Abstract
Objective
To describe the implementation of a virtual, multi-institutional educational collaboration involving over 50 general surgery residency programs during the COVID-19 pandemic that enabled enhanced learning for surgical residents despite social-distancing requirements.
Design
Description of Virginia Commonwealth University's virtual educational augmentation program and the development of a collaborative teaching network during the coronavirus pandemic.
Setting
This collaboration was initiated by Virginia Commonwealth University's Department of Surgery, Richmond, VA, and grew to include general surgery residency programs from across the nation.
Participants
General surgery residents and faculty from Departments of General Surgery were recruited locally via direct emails and nationally via the Association of Program Directors’ listserv and Twitter. In total, 52 institutions participated from every part of the country.
Results
A virtual, multi-institutional collaborative lecture series was initiated that grew to involve over 50 general surgery residency programs, allowing for daily didactics by experts in their fields during the initial surge of the COVID-19 pandemic, while maintaining social distancing and the provision of essential clinical care.
Conclusion
A multi-institutional collaboration enabled continued didactic education during the coronavirus pandemic, vastly broadening the expertise, scope and variety available to residents, while decreasing burden on faculty. We believe this can serve as a framework for future multi-institutional collaborations that extend beyond the COVID-19 era.
Key words: COVID-19, pandemic, surgical education, multi-institutional collaboration, social distancing, virtual curriculum
COMPETENCIES: Medical Knowledge, Interpersonal and Communication Skills, Systems-Based Practice, Professionalism
INTRODUCTION
In December 2019, a novel coronavirus emerged in Wuhan, China,1 that destabilized global health care systems. To date, the only effective means of slowing this virulent virus’ transmission has been strict adherence to social distancing measures2 , 3 and the use of personal protective equipment (PPE).4 , 5
On March 13, 2020, as COVID-19 cases increased in the United States, the American College of Surgeons, followed by numerous medical societies,6, 7, 8, 9 recommended that elective surgeries be postponed indefinitely to decrease strain on hospital infrastructure and preserve PPE.10 In response, general surgery residencies restructured resident schedules to minimize exposures, conserve PPE, and secure a healthy workforce for potential surges.
Subsequent decreases in operative caseloads, social distancing requirements, and state guidelines severely restricted traditional teaching methodologies such as intraoperative learning and in-person didactics. The COVID-19 crisis thus rapidly propelled interactive technology from a limited adjunct in surgical education to the mainstay of scholarship, as it enabled residents and faculty to connect despite physical separation. Residencies transitioned lectures, journal clubs, and conferences to virtual platforms, allowing broad participation while minimizing social interactions.11, 12, 13 Though programs acknowledged these virtual platforms could facilitate multi-institutional educational curricula,14, 15, 16 to our knowledge, nothing has been published that describes their actual development. Herein, we describe how Virginia Commonwealth University (VCU) harnessed technology to capitalize on the wealth of surgical expertise beyond their institution, creating a novel, multiprogram lecture series to benefit surgical residents nationally. Further, we advocate for the integration of such collaborations into surgical curricula during the COVID-19 era and beyond.
BUILDING A MULTI-INSTITUTIONAL COLLABORATION
In response to the cancellation of elective surgeries and the enactment of social distancing guidelines, VCU's in-person surgical didactics were cancelled indefinitely. The VCU education team quickly developed a remote teaching strategy centered around video-conferenced lectures highlighting evidence-based medicine.
However, limitations in VCU core faculty availability restricted lecture frequency and failed to capitalize on the increased time residents now had for education. VCU therefore sought to enhance their learning opportunities by developing a multi-institutional educational collaboration that established daily lectures for surgical residents across the country, known as The National Surgery Resident Lecture Series (NSRLS). Partnerships with geographically close residencies were initiated by email. Broader involvement was sought via the Association of Program Directors’ listserv and Twitter advertisements. Participation was voluntary, free and supplemental to each individual institution's didactics.
To develop the curriculum, a list of general surgery topics (Table 1 ), loosely based on content from the General Surgery Qualifying Exam, was provided to participating institutions. Faculty from these institutions then volunteered to present based on expertise and availability. Presentations were one hour and delivered via Zoom (Zoom Video Communications, Inc., San Jose, California, USA) to allow for interaction, recording and attendance tracking. Didactics were PowerPoint (Microsoft Corporation, Redmond, Washington, USA) based and combined lecture with interactive cases to foster resident engagement. Faculty used the Socratic method and/or polling to increase participation. Residents were encouraged to ask questions via the chat box which were either answered in real-time by a designated expert or posed to the presenter as appropriate. Additionally, each lecturer provided and discussed 2 prerequisite, recently published journal articles that changed clinical practice, allowing learners to critically analyze research methods and understand each study's role in shaping current surgical standards.
TABLE 1.
General Surgery Topics Sent to Participating Institutions To Recruit Expert Lecturers.
| Basic Science |
| Vascular |
| Colorectal |
| Endocrine |
| Thoracic |
| Trauma |
| Bariatric/Minimally invasive |
| Pediatric |
| Cardiac |
| Oncology |
| Acute Care Surgery |
| Transplant |
| Critical Care |
| Breast |
| Pancreas |
| Liver |
| Upper Alimentary Tract |
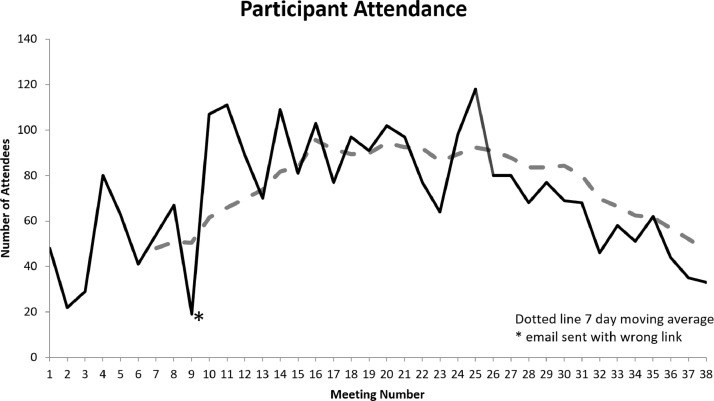
Immediate benefits of collaboration included offloading excessive burden of presentations from local faculty while enhancing resident education by cultivating diverse lectures from experts at each institution. Presentations were scheduled for noon ET to accommodate West Coast programs, allow adequate time for rounds, patient care, and administrative tasks for those in the hospital, and encourage participation from those at home. Lectures were recorded and housed in an online repository for later review. After initial deployment, the number of participants quickly increased with 80 to 100 devices logged on at any given time (many with multiple users) from over 50 surgical residency programs. As the Centers for Disease Control and Prevention (CDC) guidelines evolved17 and institutions resumed semi-elective cases, attendance decreased into the 40 to 60 range (Fig. 1 ). Additionally, increased operative caseloads depleted critical infrastructure from the NSRLS as the VCU residents and faculty who had built the program resumed fulltime clinical responsibilities. Availability of the multi-institutional faculty was similarly reduced. The program was therefore terminated in late May after a full 8-week schedule (38 lectures).
FIGURE 1.
Number of devices logged-in by meeting number (solid line). Seven-day average number of devices logged-in (broken line). Of note: On the day of meeting number 9, the incorrect Zoom code was emailed to participants.
DISCUSSION
The NSRLS is a multi-institutional collaborative effort that provided supplemental, CDC-compliant didactics to surgical residents during the beginning of the COVID-19 pandemic. Despite the decision to discontinue the program, we believe there is significant benefit to similar shared education models being adapted across the country. With over 50 participating surgery programs, the NSRLS allowed for high-quality lectures from experts in their fields to be delivered virtually, optimizing both time and resources. More importantly, it provided safe learning opportunities despite social distancing requirements and alleviated the burden felt by individual programs to augment didactic sessions to compensate for decreased case volumes.
Moreover, the benefits of NSRLS extend beyond the needs of the COVID-19 era. Such collaborations dismantle disparities between surgical programs by increasing access to expertise that might otherwise be concentrated at a single institution, standardizing education across programs, enabling networking, promoting sharing of ideas, and potentially leading to joint research projects.
Future areas of improvement for multi-institutional educational programs would include rigorous curriculum development focused on both Surgical Boards review and current best practices, the standardized use of interactive Zoom elements (polling, breakout rooms, the whiteboard, etc.) to increase resident engagement and would require a didactic schedule complimentary to busy surgical practices. This likely means limiting the presentation frequency to once or twice a week and maintaining a video repository, enabling residents to view lectures even if unable to attend in real-time. Further, the NSRLS was disbanded primarily due to time constraints and a lack of dedicated personnel and infrastructure to manage the program once elective surgeries resumed. However, the widespread participation in the NSRLS demonstrates that multi-institutional collaborations are not only feasible, but in-demand, and would likely be broadly integrated into surgical education if readily available. We therefore recommend that a national lecture series be implemented by a central body or surgical association that has the infrastructure to review lectures prior to delivery to ensure high quality, effective learning experiences that are standardized across all residency programs and we believe the NSRLS's success demonstrates the feasibility of such an undertaking.
This manuscript is limited by its purely descriptive nature which focuses on one collaborative experience. It is further limited by the fact that we did not seek evaluation of the program from individual residencies. Future research in this area should include other programs’ and specialties’ experiences. It should also methodically evaluate learner and lecturer perspectives to ensure educational needs are being met, to optimize engagement in virtual presentations, and to see if secondary benefits such as increased research collaborations arise from joint didactics.
CONCLUSION
At a time when traditional teaching methodologies were limited by social distancing and workflow changes, VCU capitalized on technology's ability to bring people together regardless of physical location. In creating a multi-institutional educational collaboration, VCU expanded the expertise available to each program while diversifying faculty participation. We believe this program should serve as a framework for future multi-institutional collaborations that extend beyond the COVID-19 era.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial or not-for profit sectors.
Declaration of Competing Interest
None.
REFERENCES
- 1.Zhu N, Zhang D, Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:1–4. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koo JR, Cook AR, Park M. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis. 2020;20:678–688. doi: 10.1016/S1473-3099(20)30162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mick P, Murphy R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review. J Otolaryngol Head Neck Surg. 2020;49 doi: 10.1186/s40463-020-00424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang LY, Wang J. Anesthesia and COVID-19: What we should know and what we should do. Semin Cardiothorac Vasc Anesth. 2020;24:127–137. doi: 10.1177/1089253220921590. [DOI] [PubMed] [Google Scholar]
- 6.Center for Medicare & Medicaid Services. CMS adult elective surgery and procedures recommendations: Limit all non-essential planned surgeries and procedures, including dental, until further notice. April 7, 2020. https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf. Accessed September 16, 2020.
- 7.Haft JW, Atluri P, Ailawadi G. Adult cardiac surgery during the COVID-19 pandemic: A tiered patient triage guidance statement. Ann Thorac Surg. 2020;110:697–700. doi: 10.1016/j.athoracsur.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Society of Surgical Oncology. Resource for management options of colorectal cancer during COVID-19. April 6, 2020. https://www.surgonc.org/wp-content/uploads/2020/04/Colorectal-Resource-during-COVID-19-4.6.20.pdf. Accessed September 16, 2020.
- 9.Guy DK, Bosco III JA, Savoie III FH. AAOS guidelines for elective surgery during the COVID-19 pandemic. April 2, 2020. https://www.aaos.org/about/covid-19-information-for-our-members/aaos-guidelines-for-elective-surgery/. Accessed September 15, 2020.
- 10.American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures. March 13, 2020. https://www.facs.org/-/media/files/covid19/recommendations_for_management_of_elective_surgical_procedures.ashx. Accessed September 16, 2020.
- 11.Dedeilia A, Sotiropoulos MG, Hanrahan JG. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34:1603–1611. doi: 10.21873/invivo.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabharwal S, Ficke JR, LaPorte DM. How we do it: modified residency programming and adoption of remote didactic curriculum during the COVID-19 pandemic. J Surg Educ. 2020;77:1033–1036. doi: 10.1016/j.jsurg.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chick RC, Clifton GT, Peace KM. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coe TM, Jogerst KM, Sell NM. Practical techniques to adapt surgical resident education to the COVID-19 era. Ann Surg. 2020;272:e139–e141. doi: 10.1097/SLA.0000000000003993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stambough JB, Curtin BM, Gililland JM. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35:S60–S64. doi: 10.1016/j.arth.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almarzooq ZI, Lopes M, Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in graduate medical education. J Am Coll Cardiol. 2020;75:2635–2638. doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic non-COVID-19 care framework. Updated June 30, 2020 https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Accessed September 15, 2020.