Abstract
Background
The new coronavirus disease's (COVID-19) high risk of infection can increase the workload of healthcare workers, especially nurses, as they are most of the healthcare workforce. These problems can lead to psychological problems. Therefore, the aim of this systematic review and meta-analysis to ascertain the present impact of the COVID-19 outbreak on the prevalence of stress, anxiety, depression and sleep disturbance among nurses.
Methods
A systematic review and meta-analysis were conducted. The following databases were searched: PubMed, CHINAL, MEDLINE, EMBASE, PsycINFO, MedRxiv and Google Scholar, from January 2020 up to 26th October 2020. Prevalence rates were pooled with meta-analysis using a random-effects model. Heterogeneity was tested using I-squared (I2) statistics.
Results
A total of 93 studies (n = 93,112), published between January 2020 and September 2020, met the inclusion criteria. The overall prevalence of stress was assessed in 40 studies which accounted for 43% (95% CI 37–49). The pooled prevalence of anxiety was 37% (95% CI 32–41) in 73 studies. Depression was assessed in 62 studies, with a pooled prevalence of 35% (95% CI 31–39). Finally, 18 studies assessed sleep disturbance and the pooled prevalence was 43% (95% CI 36–50).
Conclusion
This meta-analysis found that approximately one third of nurses working during the COVID-19 epidemic were suffering from psychological symptoms. This highlights the importance of providing comprehensive support strategies to reduce the psychological impact of the COVID-19 outbreak among nurses under pandemic conditions. Further longitudinal study is needed to distinguish of psychological symptoms during and after the infectious disease outbreaks.
Keywords: COVID-19; Nurses, stress; Anxiety; Depression, sleep disturbance; Systematic review; Meta-analysis
Highlights
-
•
Meta-Analysis was conducted included 93 studies of 93,112 nurses.
-
•
Prevalence of depression and anxiety were 35% and 37% among nurses.
-
•
Prevalence of stress and sleep disturbance were 43% and 43% among nurses.
-
•
A strategy to reduce psychological impact of COVID-19 among nurses is required.
1. Introduction
At the end of December 2019, the new coronavirus disease (COVID-19) emerged in Wuhan City, Hubei province, China, and subsequently spread worldwide [1]. COVID-19 has seriously threatened human health. As of 30th January 2020, the World Health Organization (WHO) declared a public health emergency and considered COVID-19 a pandemic [2]. Globally, the WHO reported 65.6 million confirmed cases worldwide, with nearly 1.5 million deaths up until 6th December 2020 [3]. This increasing number of confirmed cases can overwhelm healthcare systems with thousands of patients needing urgent care.
This high risk of infection from COVID-19 increases the workload of healthcare workers who are involved directly in diagnoses, treatment and care of patients with COVID-19. This is particularly true of nurses, as they are most of the healthcare workforce, and they are in the closest proximity to patients with COVID-19. In June 2020, the International Council of Nurses (ICN) estimated that more than 600 nurses have died from COVID-19 worldwide [4]. In battling the sudden emergency by working at high risk of infection from patients, this can lead to mental health problems such as stress, anxiety and depression.
Previous research on the Severe Acute Respiratory Syndrome (SARS) or Middle East Respiratory Syndrome (MERS) epidemics indicates that nurses working at these times were under extraordinary amounts of pressure [5,6]. A systematic thematic review of 22 studies was conducted by Brooks et al. [7] to identify the social and occupational factors associated with the psychological wellbeing of healthcare workers during the SARS outbreak. The review found that specialized training and preparedness, working at high risk of infection, quarantine, job stress, perceived risk, poor organizational support and stigmatization all impacted on nurses' personal or professional life.
Two previous systematic reviews have been published which explore the prevalence of psychological outcomes among healthcare workers during infectious disease outbreaks [8,9]. However, to date, the psychological impact of the COVID-19 outbreak on nurses has not yet been systematically reported. Therefore, the aim of this study is to conduct a rapid systematic review and meta-analysis to ascertain the present impact of the COVID-19 outbreak on the prevalence of stress, anxiety, depression and sleep disturbance among nurses.
2. Methods
This systematic review and meta-analysis were undertaken according to the PRISMA standards. The review protocol was registered at PROSPERO (No. CRD42020193300).
2.1. Search strategy
A systematic literature search, between January 2020 and 26th October 2020, was conducted using the following databases: PubMed, CHINAL, MEDLINE, EMBASE, PsycINFO, MedRxiv and Google Scholar. Search terms used both free text words and medical subject headings, i.e. MeSH terms, to search papers in the review (Supplementary Appendix 1). In addition, reference lists were screened of the retrieved studies to identify any further studies.
2.2. Study selection
Two investigators (A.M; A.J) performed the search, scrutinizing all titles and abstracts for eligibility against the inclusion and exclusion criteria. Any disagreements were resolved through discussion with a third investigator (A. B). Studies were included in the review according to the following inclusion criteria: (1) reported prevalence of stress or anxiety or depression or sleep disturbance among nurses during COVID-19 outbreaks; (2) all types of setting; and (3), cross-sectional or cohort survey (only the baseline data were extracted). The exclusion criteria were: (1) protocol papers and conference abstracts; (2) if stress or anxiety or depression or sleep disturbance was assessed via an unvalidated scale; and (3), study did not report prevalence among nurses. For any additional information the study authors were contacted.
2.3. Quality assessment
Upon retrieval of the applicable studies, the quality assessment was completed using the Newcastle-Ottawa Scale (NOS) [10]. This scale consists of eight items that evaluate the non-randomized studies, which covered three criteria: the selection of the participants, comparability of study groups and outcome assessment. The NOS uses a score system with the lowest possible score of zero and the highest possible score of nine. The total points awarded indicate the overall quality of the study. A study was determined to be of low risk of bias when the score was 7–9, of moderate risk of bias if the score was 5–6, and high risk of bias if the score was 0–4 [11].
2.4. Data analyses
To estimate the pooled prevalence, odds ratios (ORs) with 95% Confidence Interval (CI) were calculated as the effect size by using a random-effects model. Heterogeneity was tested using I-squared (I2) statistics. A value of I2 was considered to be low with 0–25%, 25–50% as moderate and 50–75% considered as high heterogeneity [12]. In addition, subgroup analyses to test the significant differences in the prevalence of stress, anxiety, depression and sleep disturbance between different groups (setting, frontline or second line; data collection month, NOS,) were performed when there were at least four studies per subgroup. A sensitivity analysis was performed by removing one study at a time to evaluate the impact of pooled prevalence of remining studies [13].
Funnel plots were found to be an inaccurate method for assessing publication bias in meta-analyses of proportion studies [14,15]. Therefore, publication bias was estimated using Egger's liner regression test and funnel plot [16]. A p value of less than 0.05 was considered as statistically significant. Meta-analysis was conducted using Comprehensive Meta-Analysis software, version 2.2 (Englewood, New Jersey, USA). Forest plots were constructed using a Microsoft Excel spreadsheet constructed by Neyeloff et al. [17].
3. Results
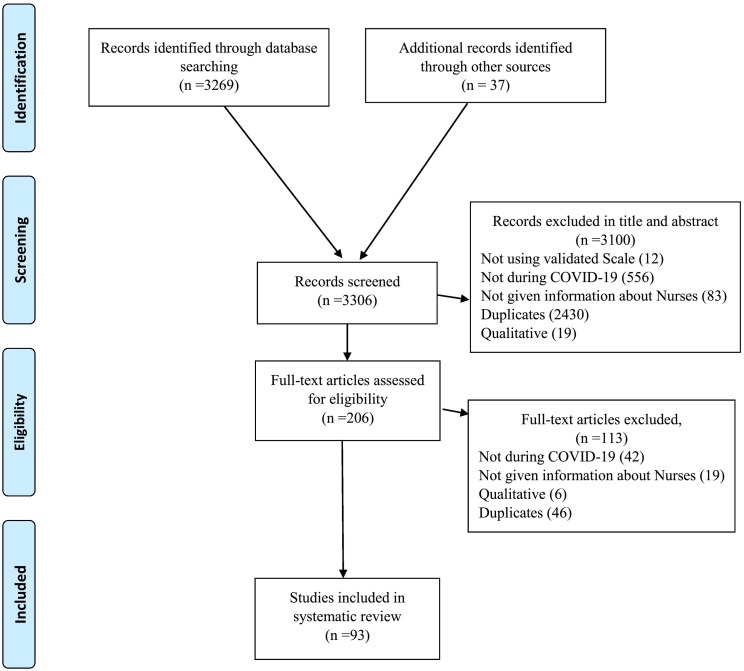
The database search identified 3306 papers; of these, 3100 papers were excluded during title and abstract screening for the following reasons: 556 papers were not conducted during the COVID-19 period; 83 did not give information about nurses; 2430 were duplicated papers. A further, 113 papers were excluded during full text review. As such, 93 studies were identified as eligible for meta-analysis (Fig. 1 shows the PRISMA flow chart).
Fig. 1.
PRISMA diagram.
3.1. General characteristics
Ninety-three studies, involving 93,112 nurses, were included in this meta-analysis. All studies were conducted between January 2020 and September 2020: eight in January, 36 in February, 13 in March, 13 in April, six in May, two in June, two in July and one in September. Twenty preprint studies [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]] were included in the analyses. All studies included in this meta-analysis were of cross sectional design. The vast majority (n = 67 studies) were conducted in hospital settings; seventeen were mixed setting and only nine studies did not provide setting information. Thirty-four studies involved nurses who worked on the frontline in the fight against the COVID-19 epidemic; however, 49 studies involved mixed nurses, i.e. those working in the frontline and second line, whereas ten studies did not give this information. Forty-nine studies originated from China, four from each Turkey and Iran, three from Italy, two each from Germany, Jordan, Nepal, Pakistan, Spain, the USA and the UK, and one from each of the following: Austrian, Bahrain, Croatia, Egypt, Ethiopia, France, Greece, Korea, Kosovo, KSA, Malawi, Mongolian, Poland, Portugal, Russia, Singapore and Switzerland. Two study was conducted in more than one country [38,39]. (See Table 1 for a general characteristics of studies).
Table 1.
Characteristics of the included studies (n = 93):
| Study | Preprint | Setting | Frontline | Country | Month | Measure | Events | Total Sample | Instrument | Cut Off |
NOS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Cai et al., (2020) | No | NG | NG | China | February | Stress | 72 | 546 | SCL-90 | ≥160 | Moderate |
| 2 | Z. Zhu et al., (2020) | No | Hospital | Frontline | China | February | Stress | 1130 | 3417 | IES-R | ˃33 | Low |
| Anxiety | 863 | 3417 | GAD-7 | ≥8 | ||||||||
| Depression | 489 | 3417 | PHQ-9 | ≥10 | ||||||||
| 3 | Choudhury et al., (2020) | No | NG | Mixed | UK | April | Stress | 7 | 23 | PSS-4 | NG | Moderate |
| Anxiety | 7 | 23 | GAD-7 | ≥10 | ||||||||
| Depression | 6 | 23 | PHQ-9 | ≥10 | ||||||||
| 4 | Lai et al., (2020) | No | Hospital | Mixed | China | January | Stress | 569 | 764 | IES-R | ≥26 | Low |
| Anxiety | 360 | 764 | GAD-7 | ≥10 | ||||||||
| Depression | 409 | 764 | PHQ-9 | ≥10 | ||||||||
| Insomnia | 292 | 764 | ISI | ≥15 | ||||||||
| 5 | Liu et al., (2020) | Yes | Hospital | Mixed | China | February | Stress | 432 | 2826 | SRQ-20 | ≥7 | Low |
| Anxiety | 497 | 2826 | SAS | ≥50 | ||||||||
| Depression | 1108 | 2826 | SDS | ≥50 | ||||||||
| 6 | Yin et al., (2020) | No | NG | NG | China | February | Stress | 110 | 246 | PCL-5 | ≥33 | Moderate |
| 7 | J. Zhu et al., (2020) | No | Hospital | Frontline | China | February | Anxiety | 24 | 86 | SAS | ≥50 | Moderate |
| Depression | 37 | 86 | SDS | ≥50 | ||||||||
| 8 | Guo et al., (2020) | Yes | Hospital | Mixed | China | February | Anxiety | 1100 | 5900 | SAS | ≥50 | Low |
| Depression | 2006 | 5900 | SDS | ≥50 | ||||||||
| 9 | Xiao et al., (2020) | No | Hospital | Mixed | China | January | Anxiety | 210 | 359 | HADS | ≥8 | Low |
| Depression | 224 | 359 | HADS | ≥8 | ||||||||
| 10 | Wang et al., (2020) | No | Hospital | Mixed | China | February | Stress | 34 | 202 | PCL-5 | ≥50 | Low |
| 11 | Wang et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 29 | 75 | SAS | ≥50 | Moderate |
| Depression | 10 | 75 | SDS | ≥50 | ||||||||
| Sleep disturbance | 18 | 75 | PSQI | ˃7 | ||||||||
| 12 | Zhang et al., (2020) | No | Hospital | Frontline | China | February | Anxiety | 473 | 984 | GAD-7 | ≥10 | Moderate |
| Depression | 526 | 984 | PHQ-9 | ≥10 | ||||||||
| Insomnia | 395 | 984 | ISI | ≥8 | ||||||||
| 13 | Mo et al., (2020) | No | Hospital | Frontline | China | February | Stress | 59 | 180 | SOS | NG | Moderate |
| Anxiety | 72 | 180 | SAS | ≥50 | ||||||||
| 14 | Huang et al., (2020) | No | Hospital | Frontline | China | February | Stress | 46 | 160 | PTSD | ≥50 | Moderate |
| Anxiety | 43 | 160 | SAS | ≥50 | ||||||||
| 15 | García-Fernández et al., (2020) | No | NG | NG | Spain | March | Stress | 105 | 233 | ASDI | NG | Moderate |
| Anxiety | 213 | 233 | HAM-A | ≥6 | ||||||||
| Depression | 207 | 233 | BDI | ≥ 14 | ||||||||
| 16 | Szepietowski et al., (2020) | No | Hospital | NG | Poland | NG | Anxiety | 13 | 62 | GAD-7 | ≥5 | Moderate |
| Depression | 29 | 62 | PHQ-9 | ≥10 | ||||||||
| 17 | Cui et al., (2020) | Yes | Hospital | Frontline | China | February | Stress | 146 | 481 | PSS | >25 | Moderate |
| Anxiety | 200 | 481 | SAS | ≥50 | ||||||||
| 18 | Du et al., (2020) | No | Hospital | Frontline | China | January | Stress | 30 | 55 | PSS | ≥ 14 | Moderate |
| Anxiety | 21 | 55 | BAI | ≥ 8 | ||||||||
| Depression | 8 | 55 | BDI-II | ≥ 14 | ||||||||
| 19 | Zhou et al., (2020) | No | Hospital | Frontline | China | February | Sleep disturbance | 314 | 1614 | PSQI | ˃7 | Moderate |
| 20 | Jiang et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 319 | 1569 | SAS | ≥50 | Moderate |
| Depression | 514 | 1569 | SDS | ≥53 | ||||||||
| 21 | R. Zhang et al., (2020) | No | Hospital | Mixed | China | February | Stress | 29 | 203 | IES-R | ≥33 | Moderate |
| Anxiety | 29 | 203 | GAD-7 | ≥8 | ||||||||
| Depression | 21 | 203 | PHQ-9 | ≥10 | ||||||||
| Sleep disturbance | 71 | 203 | PSQI | ˃7 | ||||||||
| 22 | S. X. Zhang et al., (2020) | No | NG | NG | Peru, Ecuador, and Bolivia | April | Anxiety | 43 | 175 | GAD-7 | ≥10 | Moderate |
| 23 | Wan et al., (2020) | Yes | Hospital | Mixed | China | February | Anxiety | 775 | 885 | STAI | ≥31 | Moderate |
| 24 | Taghizadeh et al., (2020) | Yes | NG | NG | Iran | April | Anxiety | 72 | 105 | HADS-S | ≥8 | Moderate |
| Depression | 54 | 105 | HADS-D | ≥8 | ||||||||
| 25 | S. X. Zhang et al., (2020a) | No | NG | NG | Iran | February | Anxiety | 20 | 63 | GAD-7 | ≥10 | Moderate |
| Depression | 18 | 63 | PHQ-9 | ≥10 | ||||||||
| 26 | Salman et al., (2020) | Yes | Hospital | Mixed | Pakistan | February | Anxiety | 35 | 133 | GAD-7 | ≥10 | Moderate |
| Depression | 33 | 133 | PHQ-9 | ≥10 | ||||||||
| 27 | Zhpu et al., (2020) | Yes | NG | NG | China | January | Anxiety | 133 | 147 | GAD-7 | ≥10 | Moderate |
| Depression | 114 | 147 | PHQ-9 | ≥10 | ||||||||
| Sleep Disturbance | 94 | 147 | SRSS | ≥ 23 | ||||||||
| 28 | Pan et al., (2020) | No | Hospital | Frontline | China | February | Anxiety | 44 | 148 | GAD-7 | ≥5 | Moderate |
| Depression | 57 | 148 | PHQ-9 | ≥5 | ||||||||
| Insomnia | 129 | 148 | PHQ-15 | ≥10 | ||||||||
| 29 | Ning et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 60 | 295 | SAS | ≥50 | Low |
| Depression | 89 | 295 | SDS | ≥53 | ||||||||
| 30 | Y. Liu et al., (2020) | Yes | Hospital | Mixed | China | February | Stress | 297 | 577 | PSS | ≥14 | Moderate |
| Anxiety | 65 | 577 | GAD-7 | ≥10 | ||||||||
| Depression | 73 | 577 | PHQ-9 | ≥10 | ||||||||
| 31 | Otgonbaatar et al., (2020) | No | Hospital | Mixed | Mongolian | February | Stress | 309 | 473 | WSP | ≥111 | Moderate |
| 32 | Li et al., (2020) | No | Hospital | Mixed | China | February | Stress | 1127 | 3381 | IES-R | ≥33 | Moderate |
| Anxiety | 864 | 3381 | GAD-7 | ≥8 | ||||||||
| Depression | 485 | 3381 | PHQ-9 | ≥10 | ||||||||
| 33 | Lv et al., (2020) | Yes | Hospital | Mixed | China | February | Anxiety | 1280 | 3378 | GAD-7 | ≥5 | Low |
| Depression | 1297 | 3378 | PHQ-9 | ≥5 | ||||||||
| Insomnia | 1253 | 3378 | ISI | ≥8 | ||||||||
| 34 | Hu et al., (2020) | No | Hospital | Frontline | China | January | Anxiety | 833 | 2014 | SAS | ≥50 | Low |
| Depression | 878 | 2014 | SDS | ≥53 | ||||||||
| 35 | B. Wang et al., (2020) | Yes | Hospital | Mixed | China | January | Stress | 59 | 313 | PDSS | ≥11 | Moderate |
| Depression | 100 | 313 | PHQ-9 | ≥10 | ||||||||
| 36 | W. Zhang et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 39 | 197 | PHQ-4 | ≥3 | Moderate |
| Depression | 39 | 197 | PHQ-4 | ≥3 | ||||||||
| Insomnia | 102 | 197 | ISI | ˃8 | ||||||||
| 37 | Weilenmann et al., (2020) | Yes | Hospital | Mixed | Switzerland | April | Anxiety | 161 | 553 | GAD-7 | ≥10 | Moderate |
| Depression | 138 | 553 | PHQ-9 | ≥10 | ||||||||
| 38 | Sahin et al., (2020) | No | Hospital | Mixed | Turkey | April | Anxiety | 226 | 301 | BAI | ≥16 | Moderate |
| 39 | Rossi et al., (2020) | No | Hospital | Mixed | Italy | March | Stress | 105 | 474 | PSS | ≥3 | Low |
| Anxiety | 104 | 474 | GAD-7 | ≥15 | ||||||||
| Depression | 152 | 474 | PHQ-9 | ≥15 | ||||||||
| Insomnia | 55 | 474 | ISI | ˃22 | ||||||||
| 40 | Kaveh et al., (2020) | No | Hospital | Mixed | Iran | March | Anxiety | 213 | 513 | BAI | ≥16 | Moderate |
| 41 | Guixia and Hui, (2020) | No | Hospital | Mixed | China | February | Anxiety | 38 | 92 | SAS | ≥50 | Moderate |
| Depression | 53 | 92 | SDS | ≥53 | ||||||||
| 42 | Al Amer et al., (2020) | Yes | Hospital | Mixed | Jordan | March | Stress | 202 | 405 | DASS | ≥19 | Moderate |
| Anxiety | 208 | 405 | DASS | ≥10 | ||||||||
| Depression | 234 | 405 | DASS | ≥14 | ||||||||
| 43 | Shechter et al., (2020) | No | Hospital | Mixed | USA | April | Stress | 200 | 313 | PTSD | ≥3 | Low |
| Anxiety | 125 | 313 | GAD-2 | ≥3 | ||||||||
| Depression | 166 | 313 | PHQ-2 | ≥3 | ||||||||
| 44 | Naser et al., (2020) | No | Mixed | NG | Jordan | March | Anxiety | 61 | 151 | GAD-7 | ≥15 | Moderate |
| Depression | 70 | 151 | PHQ-9 | ≥15 | ||||||||
| 45 | Que et al., (2020) | No | Mixed | Mixed | China | February | Anxiety | 107 | 208 | GAD-7 | ≥10 | Moderate |
| Depression | 96 | 208 | PHQ-9 | ≥10 | ||||||||
| Insomnia | 70 | 208 | ISI | ≥15 | ||||||||
| 46 | Jahrami et al., (2020) | No | Mixed | Mixed | Bahrain | April | Stress | 95 | 119 | PSS | ≥14 | Moderate |
| Sleep disturbance | 87 | 119 | PSQI | ≥5 | ||||||||
| 47 | Koksal et al., (2020) | No | Mixed | Mixed | Turkey | April | Anxiety | 197 | 339 | HADS | ≥10 | Moderate |
| Depression | 130 | 339 | HADS | ≥7 | ||||||||
| 48 | Tu et al., (2020) | No | Hospital | Frontline | China | February | Anxiety | 40 | 100 | GAD-7 | ≥4 | Low |
| Depression | 46 | 100 | PHQ-9 | ≥10 | ||||||||
| Sleep disturbance | 60 | 100 | PSQI | ≥7 | ||||||||
| 49 | Yang et al., (2020) | Yes | Hospital | Mixed | China | March | Anxiety | 193 | 1017 | SAS | ≥50 | Moderate |
| Depression | 335 | 1017 | SDS | ≥50 | ||||||||
| 50 | Chekole et al., (2020) | No | Mixed | Mixed | Ethiopia | April | Stress | 68 | 100 | PSS | >20 | Moderate |
| 51 | Fang et al., (2020) | Yes | NG | NG | China | NG | Depression | 117 | 293 | SDS | ≥40 | Moderate |
| 52 | Jia et al., (2020) | No | Hospital | Mixed | China | January | Anxiety | 156 | 867 | SAS | ≥50 | Moderate |
| 53 | Zerbini et al., (2020) | No | Hospital | Mixed | Germany | April | Stress | 34 | 75 | PHQ-9 | ≥ 5 | Moderate |
| Anxiety | 12 | 75 | GAD-7 | ≥ 10 | ||||||||
| Depression | 22 | 75 | PHQ-9 | ≥ 10 | ||||||||
| 54 | Pouralizadeh et al., (2020) | No | Hospital | Mixed | Iran | April | Anxiety | 171 | 441 | GAD-7 | ≥10 | Moderate |
| Depression | 165 | 441 | PHQ-9 | ≥10 | ||||||||
| 55 | Gallopeni et al., (2020) | No | Hospital | Mixed | Kosovo | April | Anxiety | 137 | 304 | HADS | ≥11 | Moderate |
| Depression | 106 | 304 | HADS | ≥11 | ||||||||
| 56 | Li et al., (2020a) | No | Hospital | Frontline | China | February | Anxiety | 136 | 176 | HAM-A | ≥14 | Moderate |
| 57 | Chorwe-Sungani, (2020) | Yes | Mixed | Mixed | Malawi | September | Anxiety | 26 | 102 | CAS | ≥9 | Moderate |
| 58 | Saricam, (2020) | No | Hospital | Frontline | Turkey | April | Anxiety | 57 | 123 | STAI | ≥57 | Moderate |
| 59 | Arafa et al., (2020) | No | Hospital | Frontline | KSA & Egypt | April | Stress | 55 | 103 | DASS | ≥10 | Moderate |
| Anxiety | 61 | 103 | DASS | ≥8 | ||||||||
| Depression | 65 | 103 | DASS | ≥8 | ||||||||
| 60 | Silwal et al., (2020) | No | Hospital | Frontline | Nepal | April | Stress | 24 | 152 | DASS | ≥19 | Moderate |
| Anxiety | 64 | 152 | DASS | ≥10 | ||||||||
| Depression | 30 | 152 | DASS | ≥14 | ||||||||
| 61 | Li et al., (2020b) | No | Hospital | Frontline | China | March | Stress | 220 | 356 | PCL-5 | ≥33 | Low |
| 62 | Hong et al., (2020) | No | Hospital | Frontline | China | February | Anxiety | 379 | 4692 | GAD-7 | ≥10 | Low |
| Depression | 442 | 4692 | PHQ-9 | ≥10 | ||||||||
| 63 | Hoedl et al., (2020) | Yes | Mixed | Mixed | Austrian | July | Stress | 1751 | 2602 | PSS | ≥14 | Moderate |
| 64 | Xiaozheng et al., (2020) | No | Hospital | Frontline | China | March | Insomnia | 24 | 97 | AIS | ≥6 | Moderate |
| 65 | Zhan et al., (2020a) | No | Hospital | Frontline | China | March | Stress | 789 | 1794 | PSS | ≥25 | Low |
| Insomnia | 948 | 1794 | AIS | ≥6 | ||||||||
| 66 | AlAteeq et al., (2020) | No | Hospital | Mixed | KSA | March | Anxiety | 44 | 132 | GAD-7 | ≥10 | Moderate |
| Depression | 50 | 132 | PHQ-9 | ≥10 | ||||||||
| 67 | Khanal et al., (2020) | No | Hospital | Frontline | Nepal | May | Anxiety | 94 | 167 | HADS | ≥7 | Moderate |
| Depression | 78 | 167 | HADS | ≥7 | ||||||||
| Insomnia | 50 | 167 | ISI | ≥10 | ||||||||
| 68 | Bachilo et al., (2020) | Yes | Mixed | Mixed | Russia | May | Anxiety | 55 | 139 | GAD-7 | ≥5 | Moderate |
| Depression | 68 | 139 | PHQ-9 | ≥5 | ||||||||
| 69 | Wanigasooriya et al., (2020) | Yes | Hospital | Frontline | UK | July | Stress | 226 | 775 | IES-R | ˃33 | Moderate |
| Anxiety | 276 | 775 | PHQ-4 | ≥3 | ||||||||
| Depression | 255 | 775 | PHQ-4 | ≥3 | ||||||||
| 70 | Leng et al., (2020) | No | Hospital | Frontline | China | February | Stress | 20 | 90 | PSS | ˃25 | Moderate |
| 71 | Aksoy and Koçak, (2020) | No | Mixed | Mixed | Turkey | April | Anxiety | 264 | 726 | STAI | ≥35 | Moderate |
| 72 | Hendy et al., (2020) | No | Hospital | Frontline | Egypt | April | Stress | 293 | 374 | NSS | ≥40 | Moderate |
| 73 | Zhan et al., (2020b) | No | Hospital | Frontline | China | March | Stress | 1298 | 2667 | PSS | ≥25 | Low |
| Anxiety | 1062 | 2667 | GAD-7 | ≥10 | ||||||||
| Depression | 1458 | 2667 | PHQ-9 | ≥10 | ||||||||
| 74 | Skoda et al., (2020) | No | Mixed | Mixed | Germany | March | Anxiety | 172 | 1511 | GAD-7 | ≥10 | Moderate |
| 75 | Nie et al., (2020) | No | Hospital | Frontline | China | February | Stress | 194 | 263 | IES-R | ˃33 | Moderate |
| 76 | Zhu et al., (2020) | No | Mixed | Mixed | China | January | Anxiety | 1502 | 6107 | SAS | ≥50 | Low |
| Depression | 2908 | 6107 | SDS | ≥50 | ||||||||
| 77 | Chen et al., (2020) | No | Mixed | Mixed | China | February | Anxiety | 45 | 311 | GAD-7 | ≥10 | Moderate |
| Depression | 53 | 311 | PHQ-9 | ≥10 | ||||||||
| 78 | Tselebis et al., (2020) | Yes | Hospital | Frontline | Greece | May | Stress | 75 | 150 | PSS | ≥14 | Moderate |
| Insomnia | 74 | 150 | AIS | ≥6 | ||||||||
| 79 | Prasad et al., (2020) | No | Mixed | Mixed | USA | April | Stress | 208 | 248 | IES-R | ˃26 | Moderate |
| Anxiety | 85 | 248 | GAD-7 | ≥10 | ||||||||
| Depression | 54 | 248 | PHQ-2 | ≥3 | ||||||||
| 80 | Lee et al., (2020) | No | Hospital | Frontline | Singapore | June | Anxiety | 52 | 155 | HADS | ≥11 | Moderate |
| Depression | 49 | 155 | HADS | ≥11 | ||||||||
| 81 | Azoulay et al., (2020) | No | Hospital | Frontline | France | May | Anxiety | 249 | 498 | HADS | ≥11 | Moderate |
| Depression | 158 | 498 | HADS | ≥11 | ||||||||
| 82 | Xiong et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 94 | 231 | GAD-7 | ≥10 | Moderate |
| Depression | 61 | 231 | PHQ-9 | ≥10 | ||||||||
| 83 | Sampaio et al., (2020) | No | Mixed | Mixed | Portugal | April | Stress | 210 | 767 | DASS | ≥10 | Moderate |
| Anxiety | 250 | 767 | DASS | ≥6 | ||||||||
| Depression | 166 | 767 | DASS | ≥7 | ||||||||
| 84 | Buselli et al., (2020) | No | Hospital | Frontline | Italy | May | Anxiety | 20 | 133 | GAD-7 | ≥10 | Moderate |
| Depression | 27 | 133 | PHQ-9 | ≥10 | ||||||||
| 85 | Salopek-Žiha et al., (2020) | No | Mixed | Mixed | Croatia | April | Stress | 10 | 97 | DASS | ≥10 | Moderate |
| Anxiety | 12 | 97 | DASS | ≥6 | ||||||||
| Depression | 14 | 97 | DASS | ≥7 | ||||||||
| 86 | Wasim et al., (2020) | No | Hospital | Frontline | Pakistan | June | Insomnia | 46 | 78 | ISI | ≥8 | Moderate |
| 87 | Ahn et al., (2020) | Yes | Hospital | Frontline | Korea | April | Anxiety | 345 | 967 | GAD-7 | ≥5 | Moderate |
| Depression | 172 | 967 | PHQ-9 | ≥10 | ||||||||
| 88 | Zheng et al., (2020) | No | Mixed | Mixed | China | February | Anxiety | 2643 | 3228 | SAS | ≥50 | Low |
| Depression | 2121 | 3228 | SDS | ≥50 | ||||||||
| 89 | Gorini et al., (2020) | No | Hospital | Frontline | Italy | May | Stress | 125 | 214 | IES-R | ˃26 | Moderate |
| Anxiety | 78 | 214 | GAD-7 | ≥10 | ||||||||
| Depression | 66 | 214 | PHQ-2 | ≥3 | ||||||||
| 90 | An et al., (2020) | No | Hospital | Frontline | China | March | Depression | 481 | 1103 | PHQ-9 | ≥10 | Moderate |
| 91 | Zhang et al., (2020) | No | Mixed | Mixed | China | April | Stress | 111 | 468 | PCL | ≥50 | Moderate |
| 92 | Ruiz-Fernández et al., (2020) | No | Hospital | Frontline | Spain | April | Stress | 265 | 348 | PSS | ≥25 | Moderate |
| 93 | Han et al., (2020) | No | Hospital | Mixed | China | February | Anxiety | 4539 | 22,034 | SAS | ≥50 | Low |
| Depression | 6324 | 22,034 | SDS | ≥50 |
AIS = Athens Insomnia Scale; ASDI = Acute Stress Disorder Inventory; BAI=Beck Anxiety Inventory; BDI=Beck Depression Inventory; CAS = Coronavirus Anxiety Scale; DASS=Depression, Anxiety, and Stress Scale; GAD = Generalized Anxiety Disorder; HADS=Hospital Anxiety and Depression Scale; HAM-A = Hamilton Anxiety Rating Scale; IES-R = Impact of Event Scale-Revised; ISI=Insomnia Severity Index; NG = Not Given; NSS=Nursing Stress Scale; PCL-5 = PTSD Checklist for DSM-5; PDSS=Panic Disorder Severity Scale; PHQ = Patient Health Questionnaire; PSQI=Pittsburgh Sleep Quality Index; PSS=Perceived Stress Scale; PTSD=Post-Traumatic Stress Disorder; SAS = Zung Self-rating Anxiety Scale; SCL-90 = Symptom Check-List-90; SDS = Zung Self-rating Depression Scale; SOS=Stress Overload Scale; SRQ = Self-Reporting Questionnaire; SRSS=Sleep Self-Assessment Scale; STAI=State-Trait Anxiety Inventory; WSP=Work Stress Profile.
3.2. Quality assessment
The studies were assessed using the NOS checklist. Nineteen studies were classified as having a low risk of bias and seventy-four as moderate. The detailed results of the quality assessment of the studies included in this meta-analysis are listed in Table 2 .
Table 2.
Quality assessment result of observational studies (n = 93) using the Newcastle-Ottawa Scale:
| Study | Representativeness of the sample (One Point) | Sample Size (One Point) | Non-Respondents (One Point) | Ascertainment of the exposure (One Point) | Study controls for other variable (Two Point) | Assessment of Outcome (One Point) | Statistical Test (One Point) | Adequate Follow up time (One Point) | Score | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Cai et al., (2020) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 | Moderate |
| 2 | Z. Zhu et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 3 | Choudhury et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 4 | Lai et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 5 | Liu et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 6 | Yin et al., (2020) | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 7 | J. Zhu et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 8 | Guo et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 9 | Xiao et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 10 | Wang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Low |
| 11 | Wang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 12 | Zhang et al., (2020) | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 6 | Moderate |
| 13 | Mo et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 14 | Huang et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 15 | García-Fernández et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 16 | Szepietowski et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 17 | Cui et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 18 | Du et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 19 | Zhou et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 20 | Jiang et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 21 | R. Zhang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 22 | S. X. Zhang et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 23 | Wan et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 24 | Taghizadeh et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 25 | S. X. Zhang et al.,(2020a) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 26 | Salman et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 27 | Zhpu et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 28 | Pan et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 29 | Ning et al.,(2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 30 | Y. Liu et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 31 | Otgonbaatar et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 32 | Li et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 33 | Lv et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 34 | Hu et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 35 | B. Wang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 36 | W. Zhang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 37 | Weilenmann et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 38 | Sahin et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 39 | Rossi et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 40 | Kaveh et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 41 | Guixia and Hui, (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 42 | Al Amer et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 43 | Shechter et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 44 | Naser et al., (2020) | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 45 | Que et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 46 | Jahrami et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 47 | Koksal et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 48 | Tu et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 49 | Yang et al., (2020) | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 50 | Chekole et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 51 | Fang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 52 | Jia et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 53 | Zerbini et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 54 | Pouralizadeh et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 55 | Gallopeni et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 56 | Li et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 57 | Chorwe-Sungani, (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 58 | Saricam, (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 59 | Arafa et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 60 | Silwal et al., (2020) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 | Moderate |
| 61 | Li et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 62 | Hong et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 63 | Hoedl et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 64 | Xiaozheng et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 65 | Zhan et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 66 | AlAteeq et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 67 | Khanal et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 68 | Bachilo et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 69 | Wanigasooriya et al., (2020) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 | Moderate |
| 70 | Leng et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 71 | Aksoy and Koçak, (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 72 | Hendy et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 73 | Zhan et al., (2020b) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 74 | Skoda et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 75 | Nie et al., (2020) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 | Moderate |
| 76 | Zhu et al., (2020) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low |
| 77 | Chen et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 78 | Tselebis et al., 2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 79 | Prasad et al., 2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 80 | Lee et al., 2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 81 | Azoulay et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 82 | Xiong et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 83 | Sampaio et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate |
| 84 | Buselli et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 85 | Salopek-Žiha et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 86 | Wasim et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 87 | Ahn et al., (2020) | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate |
| 88 | Zheng et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
| 89 | Gorini et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 90 | An et al., (2020) | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 6 | Moderate |
| 91 | Zhang et al., (2020) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | Moderate |
| 92 | Ruiz-Fernández et al., (2020) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate |
| 93 | Han et al., (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | Low |
3.3. Prevalence of stress
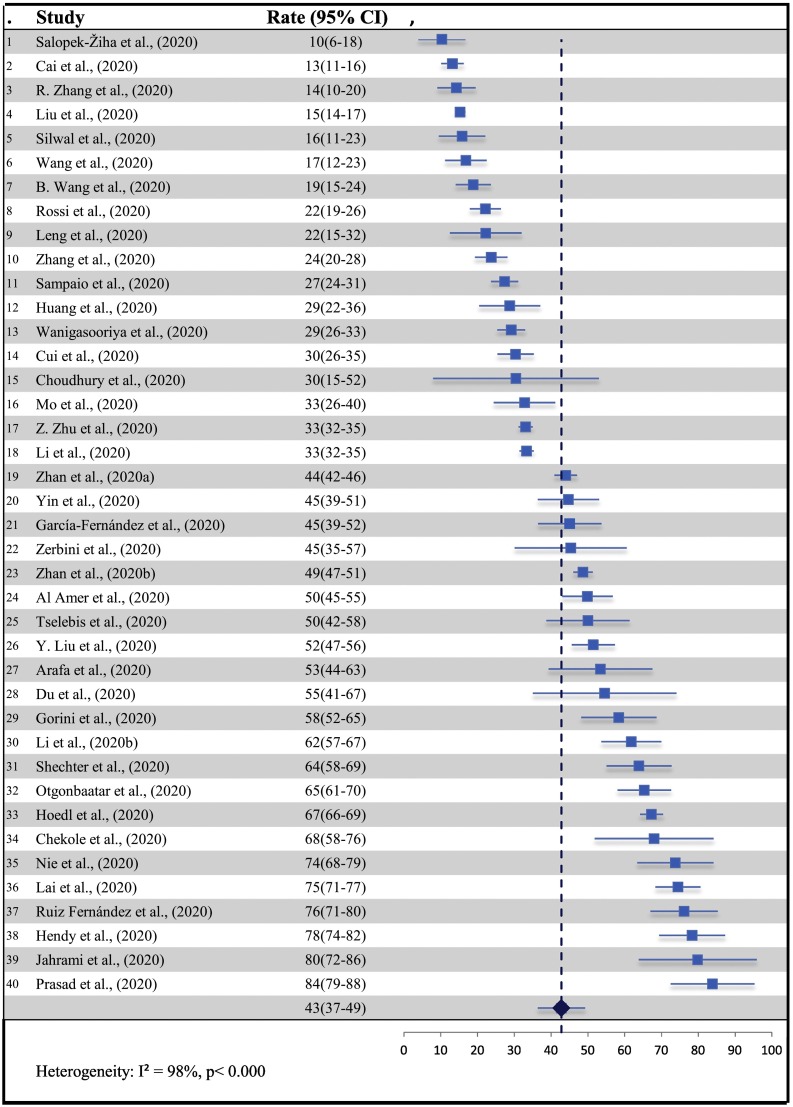
Stress was estimated in 40 studies [18,20,25,27,29,33,35,36,[39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70]]. The overall pooled point estimates of prevalence for stress varied between 10% and 84% (Fig. 2 : forest plots). All meta-analyses of prevalence estimates of stress reported by the 40 studies yielded a summary prevalence of 43% (11,139/27,034 participants, 95% CI 37–49). Sensitivity analysis by excluding one study each time demonstrated that no differences in the overall estimation by more or less than 1%. There was significant heterogeneity between studies to estimate the prevalence (p < 0.000, I2 = 98).
Fig. 2.
Forest Plot of the Prevalence of Stress (N = 40).
The pooled prevalence according to the month of data collected was as follows: February: 32% (n = 14; 95% CI 25–41; I2 = 98), March: 45% (n = 6; 95% CI 37–53; I2 = 96) and April: 50% (n = 13; 95% CI 35–66; I2 = 98). Seventeen studies [20,35,36,39,43,44,46,54,[57], [58], [59], [60], [61], [62], [63],67,69] involving nurses who were working on the frontline showed stress prevalence at 46% (95% CI = 39–54; I2 = 97), whereas 20 studies including mixed nurses working in the frontline and second line showed the stress prevalence was 42% (95% CI = 31–53, I2 = 99). Thirteen studies that used the Perceived Stress Scale (PSS) showed a pooled prevalence of stress at 50% (95% CI = 41–59, I2 = 98), whereas eight studies [35,45,[54], [55], [56],63,64,67] using the Impact of Event Scale-Revised (IES-R) had a pooled prevalence of 50% (95% CI = 37–63, I2 = 99). The other studies used different scales. In the subgroup analyses using the NOS, the pooled prevalence in studies (n = 9) with low risk of bias accounted for 41% (95% CI = 29–54, I2 = 99), whereas those with a moderate risk of bias (n = 31) accounted for 43% (95% CI = 36–52, I2 = 98).
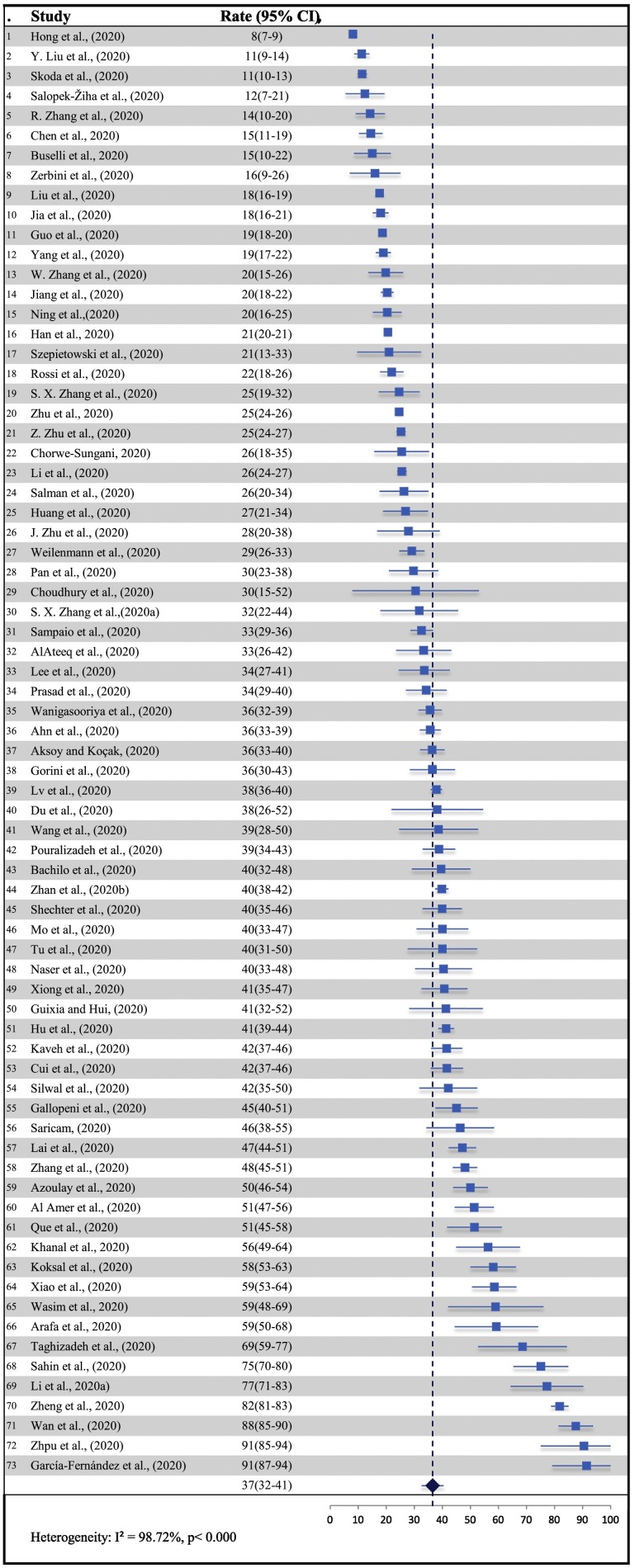
3.4. Prevalence of anxiety
The overall pooled point estimates of prevalence for anxiety varied between 8% and 91%, which was reported by 73 studies [[18], [19], [20], [21], [22], [23], [24], [25], [26],[28], [29], [30],32,34,35,[37], [38], [39],[42], [43], [44], [45], [46],48,49,51,[53], [54], [55], [56], [57],62,[64], [65], [66], [67],[71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106]] (Fig. 3 : forest plots). All meta-analyses of prevalence estimates of anxiety yielded a summary prevalence of 37% (23,535/81,561 participants, 95% CI 32–41). The pooled prevalence did not change in sensitivity analysis by excluding one study each time by less than 2%. There was significant heterogeneity between studies to estimate the prevalence (p < 0.000, I2 = 99).
Fig. 3.
Forest Plot of the Prevalence of Anxiety (N = 73).
The prevalence of anxiety among nurses who worked on the frontline (n = 24) was high at 39% (95% CI = 32–46, I2 = 98) compared to mixed studies (n = 42), which was 32% (95% CI = 27–38, I2 = 99%). In the subgroup analyses by month, according to when the study was conducted, the pooled prevalence of anxiety was 45% (n = 7; 95% CI = 33–58, I2 = 99), 32% (n = 29; 95% CI = 25–40, I2 = 99), 38% (n = 9; 95% CI = 26–52, I2 = 98), 40% (n = 18; 95% CI = 34–46.2, I2 = 95) and 39% (n = 5; 95% CI = 28–51, I2 = 93) for January, February, March, April and May, respectively. Thirty-two studies used the Generalized Anxiety Disorder-7 (GAD-7) scale, which showed the highest anxiety prevalence at 30% (95% CI = 25–35, I2 = 98), whereas studies (n = 16) using the Zung Self-Rating Anxiety Scale (SAS) reported anxiety prevalence at 30% (95% CI = 22–39, I2 = 99). The prevalence of anxiety in the low risk of bias studies (n = 16) was 32% (95% CI = 24–41, I2 = 99); in studies (n = 57) with a moderate risk of bias, the pooled prevalence was 38% (95% CI = 33–43, I2 = 97).
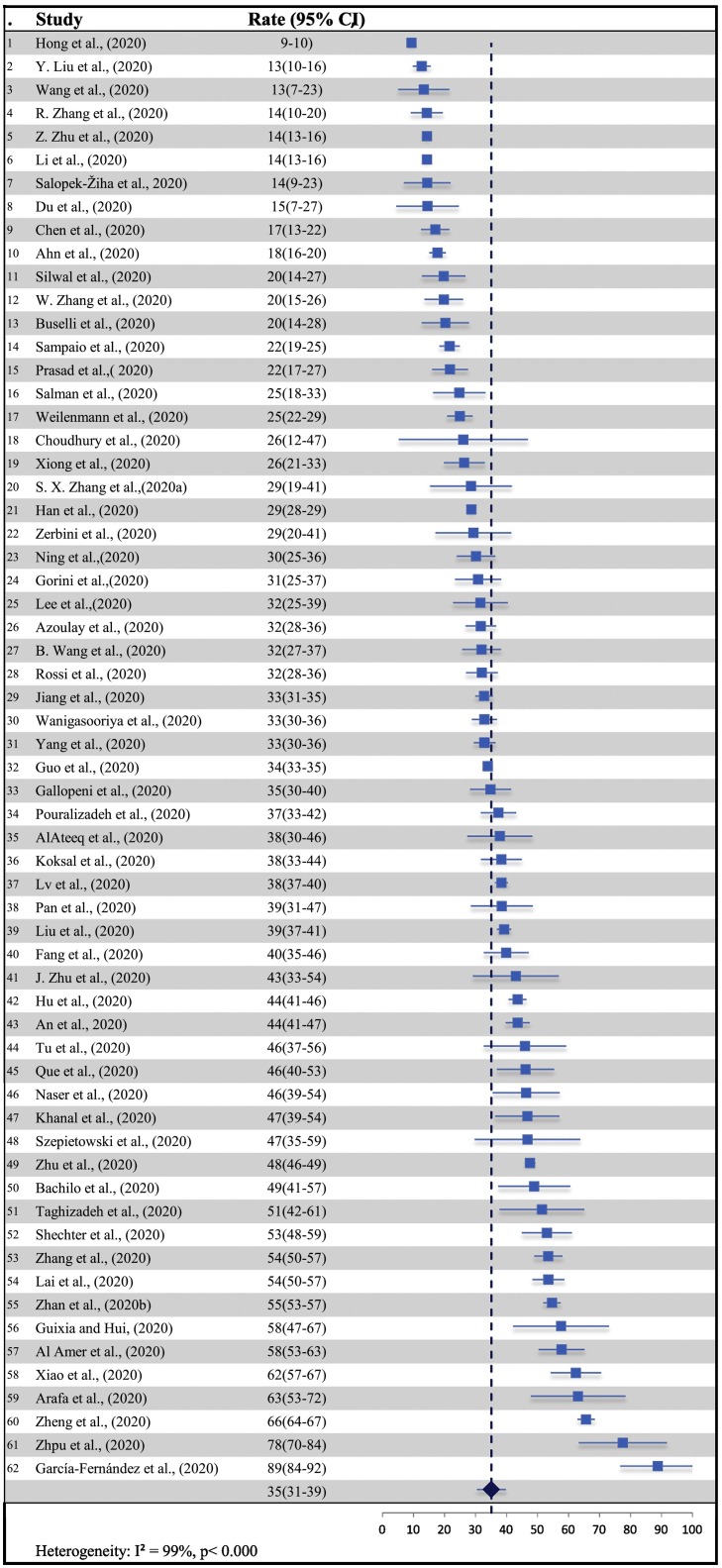
3.5. Prevalence of depression
The overall pooled point estimates of depression reported by the 62 studies [19,[22], [23], [24], [25], [26], [27], [28], [29], [30], [31],34,35,37,39,42,43,45,48,49,51,[53], [54], [55], [56], [57],62,[64], [65], [66], [67],[71], [72], [73], [74],[77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88],90,91,[94], [95], [96],[99], [100], [101], [102], [103],[105], [106], [107], [108]] varied between 9% and 89% (Fig. 4 : forest plots). The pooled point prevalence of depression was 35% (25,769/76,992 participants, 95% CI 31–39). In sensitivity analysis, no study had an implication for the pooled prevalence by more or less than 1%. There was significant heterogeneity between studies to estimate the prevalence (p < 0.000, I2 = 99). The pooled prevalence according to the month of data collected was as follows: January: 49% (n = 7; 95% CI 42–56; I2 = 95), February: 29% (n = 24; 95% CI 24–35; I2 = 99), March: 50% (n = 8; 95% CI 27–45; I2 = 97), April: 31% (n = 14; 95% CI 25–39; I2 = 95) and May: 35.1% (n = 5; 95% CI 27–45; I2 = 89). Nineteen studies involving nurses who were working on the frontline showed the depression prevalence at 33% (95% CI = 24–43, I2 = 99), whereas 36 studies including nurses working on the frontline and second line showed the depression prevalence was 33% (95% CI = 29–37, I2 = 98).
Fig. 4.
Forest Plot of the Prevalence of Depression (N = 62).
Twenty-nine studies used the Patient Health Questionare-9 (PHQ-9) scale had a pooled prevalence of 32% (95% CI = 25–40, I2 = 99), whereas thirteen studies used the Zung Self-Rating Depression Scale (SDS) had a pooled prevalence of 39% (95% CI = 32–46, I2 = 99). The other studies used different scales. In the subgroup analyses using the NOS, the pooled prevalence in studies (n = 16) with low risk of bias was 39% (95% CI = 32–47, I2 = 99), whereas the moderate risk of bias studies (n = 46) accounted for 34% (95% CI = 29–39, I2 = 97).
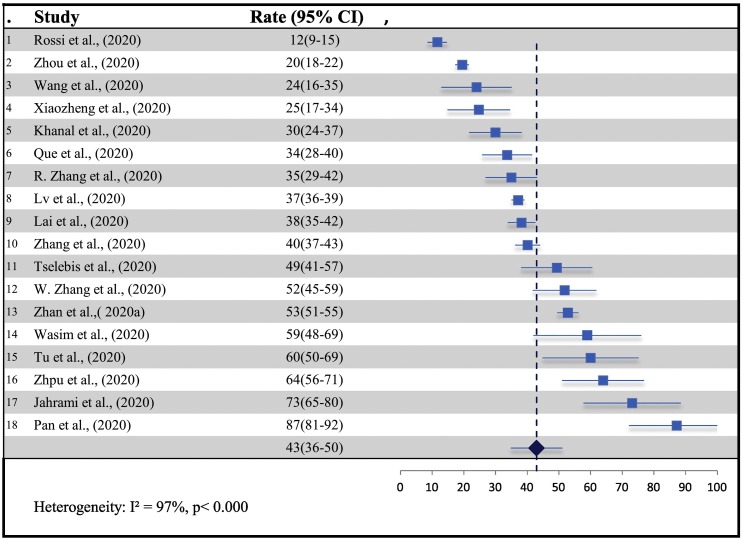
3.6. Prevalence of sleep disturbance
The prevalence rate of sleep disturbance in 18 studies [24,26,36,48,52,55,56,59,72,79,82,84,86,88,96,104,109,110] ranged from 12% to 87% (Fig. 5 : Forest plots) with pooled prevalence estimates of 43% (4082/10,697 participants, 95% CI 36–50). In sensitivity analysis, no study had an implication for the pooled prevalence by more or less than 2%. There was significant heterogeneity between studies to estimate the prevalence (p < 0.000, I2 = 97). The studies (n = 9) including frontline nurses reported the prevalence of sleep disturbance at 47% (95% CI = 34–60.1, I2 = 98), whereas the studies (n = 8) including mixed nurses reported the prevalence at 37% (95% CI = 28–46, I2 = 96).
Fig. 5.
Forest Plot of the Prevalence of Sleep Disturbance (N = 18).
Eight studies used the Insomnia Severity Index (ISI) scale with a pooled prevalence of 36% (95% CI = 30–43, I2 = 95), whereas five studies used the Pittsburgh Sleep Quality Index (PSQI) with a pooled prevalence of 41% (95% CI = 22–64, I2 = 98). The other studies used different scales. In the subgroup analyses using the NOS, the pooled prevalence in studies (n = 5) with low risk of bias was 38% (95% CI = 27–50, I2 = 98), whereas the moderate risk of bias studies (n = 13) accounted for 45% (95% CI = 35–57, I2 = 97).
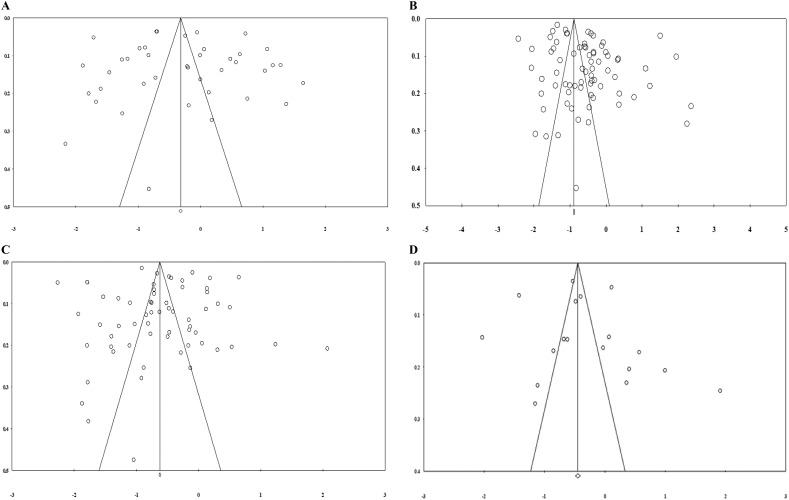
3.7. Publication bias
Funnel plots indicated evidence of publication bias using visual inspection (Fig. 6 ). However, Egger's regression test in stress (n = 40) (p = 0.42), anxiety (n = 73) (p = 0.29), depression (n = 38) (p = 0.35) and sleep disturbance (n = 18) (p = 0.38) did not show presence of publication bias.
Fig. 6.
Funnel plots test publication bias as following A:Stress (n = 40 studies); B: Anixity (n = 73 studies) C: Depression (n = 62); and D: Sleep Disterbance (n = 18).
4. Discussion
The psychological health of nurses during the COVID-19 pandemic is important, as this can impact their performance and reduce the quality of care provided. Sadly, there have been several reports of suicides among healthcare professionals due to psychological pressures and the possible fear of dying [111,112].
This meta-analysis is the first to estimate the aggregate prevalence of stress, anxiety, depression and sleep disturbance among nurses during the COVID-19 pandemic. The review included 93 cross-sectional studies of a total of 93,112 nurses showing high proportions of those symptoms. The aggregate prevalence of stress, anxiety, depression and sleep disturbance (43%, 37%, 35% and 43%, respectively) among nurses during the COVID-19 outbreak suggests that at least one third of nurses have experienced stress, anxiety, depression and sleep disturbance. These results are higher than those reported in the general population during the same period. Shi et al. [113] reported that in the general population, 24% of people had stress, 32% had anxiety, 28% had depression and 29% had insomnia. This was because the nurses were more exposed to patients with COVID-19.
The results of current review are even higher when compared with the reported prevalence during the MERS and SARS epidemics among nurses: 11% for stress [114], 20% for depression [115], 30% for anxiety [116] and 10% for sleep disturbance [117]. This may be because COVID-19 is rapidly spread, is human-to-human transmissible [1], and is potentially fatal. These factors are exacerbated by the shortage of personal protective equipment, increased working hours and new or unfamiliar clinical guidelines for the management of COVID-19 patients [118]. Altogether, these factors can increase nurses' experience of stress, anxiety, depression and sleep disturbance.
This meta-analysis found that the pooled prevalence varied between studies; for example, ranging between 10% [66] - 84% [52,64] for stress, 8% [94] - 91% [51] for anxiety, 9% [94] - 89% [51] for depression and 12% [48] - 87% [72] for sleep disturbance. This could be explained by the diversity of the assessment scale, healthcare system, population characteristics and lifestyles. Another possible reasons of differences in prevalence the variation in cut-offs scores of elevated symptoms for same instrument. For example; as shown in Table 1, the cut-off score of IES-R scale in Zhu et al. [54] was ˃33, whereas Lai et al. [55] used ≥26. The GAD-7 cut off score was ≥8 in Zhang et al. [56] and ≥ 10 by Zhpu et al. [24]. In depression, Lv et al. [26] used ≥5, while Li et al. [45] used ≥10 as cut off score of PHQ-9. The ISI cut off score was ≥15 in Que. et al. [82], whereas ˃8 in Zhang et al. [88].
The studies' quality was assessed using the NOS; all studies fell into the medium-quality and low-quality categories. The bias mainly involved the selection and size of samples, and follow-up time. Therefore, the amount of heterogeneity between the studies in terms of pooled prevalence and moderate analyses were low. Most importantly the Egger's test showed an absence of a publication bias.
The major strength of this meta-analysis is the large sample size of over 93,112 articles drawn from 93 studies, which estimated the psychological impacts on nurses during the COVID-19 outbreak. However, there are several potential limitations to this this meta-analysis. First, this review searched medRxiv's preprint studies, which are still not peer reviewed, which may introduce publication bias. Second, the majority of the studies (n = 69) were conducted in Asia, the generalization of the finding may be limited. Third, there is a possibility that some studies were not included in this meta-analysis, although this analysis used different MeSH terms and several databases. In addition, only studies published, unpublished or translated into English were included in this analysis. Fourth, stress, anxiety, depression and sleep disturbance were assessed using various scales and measures; this led to variability between studies and could increase the errors of prevalence estimates. Fifth, there were insufficient data available on the demographic and clinical characteristics, so not all information could be eliminated thoroughly. Finally, all findings were derived from cross-sectional design, which can reduce the ability to draw conclusions about changes in the psychological symptoms and associated factor [119]. It is important for further research to conduct a longitudinal study to identify the prevalence of symptoms during and after the infectious disease outbreaks.
Altogether, stress, anxiety, depression and sleep disturbance are significant problems for nurses worldwide during an infection disease outbreaks. The results of this meta-analysis have a number of potential implications for interventions to improve the psychological wellbeing of nurses during crises. For example, organizations should provide counselling support services or online workshops and training material to enable them to come over any psychological problems [120].
In addition, they should improve the working conditions of nurses by increasing manpower and resource allocation. Nurse managers play a crucial role through effective communication, rotating nurses, implementing flexible schedules and encouraging nurses to use psychosocial and psychological support service [121].
5. Conclusions
This is the first systematic review and meta-analysis reporting pooled prevalence estimates for stress, anxiety, depression and sleep disturbance among nurses during the COVID-19 outbreak. The findings show that over one third of nurses have experienced stress, anxiety, depression and sleep disturbance during the COVID-19 outbreak, which is higher than the previous MERS and SARS epidemics. Furthermore, these results highlight the need for appropriate interventions that can reduce psychological impacts on nurses.
Funding
No sources of funding.
Contributions
A.M and A.J and A.B designed the protocol, literature search, data synthesis interpreted the results, and wrote the manuscript and contributed to the conceptualization and design and the manuscript preparation.
Declaration of Competing Interest
The authors certify that there is no actual or potential conflict of interest in relation to this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychores.2020.110343.
Appendix A. Supplementary data
Appendix A: Searching Terms.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization, Statement on the second meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV), (2020) 2005. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov
- 3.WHO WHO Coronavirus Disease (COVID-19) Dashboard. 2020. https://covid19.who.int
- 4.ICN . ICN - Int. Counc. Nurses. 2020. More than 600 nurses die from COVID-19 worldwide.https://www.icn.ch/news/more-600-nurses-die-covid-19-worldwide (accessed June 14, 2020) [Google Scholar]
- 5.Chong M.-Y., Wang W.-C., Hsieh W.-C., Lee C.-Y., Chiu N.-M., Yeh W.-C., Huang O.-L., Wen J.-K., Chen C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry J. Ment. Sci. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 6.Lee S.M., Kang W.S., Cho A.-R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brooks S.K., Dunn R., Amlôt R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018;60:248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 8.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiao J., Fang M., Chen Q., He B. SARS, MERS and COVID-19 among healthcare workers: a narrative review. J. Infect. Public Health. 2020;13:843–848. doi: 10.1016/j.jiph.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Well G.A., Shea B., O'Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2020. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 11.Li M., Katikireddi S.V. Urban-rural inequalities in suicide among elderly people in China: a systematic review and meta-analysis. Int. J. Equity Health. 2019;18:2. doi: 10.1186/s12939-018-0881-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patsopoulos N.A., Evangelou E., Ioannidis J.P.A. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008;37:1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunter J.P., Saratzis A., Sutton A.J., Boucher R.H., Sayers R.D., Bown M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014;67:897–903. doi: 10.1016/j.jclinepi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Moreno S.G., Sutton A.J., Ades A., Stanley T.D., Abrams K.R., Peters J.L., Cooper N.J. Assessment of regression-based methods to adjust for publication bias through a comprehensive simulation study. BMC Med. Res. Methodol. 2009;9:2. doi: 10.1186/1471-2288-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neyeloff J.L., Fuchs S.C., Moreira L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res. Notes. 2012;5:52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Z., Han B., Jiang R., Huang Y., Ma C., Wen J., Zhang T., Wang Y., Chen H., Ma Y. Mental Health Status of Doctors and Nurses During COVID-19 Epidemic in China. Lancet. 2020 doi: 10.2139/ssrn.3551329. [DOI] [Google Scholar]
- 19.Guo J., Liao L., Wang B., Li X., Guo L., Tong Z., Guan Q., Zhou M., Wu Y., Zhang J., Gu Y. Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. Lancet Psychiatry. 2020 doi: 10.2139/ssrn.3550050. [DOI] [Google Scholar]
- 20.Cui S., Jiang Y., Shi Q., Zhang L., Kong D., Qian M., Chu J. Impact of COVID-19 on psychology of nurses working in the emergency and fever outpatient:A cross-sectional survey. BMC Psychiatry. 2020 doi: 10.21203/rs.3.rs-20777/v1. [DOI] [Google Scholar]
- 21.Wan Z., Lian M., Ma H., Cai Z., Xianyu Y. Factors Associated with Burnout among Chinese Nurses during COVID-19 Epidemic: a cross-sectional study. BMC Nurs. 2020 doi: 10.21203/rs.3.rs-31486/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taghizadeh F., Hassannia L., Moosazadeh M., Zarghami M., Taghizadeh H., Dooki A.F., Navaei R.A., Hedayatizadeh-Omran A. Anxiety and Depression in Health Workers and General Population During COVID-19 Epidemic in IRAN: A Web-Based Cross-Sectional Study. MedRxiv. 2020 doi: 10.1101/2020.05.05.20089292. 2020.05.05.20089292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salman M., Raza M.H., Mustafa Z.U., Khan T.M., Asif N., Tahir H., Shehzadi N., Hussain K. The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: a web-based, cross-sectional study from Pakistan. MedRxiv. 2020 doi: 10.1101/2020.06.03.20119867. 2020.06.03.20119867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhpu P., Du N., OuYang Y. 2020. Investigation on the Mental Health of Healthcare Workers for Aid in Hu Bei Province During the Outbreak of Covid-19 Based on the Network Survey. [DOI] [Google Scholar]
- 25.Liu Y., Liu X., Gao B., Li C., Liang X. 2020. Mental distress among frontline healthcare workers outside the central epidemic area during the novel coronavirus disease (COVID-19) outbreak in China: A cross-sectional study. [DOI] [Google Scholar]
- 26.Lv Y., Yao H., Xi Y., Zhang Z., Zhang Y., Chen J., Li J., Li J., Wang X., Luo G.Q. 2020. Social Support Protects Chinese Medical Staff from Suffering Psychological Symptoms in COVID-19 Defense, Lancet Psychiatry. [DOI] [Google Scholar]
- 27.Wang B., Sun J., Gao F., Chen J., Shi L., Li L., Tang Y., Wang K., Lu H. A study on mental health status among the staff in a designated hospital for COVID-19. Prepr. Res. Sq. 2020 doi: 10.21203/rs.3.rs-23224/v1. [DOI] [Google Scholar]
- 28.Weilenmann S., Ernst J., Petry H., Sazpinar O., Pfaltz M.C., Gehrke S., Paolercio F., von Kaenel R., Spiller T.R. Health Care WorkersMental Health During the First Weeks of the SARS-CoV-2 Pandemic in Switzerland: A Cross-Sectional Study. MedRxiv. 2020 doi: 10.1101/2020.05.04.20088625. 2020.05.04.20088625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al Amer R., Malak M., Aburumman G., Darwish M., Nassar M., Darwish M., Randal S. 2020. Prevalence and Correlates of Psychological Reactions Among Jordanian Nurses During the Coronavirus Disease 2019. [DOI] [Google Scholar]
- 30.Yang M., He P., Xu X., Wang J., Wang Y., Liu K., Wen L., Xiao X., He Y., Tang W., Zhao R., Cao Y., Chen L., Wei Y., Lan C., Wang X., Wang B., Wang W., Zhao M., Zhao M., Lin H., Yue R., Deng M., Deng T., Kuang L., Chen D. Disrupted Rhythms of Life, Work and Entertainment Behaviours and Their Associations with Mental Health Problems under the Stress of COVID-19 Epidemic: A Survey in 5854 Chinese People with Different Backgrounds. Res. Sq. 2020 doi: 10.21203/rs.3.rs-27400/v1. [DOI] [Google Scholar]
- 31.Fang X.-H., Wu L., Lu L.-S., Kan X.-H., Wang H., Xiong Y.-J., Ma D.-C., Wu G.-C. Analysis on mental health status and needs of health care workers in designated medical institutions of tuberculosis during the epidemic period of COVID-19. BMC Psychiatry. 2020 doi: 10.21203/rs.3.rs-25934/v1. [DOI] [Google Scholar]
- 32.Chorwe-Sungani G. Assessing COVID-19 related anxiety among nurses in Malawi. Res. Sq. 2020 doi: 10.21203/rs.3.rs-79619/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoedl M., Bauer S., Eglseer D. Influence of nursing staff working hours on the stress level during the COVID-19 pandemic: a cross-sectional online survey. MedRxiv. 2020 doi: 10.1101/2020.08.12.20173385. 2020.08.12.20173385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bachilo E., Barylnik J., Shuldyakov A., Efremov A., Novikov D. Mental Health of Medical Workers during the COVID-19 Pandemic in Russia: Results of a Cross-Sectional Study. MedRxiv. 2020 doi: 10.1101/2020.07.27.20162610. Submitted for publication. [DOI] [Google Scholar]
- 35.Wanigasooriya K., Palimar P., Naumann D., Ismail K., Fellows J.L., Logan P., Thompson C.V., Bermingham H., Beggs A.D., Ismail T. Mental health symptoms in a cohort of hospital healthcare workers following the first peak of the Covid-19 pandemic in the United Kingdom. MedRxiv. 2020 doi: 10.1101/2020.10.02.20205674. 2020.10.02.20205674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tselebis A., Lekka D., Sikaras C., Tsomaka E., Tassopoulos A., Ilias I., Bratis D., Pachi A. Sleep Disorders, Perceived Stress and Family Support Among Nursing Staff During the Pandemic Crisis. Res. Sq. 2020 doi: 10.21203/rs.3.rs-44847/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahn M.H., Shin Y.-W., Kim J.H., Kim H.J., Lee K.-U., Chung S. High Work-related Stress and Anxiety Response to COVID-19 among Healthcare Workers in South Korea: SAVE study. PsyArXiv. 2020 doi: 10.31234/osf.io/9nxth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang S.X., Sun S., Jahanshahi A.A., Alvarez-Risco A., Ibarra V.G., Li J., Patty-Tito R.M. Developing and testing a measure of COVID-19 organizational support of healthcare workers – results from Peru. Ecuador, and Bolivia, Psychiatry Res. 2020;113174 doi: 10.1016/j.psychres.2020.113174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arafa A., Mohammed Z., Mahmoud O., Elshazley M., Ewis A. Depressed, anxious, and stressed: what have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chekole Y.A., Yimer S., Mekuriaw B., Mekonnen S. Prevalence and risk factors of perceived stress on COVID-19 among health care providers in Dilla town health institutions, southern Ethiopia: a cross-sectional study. Adv. Public Health. 2020;7 doi: 10.1155/2020/5036861. [DOI] [Google Scholar]
- 41.Cai W., Lian B., Song X., Hou T., Deng G., Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona virus disease 2019. Asian J. Psychiatr. 2020;51:102111. doi: 10.1016/j.ajp.2020.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choudhury T., Debski M., Wiper A., Abdelrahman A., Chalil S., More R., Goode G., Patel B., Abdelaziz H.K., Wild S. Covid-19 Pandemic: Looking after the Mental Health of our Healthcare Workers. J. Occup. Environ. Med. 2020 doi: 10.1097/JOM.0000000000001907. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 43.Du J., Dong L., Wang T., Yuan C., Fu R., Zhang L., Liu B., Zhang M., Yin Y., Qin J., Bouey J., Zhao M., Li X. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry. 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Laodong Weisheng Zhiyebing Zazhi. 2020;38:192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 45.Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., Zhang C., Zhu S., Zhu Z., Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatry. 2020 doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- 46.Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., Qin M., Huang H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. n/a. 2020 doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Otgonbaatar D., Ts L., Ariunaa D., Tundevrentsen A., Naranbaatar N., Munkhkhand J. Occupational stress in nurse sAA—the study provided during the urged pandemic COVID-19 quarantine period. Psychology. 2020;11:704–712. doi: 10.4236/psych.2020.115048. [DOI] [Google Scholar]
- 48.Rossi R., Socci V., Pacitti F., Lorenzo G.D., Marco A.D., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open. 2020;3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., Claassen J., Cornelius T., Derby L., Dong M., Givens R.C., Hochman B., Homma S., Kronish I.M., Lee S.A.J., Manzano W., Mayer L.E.S., McMurry C.L., Moitra V., Pham P., Rabbani L., Rivera R.R., Schwartz A., Schwartz J.E., Shapiro P.A., Shaw K., Sullivan A.M., Vose C., Wasson L., Edmondson D., Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yin Q., Sun Z., Liu T., Ni X., Deng X., Jia Y., Shang Z., Zhou Y., Liu W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin. Psychol. Psychother. 2020;27:384–395. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.García-Fernández L., Romero-Ferreiro V., López-Roldán P.D., Padilla S., Calero-Sierra I., Monzó-García M., Pérez-Martín J., Rodriguez-Jimenez R. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol. Med. 2020:1–3. doi: 10.1017/S0033291720002019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jahrami H., BaHammam A.S., AlGahtani H., Ebrahim A., Faris M., AlEid K., Saif Z., Haji E., Dhahi A., Marzooq H., Hubail S., Hasan Z. 2020. The Examination of Sleep Quality for Frontline Healthcare Workers during the Outbreak of COVID-19, Sleep Breath. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zerbini G., Ebigbo A., Reicherts P., Kunz M., Messman H. Psychosocial burden of healthcare professionals in times of COVID-19 – a survey conducted at the University Hospital Augsburg. Ger. Med. Sci. 2020;18 doi: 10.3205/000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W., Zhu S., Fan Y., Chen Y., Hu J., Liu J., Wang W. COVID-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24:100443. doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang R., Hou T., Kong X., Wang G., Wang H., Shuyu X., Jingzhou X., Jingwen H., Lei X., Wang Y., Jing D., Huang Y., Su T., Tang Y. Effects of region, epidemic stage, and demographic characteristics on sleep quality and mental disturbances among health care workers during COVID-19 outbreak. BMC Health Serv. Res. 2020 doi: 10.3886/E119159V1. [DOI] [Google Scholar]
- 57.Silwal M., Koirala D., Koirala S., Lamichhane A. Depression, Anxiety and Stress among Nurses during Corona Lockdown in a Selected Teaching Hospital, Kaski, Nepal. J. Health Allied Sci. 2020;10:82–87. doi: 10.37107/jhas.210. [DOI] [Google Scholar]
- 58.Li X., Zhou Y., Xu X. Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: A predictive study. J. Nurs. Manag. n/a. 2020 doi: 10.1111/jonm.13146. [DOI] [PubMed] [Google Scholar]
- 59.Zhan Y., Liu Y., Liu H., Li M., Shen Y., Gui L., Zhang J., Luo Z., Tao X., Yu J. Factors associated with insomnia among Chinese front-line nurses fighting against COVID-19 in Wuhan: a cross-sectional survey. J. Nurs. Manag. 2020;28 doi: 10.1111/jonm.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leng M., Wei L., Shi X., Cao G., Wei Y., Xu H., Zhang X., Zhang W., Xing S., Wei H. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs. Crit. Care. n/a. 2020 doi: 10.1111/nicc.12528. [DOI] [PubMed] [Google Scholar]
- 61.Hendy A., Abozeid A., Sallam G., Fattah H.A.A., Reshia F.A.A. Predictive factors affecting stress among nurses providing care at COVID-19 isolation hospitals at Egypt. Nurs. Open. n/a. 2020 doi: 10.1002/nop2.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhan Y., Zhao S., Yuan J., Liu H., Liu Y., Gui L., Zheng H., Zhou Y., Qiu L., Chen J., Yu J., Li S. Prevalence and influencing factors on fatigue of first-line nurses combating with COVID-19 in China: a descriptive cross-sectional study. Curr. Med. Sci. 2020:1–11. doi: 10.1007/s11596-020-2226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nie A., Su X., Zhang S., Guan W., Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J. Clin. Nurs. 2020;29:4217–4226. doi: 10.1111/jocn.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Prasad A., Civantos A.M., Byrnes Y., Chorath K., Poonia S., Chang C., Graboyes E.M., Bur A.M., Thakkar P., Deng J., Seth R., Trosman S., Wong A., Laitman B.M., Shah J., Stubbs V., Long Q., Choby G., Rassekh C.H., Thaler E.R., Rajasekaran K. Snapshot Impact of COVID-19 on Mental Wellness in Nonphysician Otolaryngology Health Care Workers: A National Study. OTO Open. 2020;4 doi: 10.1177/2473974X20948835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sampaio F., Sequeira C., Teixeira L. Nurses’ mental health during the Covid-19 outbreak: a cross-sectional study. J. Occup. Environ. Med. 2020;62:783–787. doi: 10.1097/JOM.0000000000001987. [DOI] [PubMed] [Google Scholar]
- 66.Salopek-Žiha D., Hlavati M., Gvozdanović Z., Gašić M., Placento H., Jakić H., Klapan D., Šimić H. Differences in Distress and Coping with the COVID-19 Stressor in Nurses and Physicians. Psychiatr. Danub. 2020;32:287–293. doi: 10.24869/psyd.2020.287. [DOI] [PubMed] [Google Scholar]
- 67.Gorini A., Fiabane E., Sommaruga M., Barbieri S., Sottotetti F., La Rovere M.T., Tremoli E., Gabanelli P. Mental health and risk perception among Italian healthcare workers during the second month of the Covid-19 pandemic. Arch. Psychiatr. Nurs. 2020 doi: 10.1016/j.apnu.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang H., Shi Y., Jing P., Zhan P., Fang Y., Wang F. Posttraumatic stress disorder symptoms in healthcare workers after the peak of the COVID-19 outbreak: a survey of a large tertiary care hospital in Wuhan. Psychiatry Res. 2020;113541 doi: 10.1016/j.psychres.2020.113541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ruiz-Fernández M.D., Ramos-Pichardo J.D., Ibáñez-Masero O., Cabrera-Troya J., Carmona-Rega M.I., Ortega-Galán Á.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J. Clin. Nurs. 2020;29:4321–4330. doi: 10.1111/jocn.15469. [DOI] [PubMed] [Google Scholar]
- 70.Wang Y.-X., Guo H.-T., Du X.-W., Song W., Lu C., Hao W.-N. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore) 2020;99:e20965. doi: 10.1097/MD.0000000000020965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jiang M., Li S., She D., Yan F., Chung Y.F., Han L. The Psychological Effect of 2019 Coronavirus Disease Outbreak on Nurses Living in Islamic Culture Dominant Region, China. Res. Sq. 2020 doi: 10.21203/rs.3.rs-18075/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pan X., Xiao Y., Ren D., Xu Z., Zhang Q., Yang L., Liu F., Hao Y., Bai Y., Zhao F. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: A cross-sectional survey. Asia-Pac. Psychiatry. 2020:e12427. doi: 10.1111/appy.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ning X., Yu F., Huang Q., Li X., Luo Y., Huang Q., Chen C. The mental health of neurological doctors and nurses in Hunan Province, China, during the COVID-19 outbreak. Res. Sq. 2020 doi: 10.21203/rs.3.rs-22061/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hu D., Kong Y., Li W., Han Q., Zhang X., Zhu L.X., Wan S.W., Liu Z., Shen Q., Yang J. Frontline Nurses’ Burnout, Anxiety, Depression, and Fear Statuses and their Associated Factors during the COVID-19 Outbreak in Wuhan, China: A Big-Scale Cross-Sectional Study. Lancet. 2020 doi: 10.2139/ssrn.3566144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sahin T., Aslaner H., Eker O., Gokcek M., Dogan M. A Questionnaire Study Effect of COVID-19 Pandemic on Anxiety and Burnout Levels in Emergency Healthcare Workers. Int. J. Med. Sci. Clin. Invent. 2020;7:4991–5001. doi: 10.18535/ijmsci/v7i09.010. [DOI] [Google Scholar]
- 76.Kaveh M., Davari-tanha F., Varaei S., Shirali E., Shokouhi N., Nazemi P., Ghajarzadeh M., Feizabad E., Ashraf M.A. Anxiety levels among Iranian health care workers during the COVID-19 surge: A cross-sectional study. MedRxiv. 2020 doi: 10.1101/2020.05.02.20089045. 2020.05.02.20089045. [DOI] [Google Scholar]
- 77.Guixia L., Hui Z. A Study on Burnout of Nurses in the Period of COVID-19. Am. J. Appl. Psychol. 2020;9:31. doi: 10.11648/j.pbs.20200903.12. [DOI] [Google Scholar]
- 78.Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., AL-Hadithi H.T., Ali D., Abuthawabeh R., Abdelwahab G.M., Alhartani Y.J., Muhaisen H.A., Dagash A., Alyami H.S. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020 doi: 10.1002/brb3.1730. e01730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang S., Xie L., Xu Y., Yu S., Yao B., Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. 2020 doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J. Affect. Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Szepietowski J.C., Krajewski P., Biłynicki-Birula R., PoznaŃski P., Krajewska M., Rymaszewska J., Matusiak Ł. Mental health status of health care workers during the COVID-19 outbreak in Poland: one region, two different settings. Dermatol. Ther. 2020 doi: 10.1111/dth.13855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Que J., Shi L., Deng J., Liu J., Zhang L., Wu S., Gong Y., Huang W., Yuan K., Yan W., Sun Y., Ran M., Bao Y., Lu L. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koksal E., Dost B., Terzi Ö., Ustun Y.B., Özdin S., Bilgin S. Evaluation of depression and anxiety levels and related factors among operating theatre workers during the novel coronavirus (COVID-19) pandemic. J. Perianesth. Nurs. 2020 doi: 10.1016/j.jopan.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tu Z., He J., Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine (Baltimore) 2020;99:e20769. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhu J., Sun L., Zhang L., Wang H., Fan A., Yang B., Li W., Xiao S. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., Zhang J., Liu Z., Zhang B. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel coronavirus disease outbreak. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang S.X., Liu J., Afshar Jahanshahi A., Nawaser K., Yousefi A., Li J., Sun S. At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang W., Wang K., Yin L., Zhao W., Xue Q., Peng M., Min B., Tian Q., Leng H., Du J., Chang H., Yang Y., Li W., Shangguan F., Yan T., Dong H., Han Y., Wang Y., Cosci F., Wang H. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jia P.U., Guirong L.I., Lulu C.A.O., Yuanchen W.U., Linglin X.U. Investigation and analysis of the psychological status of the clinical nurses in a class A hospital facing the novel coronavirus pneumonia. Chongqing Med. 2020;49 doi: 10.3760/cma.j.issn.9999-998X.2020.0015. E015–E015. [DOI] [Google Scholar]
- 90.Pouralizadeh M., Bostani Z., Maroufizadeh S., Ghanbari A., Khoshbakht M., Alavi S.A., Ashrafi S. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: a web-based cross-sectional study. Int. J. Afr. Nurs. Sci. 2020;13:100233. doi: 10.1016/j.ijans.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gallopeni F., Bajraktari I., Selmani E., Tahirbegolli I.A., Sahiti G., Muastafa A., Bojaj G., Muharremi V.B., Tahirbegolli B. Anxiety and depressive symptoms among healthcare professionals during the Covid-19 pandemic in Kosovo: a cross sectional study. J. Psychosom. Res. 2020;137:110212. doi: 10.1016/j.jpsychores.2020.110212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li R., Chen Y., Lv J., Liu L., Zong S., Li H., Li H. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine (Baltimore) 2020;99 doi: 10.1097/MD.0000000000021413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Saricam M. COVID-19-related anxiety in nurses working on front lines in Turkey. Nurs. Midwifery Stud. 2020;9:178. doi: 10.4103/nms.nms_40_20. [DOI] [Google Scholar]
- 94.Hong S., Ai M., Xu X., Wang W., Chen J., Zhang Q., Wang L., Kuang L. Immediate psychological impact on nurses working at 42 government-designated hospitals during COVID-19 outbreak in China: a cross-sectional study. Nurs. Outlook. 2020 doi: 10.1016/j.outlook.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.AlAteeq D.A., Aljhani S., Althiyabi I., Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. J. Infect. Public Health. 2020;13:1432–1437. doi: 10.1016/j.jiph.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Khanal P., Devkota N., Dahal M., Paudel K., Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob. Health. 2020;16:1–12. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Aksoy Y.E., Koçak V. Psychological effects of nurses and midwives due to COVID-19 outbreak: the case of Turkey. Arch. Psychiatr. Nurs. 2020;34:427–433. doi: 10.1016/j.apnu.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Skoda E.-M., Teufel M., Stang A., Jöckel K.-H., Junne F., Weismüller B., Hetkamp M., Musche V., Kohler H., Dörrie N., Schweda A., Bäuerle A. Psychological burden of healthcare professionals in Germany during the acute phase of the COVID-19 pandemic: differences and similarities in the international context. J. Public Health. 2020 doi: 10.1093/pubmed/fdaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X., Yang L., Song J., Bai T., Hou X. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc. Psychiatry Psychiatr. Epidemiol. 2020:1–9. doi: 10.1007/s00127-020-01954-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lee M.C.C., Thampi S., Chan H.P., Khoo D., Chin B.Z.B., Foo D.P.X., Lua C.B., Lewin B., Jacob R. Psychological distress during the COVID-19 pandemic amongst anaesthesiologists and nurses. Br. J. Anaesth. 2020;125:e384–e386. doi: 10.1016/j.bja.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Azoulay E., Cariou A., Bruneel F., Demoule A., Kouatchet A., Reuter D., Souppart V., Combes A., Klouche K., Argaud L., Barbier F., Jourdain M., Reignier J., Papazian L., Guidet B., Géri G., Resche-Rigon M., Guisset O., Labbé V., Mégarbane B., Van Der Meersch G., Guitton C., Friedman D., Pochard F., Darmon M., Kentish-Barnes N., FAMIREA study group Symptoms of Anxiety, Depression and Peritraumatic Dissociation in Critical Care Clinicians Managing COVID-19 Patients: A Cross-Sectional Study. Am. J. Respir. Crit. Care Med. 2020 doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Xiong H., Yi S., Lin Y. The psychological status and self-efficacy of nurses during COVID-19 outbreak: a cross-sectional survey. J. Health Care Organ. Provis. Financ. 2020;57 doi: 10.1177/0046958020957114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Buselli R., Corsi M., Baldanzi S., Chiumiento M., Del Lupo E., Dell’Oste V., Bertelloni C.A., Massimetti G., Dell’Osso L., Cristaudo A., Carmassi C. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19) Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17176180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wasim T., Raana G.E., Bushra N., Riaz A. Effect of COVID-19 Pandemic on Mental Wellbeing of Healthcare Workers in Tertiary Care Hospital. Ann. King Edw. Med. Univ. 2020;26:140–144. [Google Scholar]
- 105.Zheng R., Zhou Y., Fu Y., Xiang Q., Cheng F., Chen H., Xu H., Fu L., Wu X., Feng M., Ye L., Tian Y., Deng R., Liu S., Jiang Y., Yu C., Li J. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: A cross-sectional study. Int. J. Nurs. Stud. 2020 doi: 10.1016/j.ijnurstu.2020.103809. 103809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Han L., Wong F.K.Y., She D.L.M., Li S.Y., Yang Y.F., Jiang M.Y., Ruan Y., Su Q., Ma Y., Chung L.Y.F. Anxiety and depression of nurses in a north West Province in China during the period of novel coronavirus pneumonia outbreak. J. Nurs. Scholarsh. 2020;52:564–573. doi: 10.1111/jnu.12590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhu J., Ying W., Zhang L., Peng G., Chen W., Anto E.O., Wang X., Lu N., Gao S., Wu G., Yan J., Ye J., Wu S., Yu C., Yue M., Huang X., Xu N., Ying P., Chen Y., Tan X., Wang W. Psychological symptoms in Chinese nurses may be associated with predisposition to chronic disease: a cross-sectional study of suboptimal health status. EPMA J. 2020 doi: 10.1007/s13167-020-00225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-Z., An F.-R., Xiang Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhou Y., Yang Y., Shi T., Song Y., Zhou Y., Zhang Z., Guo Y., Li X., Liu Y., Xu G., Cheung T., Xiang Y.-T., Tang Y. Prevalence and Demographic Correlates of Poor Sleep Quality Among Frontline Health Professionals in Liaoning Province, China During the COVID-19 Outbreak. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Xiaozheng L., Lijuan W., Jisheng Z. Investigation of sleep quality of 150 first-line medical staff responding to COVID-19. Int J Psychiatr Res. 2020;3:1–6. [Google Scholar]
- 111.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav. Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.The National Federation of Nurses of Italy Work and profession, the covid-19 front, you don't just die from the virus, fnopi. 2020. https://www.fnopi.it/2020/03/24/san-gerardo-infermiera-suicida/
- 113.Shi L., Lu Z.-A., Que J.-Y., Huang X.-L., Liu L., Ran M.-S., Gong Y.-M., Yuan K., Yan W., Sun Y.-K., Shi J., Bao Y.-P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open. 2020;3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen C.-S., Wu H.-Y., Yang P., Yen C.-F. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr. Serv. Wash. DC. 2005;56:76–79. doi: 10.1176/appi.ps.56.1.76. [DOI] [PubMed] [Google Scholar]
- 115.Tham K., Tan Y., Loh O., Tan W., Ong M., Tang H. Psychological morbidity among emergency department doctors and nurses after the SARS outbreak. Hong Kong J. Emerg. Med. 2005;12:215–223. doi: 10.1177/102490790501200404. [DOI] [PubMed] [Google Scholar]
- 116.Lancee W.J., Maunder R.G., Goldbloom D.S. Coauthors for the impact of SARS study, prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bai Y., Lin C.-C., Lin C.-Y., Chen J.-Y., Chue C.-M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004;55:1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 118.Ayanian J.Z. Mental health needs of health care workers providing frontline COVID-19 care. JAMA Health Forum. 2020;1:e200397. doi: 10.1001/jamahealthforum.2020.0397. [DOI] [PubMed] [Google Scholar]
- 119.Thombs B.D., Bonardi O., Rice D.B., Boruff J.T., Azar M., He C., Markham S., Sun Y., Wu Y., Krishnan A., Thombs-Vite I., Benedetti A. Curating evidence on mental health during COVID-19: a living systematic review. J. Psychosom. Res. 2020;133:110113. doi: 10.1016/j.jpsychores.2020.110113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.WHO Coronavirus disease (COVID-19) outbreak: rights,roles and responsibilities of health workers, including key considerations for occupational safety and health. 2020. https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-covid-19.pdf?sfvrsn=bcabd401_0
- 121.WHO Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A: Searching Terms.