not have any PEMC that may increase susceptibility to COVID-19; whereas, 20.3 % of the participants (n = 152) reported having at least one chronic medical condition (e.g., asthma, diabetes, kidney disease, high blood pressure, chronic obstructive pulmonary disease, heart disease, and an autoimmune disease). The majority of the participants (75.1 %; n = 561) did not report a history of mental health disorder diagnosis; 24.0 % of the participants (n = 179) reported a history of one or multiple mental health disorder diagnoses (e.g., obsessive compulsive disorder, generalized anxiety disorder, PTSD, bipolar disorder, major depressive disorder, panic disorder, and social anxiety disorder); and .9% (n = 7) of the participants indicated that they were uncertain whether they received a psychiatric diagnosis. The results of univariate analyses of variance (ANOVAs) indicated significant differences among these three groups of participants in terms of PVC (F[2, 744] = 3.557, p = .029, η2 = .009), COVID-19-related worries (F[2, 744] = 6.995, p = .001, η2 = .018), social isolation (F[2, 744] = 9.142, p < .001, η2 = .024), and TS symptoms (F[2, 744] = 7.887, p < .001, η2 = .021). However, the follow-up post-hoc tests indicated that participants who were uncertain about whether they received a diagnosis did not differ from the participants who received a psychiatric diagnosis on any of these variables. Therefore, we created a categorical variable (i.e., PEMHC) with two levels: participants who did not receive a diagnosis (n = 561, 75.1 %) and those who received a diagnosis or were uncertain whether they received a diagnosis (n = 186, 24.9 %).
Table 1 presents descriptive information about participants’ exposure to COVID-19. As can be seen, only a very small percentage of the participants reported having direct exposure to COVID-19, such as being in contact with an infected person or living in the same household as an infected person. Only seven participants reported being tested for COVID-19 and none of these participants had a confirmed diagnosis of COVID-19. Of the 22 participants who personally knew someone who died of COVID-19, 9.1 % (n = 2) described their relationship to the deceased person as an immediate family member, 18.2 % (n = 4) as an extended family member, 9.1 % (n = 2) as a close friend, 18.2 % (n = 4) as a co-worker/colleague, 40.9 % (n = 9) as an acquaintance, and 4.5 % (n = 1) as “other” (high school science teacher).
The examination of the bivariate correlations (see Table 2) indicated that the predictor variables were not extremely highly correlated with each other (the highest correlation coefficient was .518). The collinearity diagnostics indicated that the highest variance inflation factor (VIF) was 1.648 for Model 1, and 1.671 for Model 2. These findings suggest that there was no problematic multicollinearity in the data.
3.2. Main analyses
3.2.1. Mediation analysis (Model 1)
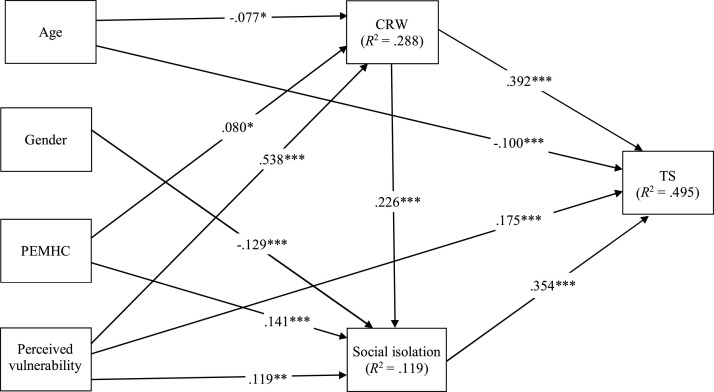
The results of the mediation analysis indicated that all hypothesized direct effects were significant, and the pattern of the relationships was in the expected direction. Regarding the control variables, PEMC did not significantly predict the mediators or TS. Older age was associated with less COVID-19-related worries and less TS. PEMHC were associated with increased social isolation and more COVID-19-related worries. In addition, gender had a negative effect on social isolation, suggesting that men reported higher social isolation following the COVID-19 outbreak than women. The direct effects of the predictors on outcome variables are shown in Table 3 . The standardized regression weights for significant direct effects are presented Fig. 1 .
Table 3.
Direct Effects (Model 1).
| Independent variable | Dependent variable | Unstandardized coefficient (b) | SE | t | p | 95 % CI (lower, upper) |
|---|---|---|---|---|---|---|
| Age → | COVID-19 worries | −.005 | .002 | −2.271 | .023 | −.009, -.0007 |
| Gender → | COVID-19 worries | .083 | .049 | 1.701 | .089 | −.013, .179 |
| PEMC → | COVID-19 worries | −.108 | .068 | −1.596 | .111 | −.241, .025 |
| PEMHC → | COVID-19 worries | .140 | .056 | 2.510 | .012 | .030, .249 |
| PVC → | COVID-19 worries | .279 | .018 | 15.674 | < .001 | .244, .314 |
| Age → | Social isolation | −.001 | .003 | −.344 | .731 | −.007, .005 |
| Gender → | Social isolation | −.246 | .069 | −3.543 | < .001 | −.382, -.110 |
| PEMC → | Social isolation | −.111 | .096 | −1.156 | .248 | −.299, .076 |
| PEMHC → | Social isolation | .311 | .079 | 3.936 | < .001 | .156, .467 |
| PVC → | Social isolation | .078 | .029 | 2.672 | .008 | .021, .135 |
| COVID-19 worries → | Social isolation | .287 | .052 | 5.526 | < .001 | .185, .389 |
| Age→ | Traumatic stress | −.007 | .002 | −3.512 | < .001 | −.011, -.003 |
| Gender → | Traumatic stress | −.015 | .044 | −.342 | .732 | −.102, .071 |
| PEMC → | Traumatic stress | −.100 | .061 | −1.659 | .098 | −.219, .018 |
| PEMHC → | Traumatic stress | .049 | .050 | .968 | .333 | −.050, .148 |
| PVC → | Traumatic stress | .096 | .018 | 5.210 | < .001 | .060, .132 |
| COVID-19 worries → | Traumatic stress | .415 | .033 | 12.412 | < .001 | .349, .480 |
| Social isolation → | Traumatic stress | .295 | .023 | 12.728 | < .001 | .249, .340 |
Note. SE = standard error; CI = confidence interval; PEMC = pre-existing medical conditions; PEMHC = pre-existing mental health conditions; PVC = perceived vulnerability to COVID-19. Gender is coded as 0 = man, 1 = woman. PEMC is coded as 0 = no, 1 = yes. PEMHC is coded as 0 = no, 1 = yes or uncertain.
Fig. 1.
Standardized Parameter Estimates of Model 1.
Note. Non-significant relationships are not shown. PEMHC = pre-existing mental health conditions; CRW = COVID-19-related worries; TS = traumatic stress. Gender is coded as 0 = man, 1 = woman. PEMHC is coded as 0 = no, 1 = yes or uncertain.
* p < .05. ** p < .01. *** p < .001.
The results of the bootstrap analysis indicated that the hypothesized two-step indirect path from PVC to TS through COVID-19-related worries and social isolation was significant (ß = .043, B = .024, bootstrap SE = .005, 95 % bootstrap CI = [.014, .034]). In addition, two one-step paths from PVC to TS — one through COVID-19-related worries (ß = .211, B = .116, bootstrap SE = .014, 95 % bootstrap CI = [.090, .144]) and another through social isolation (ß = .042, B = .023, bootstrap SE = .009, 95 % bootstrap CI = [.006, .040]) — were significant. These findings provide support for our hypothesized model, and suggest that the relationship between PVC and TS is mediated by COVID-19-related worries and social isolation.
3.2.2. Moderated mediation analysis (Model 2)
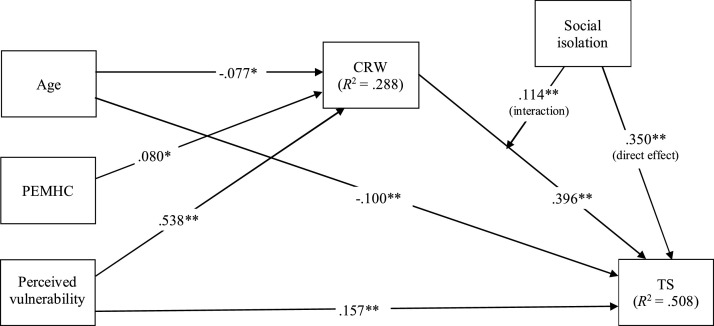
Supporting our hypothesized model 2, the results of the moderated mediation analysis indicated that the indirect effect of PVC on TS was significantly moderated by social isolation (the index of moderated mediation = .035, bootstrap SE = .010, 95 % bootstrap CI [.015, .055]). To better understand the nature of these relationships, we examined conditional indirect effects of PVC on TS at low (−1 SD = −.956), medium (mean = .00) and high (+1 SD. = .956) levels of social isolation. Results indicated that the indirect effect of PVC on TS through COVID-19-related worries was significant at low (b = .083, bootstrap SE = .014, 95 % bootstrap CI [.057, .110]), medium (b = .117, bootstrap SE = .013, 95 % bootstrap CI [.091, .143]), and high levels of social isolation (b = .151, bootstrap SE = .019, 95 % bootstrap CI [.113, .188]); however, the strength of this indirect association was higher at medium and high levels of social isolation. Table 4 presents the unstandardized regression coefficients of Model 2. The standardized regression coefficients for significant effects are presented in Fig. 2 .
Table 4.
Direct Effects (Model 2).
| Independent variable | Dependent variable | Unstandardized coefficient (b) | SE | t | p | 95 % CI (lower, upper) |
|---|---|---|---|---|---|---|
| Age → | COVID-19 worries | −.005 | .002 | −2.271 | .023 | −.009, -.0007 |
| Gender → | COVID-19 worries | .083 | .049 | 1.701 | .089 | −.013, .179 |
| PEMC → | COVID-19 worries | −.108 | .068 | −1.596 | .111 | −.241, .025 |
| PEMHC → | COVID-19 worries | .140 | .056 | 2.510 | .012 | .030, .249 |
| PVC → | COVID-19 worries | .279 | .018 | 15.674 | < .001 | .244, .314 |
| Age→ | Traumatic stress | -.007 | .002 | −3.567 | < .001 | −.011, -.003 |
| Gender → | Traumatic stress | -.012 | .044 | -.266 | .790 | -.097, .074 |
| PEMC → | Traumatic stress | -.083 | .060 | −1.389 | .165 | -.201, .034 |
| PEMHC → | Traumatic stress | .049 | .050 | .988 | .324 | −.049, .147 |
| PVC → | Traumatic stress | .086 | .018 | 4.720 | < .001 | .051, .122 |
| COVID-19 worries → | Traumatic stress | .418 | .033 | 12.681 | <.001 | .354, .483 |
| Social isolation → | Traumatic stress | .291 | .022 | 12.727 | < .001 | .246, .336 |
| CRW X social isolation → | Traumatic stress | .126 | .028 | 4.493 | < .001 | .071, .182 |
Note. SE = standard error; CI = confidence interval; PEMC = pre-existing medical conditions; PEMHC = pre-existing mental health conditions; PVC = perceived vulnerability to COVID-19; CRW = COVID-19-related worries. Gender is coded as 0 = man, 1 = woman. PEMC is coded as 0 = no, 1 = yes. PEMHC is coded as 0 = no, 1 = yes or uncertain.
Fig. 2.
Standardized Parameter Estimates of Model 2.
Note. Non-significant relationships are not shown. PEMHC = pre-existing mental health conditions; CRW = COVID-19-related worries; TS = traumatic stress. PEMHC is coded as 0 = no, 1 = yes or uncertain.
* p < .05. ** p < .001.
3.3. Additional analyses
We conducted additional analyses to determine whether our model results were different after removing the 42 participants who have been tested for COVID-19, reported exposure to COVID-19 (i.e., being in contact with an infected person, living with an infected person, or having an infected family member), or know someone who died of COVID-19. Removing these participants (n = 705) did not change the significance or the direction of our main findings. In addition, the amount of variance explained in TS by our models was not substantially different with or without these participants.
4. Discussion
We tested two models in the present study to examine the factors that contribute to COVID-19-related TS among individuals who are not directly affected by COVID-19. Our first model examined whether COVID-19-related worries and social isolation mediate the relationship between PVC and TS. Results indicated that, after controlling for age, gender, and pre-existing mental health and physical health conditions, the direct effects of PVC on mediators and the outcome variable were significant, suggesting that participants who perceive themselves as highly vulnerable to COVID-19 reported more COVID-19-related worries and higher social isolation and TS than those who perceived themselves as less vulnerable to COVID-19. The analysis of indirect effects indicated that the relationship between PVC and TS was mediated by COVID-19-related worries and social isolation. Specifically, a significant two-step indirect path from PVC to TS suggested that higher levels of PVC may increase COVID-19-related worries, which in turn, may heighten a sense of isolation and hence increase TS. In addition, one step paths from PVC to TS through each mediator variable were significant, suggesting that PVC had positive direct effects on both COVID-19-related worries and social isolation, which in turn positively predicted TS. These findings provide support for our first model and suggest that PVC may exert both direct and indirect effects on TS.
Our second model examined whether social isolation may strengthen the indirect effect of PVC on TS (via COVID-19-related worries) by moderating the effect of COVID-19-related worries on TS. Supporting this model, we found that the indirect effect of PVC on TS was dependent on the level of social isolation. At high and medium levels of social isolation, PVC had a stronger positive indirect effect on TS; whereas, at low levels of social isolation, this indirect effect was weaker. Taken together with the results of the first model, these findings suggest that PVC and the resulting COVID-19-related worries may increase social isolation, which in turn, may increase TS by both mediating and moderating the effect of COVID-19-related worries on TS.
While previous research has highlighted adaptive functions of perceived vulnerability to disease (e.g., promoting health-protective behaviors and/or intentions) (e.g., Sheeran, Harris, & Epton, 2014), the results of the present study suggest that an increased sense of vulnerability during the current pandemic may increase TS. For some individuals, these acute TS reactions may develop into chronic PTSD, which can be difficult to treat. A meta analysis indicated that only 54 % of the individuals who completed treatment of PTSD showed clinically meaningful improvement in their symptoms (Bradley, Greene, Russ, Dutra, & Westen, 2005). Therefore, timely interventions that focus on prevention and early identification and treatment for individuals who show symptoms of TS could play a critical role in reducing the mental health burden of infectious disease pandemics. Our findings provide preliminary evidence that reducing disease-related risk perceptions and disease-related worries during the early phases of pandemics might help decrease TS in the general population of adults. In addition, given that social isolation both mediates and moderates the indirect effect of PVC on TS, it might be one of the key variables that can be targeted in early interventions to reduce TS.
Although social isolation may be an inevitable result of infectious disease outbreaks that require strict social distancing measures, the results of the present study suggest that people’s disease-related perceptions and worries may also play a significant role in the degree to which they experience social isolation. As previously noted, disease-related concerns and higher perceived vulnerability to disease can increase interpersonal avoidance, as well as self-relevant biases such as perceiving oneself as less extraverted, less agreeable, and less open to new experiences (e.g., Mortensen et al., 2010; Sacco et al., 2014). These biases may not only reduce face-to-face interaction with others, but they can also reduce other safer forms social interaction, making individuals vulnerable to social isolation and its negative psychological consequences. Therefore, an adaptive level of risk awareness and adaptive regulation of disease-related worries during infectious disease outbreaks may enhance individuals’ ability to remain socially connected without increasing one’s risk of infection.
Past research and recent COVID-19 literature provide some insights into the factors that may help reduce COVID-19-related worries and perceptions of threat (e.g., Chao, Xue, Liu, Yang, & Hall, 2020; Ho et al., 2005; Mertens, Gerritsen, Duijndam, Salemink, & Engelhard, 2020; Roy et al., 2020). For example, recent studies indicate that exposure to COVID-19-related news and stressful content through media and/or social networking sites is associated with increased COVID-19-related worries and distress (e.g., Chao et al., 2020; Mertens et al., 2020; Roy et al., 2020). On the other hand, receiving adequate and accurate information about COVID-19 (e.g., transmission routes of the virus; regular updates about number of persons recovered from COVID-19), knowledge of COVID-19 and prevention methods, and practicing precautionary measures against COVID-19 have been linked to less COVID-19-related worries and distress (Chao et al., 2020; Wang et al., 2020). Therefore, helping individuals access accurate information about COVID-19 through trusted sources and reducing their exposure to unhelpful, inaccurate, or anxiety-provoking information may help them better regulate their COVID-19-related worries and fears.
There are some limitations of the present study that should be taken into consideration when interpreting our findings. First, our findings are based on correlational and cross-sectional data; therefore, causal conclusions cannot be drawn based on our findings. Second, research suggests that the quality of data obtained from Amazon Mturk samples outperform or are comparable to the data obtained from other samples (e.g., student samples or subject pool participants, professional panels) (e.g., Hauser & Schwarz, 2016; Kees, Berry, Burton, & Sheehan, 2017). In addition, our sample was approximately comparable to the general United States population in terms of gender distribution; however, some ethnic and racial groups (e.g., African American, Hispanic/Latinx) were underrepresented in our sample (see The United States Census Bureau, 2019). Further, compared to the general population (age 25 and older) (see The United States Census Bureau, 2020), a slightly higher percentage of our participants had a bachelor’s degree (36 % vs. 42.7 %, respectively). Therefore, generalizations to people of color and less educated individuals should be made with caution, particularly considering the disproportionate impact of COVID-19 on people of color and other socially disadvantaged populations (e.g., hospitalization and mortality rates, exposure to pandemic-related stressors) (for a discussion and review, see Boyraz & Legros, 2020).
Third, we adapted items from existing instruments to measure PVC and COVID-19-related worries because there were no valid and reliable instruments to measure these constructs at the time of our data collection. Although our findings provided preliminary support for the psychometric characteristics of these modified instruments, a more comprehensive examination of the reliability and validity of these instruments is needed. Forth, we controlled for PEMHC in our models; however, we did not take the type of psychiatric diagnosis into account. Recent findings suggest that people who have anxiety disorders may experience greater COVID-related stress than those who have mood disorders (Asmundson et al., 2020). Therefore, future studies may consider controlling for the type of PEMHC.
In conclusion, while awareness of personal risk of COVID-19 infection may facilitate self-protective behaviors, the present study suggests that high levels of PVC during the current pandemic may increase TS both by having a direct effect on TS, as well as by increasing COVID-19-related worries and social isolation. In addition, our findings suggest that individuals who experience greater social isolation during this pandemic may experience more difficulty in regulating their COVID-19-related worries, which may increase their vulnerability to COVID-19-related TS. Although future experimental and longitudinal research is needed, our findings suggest that early interventions that promote social connectedness and adaptive regulation of disease-related worries may help reduce pandemic-related TS.
Funding
This study is funded by a Pace University Scholarly Research Grant.
Declaration of Competing Interest
None
References
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Landry C.A., Rachor G.S., McKay D., Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bo H.-X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological Medicine. 2020 doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyraz G., Legros D.N. Coronavirus disease (COVID-19) and traumatic stress: Probable risk factors and correlates of posttraumatic stress disorder. Journal of Loss & Trauma. 2020;25(6–7):503–522. doi: 10.1080/15325024.2020.1763556. [DOI] [Google Scholar]
- Bradley R., Greene J., Russ E., Dutra L., Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry. 2005;162(2):214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Brewin C.R., Andrews B., Valentine J.D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C. Social isolation and health, with an emphasis on underlying mechanisms. Perspectives in Biology and Medicine. 2003;46(3):S39–S52. [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020, June 25). Coronavirus disease 2019 (COVID-19): People of any age with underlying medical conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html. [PubMed]
- Chao M., Xue D., Liu T., Yang H., Hall B.J. Media use and acute psychological outcomes during COVID-19 outbreak in China. Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. The American Psychologist. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S., Hoberman H.M. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13(2):99–125. doi: 10.1111/j.1559-1816.1983.tb02325.x. [DOI] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Dryhurst S., Schneider C.R., Kerr J., Freeman A.L.J., Recchia G., van der Bles A.M. Risk perceptions of COVID-19 around the world. Journal of Risk Research. 2020;0(0):1–13. doi: 10.1080/13669877.2020.1758193. [DOI] [Google Scholar]
- Duncan L.A., Schaller M. Prejudicial attitudes toward older adults may be exaggerated when people feel vulnerable to infectious disease: Evidence and implications. Analyses of Social Issues and Public Policy (ASAP) 2009;9(1):97–115. doi: 10.1111/j.1530-2415.2009.01188.x. [DOI] [Google Scholar]
- Duncan L.A., Schaller M., Park J.H. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Personality and Individual Differences. 2009;47(6):541–546. doi: 10.1016/j.paid.2009.05.001. [DOI] [Google Scholar]
- Ehlers A., Clark D.M. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Forte G., Favieri F., Tambelli R., Casagrande M. COVID-19 pandemic in the italian population: Validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. International Journal of Environmental Research and Public Health. 2020;17(11):4151. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser D.J., Schwarz N. Attentive turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior Research Methods. 2016;48(1):400–407. doi: 10.3758/s13428-015-0578-z. [DOI] [PubMed] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. An index and test of linear moderated mediation. Multivariate Behavioral Research. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. second edition. Guilford Press; 2018. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Ho S.M.Y., Kwong-Lo R.S.Y., Mak C.W.Y., Wong J.S. Fear of severe acute respiratory syndrome (SARS) among health care workers. Journal of Consulting and Clinical Psychology. 2005;73(2):344–349. doi: 10.1037/0022-006X.73.2.344. [DOI] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H., Nan J., Lv Z., Yang J. Psychological impacts of the COVID-19 epidemic on Chinese people: Exposure, post-traumatic stress symptom, and emotion regulation. Asian Pacific Journal of Tropical Medicine. 2020;13(6):252. doi: 10.4103/1995-7645.281614. [DOI] [Google Scholar]
- Kees J., Berry C., Burton S., Sheehan K. An analysis of data quality: Professional panels, student subject pools, and Amazon’s Mechanical Turk. Journal of Advertising. 2017;46(1):141–155. doi: 10.1080/00913367.2016.1269304. [DOI] [Google Scholar]
- Laubmeier K.K., Zakowski S.G. The role of objective versus perceived life threat in the psychological adjustment to cancer. Psychology & Health. 2004;19(4):425–437. doi: 10.1080/0887044042000196719. [DOI] [Google Scholar]
- MacKinnon D.P., Lockwood C.M., Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meli L., Kautz M., Julian J., Edmondson D., Sumner J.A. The role of perceived threat during emergency department cardiac evaluation and the age-posttraumatic stress disorder link. Journal of Behavioral Medicine. 2018;41(3):357–363. doi: 10.1007/s10865-017-9904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens G., Gerritsen L., Duijndam S., Salemink E., Engelhard I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S.L., Maner J.K. Overperceiving disease cues: The basic cognition of the behavioral immune system. Journal of Personality and Social Psychology. 2012;102(6):1198–1213. doi: 10.1037/a0027198. [DOI] [PubMed] [Google Scholar]
- Mortensen C.R., Becker D.V., Ackerman J.M., Neuberg S.L., Kenrick D.T. Infection breeds reticence: The effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychological Science. 2010;21(3):440–447. doi: 10.1177/0956797610361706. [DOI] [PubMed] [Google Scholar]
- Neuberg S.L., Kenrick D.T., Schaller M. Human threat management systems: Self-protection and disease avoidance. Neuroscience and Biobehavioral Reviews. 2011;35(4):1042–1051. doi: 10.1016/j.neubiorev.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer E.J., Best S.R., Lipsey T.L., Weiss D.S. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Park T., Ju I., Ohs J.E., Hinsley A. Optimistic bias and preventive behavioral engagement in the context of COVID-19. Research in Social and Administrative Pharmacy. 2020 doi: 10.1016/j.sapharm.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco D.F., Young S.G., Hugenberg K. Balancing competing motives: Adaptive trade-offs are necessary to satisfy disease avoidance and interpersonal affiliation goals. Personality & Social Psychology Bulletin. 2014;40(12):1611–1623. doi: 10.1177/0146167214552790. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Harris P.R., Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychological Bulletin. 2014;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Sun L., Sun Z., Wu L., Zhu Z., Zhang F., Shang Z. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. MedRxiv. 2020 doi: 10.1101/2020.03.06.20032425. [DOI] [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. (pp. xvi, 158) [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020 doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The United States Census Bureau. (2019, July 1). Quick facts: United States. https://www.census.gov/quickfacts/fact/table/US/PST045219.
- The United States Census Bureau. (2020, March 30). U.S. Census Bureau releases new educational attainment data. The United States Census Bureau. https://www.census.gov/newsroom/press-releases/2020/educational-attainment.html.
- Tolin D.F., Foa E.B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD atwww.ptsd.va.gov.
- Weinstein N.D. Unrealistic optimism about susceptibility to health problems. Journal of Behavioral Medicine. 1982;5(4):441–460. doi: 10.1007/BF00845372. [DOI] [PubMed] [Google Scholar]
- Weinstein N.D. Unrealistic optimism about susceptibility to health problems: Conclusions from a community-wide sample. Journal of Behavioral Medicine. 1987;10(5):481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020, August 30). Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Wortmann J.H., Jordan A.H., Weathers F.W., Resick P.A., Dondanville K.A., Hall-Clark B. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016;28(11):1392–1403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]