Abstract
Context
Hospice care focuses on improving the quality of end-of-life care and respecting patients’ preferences regarding end-of-life treatment. The impact of coronavirus disease 2019 (COVID-19) on the utilization of hospice services is unknown.
Objectives
To investigate the utilization of hospice care services before and during the COVID-19 pandemic.
Methods
All patients (n = 19,900) cared for at Taipei City Hospital from January 2019 to April 2020 were divided into three time points: January–April 2019 (before COVID-19), May–December 2019 (interim), and January–April 2020 (during COVID-19). This cohort study compared the monthly utilization of hospice services before and during the COVID-19 pandemic.
Results
There was no significant difference in hospice home visits (194 vs. 184; P = 0.686) and new enrollments (15 vs. 14; P = 0.743) to hospice home care before and during the pandemic. However, the bed occupancy rate in hospice units in the hospital was significantly reduced from 66.2% before the pandemic to 37.4% during the pandemic (P = 0.029), whereas that in nonhospice units had a nonsignificant decrease from 81.6% before the pandemic to 71.8% during the pandemic (P = 0.086). During the pandemic, the number of inpatient days was affected more severely in hospice units than in nonhospice units (−42.4% vs. −10.9%; P = 0.029).
Conclusions
This study suggests that hospice home care services were maintained during the COVID-19 pandemic, while the utilization of hospice inpatient care services reduced. Home care for hospice patients is an essential component of palliative care during a pandemic.
Key Words: COVID-19, pandemic, hospice care service, cohort study
Introduction
The highly contagious coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 resulted in a rapid global pandemic in 2020. In December 2019, cases of COVID-19 appeared in China. Subsequently, the disease spread, and on March 11, 2020, the World Health Organization declared COVID-19 a pandemic.1 By the end of May, over 5.7 million people worldwide were infected, with over 357,736 fatalities. The influence of pandemics caused by new virus types on medical usage rates has been widely discussed.2 , 3 However, related literature on hospice care is lacking.
Hospice and palliative care are the standard of care for patients with advanced diseases and are recommended for those with a limited life expectancy. In Taiwan, National Health Insurance covers hospice programs, including hospice inpatient units and home care services.4 Hospice care is now widely accepted in Taiwan.5
On January 21, 2020, Taiwan had its first local COVID-19 case. To prevent an outbreak, the Taiwan Centers for Disease Control implemented several strategies, including border control, case identification, and quarantine of suspected cases.6 By May 30, 442 laboratory-confirmed COVID-19 cases were reported to the Taiwan Centers for Disease Control; the associated deaths numbered seven.7
Despite the available information, it remains unknown whether the COVID-19 pandemic has had an impact on hospice service utilization. Therefore, we conducted a cohort study to investigate the utilization of hospice services before and during the pandemic by directly comparing services in January–April 2019 with those in January–April 2020, also examining the May–December 2019 period to explore the timing of changes over 2019. Finally, we examined differences in nonhospice hospital utilization during these time periods for comparison.
Methods
Data Sources
Taipei City Hospital (TCH), the largest health care organization in Northern Taiwan, launched a large-scale program to provide hospice inpatient and home care services in 2015.8, 9, 10 This cohort study examined patients admitted to TCH's Renai and Zhongxiao branches from January 2019 through April 2020. All identifiable patient information was encrypted. The study protocol was approved by the institutional review board (TCHIRB-10904009-E).
Study Design
The primary study goal was a before-and-during comparison of monthly utilization of inpatient and home hospice; the periods in consideration were January–April 2019 and 2020. Thus, we examined inpatient care for nonhospice patients during these same time periods. We also examined the trends of medical utilization in hospice and nonhospice units from January 2019 through April 2020 to explore the timing of changes.
Outcome Variable
January–April 2019 was defined as before pandemic and January–April 2020 as during the pandemic. Medical care service utilization included bed occupancy rates, before-and-after patient day differences by percentage, new enrollments in the hospice home care program, and number of hospice home visits. Bed occupancy rate was calculated as the number of occupied beds per day divided by the number of available beds multiplied by the number of days in a given period. Before-and-after patient day differences as percentage were assessed as ([patient days in a month in 2020] – [patient days in a month in 2019])/(patient days in a month in 2019). Inpatient demographic information included age, sex, length of stay, medical expenses, comorbidities, and death. Comorbidities included cancer, diabetes, chronic obstructive pulmonary diseases, coronary heart disease, congestive heart failure, chronic kidney disease, and dementia.
Statistical Analysis
A two-sample t-test was conducted to compare age, length of stay, and medical expenses in hospitalized patients before and during the pandemic. Categorical data were analyzed with Pearson's χ2 or Fisher's exact test where appropriate. Wilcoxon rank sum test was conducted to analyze the difference in bed occupancy rates, hospice home care visits, and new enrollments in the hospice home care program before and during the pandemic. Statistical significance was set at 5%, and all analyses were conducted using SAS (version 9.4; SAS Institute, Inc., Cary, NC).
Results
Participants
This study included 19,900 patients hospitalized at TCH from January 2019 through April 2020: 7633 (36.6%) in January–April 2019 and 5933 (28.5%) in January–April 2020. The overall mean (standard deviation) age was 61.4 (20.3) years, and 50.9% of the participants were male (Table 1 ).
Table 1.
Baseline Characteristics of Study Subjects
| Variable | Total, N = 19,900 (%) | Before Pandemic, (January–April 2019) n = 7633 (%) | During Pandemic, (January–April 2020) n = 5933 (%) |
|---|---|---|---|
| Age, years | |||
| Mean ± SD | 58.3 ± 24.6 | 61.2 ± 23.2 | 60.8 ± 22.9 |
| <65 | 10,683 (53.7) | 3826 (50.1) | 2992 (50.4) |
| ≥65 | 9217 (46.3) | 3807 (49.9) | 2941 (49.6) |
| Sex | |||
| Female | 9776 (49.1) | 3836 (50.3) | 2840 (47.9) |
| Male | 10,124 (50.9) | 3797 (49.7) | 3093 (52.1) |
Hospice Home Care Visits and New Enrollments in Hospice Home Care Before and During the Pandemic
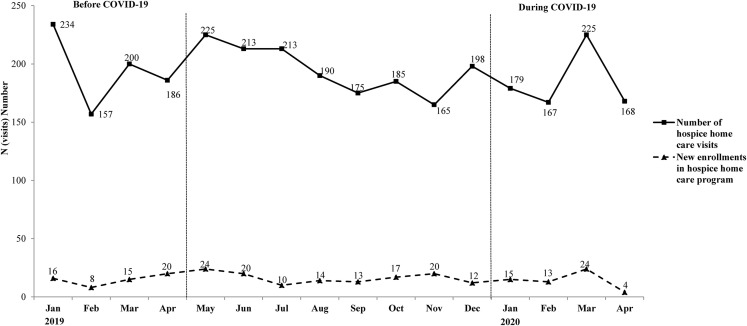
The mean monthly hospice home care visits were 194 and 184 before and during the pandemic, respectively. Moreover, the mean monthly new enrollments in the hospice home care program were 15 and 14 before and during the pandemic, respectively. There was no significant change in the trend of hospice home care visits and new enrollments in the hospice home care program before and during the pandemic (Fig. 1 ).
Fig. 1.
Trends of hospice home care visits and new enrollments in the hospice home care program before and during COVID-19 pandemic. COVID-19 = coronavirus disease 2019.
Characteristics of Inpatient Hospice and Nonhospice Before and During the Pandemic
There was no significant difference in age and sex among the patients admitted to inpatient hospice units before and during the pandemic. However, as compared with patients admitted to nonhospice units before the pandemic, those admitted during the pandemic were younger and more likely to be male (Table 2 ). They also had a shorter length of stay (7.5 vs. 8.9 days; P < 0.001) and a trend toward lower medical expenses (2506 vs. 2627; P = 0.059) (Table 2).
Table 2.
Characteristics of Inpatient Hospice and Nonhospice Before (January–April 2019) and During COVID-19 Pandemic (January–April 2020)
| Characteristics | Nonhospice Units |
Hospice Units |
||||
|---|---|---|---|---|---|---|
| No. (%) of Subjectsa |
P | No. (%) of Subjectsa |
P | |||
| Before Pandemic, n = 7482 (%) | During Pandemic, n = 5878 (%) | Before Pandemic, n = 151 (%) | During Pandemic, n = 55 (%) | |||
| Demographics | ||||||
| Age, years | ||||||
| Mean ± SD | 60.8 ± 23.1 | 60.6 ± 22.9 | 0.529 | 80.0 ± 13.5 | 79.8 ± 11.4 | 0.912 |
| <65 | 3799 (50.8) | 2988 (50.8) | 0.947 | 27 (17.9) | 4 (7.3) | 0.060 |
| ≥65 | 3683 (49.2) | 2890 (49.2) | 124 (82.1) | 51 (92.7) | ||
| Sex | ||||||
| Female | 3763 (50.3) | 2814 (47.9) | 0.006 | 73 (48.3) | 26 (47.3) | 0.892 |
| Male | 3719 (49.7) | 3064 (52.1) | 78 (51.7) | 29 (52.7) | ||
| Comorbidity | ||||||
| Cancer | 2206 (29.5) | 1959 (33.3) | <0.001 | 98 (64.9) | 39 (70.9) | 0.419 |
| Diabetes | 1080 (14.4) | 792 (13.5) | 0.112 | 19 (12.6) | 6 (10.9) | 0.745 |
| COPD | 139 (1.9) | 114 (1.9) | 0.731 | 4 (2.6) | 2 (3.6) | 0.313 |
| Coronary heart disease | 408 (5.5) | 338 (5.8) | 0.458 | 7 (4.6) | 3 (5.5) | 0.266 |
| Congestive heart failure | 260 (3.5) | 215 (3.7) | 0.571 | 12 (7.9) | 3 (5.5) | 0.212 |
| Chronic kidney disease | 389 (5.2) | 282 (4.8) | 0.291 | 11 (7.3) | 4 (7.3) | 0.236 |
| Dementia | 100 (1.3) | 66 (1.1) | 0.268 | 6 (4.0) | 2 (3.6) | 0.315 |
| Outcomes | ||||||
| Length of stays ± SD | 8.9 ± 15.3 | 7.5 ± 8.96 | <0.001 | 17.1 ± 14.8 | 15.8 ± 14.5 | 0.571 |
| Medical expensesb ± SD | 2627 ± 4399 | 2506 ± 2979 | 0.059 | 2996 ± 3377 | 2739 ± 3808 | 0.641 |
| Death | 269 (3.6) | 218 (3.7) | 0.728 | 114 (75.5) | 55 (72.7) | 0.686 |
COVID-19 = coronavirus disease 2019; COPD = chronic obstructive pulmonary disease.
Unless stated otherwise.
Medical expenses are presented in US dollars. (US dollars: NT dollars = 1: 30.19).
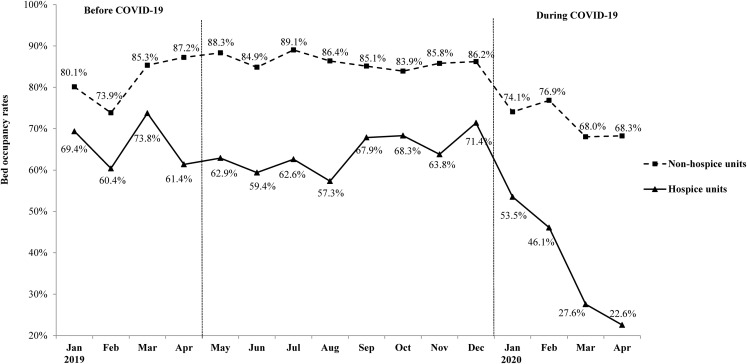
Bed Occupancy Rates in Hospice and Nonhospice Units Before and During the Pandemic
Fig. 2 shows the bed occupancy rates in hospice and nonhospice units before and during the pandemic. In 2019, the average bed occupancy rate in nonhospice units was over 80%, whereas that in hospice units was over 60%. During the pandemic, the bed occupancy rate in nonhospice units showed a nonsignificant decrease to 68% (P = 0.054), whereas that in hospice units was significantly reduced from 71.4% in December 2019 to 22.6% in April 2020 (P = 0.005) (Fig. 2).
Fig. 2.
Trends of bed occupancy rates in hospice and nonhospice units before and during the COVID-19 pandemic. COVID-19 = coronavirus disease 2019.
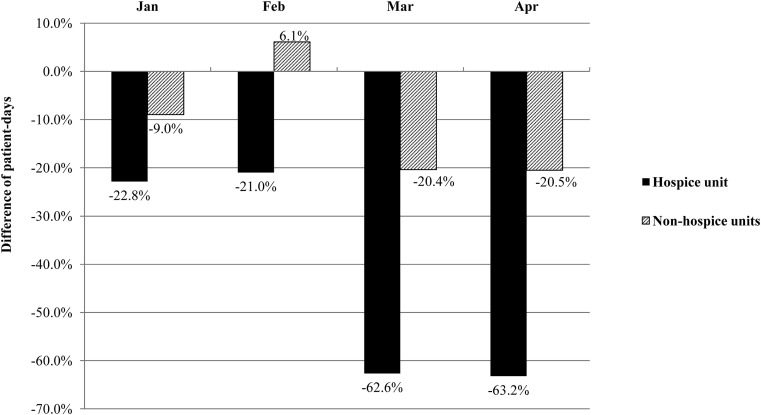
Patient Days in Hospice and Nonhospice Units Before and During the Pandemic
Fig. 3 shows the differences in patient days in hospice and nonhospice units before and during the pandemic. As compared with the before-pandemic number, the number of patient days in hospice units significantly decreased by 21.0% to 63.2%, whereas that in nonhospice units significantly decreased less dramatically by 9.0% to 20.5% during the pandemic.
Fig. 3.
Differences in monthly patient days in hospice and nonhospice units before (January–April 2019) and during (January–April 2020) the COVID-19 pandemic. COVID-19 = coronavirus disease 2019.
Discussion
There was no significant change in hospice home care visits and new enrollments in the hospice home care program before and during the COVID-19 pandemic. However, the bed occupancy rate for inpatient hospice units was significantly reduced from 71.4% in December 2019 to 22.6% in April 2020. As compared with before the pandemic, the number of patient days for inpatient hospice units significantly decreased during the pandemic. We are not aware of other studies that have examined the effect of the COVID-19 pandemic on inpatient or home hospice utilization.
Although hospice care has been promoted in Taiwan for years, our study suggests that inpatient hospice services in hospitals have been significantly affected by the COVID-19 pandemic, more dramatically than nonhospice units. However, in our setting, hospice home care was not reduced and enabled patients near the end of their lives to continue to receive services and be with their families. Thus, hospice home care provides an important service in situations such as the COVID-19 pandemic. Given that the absence of high-quality end-of-life care is a grievous humanitarian problem, home hospice care should be a key focus during pandemics.3
During the current pandemic, people worldwide have died in quarantine, where their families could not comfort them at their deathbeds.11 This represents an enormous challenge for the development of palliative and hospice care. It is imperative for governments and health-care systems to strike a balance between infection control and humanitarian issues.
In the experience from severe acute respiratory syndrome, 56.3% of infected cases were related to nosocomial infection.12 Although this proportion seems lower in the current situation, a key aspect for controlling the COVID-19 pandemic is promoting the reduction of elective hospitalizations and family visits. Hospitals worldwide have implemented infection control measures at their entrances. During the peak of the pandemic in Taiwan (April 2020), inpatient hospice bed occupancy was reduced by over 60% compared with the previous year, which may be related to these visitation restrictions. This reduction may also be due in part to fear of contagion. Further studies are needed to understand the psychological effects of pandemics on palliative and hospice care.
An important limitation of this study is that it was restricted to a single hospital system in a single city, limiting the generalizability of the findings to other areas. It will be important to explore these issues in other cities and countries over time.
Conclusion
Hospice home care services were maintained during the COVID-19 pandemic while the utilization of hospice inpatient care services was dramatically reduced. As the COVID-19 pandemic continues to influence the ability of family members to visit loved ones in the hospital, hospice care will need to dynamically adjust its service capacity, identifying and meeting hospice and palliative care needs in nonhospice units, strengthening the promotion of hospice home care and telehealth palliative care models for people in home isolation or trapped abroad who cannot attend to family members, thereby providing continuous high-quality palliative care.
Disclosures and Acknowledgments
The authors disclose no conflict of interest in the writing of this article.
This study was funded by the Ministry of Science and Technology, Taiwan, (MOST108–2635-B-532–001) and by a grant from the Department of Health, Taipei City Government, Taiwan. The authors thank Shu-Yi Lin, Feng-Shiang Cheng, and Shih-Han Weng for research assistance and statistics consultation.
Footnotes
Hsiao-Yun Hu and Yung-Feng Yen contributed equally to this work.
References
- 1.World Health Organization WHO announces COVID-19 outbreak a pandemic. 2020. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic Available from.
- 2.Chang H.J., Huang N., Lee C.H. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94:562–564. doi: 10.2105/ajph.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen T.J., Lin M.H., Chou L.F., Hwang S.J. Hospice utilization during the SARS outbreak in Taiwan. BMC Health Serv Res. 2006;6:94. doi: 10.1186/1472-6963-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shih T.C., Chang H.T., Lin M.H. Trends of do-not-resuscitate orders, hospice care utilization, and late referral to hospice care among cancer decedents in a tertiary hospital in Taiwan between 2008 and 2014: a hospital-based observational study. J Palliat Med. 2017;20:838–844. doi: 10.1089/jpm.2016.0362. [DOI] [PubMed] [Google Scholar]
- 5.Chen P.J., Liang F.W., Ho C.H. Association between palliative care and life-sustaining treatments for patients with dementia: a nationwide 5-year cohort study. Palliat Med. 2018;32:622–630. doi: 10.1177/0269216317751334. [DOI] [PubMed] [Google Scholar]
- 6.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 7.Taiwan Centers for Disease Control and Prevention Surveillance of COVID-19. 2020. https://www.cdc.gov.tw/En Available from.
- 8.Huang S.J., Huang C.Y., Woung L.C. The 2018 Taipei declaration for ultimate integration of palliative care. J Palliat Med. 2019;22:476–477. doi: 10.1089/jpm.2019.0055. [DOI] [PubMed] [Google Scholar]
- 9.Yen Y.F., Huang L.Y., Hu H.Y. Association of advance directives completion with the utilization of life-sustaining treatments during the end-of-life care in older patients. J Pain Symptom Manage. 2018;55:265–271. doi: 10.1016/j.jpainsymman.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Yen Y.F., Lee Y.L., Hu H.Y. An interventional study for the early identification of patients with palliative care needs and the promotion of advance care planning and advance directives. J Pain Symptom Manage. 2020;59:974–982. doi: 10.1016/j.jpainsymman.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Pahuja M., Wojcikewych D. Systems barriers to assessment and treatment of COVID-19 positive patients at the end of life. J Palliat Med. 2020 doi: 10.1089/jpm.2020.0190. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Chen K.T., Twu S.J., Chang H.L. SARS in Taiwan: an overview and lessons learned. Int J Infect Dis. 2005;9:77–85. doi: 10.1016/j.ijid.2004.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]