Abstract
Self-medication impacts both negatively and positively the health of people, which has become evident during the COVID-19 pandemic. The study aimed to assess the prevalence of self-medicated drugs used for respiratory symptoms, as COVID-19 preventive, for its symptoms or once tested positive. To determine the perception of symptom relief and demographic variables that promote self-medication in Peru. We performed a cross-sectional, analytical, multicenter study in 3792 study respondents on the use, the reason for use, and perception of relief after the use of six drugs during the quarantine period. An online questionnaire was developed, pretested and submitted to the general public. Multivariable logistic regression was used to ascertain factors that influence an individual’s desire to self-medicate, associations were considered significant at p < 0.05 and using region (coast, mountain and jungle) as cluster group. The majority of respondents self-medicated with acetaminophen for respiratory symptoms and mainly because they had a cold or flu. It was observed that all the surveyed drugs (acetaminophen, ibuprofen, azithromycin, penicillin, antiretrovirals and hydroxychloroquine) were consumed for various symptoms including: fever, fatigue, cough, sneezing, muscle pain, nasal congestion, sore throat, headache and breathing difficulty. Over 90% of respondents perceived relief of at least one symptom. Multivariable logistic regression showed that older people have a higher frequency of antiretroviral self-medication, respondents who currently have a job had a higher frequency of penicillin self-medication, and that respondents from the Andes consumed less acetaminophen, while the ones from the rainforest consumed it more. There were significant percentages of self-medication, including drugs without sufficient scientific evidence. Age, region where one lived and job status were variables associated with self-medication frequency. Continuous awareness and sensitization about the risks of self-medication are warranted.
Keywords: Self-medication, Prevalence, Drug use, SARS-CoV-2, COVID-19, Peru
1. Introduction
The COVID-19 pandemic has triggered a general lock-down in most of the world, leaving the general sense that the only resource that people has is to self-help, self-care and self-medicate (Matias et al., 2020). The latter gets worsened with the infodemic of fake news that accompanied the COVID-19 pandemic (Tasnim et al., 2020, Alvarez-Risco et al., 2020), and the vast exposure in the news related to any study (in vitro, pre-clinical or clinical) that sheds light into a possible preventive or treatment option (Mallhi et al., 2020). This has resulted in the self-medication of various prescription drugs that have no confirmed clinical efficacy against SARS-CoV-2 (Mallhi et al., 2020). Some of them include the anti-malaria drug hydroxychloroquine (Hasan et al., 2020), the antibiotic azithromycin (Molina et al., 2020), the non-steroidal anti-inflammatory drug (NSAID) ibuprofen (Sodhi et al., 2020) and the antiretrovirals lopinavir and ritonavir (Lim et al., 2020). Because of the lack of monitoring, these drugs could cause a shortage of these drugs for patients that need them for approved conditions (Jaffe, 2020), a direct impact in the price of these drugs (Busari et al., 2020), and jeopardize peoples’ health due to their known adverse events (Mallhi et al., 2020, Rojas et al., 2020).
Peru is among the top 5 countries in the world in reported COVID-19 cases, and second in Latin America, only after Brazil (Dong et al., 2020a). On September 20, 2020 Peru reported 768,895 COVID-19 cases with a 4.08% lethality rate (MINSA, 2020d). As Peru becomes a new epicenter of the pandemic in Latin America multiple publications have illustrated its fragmented healthcare system, which has not been the most effective during the COVID-19 pandemic resulting in a high number of physicians’ deaths (Gonzales-Tamayo et al., 2020b) and detrimental effects in the mental status of healthcare workers (Yáñez et al., 2020e). Furthermore, Peru has reported discrepancies in the official reports of COVID-19 deaths nationwide (Yáñez et al., 2020c), poor execution of SARS-CoV-2 testing and reporting (Yáñez et al., 2020b), and an increase number of COVID-19 cases in children and adolescents (Yáñez et al., 2020a, Yáñez et al., 2020d). The Ministry of Health in Peru was prompt in publishing COVID-19 symptomatic pharmacological treatment options to try to control de pandemic (MINSA, 2020c). This included the use in the clinical setting of hydroxychloroquine and ivermectin for mild COVID-19 cases; and hydroxychloroquine plus azithromycin and/or chloroquine phosphate plus ivermectin for moderate and severe COVID-19 cases (MINSA., 2020c, Rojas et al., 2020). It comes as no surprise that self-medication has become common in Peru as panic became generalized among the general public who is anxiously waiting for any positive news regarding the prevention and treatment of this viral infection. This becomes aggravated since Peru occupies the fifth place in the world for COVID-19 confirmed cases (Dong et al., 2020a), and it currently is the country with the highest mortality rate (MenaFN, 2020).
This self-medication trend has been reported to have increased worldwide based in the number of Google searches since the pandemic started (Onchonga, 2020). This global trend has caused a tremendous medical challenge (Hughes et al., 2001, Mandal, 2015) because the various prescription drugs currently approved for COVID-19 symptoms carry adverse drug reactions (Onchonga et al., 2020). Furthermore, there is high risk of incorrect dosage, improper route of administration, longer use than intended, improper storage, risk of dependency to abuse, and increased prevalence of pathogenic resistance to drugs (Onchonga et al., 2020, Menary et al., 2011). Even though, self-medication intention is common worldwide it has only been reported in South Arabia (Mansuri et al., 2020) and Kenya (Onchonga et al., 2020). However, these studies assessed the prevalence of self-medication but did not surveyed what drugs where actually consumed. In this way, we designed this cross-sectional study to investigate the pattern of self-medication among the general public in Peru during the COVID-19 pandemic. The objectives of this study were to assess the prevalence of self-medicated drugs used for respiratory symptoms, as COVID-19 preventive, for its symptoms or once tested positive. To determine the perception of symptom relief and if there are any demographic variables that promote self-medication in Peru. The results would inform healthcare policy makers on the measures to improve in Peru as they strive to save lives.
2. Methods
2.1. Study design
We conducted an online cross-sectional multicenter survey, which was initially evaluated by experts from different provinces of Peru based on the Delphi method (Varela-Ruiz et al., 2012). After including the experts’ observations, a pilot study was performed (from May 25 to June 3) with 480 respondents in all the 25 provinces of Peru. The pilot data was used to calculate the minimum sample size necessary for the actual study. It was determined that a minimum sample size of 3,138 was necessary to achieve a minimum percentage difference of 2.5% (49.0% versus 51.5%), a statistical power of 80%, and a confidence level of 95% (data not shown). The sample size was calculated using power analysis (Walker et al., 2017).
The actual survey consisted of an online questionnaire in Google surveys that was sent via WhatsApp, Messenger, and Facebook, and it was configured to submit an email at the end of the survey so that investigation group can eliminate duplicate answers. The shared questionnaire was made anonymous ensuring data confidentiality and reliability. This survey was shared in Spanish, as this is the official language in Peru. The survey was performed from June 5 to 17 after approximately 3 months of lockdown and social distancing measures in Peru due to the COVID-19 outbreak. At the beginning of the survey (June 5) the number of COVID-19 confirmed cases was 187,400 and 5,162 deaths (MINSA, 2020a), while at the end of the survey (June 17) the confirmed cases increased to 240,908 and the deaths increased to 7,257 (MINSA, 2020b). We surveyed general public who were adults (over 18 years old) in the 25 Peruvian provinces. Participants were recruited through the COVID-19-GIS-Peru network. Grupo de Investigación en Salud (GIS) stands for Health Research Group, a network of investigators that include physicians, health professionals and students performing COVID-19 social epidemiological studies in Peru and Latinamerica (Mejia et al., 2020a, Mejia et al., 2020b, Mejia et al., 2020c, Mejia et al., 2020d, Mejia et al., 2020e, Araujo-Banchon et al., 2020, Yáñez et al., 2020c).
2.2. Outcomes and covariates
The survey (Annex 1) included 11 questions, 7 were demographic questions and 4 questions related to self-medication of drugs to prevent and treat respiratory symptoms: drug selection, reasoning for self-medication, symptoms they were looking to improve, and if any of the drugs improved those symptoms. The demographic questions included city where they live, gender, age, marital status, education level, job status, and type of job.
The respondents were asked to indicate if during the COVID-19 lockdown they consumed any of the following drugs: acetaminophen, ibuprofen, azithromycin, hydroxychloroquine, penicillin, antiretrovirals (lopinavir, ritonavir, remdesivir, and others), or any other drug (open question) for respiratory symptoms. The selection of drugs was based on the COVID-19 symptom treatment options approved in Peru at the time (MINSA, 2020c) and based on the drugs reported by the media to be viable treatment options. The respondents were asked to select the reason to use of these drugs from a 7-item list that included: had a cold/flu, no symptoms, COVID-19 prevention, had COVID-19 symptoms, COVID-19 positive, consume the drug regularly, other reason (open question).
The respondents were then presented with an 11-item list that included the most common COVID-19 symptoms reported by the Center of Disease Control and Prevention (CDC) (CDC, 2020). The respondents were asked to select the symptom(s) why they consumed any of the drug(s) indicated on the previous question. The symptoms included fever, fatigue, cough, muscle ache, nasal congestion, sore throat, headache, breathing difficulty. Sneezing was included since it is a usual cold or flu symptom that often gets confused with a COVID-19 symptom. No symptom and other symptom (open question) was also included. Loss of taste or smell, nausea/vomiting and diarrhea were not included. Loss of smell (anosmia) was still debated as a COVID-19 symptom at the time of the preparation of the survey. Even though anosmia was reported in some COVID-19 patients as early as April, it is until June 2020 when concrete scientific reports and reviews were published (Meng et al., 2020).
Finally, the respondents were asked to indicate any symptom improvement after drug intake using the 5-item Likert scale with the following options: improved all symptoms, improved most of the symptoms, improved a few of the symptoms, improved only one symptom, did not alleviate any of the symptoms.
2.3. Statistical analysis
Data analysis was done in STATA version 14 (Stata Corp) with a significance level set at p < 0.05. The instrument consistency was assessed using the Kuder–Richardson Formula 20 (KR-20) (Tschannen et al., 2020) for the dichotomous variable of either using (or not) any of the assessed drugs during the lockdown in Peru. The instrument validity was assessed with the known-groups validity approach by fitting multivariate analysis (Jones et al., 2018) to estimate the preference of self-medication for the surveyed drugs using sex, age, marital status, job status, educational status, and region as control variables. Univariate statistics was performed using frequencies and percentages for categorical variables. For analytical statistics, adjusted prevalence ratios (aPR) and 95% confidence intervals (CI) were obtained using generalized linear models (GLM), with Poisson family, log-link function, robust models and using region (coast, mountain and jungle) as cluster group.
Peru gets divided into three geographic regions because the Andes Mountains, these regions are the Coast (Costa), the Peruvian Andes (Sierra), and the Jungle (Selva) (WHO, 2013). This geographical division is accompanied with marked differences in access, roads, urbanization, population distribution, health and education services. This results in marked differences in health conditions with the coast, Andes and rainforest having the under-5 mortality rate at 26%, 39% and 42%, respectively (WHO, 2013). This is in part due to different behaviors toward urgency for medical treatment and the prevalence of pharmacological use. In order to assess differences in our study we used region as a cluster group.
2.4. Ethical approval
The survey was approved by the Universidad Privada Antenor Orrego ethics committee (#0209–2020-UPAO). The participants remained anonymous and had the option to finish the survey at any time, and their information was kept confidential. All the survey participants were well-versed on the study intentions and were required to consent before the enrollment. The participants were not involved in any of the planning, execution and reporting stages of the study.
3. Results
3.1. Sociodemographic characteristics of the respondents
The survey was sent to 6,000 people in the 25 provinces of Peru in order to achieve the minimum sample size of 3,138 calculated based on power analysis. Out of the 6,000 surveys sent online, we received 3,792 responses indicating a 63.2% response rate. Most participants were female (2066 [54.5%]), aged 18 to 85 years, single (3046 [80.3%]), had a bachelor degree or higher (2850 [75.2%]), had a job (1219 [32.1%]) and the predominant job industry was healthcare (315 [25.8%]) as shown in Table 1. The obtained KR-20 values for the dichotomous variable of either using (or not) any of the assessed drugs during the lockdown in Peru was > 0.7.
Table 1.
Socio-demographic characteristics of respondents during the COVID-19 lockdown in Peru.
| Socio-demographic variable | N (%) |
|---|---|
| Gender | |
| Male | 1726 (45.5) |
| Female | 2066 (54.5) |
| Age (years)a | 23 (20–29) |
| Marital status | |
| Single | 3046 (80.3) |
| Married | 498 (13.1) |
| In a domestic partnership | 188 (5.0) |
| Divorced | 39 (1.0) |
| Widowed | 21 (0.6) |
| Education level | |
| No studies | 3 (0.1) |
| Primary school | 7 (0.2) |
| Highschool | 566 (14.9) |
| Associate | 366 (9.6) |
| Bachelor | 2626 (69.3) |
| Postgraduate | 224 (5.9) |
| Work industry | |
| Food | 69 (5.7) |
| Commerce | 124 (10.2) |
| Construction | 64 (5.3) |
| Education | 214 (17.6) |
| Housekeeper | 19 (1.6) |
| Entertainment | 13 (1.1) |
| Police/Armed forces | 78 (6.4) |
| Healthcare | 315 (25.8) |
| Transportation | 22 (1.8) |
| Tourism | 11 (0.9) |
| Telecommunications | 45 (3.7) |
| Other | 245 (20.2) |
Median and interquartile range.
3.2. Non COVID-19 related reasons for self-medication
As shown on Table 2, the majority of respondents did not self-medicate (2526 [66.6%]) with any of the surveyed drugs (acetaminophen, ibuprofen, azithromycin, hydroxychloroquine, penicillin or azithromycin). Out of the 3792 respondents, it was observed that 1023 respondents reported that they consumed acetaminophen during lockdown, while 281 consumed ibuprofen, 182 azithromycin, 87 penicillin, 60 antiretrovirals and 28 hydroxychloroquine. For all the drugs the main reason for consumption was because the person reported they had a cold or flu. It was observed that a portion of respondents self-medicated because other reasons. For instance, 178 and 75 respondents consumed acetaminophen and ibuprofen, respectively for other reasons, which could be attributed to their broad use as pain relievers and antipyretics. Similarly, for the antibiotics azithromycin and penicillin it was reported that 16 and 28 people, respectively consumed them for other reasons. To a lower extent it was reported that 2 people used the anti-malarial drug hydroxychloroquine for other reasons. We also surveyed if these drugs were consumed regularly, and it was observed that 76 people consumed acetaminophen, 26 ibuprofen, 15 azithromycin, 6 penicillin, 5 antiretrovirals and 3 hydroxychloroquine. Even more concerning, was to observe that people in Peru consumed these drugs without any symptom. For instance, 17 consumed acetaminophen, 7 ibuprofen, 3 azithromycin, 2 hydroxychloroquine, 1 penicillin and another one antiretrovirals. It needs to be acknowledged that the same respondent could have used more than one drug at the same time.
Table 2.
Self-medication, reason and respiratory symptom improvement with various drugs during the COVID-19 lockdown in Peru.
| Variables | Acetaminophen | Ibuprofen | Azithromycin | Hydroxychloroquine | Penicillin | Antiretrovirals |
|---|---|---|---|---|---|---|
| Use during lockdown | ||||||
| Yes | 1023 (27.0%) | 282 (7.4%) | 182 (4.8%) | 28 (0.7%) | 87 (2.3%) | 60 (1.6%) |
| No | 2769 (73.0%) | 3510 (92.6%) | 3610 (95.2%) | 3764 (99.3%) | 3705 (97.7%) | 3732 (98.4%) |
| Reason | ||||||
| Cold or flu | 675 (66.0%) | 162 (57.6%) | 98 (53.9%) | 14 (50.0%) | 60 (68.9%) | 41 (68.3%) |
| No symptoms | 17 (1.7%) | 7 (2.5%) | 3 (1.7%) | 2 (7.2%) | 1 (1.2%) | 1 (1.7%) |
| COVID-19 preventive | 6 (0.6%) | 1 (0.4%) | 7 (3.9%) | 3 (10.7%) | 2 (2.3%) | 4 (6.7%) |
| COVID-19 symptoms | 65 (5.4%) | 9 (3.2%) | 23 (12.6%) | 1 (3.6%) | 1 (1.2%) | 3 (5.0%) |
| COVID-19 positive | 6 (0.6%) | 1 (0.4%) | 8 (4.4%) | 3 (10.7%) | 1 (1.2%) | 1 (1.7%) |
| Consume it regularly | 76 (7.4%) | 26 (9.2%) | 15 (8.2%) | 3 (10.7%) | 6 (6.9%) | 5 (8.3%) |
| Other reason | 178 (17.3%) | 75 (26.7%) | 28 (15.4%) | 2 (7.1%) | 16 (18.3%) | 5 (8.3%) |
| Symptom improvement | ||||||
| All symptoms improved | 482 (47.1%) | 136 (48.4%) | 79 (43.4%) | 12 (42.9%) | 41 (47.1%) | 36 (60.0%) |
| Many symptoms improved | 287 (28.0%) | 66 (23.5%) | 56 (30.8%) | 7 (25.0%) | 30 (34.5%) | 18 (30.0%) |
| Some symptoms improved | 96 (9.4%) | 34 (12.1%) | 27 (14.8%) | 6 (21.4%) | 6 (6.9%) | 5 (8.3%) |
| One symptom improved | 135 (13.2%) | 34 (12.1%) | 11 (6.0%) | 1 (3.6%) | 7 (8.0%) | 0 (0.0%) |
| No improvement | 23 (2.3%) | 11 (3.9%) | 9 (5.0%) | 2 (7.1%) | 3 (3.5%) | 1 (1.7%) |
3.3. COVID-19 related reasons for self-medication
On our survey we included three reasons for drug use related to COVID-19: as a preventive, presence of symptoms, and confirmed case. When these three reasons were combined it was observed that the drug with the highest self-medication was acetaminophen with 77 respondents, azithromycin (38), ibuprofen (11), antiretrovirals (8), hydroxychloroquine (7) and penicillin (4). It was observed that as a COVID-19 preventive, 7 respondents self-medicated with azithromycin, 6 with acetaminophen, 4 with antiretrovirals, 3 with hydroxychloroquine, 2 with penicillin and 1 with ibuprofen. When COVID-19 symptoms were present, the trend changed with acetaminophen been the drug with the highest self-medication (65), followed by azithromycin (23), ibuprofen (9), antiretrovirals (3), hydroxychloroquine (1) and penicillin (1). We also surveyed the self-medication use when diagnosed as COVID-19 positive and it was observed that 8 people used azithromycin, 6 acetaminophen, 3 hydroxychloroquine, and 1 person for ibuprofen, penicillin and antiretrovirals (Table 2).
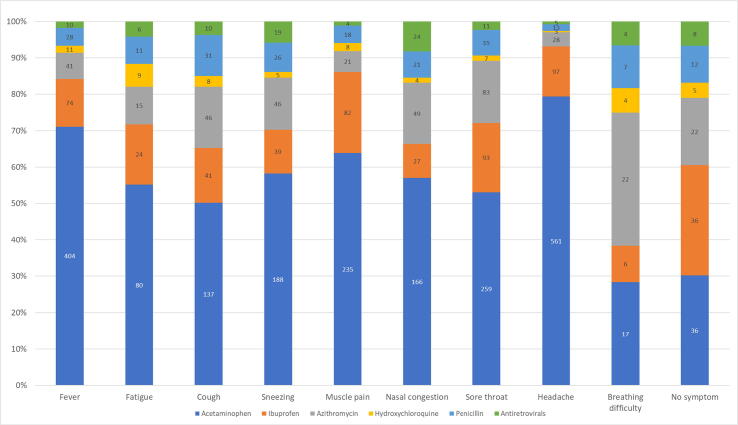
3.4. Respiratory symptoms attributed to self-medication
Fig. 1 shows the distribution of respiratory symptoms for which the respondents self-medicated with the various drugs we surveyed. The respiratory symptoms we surveyed for were fever, fatigue, cough, sneezing, muscle pain, nasal congestion, sore throat, headache and breathing difficulty. We also surveyed if the respondents self-medicated without any symptom. It was observed that for all the symptoms, except breathing difficulty, the most self-medicated drug was acetaminophen. In the case of fever, 568 respondents indicated that they consumed at least one of the drugs we surveyed for. For fatigue 145 respondents, 273 for cough, 323 for sneezing, 368 for muscle pain, 291 for nasal congestion, 488 for sore throat, 707 for headache, 60 for breathing difficulty, and 119 without any symptom. In the case of fever, the predominant drugs consumed were acetaminophen (404 [71%]) followed by ibuprofen (74 [13%]). For fatigue, 80 (55.2%) used acetaminophen followed by ibuprofen 24 (16.6%); for cough 137 (50.2%) consumed acetaminophen and 46 (16.8%) azithromycin. In the case of sneezing, often confused as a COVID-19 symptom, the most used drug for this symptom was acetaminophen (188 [58.2%]) followed by azithromycin (46 [14.2%]). For muscle pain the most consumed drugs were the analgesics acetaminophen (235 [63.8%]) and ibuprofen (82 [22.3%]), similar situation was observed for sore throat: acetaminophen (259 [53.1%]) and ibuprofen (93 [19.1%]) and for headache: acetaminophen (561 [79.3%]) and ibuprofen (97 [13.7%]). For nasal congestion, 166 (57.0%) used acetaminophen and 49 (16.8%) azithromycin; while for breathing difficulty 22 (36.7%) used azithromycin and 17 (28.3%) acetaminophen. It became alarming that 119 respondents consumed the surveyed drugs without any symptom with the following distribution: acetaminophen (36 [30.3%]), ibuprofen (36 [30.3%]), azithromycin (22 [18.5%]), penicillin (12 [10.1%]), antiretrovirals (8 [6.7%]) and hydroxychloroquine (5 [10.1%])
Fig. 1.
Respiratory symptom distribution for self-medication of various drugs during the COVID-19 lockdown in Peru.
3.5. Perception of symptom improvement after self-medication
The majority of respondents indicated that they perceived that at least one symptom improved with the use of acetaminophen (1000 [97.7%]), ibuprofen (270 [96.1%]), azithromycin (173 [95.0%]), penicillin (84 [96.5%]), antiretrovirals (59 [98.3%]) and hydroxychloroquine (26 [92.9%]) (Table 2). However, this could have been attributed to the combined use of more than one of these drugs or the combination of other drugs that were not assessed in this study. It was observed that a portion of respondents self-medicated because other reasons, which could be attributed to the broad application of the surveyed drugs. For instance, acetaminophen and ibuprofen are widely used as pain relievers and antipyretics. Similarly, azithromycin and penicillin are antibiotics that are consumed for various conditions, and in the case of the anti-malarial drug hydroxychloroquine is also used for lupus and rheumatoid arthritis (Jaffe, 2020).
The respondents had the option to indicate any other drug that they used for respiratory symptoms and various drug classes were reported such as antihistamines (cetirizine, chlorphenamine, loratadine), nonsteroidal anti-inflammatory drugs (NSAIDs) (naproxen, diclofenac), antibiotics (amoxicillin), corticosteroids (dexamethasone), analgesics (metamizole), flu medicine (not specified), vitamin supplements (vitamin C), and others (ginger, garlic, honey, onion, lemon, eucalyptus and sodium bicarbonate). Regarding the total responses for other drugs, the most frequent was cetirizine (13%) followed by chlorphenamine (9%), and naproxen (7%).
3.6. Multivariate analysis of the factors prompting respondents to self-medication
In the multivariate analysis (Table 3), it was observed that older respondents had a higher frequency of antiretroviral self-medication (aPR: 1.07; 95% CI: 1.00–1.14; p-value: 0.043) when adjusted for gender, marital status, job status, and educational level. It was also observed that respondents who currently have a job had a higher frequency of penicillin self-medication (aPR: 8.86; 95% CI: 1.27–61-93; p-value: 0.028) when adjusted for gender, age, marital status, and level of education. The region (coast, Andes and rainforest) was used a cluster group with the consumption of drugs in the coast used as the category for comparison. It was observed that for acetaminophen, the respondents from the Andes consumed it less (aPR: 0.47, 95% CI: 0.29–0.74, p-value: 0.001), while the respondents from the rainforest consumed more acetaminophen (aPR: 2.68, 95% CI: 1.24–5.79, p-value: 0.012). There were no other significant differences in consumption of the other drugs between regions of Peru.
Table 3.
Multivariate analysis of the factors associated with the self-medication of various drugs during the COVID-19 lockdown in Peru.
| Variables | Acetaminophen | Ibuprofen | Azithromycin | Hydroxychloroquine | Penicillin | Antiretrovirals |
|---|---|---|---|---|---|---|
| Sex | 0.574 | 0.988 | 0.911 | 0.433 | 0.299 | 0.563 |
| Age (years)* | 0.542 | 0.445 | 0.380 | 0.908 | 0.207 | (+) 0.043 |
| Single marital status | 0.787 | 0.448 | 0.070 | 0.671 | Not converge | 0.175 |
| Currently have a job | 0.500 | 0.740 | 0.109 | 0.141 | (+) 0.028 | 0.891 |
| At least Bachelor’s degree | 0.602 | 0.740 | 0.206 | 0.627 | 0.845 | 0.742 |
| Region of Peru | ||||||
| Coast | This category served as a comparison | |||||
| Andes | (−) 0.001 | 0.353 | 0.055 | 0.877 | 0.537 | 0.347 |
| Rainforest | (+) 0.012 | 0.146 | 0.992 | Not converge | Not converge | Not converge |
The dependent variable corresponds to the sum of respondents who used the drugs as a preventive, presence of symptoms, and confirmed case.
The reported p-values were obtained by generalized linear models, with the Poisson family, log link function, and robust models.
p-values < 0.05 have a sign that indicates whether there was a positive or negative association with the dependent variable.
This variable was taken quantitatively.
4. Discussion
Self-medication is more common in countries where healthcare systems tend to be less effective because of long waiting time in healthcare facilities, difficulty in obtaining physicians’ appointments, insufficient stock of essential medicines, delay in attention and insufficient amount of available beds/space in healthcare facilities (Meena et al., 2016). Even before the pandemic Peru already reunited all these characteristics (Alvarez-Risco et al., 2016, Alvarez-Risco et al., 2018), which became more evident during the COVID-19 pandemic exposing Peru’s fragmented and underfunded healthcare system (Gonzales-Tamayo et al., 2020a). Most of the respondents in our study were healthcare workers that during the lockdown have been the first respondents exposed to higher risk of becoming infected with COVID-19 (Ing et al., 2020). The long hours at work under difficult and stressful circumstances (Bogren et al., 2020) have caused an increase in anxiety, distress and overall psychological burden in healthcare workers in Peru (Yáñez et al., 2020e). These conditions have been reported to trigger self-medication in order to face work-related stress, pressure, discomfort and anxiety (Omolase et al., 2007, Barros et al., 2009). The general public is also under stress, anxiety and distress conditions as Peru reports a high number of physician deaths because of COVID-19 (Gonzales-Tamayo et al., 2020a) and has recently became the country with the highest mortality in the world (MenaFN, 2020, Yáñez et al., 2020c).
Our study reported that acetaminophen was the drug most consumed with higher use in the rainforest and lower in the Andes when compared to the coast of Peru. Acetaminophen has also been reported to be a drug that is preferentially self-medicated in Ethiopia (Shafie et al., 2018) and Brazil (Barros et al., 2019) for chronic pain. It has been reported that acetaminophen is widely used by health science major students in Nigeria as a pain reliever (Esan et al., 2018). However, it is alarming that its consumption is believed to be non-toxic regardless of the dose (Esan et al., 2018). Acetaminophen standard therapeutic oral dose is 0.5–1 g every 4–6 h to a maximum of 4 g/day, but more importantly it has a dose-dependent toxicity (Roberts et al., 2016). Acetaminophen can cause hepatoxicity after major overdose (Prescott, 2000), and severe liver damage has been observed with long-term use even at therapeutic doses in patients with alcoholic liver disease or viral infections (Day et al., 2000). Furthermore, it has been reported that long-term consumption of acetaminophen carries a potential risk factor for chronic renal failure (McLaughlin et al., 1998), cardiovascular, gastrointestinal and even mortality (Roberts et al., 2016). Therefore, acetaminophen is a drug to consume with caution especially considering that its sales has increased significantly during the COVID-19 pandemic (Romano et al., 2020).
Ibuprofen was the second drug most consumed (7.4%) in our study even though it has been reported that this NSAID increases the risk of developing thromboembolism in COVID-19 patients (Arjomandi Rad et al., 2020). Furthermore, it has been proposed that it could worsen the course of COVID-19 infection (Yang et al., 2020, Favalli et al., 2020, Fang et al., 2020), but more evidence is still needed (Torjesen, 2020). It also needs to considered that ibuprofen alone or in combination with acetaminophen could mask the fever during COVID-19 infection causing a delay in diagnosis and treatment (Favalli et al., 2020, Torjesen, 2020).
Regarding the consumption of the antibiotic azithromycin, one in five respondents who consumed it reported that they consumed it without having any respiratory symptom, as a preventive measure or because they thought they would have COVID-19. In an in vitro study, the combination of azithromycin and hydroxychloroquine showed a synergistic effect against SARS-CoV-2, and it was also reported on the possible anti-inflammatory properties of azithromycin, which could improve the disease progression (Damle et al., 2020, Andreani et al., 2020). However, its administration in combination therapy with hydroxychloroquine has been implicated in the elevation of the QT interval (Mercuro et al., 2020). Given the limited data available to ensure the efficacy of combination therapy, the American Society for Infectious Diseases recommends that the hydroxychloroquine/ chloroquine plus azithromycin combination be limited to clinical trials (Mercuro et al., 2020, Bhimraj et al., 2020). Regarding the self-medication of hydroxychloroquine, our study reported that one in four respondents who consumed it said that it was without symptoms, as a preventive measure or because they developed COVID-19 symptoms. The combined use of hydroxychloroquine and azithromycin was publicly endorsed by President Trump, which caused self-medication causing several reports of severe poisoning in Nigeria and USA (Busari et al., 2020). This public endorsement triggered various in vitro and in vivo studies that reported a decrease in viral load and mitigation in the cytokine storm in critically ill patients with SARS-CoV-2 (Gautret, Lagier, Parola, Hoang, Meddeb, Mailhe, et al., 2020). Similarly, various studies reported the positive use of hydroxychloroquine and azithromycin for treatment in hospitalized COVID-19 patients (Yao et al., 2020, Gautret et al., 2020a, Gautret et al., 2020b, Million et al., 2020). However, the consumption of hydroxychloroquine with or without azithromycin caused an increase in cardiotoxic risk such as QT prolongation, torsades de pointes, and sudden death in hospitalized patients with COVID-19 (Mercuro et al., 2020, Chorin et al., 2020, Ramireddy et al., 2020). Even though, the literature alerts about the possible risks with the combination of azithromycin and hydroxychloroquine it is recommended in Peru for moderate and severe COVID-19 cases in a clinical setting since May 2020 (MINSA., 2020c, Rojas et al., 2020). For mild COVID-19 patients, hydroxychloroquine is recommended at a dose of 400 mg orally every 12 h for the first day, and 200 mg orally every 12 h for 6 days (MINSA, 2020c). In the case of moderate to severe COVID-19 patients, hydroxychloroquine is recommended at a dose of 200 mg orally every 8 h for 7–10 days, or hydroxychloroquine + azithromycin at a dose regimen of 200 mg orally every 8 h for 7–10 days (hydroxychloroquine) + 500 mg orally on the first day and then 250 mg every 24 h for 5 days (MINSA, 2020c). However, on September 7, 2020 the ex-Minister of Health of Peru, Victor Zamora requested for ivermectin, hydroxychloroquine and azithromycin to be removed from the official COVID-19 treatment in Peru (RPP, 2020). It was during his administration that their use was approved, but his recent request was based on the lack of efficacy and increased risk that has been observed over the last few months (RPP, 2020).
Regarding the consumption of antiretrovirals, our study reported that one in six respondents consumed them without symptoms, as a preventive measure or because they thought they had COVID-19. Our multivariate analysis indicated that older people tend to have a higher consumption of antiretrovirals. This could be caused because the perception that any antiretroviral would have a positive effect against the viral COVID-19 infection. However, liver damage has been observed in COVID-19 patients (Velarde-Ruiz Velasco et al., 2020). Considering that antiretrovirals list liver damage as a common adverse effect (Alonso-Bello et al., 2018, Mallolas et al., 2003), it would make them inappropriate for use in COVID-19 patients. Their use is relevant for other pathologies, but a recent review has determined that there is no clear evidence of the beneficial effects of antiretrovirals in the prevention of COVID-19 (Ford et al., 2020, Dong et al., 2020b). More research is still needed to determine the cost and benefit of antiretrovirals for COVID-19.
Our study reported that 19 people self-medicated with penicillin without having symptoms, as a preventive measure or because they thought they would have COVID-19. It becomes interesting that penicillin was used because it lacks scientific information that supports its use for COVID-19. However, its use could be partially attributed to a lack of general knowledge about COVID-19 symptoms (Gomez Tejeda et al., 2020) and lack of information on what drugs to take (Huaroto et al., 2020). More research is needed in order to determine the effect of penicillin in COVID-19 patients.
The respondents indicated that they perceived an improvement in respiratory and COVID-19 symptoms after self-medication with these drugs alone or in combination. However, this could have been due to a placebo effect or because the symptoms were mild or because the majority of COVID-19 patients recover due to its lethality rate of less than 5% (MINSA, 2020d). Even though, some of these drugs in Peru do not need prescription (acetaminophen and ibuprofen), the others (azithromycin, hydroxychloroquine, penicillin and antiretrovirals) require prescription. Therefore, the pharmaceutical care system needs to be revised in Peru to prevent people to obtaining prescription-drugs so easily or in the black market. According to the World Health Organization (WHO) (WHO, 2000), it is important in a healthcare system to provide personal assessment to patients during pharmaceutical care as an important strategy to provide guidance in the use of Over-the-counter (OTC) and prescription drugs (Tong et al., 2019).
The study had as a limitation that the results cannot be extrapolated to the entire Peruvian population since a random or multilevel sampling has not been carried out for this purpose. Also, cross-sectional studies do not permit an establishment of a clear cause and effect. The objective of this article was to report the frequencies of use and find some statistical associations; however, this report becomes the first study in such a large population in Peru, which could serve as a basis for other research.
5. Conclusion
Self-medication is a significant health issue in Peru, especially during the COVID-19 pandemic. Various drugs were used for respiratory and COVID-19 related symptoms without sufficient scientific evidence. Acetaminophen was the most consumed drug, but there was also a significant use of antibiotics (penicillin and azithromycin), hydroxychloroquine, and even antiretrovirals. People in Peru consumed them as COVID-19 preventives, to treat suspected symptoms and even after a COVID-19 positive diagnosis. Acetaminophen consumption was associated with the region where one lived, antiretrovirals consumption was associated with the age of the respondent, and penicillin consumption was higher in people currently working. Continuous awareness and sensitization about the risks of self-medication are warranted. Our results should be taken with care and not interpreted as a recommendation to self-medicate nor to use these drugs thinking that they will improve symptomatology. Always seek medical help and consultation before consuming any drug. We hope these results would inform healthcare policy makers on the measures to improve pharmaceutical care as they strive to save lives.
Funding
The authors declare that no funding was received.
Author contributions
Data filtering: JFQC, EFR, DM, JMZ, KMHC, SECE, HGP; Statistical analysis: JFQC, EFR, DM, JMZ, KMHC, SECE, HG, JAY, CRM; Writing: AAR, JAY, CRM; Review of manuscript: AAR, JAY, CRM.
Role of the funding source
The authors declare that no funding was received.
Data sharing statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Annex 1. Survey to assess the use of drugs in the prevention and treatment of respiratory symptoms during the COVID-19 pandemic
Demographic data
-
1.
City where you live: ______________________
-
2.
Sex: Male () Female () I prefer not to say ()
-
3.
Age: _________ (years)
-
4.
Marital status: Single () Married () Domestic partnership () Divorced () Widowed ()
-
5.
Education level: No studies () Primary () High School () Associate () Bachelor () Postgraduate ()
-
6.
Do you currently work?
-
7.
If you work, indicate the industry: Food () Commerce () Construction () Education () Housekeeper () Entertainment () Police/Armed forces () Healthcare () Transportation () Tourism () Telecommunications () Other:____________
About the use of drugs against respiratory symptoms during the COVID-19 lockdown
-
8.
Indicate if you use any of these drugs during the COVID-19 lockdown
| Drug | Did you use it? | |
|---|---|---|
| Paracetamol / Acetaminophen | Yes () | No () |
| Ibuprofen | Yes () | No () |
| Azithromycin | Yes () | No () |
| Hydroxychloroquine | Yes () | No () |
| Penicillin | Yes () | No () |
| Antiretroviral (Lopinavir, Ritonavir, Remdesivir, etc.) | Yes () | No () |
| Another drug (please specify) ______________________ | Yes () | No () |
-
9.
Indicate the reason why you used the drugs you did during the COVID-19 lockdown
The reasons are numbered from 1 to 7
-
1.
I had a cold/flu
-
2.
I used it without having any symptom
-
3.
I used it as a preventive for COVID-19
-
4.
I had COVID-19 symptoms and self-medicated
-
5.
I was positively diagnosed with COVID-19 and self-medicated to treat it
-
6.
I consumed it regularly because other reasons
-
7.
Other (please specify)
Check only one option for each drug you used
| Drug | Why did you consume this drug? |
|---|---|
| Paracetamol / Acetaminophen | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Ibuprofen | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Azithromycin | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Hydroxychloroquine | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Penicillin | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Antiretroviral | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
| Another drug: ______________ | 1 () 2 () 3 () 4 () 5 () 6 () 7 () |
-
10.
Indicate the symptom(s) for which you use the drugs you did
Symptoms are numbered 1–11
-
1.
Fever
-
2.
Fatigue
-
3.
Cough
-
4.
Sneezing
-
5.
Muscle pain
-
6.
Nasal congestion
-
7.
Sore throat
-
8.
Headache
-
9.
Breathing difficulty
-
10.
I used this drug even though I did not have any of the previous symptoms
-
11.
Other (please specify the symptom)
You can check more than one symptom
| Drug | What symptom(s) did you use this drug for? |
|---|---|
| Paracetamol / Acetaminophen | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Ibuprofen | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Azithromycin | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Hydroxychloroquine | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Penicillin | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Antiretroviral | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
| Another drug: ______________ | 1 () 2 () 3 () 4 () 5 () 6 () 7 () 8 () 9 () 10 () 11 () |
-
11.
Indicate if you perceived the use of these drugs alleviated your symptoms
Options are numbered from 1 to 5
-
1.
I perceive that it alleviated all the symptoms
-
2.
I perceive that it alleviated most of the symptoms
-
3.
I perceive that it alleviated a few of the symptoms
-
4.
I perceive that it alleviated only one symptom
-
5.
I perceive that it did not alleviated any of the symptoms
Check only one option
| DRUGS | Did this drug alleviated your symptoms? |
|---|---|
| Paracetamol / Acetaminophen | 1 () 2 () 3 () 4 () 5 () |
| Ibuprofen | 1 () 2 () 3 () 4 () 5 () |
| Azithromycin | 1 () 2 () 3 () 4 () 5 () |
| Hydroxychloroquine | 1 () 2 () 3 () 4 () 5 () |
| Penicillin | 1 () 2 () 3 () 4 () 5 () |
| Antiretroviral | 1 () 2 () 3 () 4 () 5 () |
| Another drug: ______________ | 1 () 2 () 3 () 4 () 5 () |
References
- Alonso-Bello C.D., Reyes-Cetina I.L., Delgado-Cortés H.M., Martínez-Velázquez M., Arroyo-Mendoza M.E. Lesión hepática inducida por antirretrovirales. Rev Hosp Jua Mex. 2018;85(1):49–56. [Google Scholar]
- Alvarez-Risco A., Del-Aguila-Arcentales Shyla, Diaz-Risco S. Pharmacovigilance as a tool for sustainable development of healthcare in Peru. PharmacoVigilance Review. 2018;10(2):4–6. [Google Scholar]
- Alvarez-Risco Aldo, Turpo-Carma A., Ortiz-Palomino L., Gongora-Amaut N., Del-Aguila-Arcentales Shyla. Barreras para la implementación de la Atención Farmacéutica en establecimientos farmacéuticos de Cusco, Perú Barriers to the implementation of pharmaceutical care in pharmacies in Cusco, Peru. Pharmaceutical Care Espana. 2016;18:194–205. [Google Scholar]
- Alvarez-Risco Aldo, Mejia Christian R., Delgado-Zegarra Jaime, Del-Aguila-Arcentales Shyla, Arce-Esquivel Arturo A., Valladares-Garrido Mario J., Rosas del Portal Mauricio, Villegas León F., Curioso Walter H., Chandra-Sekar M., Yáñez Jaime A. The Peru approach against the COVID-19 infodemic: insights and strategies. Am. J. Trop. Med. Hygiene. 2020;103(2):583–586. doi: 10.4269/ajtmh.20-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreani J., Le Bideau M., Duflot I., Jardot P., Rolland C., Boxberger M., Wurtz N., Rolain J.M., Colson P., La Scola B., Raoult D. In vitro testing of combined hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect. Microb. Pathog. 2020;145 doi: 10.1016/j.micpath.2020.104228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo-Banchon W.J., Aveiro-Robalo T.R., Fernandez M.F., Castro-Pacoricona D., Moncada-Mapelli E., Chanava W., Mejia C.R. Progresión de casos de Coronavirus en Latinoamérica: Análisis comparativo a una semana de iniciada la pandemia en cada país. Kasmera. 2020;48(1) doi: 10.5281/zenodo.3830750. [DOI] [Google Scholar]
- Rad Arjomandi, Arian Robert Vardanyan, Tas Natalie R. Ibuprofen and thromboembolism in SARS-COV2. J. Thrombosis Haemostasis. 2020 doi: 10.1111/jth.14901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros Aline Reis Rocha, Griep Rosane Harter, Rotenberg Lúcia. Self-medication among nursing workers from public hospitals. Revista Latino-Americana de Enfermagem. 2009;17:1015–1022. doi: 10.1590/s0104-11692009000600014. [DOI] [PubMed] [Google Scholar]
- Barros Guilherme Antonio Moreira de, Marchetti Calonego Marco A., Mendes Rannier F., Castro Raphael A.M., Faria João F.G., Trivellato Stella A., Cavalcante Rodney S., Fukushima Fernanda B., Dias Adriano. The use of analgesics and risk of self-medication in an urban population sample: cross-sectional study. Braz. J. Anesthesiol. (Engl. Edit.) 2019;69(6):529–536. doi: 10.1016/j.bjane.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhimraj A., Morgan R.L., Shumaker A.H., Lavergne V., Baden L., Cheng V.C., Edwards K.M., Gandhi R., Muller W.J., O'Horo J.C., Shoham S., Murad M.H., Mustafa R.A., Sultan S., Falck-Ytter Y. Infectious diseases society of america guidelines on the treatment and management of patients with COVID-19. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogren Malin, Erlandsson Kerstin, Johansson Anders, Kalid Mohamed, Igal Asad Abdi, Mohamed Jamal, Said Fatumo, Pedersen Christina, Byrskog Ulrika, Osman Fatumo. Health workforce perspectives of barriers inhibiting the provision of quality care in Nepal and Somalia – A qualitative study. Sexual Reprod. Healthcare. 2020;23 doi: 10.1016/j.srhc.2019.100481. [DOI] [PubMed] [Google Scholar]
- Busari, S., Adebayo, B., 2020. Nigeria records chloroquine poisoning after Trump endorses it for coronavirus treatment. CNN, [cited 29 August 2020. Available from https://edition.cnn.com/2020/03/23/africa/chloroquine-trump-nigeria-intl/index.html.
- CDC, 2020. Coronavirus Disease 2019 Symptoms. Center for Disease Control and Prevention, [cited 04 July 2020. Available from https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
- Chorin Eh.ud., Dai Matthew, Shulman Eric, Wadhwani Lalit, Bar-Cohen Roi, Barbhaiya Chirag, Aizer Anthony, Holmes Douglas, Bernstein Scott, Spinelli Michael, Park David S., Chinitz Larry A., Jankelson Lior. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat. Med. 2020;26(6):808–809. doi: 10.1038/s41591-020-0888-2. [DOI] [PubMed] [Google Scholar]
- Damle B., Vourvahis M., Wang E., Leaney J., Corrigan B. Clinical pharmacology perspectives on the antiviral activity of azithromycin and use in COVID-19. Clin. Pharmacol. Ther. 2020 doi: 10.1002/cpt.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day Richard O., Graham Garry G., Whelton Andrew. The position of paracetamol in the world of analgesics. Am. J .Ther. 2000;7(2):51–54. doi: 10.1097/00045391-200007020-00002. [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet. Infect. Dis. 2020;20(5):533–534. doi: 10.1016/s1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong L., Hu S., Gao J. Discovering drugs to treat coronavirus disease 2019 (COVID-19) Drug Discov. Therap. 2020;14(1):58–60. doi: 10.5582/ddt.2020.01012. [DOI] [PubMed] [Google Scholar]
- Esan Deborah Tolulope, Fasoro Ayodeji Akinwande, Odesanya Opeoluwa Esther, Esan Theophilus Olaide, Ojo Elizabeth Funmilayo, Faeji Charles Oluwafemi. Assessment of self-medication practices and its associated factors among undergraduates of a private university in Nigeria. J. Environ. Public Health. 2018;2018:5439079. doi: 10.1155/2018/5439079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang Lei, Karakiulakis George, Roth Michael. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8(4) doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favalli Ennio Giulio, Ingegnoli Francesca, De Lucia Orazio, Cincinelli Gilberto, Cimaz Rolando, Caporali Roberto. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmun. Rev. 2020;19(5) doi: 10.1016/j.autrev.2020.102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford N., Vitoria M., Rangaraj A., Norris S.L., Calmy A., Doherty M. Systematic review of the efficacy and safety of antiretroviral drugs against SARS, MERS or COVID-19: initial assessment. J. Int. AIDS Soc. 2020;23(4) doi: 10.1002/jia2.25489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautret P., Lagier J.C., Parola P., Hoang V.T., Meddeb L., Sevestre J., Mailhe M., Doudier B., Aubry C., Amrane S., Seng P., Hocquart M., Eldin C., Finance J., Vieira V.E., Tissot-Dupont H.T., Honoré S., Stein A., Million M., Colson P., La Scola B., Veit V., Jacquier A., Deharo J.C., Drancourt M., Fournier P.E., Rolain J.M., Brouqui P., Raoult D. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: a pilot observational study. Travel Med. Infect. Dis. 2020;34 doi: 10.1016/j.tmaid.2020.101663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautret Philippe, Lagier JeanChristophe, Parola Philippe, Hoang Van Thuan, Meddeb Line, Mailhe Morgane, Doudier Barbara, Courjon Johan, Giordanengo Valérie, Vieira Vera Esteves, Dupont Hervé Tissot, Honoré Stéphane, Colson Philippe, Chabrière Eric, La Scola Bernard, Rolain Jean-Marc, Brouqui Philippe, Raoult Didier. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int. J. Antimicrobial Agents. 2020:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Gomez Tejeda, Jesus, Jairo, Alejandro Dieguez Guach, Ronny, Ramon Perez Abreu, Manuel, Tamayo Velazquez, Odalis, Elizabeth Iparraguirre Tamayo, Aida, 2020. Evaluación del nivel de conocimiento sobre COVID-19 durante la pesquisa en la población de un consultorio. 59 (277).
- Gonzales-Tamayo, L., Arevalo-Oropeza, M., Yáñez, J.A., 2020a. COVID-19 physician deaths in Peru: a result of an underfunded and fragmented healthcare system. F1000Research (Available at SSRN: https://ssrn.com/abstract=3676849).
- Gonzales-Tamayo, L., Arevalo-Oropeza, M., Yáñez, J.A., 2020b. COVID-19 physician deaths in Peru: a result of an underfunded and fragmented healthcare system. Available at SSRN: https://ssrn.com/abstract=3676849.
- Hasan S., Kow C.S., Merchant H.A. Is it worth the wait? Should Chloroquine or Hydroxychloroquine be allowed for immediate use in CoViD-19? Brit. J. Pharmacy. 2020;5(1):1–5. doi: 10.5920/bjpharm.745. [DOI] [Google Scholar]
- Huaroto F., Reyes N., Huamán K., Bonilla C., Curisinche-Rojas M., Carmona G., Gutierrez E., Caballero P. Intervenciones farmacológicas para el tratamiento de la Enfermedad por Coronavirus (COVID-19) Anales de la Facultad de Medicina. 2020;81(1):71–79. doi: 10.15381/anales.v81i1.17686. [DOI] [Google Scholar]
- Hughes Carmel M., McElnay James C., Fleming Glenda F. Benefits and risks of self medication. Drug Saf. 2001;24(14):1027–1037. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- Ing E.B., Xu Q., Salimi A., Torun N. Physician deaths from corona virus (COVID-19) disease. Occup. Med. 2020 doi: 10.1093/occmed/kqaa088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe Susan. Regulators split on antimalarials for COVID-19. Lancet. 2020;395(10231):1179. doi: 10.1016/S0140-6736(20)30817-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones Aaron, Feeny David, Costa Andrew P. Longitudinal construct validity of the minimum data set health status index. Health Qual. Life Outcomes. 2018;16(1):102. doi: 10.1186/s12955-018-0932-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim Jaegyun, Jeon Seunghyun, Shin Hyun Young, Kim Moon Jung, Seong Yu Min, Lee Wang Jun, Choe Kang Won, Kang Yu Min, Lee Baeckseung, Park Sang Joon. Case of the index patient who caused tertiary transmission of COVID-19 infection in Korea: the application of lopinavir/ritonavir for the treatment of COVID-19 infected pneumonia monitored by quantitative RT-PCR. J. Korean Med. Sci. 2020;35(6) doi: 10.3346/jkms.2020.35.e79. e79-e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallhi, Tauqeer Hussain, Khan, Yusra Habib, Alotaibi, Nasser Hadal, Alzarea, Abdulaziz Ibrahim, Alanazi, Abdullah Salah, Qasim, Sumera, Iqbal, Muhammad Shahid, Tanveer, Nida, 2020. Drug repurposing for COVID-19: a potential threat of self-medication and controlling measures. Postgraduate Med. J. postgradmedj-2020-138447. doi: 10.1136/postgradmedj-2020-138447. [DOI] [PMC free article] [PubMed]
- Mallolas J., Casado J.L., Martinez E., Laguno M., Blanco J.L., Lonca M., Leon A., Milinkovic A., Biglia A., Miro J.M., Garcia F., Gateli J.M. Hepatotoxicidad asociada al tratamiento antirretroviral. Enf Emerg. 2003;5(2):97–104. [Google Scholar]
- Mandal Shyamapada. Can over-the-counter antibiotics coerce people for self-medication with antibiotics? Asian Pacific J. Trop. Dis. 2015;5:S184–S186. doi: 10.1016/S2222-1808(15)60886-6. [DOI] [Google Scholar]
- Mansuri FarahM.A., Zalat Marwa M., Khan Adeel A., Alsaedi Esraa Q., Ibrahim Hanan M. Estimating the public response to mitigation measures and self-perceived behaviours towards the COVID-19 pandemic. J. Taibah Univ. Med. Sci. 2020 doi: 10.1016/j.jtumed.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matias T., Dominski F.H., Marks D.F. Human needs in COVID-19 isolation. J. Health Psychol. 2020;25(7):871–882. doi: 10.1177/1359105320925149. [DOI] [PubMed] [Google Scholar]
- McLaughlin J.K., Lipworth L., Chow W.H., Blot W.J. Analgesic use and chronic renal failure: a critical review of the epidemiologic literature. Kidney Int. 1998;54(3):679–686. doi: 10.1046/j.1523-1755.1998.00043.x. [DOI] [PubMed] [Google Scholar]
- Meena Parulekar, Nandakumar Mekoth, Ramesh C.M., Ajit Parulekar. Self-medication in developing countries a systematic review. J. Pharm. Technol. Res. Manage. 2016;4(2) doi: 10.15415/jptrm.2016.42007. [DOI] [Google Scholar]
- Mejia C.R., Rodriguez-Alarcon J.F., Carbajal M., Perez-Espinoza P., Porras-Carhuamaca L.A., Sifuentes-Rosales J., Contreras-Cabrera J.M., Carranza Esteban R.F., Ruiz Mamani P.G. Fatalismo ante la posibilidad de contagio por el coronavirus: generación y validación de un instrumento (F-COVID-19) Kasmera. 2020;47 doi: 10.5281/zenodo.3732353. [DOI] [Google Scholar]
- Mejia C.R., Rodriguez-Alarcon J.F., Carbajal M., Sifuentes-Rosales J., Campos-Urbina A.M., Charri J.C., Garay-Rios L., Al-Kassab-Cordova A., Mamami-Benito O., Apaza-Tarqui E.E. Validación de una escala breve para la medición del nivel de conocimientos básicos acerca del Coronavirus, Perú (KNOW-P-COVID-19) Kasmera. 2020;48 doi: 10.5281/zenodo.3827988. [DOI] [Google Scholar]
- Mejia C.R., Ticona D., Rodriguez-Alarcon J.F., Campos-Urbina A.M., Catay-Medina J.B., Porta-Quinto T., Garayar-Peceros H., Ignacio-Quinte C., Carranza Esteban R.F., Ruiz Mamani P.G., Tovani-Palone M.R. The Media and their informative role in the face of the coronavirus disease 2019 (COVID-19): validation of fear perception and magnitude of the issue (MED-COVID-19) Electronic J. Gen. Med. 2020;17(6):em239. doi: 10.29333/ejgm/7946. [DOI] [Google Scholar]
- Mejia, Christian R., Quispe-Sancho, Alan, Franco Rodriguez - Alarcon, J., Ccasa-Valero, Laura, Ponce-López, Vania L., Varela-Villanueva, Elizabeth S., Marticorena-Flores, Rahi K., Chamorro-Espinoza, Scherlli E., Avalos-Reyes, Maryori S., Vera-Gonzales, Jean J., 2020. Factores asociados al fatalismo ante la COVID-19 en 20 ciudades del Perú en marzo 2020. 19 (2).
- Mejia Christian R., Franco Rodriguez-Alarcon J., Garay-Rios Lizet, de Guadalupe Maria, Enriquez-Anco Alfrando Moreno, Huaytan-Rojas Kennedy, Huari Nory Huancahuari-Ñañacc, Julca-Gonzales Angel, Alvarez Christian H., Choque-Vargas José, Curioso Walter H. Percepción de miedo o exageración que transmiten los medios de comunicación en la población peruana durante la pandemia de la COVID–19. Revista Cubana de Investigaciones Biomédicas. 2020;39(2) [Google Scholar]
- MenaFN. 2020. Peru: Highest mortality rate from COVID-19. MenaFN, [cited 29 August 2020. Available from https://menafn.com/1100706914/Peru-Highest-mortality-rate-from-COVID-19.
- Menary Kyle R., Kushner Matt G., Maurer Eric, Thuras Paul. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. J. Anxiety Disord. 2011;25(3):335–339. doi: 10.1016/j.janxdis.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng Xiangming, Deng Yanzhong, Dai Zhiyong, Meng Zhisheng. COVID-19 and anosmia: a review based on up-to-date knowledge. Am. J. Otolaryngol. 2020;41(5) doi: 10.1016/j.amjoto.2020.102581. 102581-102581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercuro N.J., Yen C.F., Shim D.J., Maher T.R., McCoy C.M., Zimetbaum P.J., Gold H.S. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Million Matthieu, Lagier Jean-Christophe, Gautret Philippe, Colson Philippe, Fournier Pierre-Edouard, Amrane Sophie, Hocquart Marie, Mailhe Morgane, Esteves-Vieira Vera, Doudier Barbara, Aubry Camille, Correard Florian, Giraud-Gatineau Audrey, Roussel Yanis, Berenger Cyril, Cassir Nadim, Seng Piseth, Zandotti Christine, Dhiver Catherine, Ravaux Isabelle, Tomei Christelle, Eldin Carole, Tissot-Dupont Hervé, Honoré Stéphane, Stein Andreas, Jacquier Alexis, Deharo Jean-Claude, Chabrière Eric, Levasseur Anthony, Fenollar Florence, Rolain Jean-Marc, Obadia Yolande, Brouqui Philippe, Drancourt Michel, La Scola Bernard, Parola Philippe, Raoult Didier. Early treatment of COVID-19 patients with hydroxychloroquine and azithromycin: a retrospective analysis of 1061 cases in Marseille, France. Travel Med. Infect. Dis. 2020;35 doi: 10.1016/j.tmaid.2020.101738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MINSA. 2020a. Minsa: Casos confirmados por Coronavirus Covid-19 ascienden a 187 400 en el Perú (Comunicado N° 122). Ministerio de Salud del Perú (MINSA), [cited 04 July 2020. Available from https://www.gob.pe/institucion/minsa/noticias/181047-minsa-casos-confirmados-por-coronavirus-covid-19-ascienden-a-187-400-en-el-peru-comunicado-n-122.
- MINSA. 2020b. Minsa: Casos confirmados por Coronavirus Covid-19 ascienden a 240 908 en el Perú (Comunicado N° 135). Ministerio de Salud del Perú (MINSA), [cited 04 July 2020. Available from https://www.gob.pe/institucion/minsa/noticias/187441-minsa-casos-confirmados-por-coronavirus-covid-19-ascienden-a-240-908-en-el-peru-comunicado-n-135.
- MINSA. 2020c. Resolución Ministerial N° 270-2020-MINSA - Prevención, Diagnóstico y Tratamiento de personas afectadas por COVID-19. Ministerio de Salud del Perú.
- MINSA. 2020d. Sala Situacional COVID-19 Peru. Ministerio de Salud del Perú (MINSA), [cited 07 September 2020. Available from https://covid19.minsa.gob.pe/sala_situacional.asp.
- Molina J.M., Delaugerre C., Le Goff J., Mela-Lima B., Ponscarme D., Goldwirt L., de Castro N. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Med. Mal Infect. 2020;50(4) doi: 10.1016/j.medmal.2020.03.006. 384-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omolase C.O., Adeleke O.E., Afolabi A.O., Afolabi O.T. Self medication amongst general outpatients in a nigerian community hospital. Ann. Ibadan Postgraduate Med. 2007;5(2):64–67. doi: 10.4314/aipm.v5i2.64032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onchonga David. A Google Trends study on the interest in self-medication during the 2019 novel coronavirus (COVID-19) disease pandemic. Saudi Pharm. J. 2020;28(7):903–904. doi: 10.1016/j.jsps.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onchonga David, Omwoyo Joshua, Nyamamba Duke. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm. J. 2020;28(10):1149–1154. doi: 10.1016/j.jsps.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott Laurie F. Therapeutic misadventure with paracetamol: fact or fiction? Am. J .Ther. 2000;7(2):99–114. doi: 10.1097/00045391-200007020-00007. [DOI] [PubMed] [Google Scholar]
- Ramireddy Archana, Chugh Harpriya, Reinier Kyndaron, Ebinger Joseph, Park Eunice, Thompson Michael, Cingolani Eugenio, Cheng Susan, Marban Eduardo, Albert Christine M., Chugh Sumeet S. Experience with hydroxychloroquine and azithromycin in the coronavirus disease 2019 pandemic: implications for QT interval monitoring. J. Am. Heart Assoc. 2020;9(12) doi: 10.1161/JAHA.120.017144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts Emmert, Nunes Vanessa Delgado, Buckner Sara, Latchem Susan, Constanti Margaret, Miller Paul, Doherty Michael, Zhang Weiya, Birrell Fraser, Porcheret Mark, Dziedzic Krysia, Bernstein Ian, Wise Elspeth, Conaghan Philip G. Paracetamol: not as safe as we thought? A systematic literature review of observational studies. Ann. Rheum. Dis. 2016;75(3):552–559. doi: 10.1136/annrheumdis-2014-206914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas B., Moscoso S., Chung S.A., Limpias Terceros B., Álvarez-Risco A., Yáñez J.A. Tratamiento contra el COVID-19 en Perú y Bolivia y el riesgo de automedicarse. Revista Cubana de Farmacia. 2020 In Press. [Google Scholar]
- Romano Sónia, Galante Heloísa, Figueira Débora, Mendes Zilda, Rodrigues António Teixeira. Time-trend analysis of medicine sales and shortages during COVID-19 outbreak: data from community pharmacies. Res. Soc. Admin. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RPP. 2020. Zamora plantea el retiro de la ivermectina e hidroxicloroquina: “No han mostrado ningún beneficio”. RPP Noticias, [cited 07 September 2020. Available from https://rpp.pe/peru/actualidad/coronavirus-en-peru-victor-zamora-plantea-el-retiro-de-la-ivermectina-e-hidroxicloroquina-no-han-mostrado-ningun-beneficio-noticia-1291101?ref=rpp.
- Shafie Mensur, Eyasu Mebrahtu, Muzeyin Kedija, Worku Yoseph, Martín-Aragón Sagrario. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS ONE. 2018;13(3) doi: 10.1371/journal.pone.0194122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodhi Mohit, Etminan Mahyar. Safety of ibuprofen in patients With COVID-19: causal or confounded? Chest. 2020;158(1):55–56. doi: 10.1016/j.chest.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasnim Samia, Hossain Md Mahbub, Mazumder Hoimonty. Impact of rumors and misinformation on COVID-19 in social media. J. Prev. Med. Public Health. 2020;53(3):171–174. doi: 10.3961/jpmph.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong Vivien, Aslani Parisa. OTC Medication and pharmaceutical care. In: Alves da Costa F., van Mil J.W.F., Alvarez-Risco A., editors. The Pharmacist Guide to Implementing Pharmaceutical Care. Springer; 2019. pp. 261–276. [Google Scholar]
- Torjesen Ingrid. Ibuprofen can mask symptoms of infection and might worsen outcomes, says European drugs agency. BMJ (Clinical Research Ed.) 2020;369 doi: 10.1136/bmj.m1614. [DOI] [PubMed] [Google Scholar]
- Tschannen D., Alexander C., Tovar E.G., Ghosh B., Zellefrow C., Milner K.A. Development of the nursing quality improvement in practice tool: advancing frontline nursing practice. J. Nurs. Care Qual. 2020;35(4):372–379. doi: 10.1097/ncq.0000000000000457. [DOI] [PubMed] [Google Scholar]
- Varela-Ruiz Margarita, Díaz-Bravo Laura, García-Durán Rocío. Descripción y usos del método Delphi en investigaciones del área de la salud. Investigación en educación médica. 2012;1:90–95. [Google Scholar]
- Velarde-Ruiz Velasco J.A., García-Jiménez E.S., Remes-Troche J.M. Manifestaciones hepáticas y repercusión en el paciente cirrótico de COVID-19. Revista de Gastroenterología de México. 2020 doi: 10.1016/j.rgmx.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker V.M., Davies N.M., Windmeijer F., Burgess S., Martin R.M. Power calculator for instrumental variable analysis in pharmacoepidemiology. Int. J. Epidemiol. 2017;46(5):1627–1632. doi: 10.1093/ije/dyx090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. 2000. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. World Health Organization, [cited 05 September 2020. Available from https://apps.who.int/iris/handle/10665/66154.
- WHO. 2013. Mid-level health workers for delivery of essential health services. A global systematic review and country experiences. Global Health Workforce Alliance, [cited 04 July 2020. Available from https://www.who.int/workforcealliance/knowledge/resources/MLHWCountryCaseStudies_annex12_Peru.pdf.
- Yáñez, J.A., Alvarez-Risco, A., Delgado-Zegarra, J., 2020a. Rapid Response: Clearing the path for COVID-19 in Peru? The decision of supervised walks for children and adolescents. Brit. Med. J. [cited 03 June 2020. Available from https://www.bmj.com/content/369/bmj.m1918/rr-9.
- Yáñez, J.A., Alvarez-Risco, A., Delgado-Zegarra, J., 2020b. Rapid Response: Does Peru really have that high number of COVID-19 confirmed cases? The deception of combining RT-PCR and rapid test results. The British Med. J. [cited 01 July 2020. Available from https://www.bmj.com/content/369/bmj.m2518/rr-4.
- Yáñez, J.A., Chung, S.A., Inga-Berrospi, F., Mejia, C.R., 2020. Demographic and Geographic COVID-19 Death Risk Factors in Peru. A Nationwide Analysis. EClinicalMedicine (Available at SSRN: https://ssrn.com/abstract=3648543).
- Yáñez Jaime A, Alvarez-Risco Aldo, Delgado-Zegarra Jaime. Covid-19 in Peru: from supervised walks for children to the first case of Kawasaki-like syndrome. BMJ (Clinical Research Ed.) 2020;369 doi: 10.1136/bmj.m2418. [DOI] [PubMed] [Google Scholar]
- Yáñez Jaime A., Jahanshahi Asghar Afshar, Alvarez-Risco Aldo, Li Jizhen, Zhang Stephen X. Anxiety, distress, and turnover intention of healthcare workers in peru by their distance to the epicenter during the COVID-19 crisis. Am. J. Trop. Med. Hygiene. 2020;103(4):1614–1620. doi: 10.4269/ajtmh.20-0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Xiaobo, Yuan Yu., Jiqian Xu., Shu Huaqing, Xia Jia'an, Liu Hong, Yongran Wu., Zhang Lu., Zhui Yu., Fang Minghao, Ting Yu., Wang Yaxin, Pan Shangwen, Zou Xiaojing, Yuan Shiying, Shang You. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Xueting, Ye Fei, Zhang Miao, Cui Cheng, Huang Baoying, Peihua Niu Xu., Liu Li Zhao, Dong Erdan, Song Chunli, Zhan Siyan, Roujian Lu., Li Haiyan, Tan Wenjie, Liu Dongyang. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed] [Google Scholar]