Main Text
A new coronavirus disease (COVID-19) with infection by a novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread globally since December 2019. By 22 September 2020, more than 200 countries worldwide have reported about 30 million confirmed cases and more than 950,000 deaths.1 China has reported a total of 85,307 (including 2,758 imported) cases and 4,634 deaths.2
To control the dispersal of COVID-19, the Chinese government initiated an unprecedented lockdown in Hubei province and raised a national public health response to the highest state of emergency: level 1 of 4 levels of severity in the Chinese Emergency System on 23 January 2020. People were encouraged to stay at home as much as possible, and all public events and gatherings were canceled or delayed, which significantly reduced social contacts in public spaces (e.g., public transportation, supermarkets, offices, etc.) but increased person-to-person contacts in households.3 At the same time, the usage rate of face masks was high in public spaces (consistently >90% during the time of lockdown4). The duration for detection and diagnosis of infected individuals was shortened, and consequently diagnosed individuals and those who were in close contact with them could be isolated in a timely manner.5 With strict social distancing and non-pharmaceutical interventions, China has contained the spread of COVID-19 and reopened its economy since early April. The successful experiences in China will provide important evidence and scientific insights for other countries that are amid the pandemic.
Based on a dynamic compartmental model, this study aims to quantify the impact of social distancing on the transmission of COVID-19 in China in the presence of high coverage of face mask use.
We collected data on the number of cumulative confirmed cases (except imported cases) and deaths from 15 January 2020 to 30 August 2020 from the National Health Commission2 and Health Commission of Hubei Province.6 We used a published compartmental model7 to describe the transmission of COVID-19 in Hubei Province and all other affected provinces except Hubei (Outside Hubei) separately. The model took into consideration of both transmissions in public spaces and households. The face mask usage rate was chosen as 97.6%4 with 85% effectiveness8 during and after the national response against COVID-19. We assumed that social distancing measures can reduce the average number of daily contacts by 80% in public spaces3 but increase the contacts by two times in households9 during the lockdown and level 1 response. Details of the model structure, parameters, and calibration are shown in the Supplementary Information.
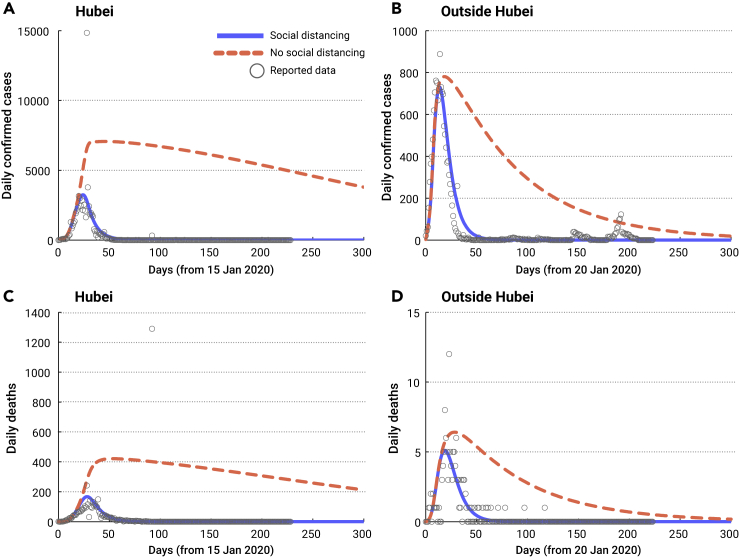
Under the status quo with social distancing, the estimated numbers of confirmed cases and deaths were 68,471 (95% confidence interval [CI], 57,316–79,625) and 4,142 (95% CI, 3,451–4,832) in Hubei Province (Figures 1A and 1C), respectively, and the disease can be controlled within 3 months, which are closely consistent with the observations. If the social distancing had never been in place, the COVID-19 epidemic would result in 1,626,028 (95% CI, 764,622–2,487,434) infections and 92,254 (95% CI, 44,335–140,173) deaths. This suggests that social distancing would prevent 95.16% (95% CI, 93.23%–97.08%) of infections and 95.27% (95% CI, 93.40%–97.15%) of deaths in Hubei Province, respectively. Moreover, it will take more than 1 year to control the disease in this scenario.
Figure 1.
COVID-19 Epidemic Trend
Model calibration and predictions based on reported confirmed COVID-19 cases and deaths in Hubei province (A and C) and outside Hubei (B and D) with and without social distancing.
Similarly, the estimated numbers of confirmed cases and deaths were 14,356 (95% CI, 13,007–15,704) and 124 (95% CI, 103–146) outside Hubei (Figures 1B and 1D) in the presence of social distancing, and these two numbers became 71,732 (95% CI, 50,929–92,535) and 621 (95% CI, 418–824) in the absence of social distancing. This indicates that social distancing would prevent 80.29% (95% CI, 76.01%–84.57%) of infections and 79.66% (95% CI, 75.28%–84.04%) of deaths outside Hubei, respectively.
We estimated that the social distancing measures might have reduced more than 95% of the epidemic in Hubei province and 80% of epidemic outside Hubei, compared with the absence of social distancing. This is consistent with previous evaluations based on various modeling approaches without considering face mask use.10 The difference in the effects of social distancing within and outside Hubei province may be due to multiple reasons, including the number of active cases, prevalence of infection in the population, and availability of medical resources.
In the absence of social distancing, the disease can still be controlled with a high rate of face mask use. However, it will lead to more than a 20-fold increase in infections and deaths and take much longer. This indicates that even an extremely high rate face mask use cannot replace social distancing. In the post-epidemic era, social distancing should be still maintained to reduce the risk of a second outbreak.
This study has several limitations. First, we did not model the variability due to changes in reporting criteria. This may introduce some bias to the projected estimates in the earlier time frames and cannot capture the sharp increase when the actual clinical diagnosis data and corrected death data (Figures 1A and 1C) were added. Second, our model cannot capture the second outbreak due to seafood market transmissions (Figure 1B), such as in Beijing city and Dalian city. Third, we did not consider the possible transmission from imported cases because the border control measures are so strict that the probability of this occurrence is extremely small. Fourth, the effect of asymptomatic infection is not involved, which may underestimate the infections in the absence of social distancing and thus the effectiveness of social distancing. We also did not consider that recovered individuals can be infected again due to the limited evidence on this. Despite these limitations, this study fills an important research gap by quantifying the impact of social distancing on the transmission of COVID-19 in China.
We conclude that social distancing measures, imposed and orchestrated by the central government as a national response against the epidemic, have greatly reduced the number of infections and deaths both in and outside Hubei in China.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81950410639 [L.Z.], 11801435 [M.S.], 11631012 [Y.X.], 81673275[Z.P.], 91846302[Z.P.]); Outstanding Young Scholars Support Program (3111500001 [L.Z.]); Xi'an Jiaotong University Basic Research and Profession Grant (xtr022019003[L.Z.], xzy032020032 [L.Z.]); and Xi'an Jiaotong University Young Scholar Support Grant (YX6J004 [L.Z.]); the Bill & Melinda Gates Foundation (20200344 [L.Z.]); China Postdoctoral Science Foundation (2018M631134, 2020T130095ZX); the Fundamental Research Funds for the Central Universities (xjh012019055, xzy032020026); Natural Science Basic Research Program of Shaanxi Province (2019JQ-187); Xi'an Special Science and Technology Projects on Prevention and Treatment of Novel Coronavirus Penumonia Emergency (20200005YX005); Zhejiang University special scientific research fund for COVID-19 prevention and control (2020XGZX056); the National S&T Major Project Foundation of China (2018ZX10715002-004, 2018ZX10713001-001); and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author Contributions
M.S., Z.P., Y.X., and L.Z. conceived and designed the study. M.S. analyzed the data, carried out the analysis and performed numerical simulations. M.S. wrote the first draft of the manuscript. All the authors contributed to writing the paper and agreed with the results and conclusions.
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.xinn.2020.100048.
Contributor Information
Yanni Xiao, Email: yxiao@mail.xjtu.edu.cn.
Lei Zhang, Email: lei.zhang1@xjtu.edu.cn.
Supplemental Information
References
- 1.World Health Organization Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
- 2.National Health Commission of China Daily report of COVID-19. http://www.nhc.gov.cn/xcs/xxgzbd/gzbd_index.shtml
- 3.Zhang J., Litvinova M., Liang Y., et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 368, 6498:1481-1486. [DOI] [PMC free article] [PubMed]
- 4.Liebao K. Mobile robot data: the face mask useage rate reached 97.6% in Wuhan city during the epidemic. http://m.kejixun.com/article/200224/488396.shtml
- 5.World Health Organization Report of the WHO-China Joint Mission on coronavirus disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- 6.Health Commission of Hubei Province Daily report of COVID-19. http://wjw.hubei.gov.cn/
- 7.Shen M., Peng Z., Guo Y., et al. Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households. Int. J. Infect. Dis. 2020;96:503–505. doi: 10.1016/j.ijid.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu D.K., Akl E.A., Duda S., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen B., Ai C., Ma L., et al. We should prepare for the transmission of COVID-19 in the long run: simulating the risk of the secondary outbreak after holiday. J. Syst. Simul. 2020 http://journal19.magtechjournal.com/Jwk3_xtfzxb/CN/Y2020/V0/I0/0 [Google Scholar]
- 10.Lai S., Ruktanonchai N., Zhou L., et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585:410–413. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.