Abstract
Background:
Parental underestimation of the severity and risks of their child’s obesity and parents’ potential implicit weight bias contribute to the reluctance to consider bariatric surgery for their adolescent children with obesity. Despite evidence for safety and efficacy of bariatric surgery in adolescents, pediatric providers may be hesitant or uncomfortable discussing the benefits of and refer patients for surgical evaluation. Understanding these barriers is an essential step towards effective long-term care in this patient population.
Objectives:
We hypothesized that parental views on bariatric surgery are primarily influenced by personal experiences with bariatric surgery, their implicit bias, understanding of health risks of obesity, and counseling by pediatric providers.
Setting:
Data collected and analyzed at an Academic Medical Center, United States.
Methods:
Following a retrospective chart review of 192 adolescents with obesity, a telephone survey of patients’ parents was conducted.
Results:
Parents of 71.4% of patients who received outpatient weight loss counseling had accurate recollection of that event. Only 12.8% of parents who were referred to lifestyle programs successfully enrolled. Neither prior personal exposure to bariatric surgery, nor enrollment of the child in a lifestyle program increased parents’ likelihood to consider bariatric surgery for their child (p=0.10 and 0.70, respectively). Most parents (84.6%) who were counseled by their pediatric provider about bariatric surgery would consider it, compared to only 34.5% of the parents who did not receive counseling (p<0.001).
Conclusions:
Counseling by pediatric providers, not involvement in lifestyle programs or exposure to bariatric surgery, increased parents’ willingness to consider bariatric surgery for their child. Given the current recommendations to incorporate bariatric surgery as a treatment modality in severe adolescent obesity, earlier counseling about the role of surgery by pediatric providers is essential. More detailed provider education on the current state of bariatric surgery in the treatment of severe adolescent obesity is also necessary.
Keywords: adolescent, pediatric, obesity, parental, bariatric surgery
INTRODUCTION
Obesity in the pediatric population is a growing problem and the urgency to address it earlier in life is becoming more recognized by pediatric providers.(1,2) Traditional approaches in adolescence are similar to those in the pediatric population and mainly focus on lifestyle modification. Although earlier findings suggested the involvement of parents in lifestyle programs contributes to program success,(3,4) more recent data point to the long-term challenges associated with the behavioral approach.(5,6) Lifestyle changes can be challenging given neural determinants of behavior outside of patients’ awareness; the abnormal body composition of obesity can be maintained by strong homeostatic mechanisms that resist the patient’s efforts to make lifestyle modifications.(7) The use of pharmacotherapy in the pediatric obese population continues to be limited due to the modest benefit of approved medications(8) at the cost of their potential adverse effects.(9) While promising, newer medications targeting severe obesity in adolescents are currently under research and are generally not considered a first-line therapy. Nevertheless, treatment algorithms that include approved medications have been described.(10)
Given the limitations of non-operative interventions in adolescents, metabolic bariatric surgery (MBS) is receiving more attention. Bariatric surgery in adolescents has gained popularity as the safety and sustained efficacy of this approach have become more recognized in recent years.(11) MBS in adults has long been proven to result in long-term weight control and improvement in cardiovascular disease risk factors (e.g. T2D, hypertension).(12,13) Emerging longitudinal data lends further support to the long-term benefits of MBS in adolescence: bariatric surgery in adolescents can result in the loss of 58–73% of excess weight, along with resolution or improvement of significant associated morbidities.(14–18) Despite increasingly positive physician attitudes towards MBS as a viable treatment option,(19) reflected in recent provider guidelines,(20) little consensus exists among physicians regarding referral practices.(21) Many physicians continue to be reluctant to refer adolescents for surgery due to concerns for adverse effects, postoperative complications, long-term outcomes, and the complicated ethics of surgery in adolescence.(22,23) Accordingly, a 2018 study found that less than 0.04% of pediatric patients with severe obesity are treated with MBS yearly in the United States.(24)
Along with physicians’ conflicting opinions regarding the proper management of adolescents struggling with obesity, parental attitudes towards their children’s weight status can also pose substantial barriers to their consideration of all effective treatment options. Parental underestimation of their children’s weight is well-established; parents are, paradoxically, more likely to exhibit this behavior if their children are classified as overweight or obese.(25) There is also a strong history of conflicting parental attitudes and controversy surrounding pediatric bariatric surgery, stemming, in part from their perceived role in the development of obesity in their children. Notably, parents’ favorability towards MBS can depend on their personal beliefs about the etiology of obesity; parents who believe that obesity is outside of their (or their child’s) control (e.g. genetic) are more likely to view bariatric surgery as an appropriate option for their child.(26) It is also important to note that parental views of their child’s obesity can be influenced by their own implicit weight bias.(27)
Such parental misconceptions and bias may represent a significant barrier towards sustained compliance with weight-loss programs and consideration of surgical treatment, especially given the importance of the parental role in managing pediatric obesity. Treatment of obesity in childhood has been shown to be more effective with a family-based approach, when both parents and children are targets of behavioral modification.(4,28) In light of the important role parents play in treating pediatric obesity, understanding parental views of their children’s obesity is essential to promote more effective treatment strategies. We aimed to examine parents’ views of their child’s weight status, ability to identify a need for intervention, and perception of access to lifestyle modification programs and surgical intervention. We hypothesized that parental views on bariatric surgery are primarily affected by personal experiences with bariatric surgery, implicit bias, understanding of the health risks of obesity, and counseling by pediatric providers.
MATERIALS & METHODS
Retrospective Medical Record Review:
With approval from the Institutional Review Board (IRB #13036), a retrospective medical record review of all patients between the ages of 14-17 years old seen in our primary pediatric and subspecialty (gastroenterology, endocrine, pulmonary, and surgery) clinics from January 1, 2017 – April 1, 2018 and identified as having “severe obesity” by their Body Mass Index (BMI) was performed. All patients included in the review were identified from the institutional database by BMI and age. Severe obesity was defined by BMI>35 kg/m2 (20), between the ages of 14 and 17 years old. Patients whose BMI was noted to be recorded incorrectly on manual chart review due to clerical error were excluded. Demographic and clinical data were collected from institutional electronic medical records. Medical and psychiatric comorbidities, sexual maturity rating (Tanner stage), discussion of obesity during clinic visits, and attempted enrollment in a lifestyle modification program, as well as actual program participation, were reviewed. Attempted enrollment was defined as involvement in a program intake process without subsequent enrollment, and program participation was defined as actual participation in program activities. Experiences with the lifestyle program offered at the examined medical center, which was advertised on the hospital website and known to pediatric providers within the institution, as well as similar programs offered at other institutions in the city were noted. Patients’ BMI and medical and psychiatric comorbidities, as defined by the specifically assigned diagnoses in the contemporary active problem list, were used to assess their eligibility for bariatric surgery according to the criteria established by the American Society for Metabolic and Bariatric Surgery.(20)
Telephone Survey:
Following the review of medical records, patients’ parents were asked to participate in a telephone survey designed to assess experiences with and attitudes towards bariatric surgery, understanding of the risks of obesity, and counseling received from pediatric providers. For detailed survey questionnaire administered to parents, see Appendix. The survey was based on questionnaire items described in relevant literature and modified for content and brevity.(19,26) The questionnaire items were piloted on test responders with no healthcare experience, reviewed by the IRB, and revised by the research team for timing and sensitivity. The survey was conducted by the research team members and introduced to the parents using a standardized greeting. A similar (less detailed) introduction was created for the voicemail messages. Certified telephone interpreter service was utilized when the preferred language stated by the respondent was other than English. Parents were asked to provide binary responses to all questions (excluding 9 and 13, which requested numerical answers). The respondents were encouraged to omit questions they found confusing, but a specific protocol of limited clarification was utilized. All protected health information was removed from the database following completion of surveys.
Data Analysis:
Correlation analysis was performed using STATA 13 (StataCorp. 2013. Stata Statistical Software: College Station, TX: StataCorp LP). Associations between nominal variables were examined using Pearson’s Chi-Square tests. Continuous variables were assessed using Student t-test. Statistically significant correlations were determined by p<0.05.
RESULTS
192 patients aged 14-17 years old were identified and included in the study. The majority of patients (61.9%) were female. Average BMI of the patients was 40.5 kg/m2 and similar between survey responders (40.6 kg/m2) and non-responders (40.3 kg/m2) (Table 1). The overall response rate of the telephone survey was 37.5% (72/192). Of all 192 parents, 53.6% (103) were unable to be reached after three attempts in a two-week period and 8.9% (17) refused to participate. Most parents who participated in the survey, 88.9% (64/72), reported being concerned about their child’s weight. Despite that concern, only 69.4% (50/72) of parents believed their child’s weight was a current health hazard. In fact, almost a quarter of the parents surveyed, 23.6% (17/72), did not consider their child’s weight status to be dangerous for their future health. When asked about the amount of weight loss which would be considered a success, the mean was 63 ± 47.5 lbs and was significantly higher among the parents of adolescents eligible for surgery at the time of the survey (80.1 ± 53.2 lbs) than those who were not (39.9 ± 24.4 lbs), p = 0.01 (Table 2).
Table 1.
Demographic data gathered from review of 192 adolescents’ medical records (72 survey responders and 120 non-responders). Data are presented as % (no.), unless otherwise indicated.
| Characteristic | All (192) | Responders (72) | Non-Responders (120) | p | |
|---|---|---|---|---|---|
| Body Mass Index (mean ± SD) | 40.5 ± 5.3 | 40.6 ± 5.7 | 40.3 ± 5.0 | 0.71 | |
| Body Mass Index > 40 | 42.7 (82) | 40.2 (33) | 59.8 (49) | 0.55 | |
| COMORBIDITIES | Obstructive sleep apnea | 8.9 (17) | 8.3 (6) | 9.2 (11) | 1 |
| Diabetes mellitus | 6.8 (13) | 5.5 (4) | 7.5 (9) | 0.77 | |
| Pre-diabetes mellitus | 9.9 (19) | 9.7 (7) | 10 (12) | 1 | |
| Non-alcoholic fatty liver disease | 2.6 (5) | 2.8 (2) | 2.5 (3) | 1 | |
| Hypertension | 12.5 (24) | 6.9 (5) | 15.8 (19) | 0.08 | |
| Gastroesophageal reflux disease | 9.4 (18) | 16.7 (12) | 5 (6) | 1 | |
| Depression | 12 (23) | 11.1 (8) | 12.5 (15) | 0.82 | |
| Anxiety | 15.1 (29) | 15.3 (11) | 15 (18) | 1 | |
| COUNSELING | Counseled on child’s obesity | 60.9 (117) | 65.3 (47) | 58.3 (70) | 0.36 |
| Counseled on lifestyle programs | 24.5 (47) | 30.6 (22) | 20.8 (25) | 0.17 | |
| Enrolled child in lifestyle program | 3.1 (6) | 5.6 (4) | 1.7 (2) | 0.20 | |
| Child eligible for bariatric surgery | 59.4 (114) | 58.3 (42) | 60 (72) | 0.88 | |
Table 2.
Responses of 72 parents (42 with a child eligible for surgery and 30 with a child ineligible for surgery) to telephone surveys. Data are presented as % (no.), unless otherwise indicated. * denotes statistical significance (p < 0.05).
| Response | All (72) | Child Eligible (42) | Child Ineligible (30) | p |
|---|---|---|---|---|
| Body Mass Index (mean ± SD) | 40.6 ± 5.7 | 43.5 ± 6.1 | 36.8 ± 1.2 | <0.01* |
| Consider child’s weight a health hazard | 69.4 (50) | 69.0 (29) | 70.0 (21) | 1 |
| Consider child’s weight a future health hazard | 76.3 (55) | 76.2 (32) | 76.7 (23) | 1 |
| Counseled on pharmacological therapy | 8.3 (6) | 9.5 (4) | 6.7 (2) | 1 |
| Would consider bariatric surgery for their child | 41.7 (30) | 45.2 (19) | 36.7 (11) | 0.63 |
| Appropriate age to consider surgery for child (mean ± SD) | 19.9 ± 5.9 | 19.3 ± 6.6 | 20.9 ± 4.5 | 0.37 |
| Amount of weight loss that would mean success (lbs) | 63 ± 47.5 | 80.1 ± 53.2 | 39.9 ± 24.4 | <0.01* |
| Had prior personal exposure to surgery | 72.2 (52) | 73.8 (31) | 70 (21) | 0.79 |
According to available documentation, 60.9% (117/192) of the patients’ families received counseling regarding the patients’ obese status in their clinic visit(s) (i.e. any documented mention of the patient’s excessive weight and the need for weight loss). The chart review indicated that only 24.5% (47/192) of eligible families received counseling on lifestyle programs during their visit(s) (Table 1). Parents of only 71.4% of patients who received outpatient weight loss program counseling had an accurate recollection of that event. Interestingly, of those parents whose children’s charts did not include such counseling, 44% stated they had received counseling (Figure 1). Overall, a small minority of all parents successfully enrolled their children in a program (3.1%), (Table 1) including those who stated that they have not received education about such a program (1/6, 16.7%). Even after being approached about it by the pediatric providers, that number was only 12.8%. In fact, most (84.6%) of the parents who correctly remembered receiving counseling on lifestyle programs did not enter their child in a program.
Figure 1.
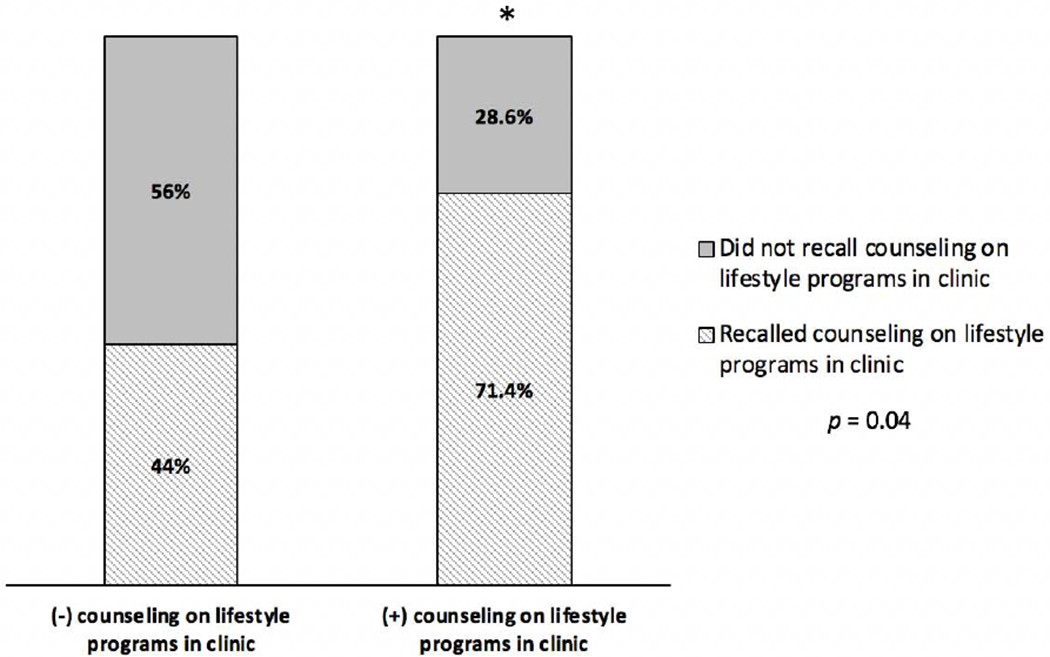
Parents’ perceptions of counseling compared to the actual counseling received, as documented. * denotes statistical significance (p < 0.05).
Slightly more than half of the patients, 59.4% (114/192), were eligible for consideration for bariatric surgery based on their BMI and comorbidities.(20) Only 3 of these 114 eligible patients (2.6%) had explicit documentation of counseling on surgical options in any of the clinic notes examined. Parents who identified their child’s weight as a future health problem were more likely to consider MBS as a viable option, but only 51.9% (27/55) of parents fell into this category (Figure 2A).
Figure 2.
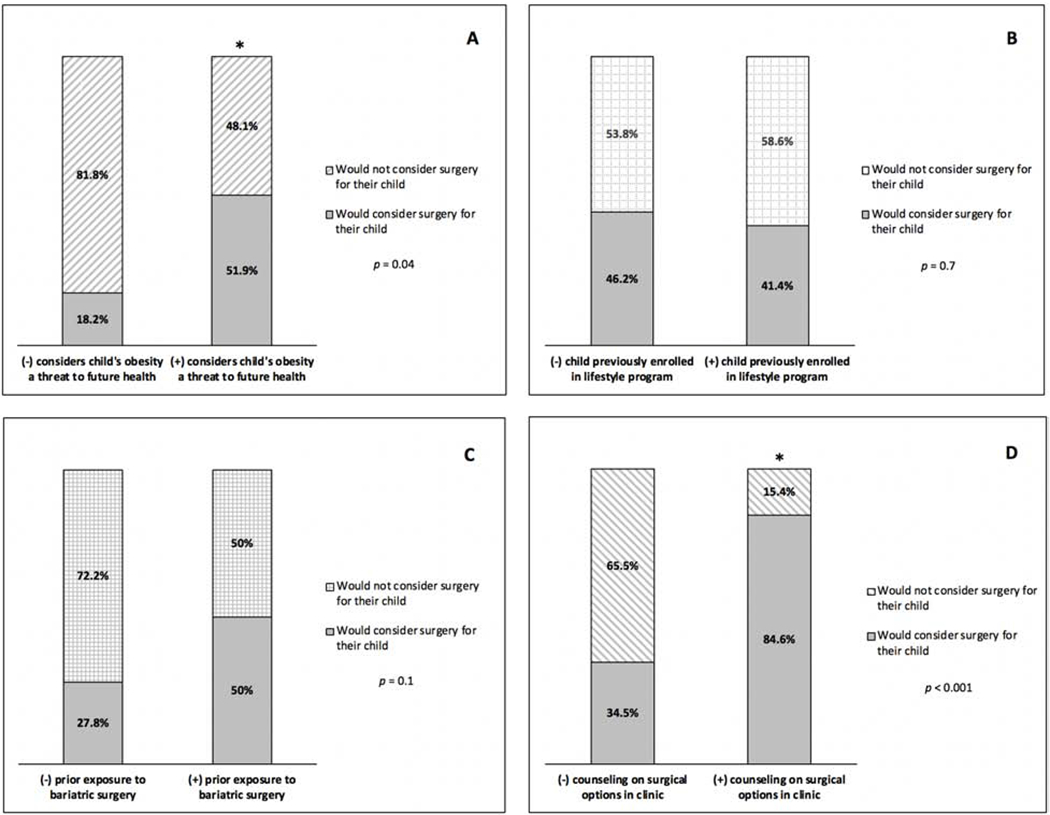
Factors influencing parents’ willingness to consider bariatric surgery for their child with severe obesity. * denotes statistical significance (p < 0.05).
When asked to consider the minimum age to undergo surgery, a majority of responders, (84.4%) believed it was inappropriate to consider surgical options before 18 years of age. The response did not differ between parents who correctly remembered counseling (mean ± SD: 19.1 ± 6.8) and those who did not receive counseling (20.2 ± 5.8) (p=0.64).
Neither prior personal exposure to weight loss surgery nor previous enrollment of their child in a lifestyle program made parents more likely to consider MBS for their child (p=0.10 and 0.70, respectively) (Figures 2B–C). However, most of the parents (84.6%) who explicitly reported that they were counseled by their pediatric providers about bariatric surgery would consider it as an option, compared to only 34.5% of the parents who did not receive counseling (p<0.001) (Figure 2D).
DISCUSSION
Provider Referrals to Lifestyle Programs
Only a minority of providers (24.5%) approached eligible patients and parents about the adolescent weight loss program offered at our institution. The program involved a 10 week intensive curriculum of exercise and nutritional counseling, followed by a scheduled series of reassessments and reinforcements by the trained providers. A dedicated adolescent bariatric program was not present at our institution at the time of this data collection. However, bariatric surgical centers for adolescents are available in close proximity in this metropolitan area. It is possible that the knowledge of our institution’s program was not as widespread as we assumed, which could contribute to our finding. However, several patients in our sample attended programs at other institutions, but their parents reported similar results to the patients who participated in the institutional program. Similar trends indicating pediatric providers’ reticence to refer patients to weight loss programs have previously been reported in the literature, suggesting a need for both better physician awareness of the positives of lifestyle programs and improvement of these programs.(29,30) Such trends also indicate that better understanding of the disease itself and realistic expectations of non-operative management are needed.
Bariatric Surgery: Parental Opinions vs. Reality
The short-term benefits of bariatric surgery in pediatric patients with severe obesity have been well-established, and emerging long-term data appear encouraging.(16) Adolescents with severe obesity who undergo weight loss surgery demonstrate long-term, sustained weight control along with resolution of major comorbidities.(14) Indeed, several studies have reported better bariatric surgery outcomes in adolescents than in adults – the positive health and psychosocial effects of MBS diminish after adolescence, when patients’ obesity and comorbidities have progressed. (16,31,32) Based on these findings, MBS should be seriously considered as a therapeutic option in younger patients struggling with severe obesity.
We assessed parental perceptions of the need for earlier surgical intervention. Only 65.3% of parents provided an opinion on the minimum age for consideration of bariatric surgery, with the median being 18 years old. However, the wide range of responses (“now”–50 years old) suggest an arbitrary approach. It stands to reason that parents may subconsciously consider the legal age of consent for the procedure a fitting cut-off, as that would shift some of the burden of the decision from the parents to the patients themselves. Earlier and more thorough counseling regarding patients’ lifestyle and surgical therapeutic options could result in a shift in parents’ mindsets regarding the appropriateness of and proper timing for pursuing surgical options for their children. Likewise, while statistically significant, the wide range of answers provided for the perceived “successful” weight loss by the parents (8 – 224 lbs) also suggests an arbitrary approach. While this may be related to higher BMI in the group eligible for surgery, it is difficult to assign a definitive explanation for these findings without additional data.
The Influence of Providers on Parents’ Decisions
The main factor influencing parents’ willingness to consider surgery for their child was whether or not they received counseling by their pediatric provider. Only a third of parents (34.5%) who did not receive provider counseling would consider bariatric surgery for their child, compared to 84.6% of parents who were counseled. This finding emphasizes the significant role provider counseling plays in parents’ decisions regarding their children’s health care and in the treatment of obesity in particular. Interestingly, such counseling did not significantly affect the perceived minimum age for consideration of bariatric surgery. It would be important to verify if the pediatric providers themselves suggested a minimum age. The concept of pediatric provider counseling as a major force behind parental adherence is also evident in other major health issues in the United States, such as parents’ decisions on vaccinations. Studies demonstrate that communicating with the child’s physician is the most important factor in parents’ decision-making on vaccinations. A strong recommendation by the provider has been shown to successfully encourage parents to vaccinate their children (33); conversely, “absent or weak recommendations from health care providers are primary drivers of poor vaccine uptake.”(34) Recently, a provider recommendation was reported to be the strongest variable influencing the rise of human papillomavirus vaccination series in adolescent boys.(33)
Given the substantial influence that provider counseling can have on how parents handle major decisions about their children’s health care, it is essential to consider earlier provider recommendations in the treatment of childhood obesity. In order to encourage parents to approve vaccinations for their children, the Center for Disease Control (CDC) routinely publishes guidelines to aid physicians in having these important conversations.(35) Similar recommendations for providers published by the CDC and American Academy of Pediatrics (AAP) would aid physicians in initiating early, thorough discussions about the range of therapeutic options for their children, including lifestyle programs and bariatric surgery.
Limitations
The primary limitations of our study are the retrospective nature of chart review, limited sample size due to the specific age range included in the study design, the recall bias inherent to surveys, and the relatively low response rate of our survey. In addition, some patients included in our study were only seen in a subspecialty clinic at our Medical Center. Given the lack of reliable access to these patients’ external medical records, it is possible that they received counseling by their primary providers not accounted for in our study. We recognize that using the research team members to administer interviews holds a potential for bias, thus we constrained the team to a specific greeting, content, and order of questions. In addition, the survey was designed to direct the responses in a binary fashion, further minimizing the potential for interpretation bias. This is a small scale exploratory study meant to assess the parental willingness to participate and provide a glimpse into their attitudes towards surgical treatment of obesity in adolescent. Despite a lack of formal validation process, we were encouraged by our high correlation findings that our results are, indeed, objective. We recognize that a formal validation of a more expanded and granular survey would be required to better understand the parental motivations and juxtapose them with pediatric provider perceptions and attitudes. The follow-up study design would involve a validated, funneled questionnaire, administered by uninvolved operators with an assessment of inter-rater reliability.
CONCLUSIONS
Given the well-established importance of parental involvement in the process of addressing obesity in adolescents, our study suggests that pediatric providers: a) counsel patients regarding available weight loss programs earlier, to maximize the benefits of early intervention, and more frequently and b) specifically introduce counseling about bariatric surgery earlier in their conversations with parents. While our exploratory study is not meant to be fully generalizable, we propose a consideration of earlier involvement of pediatric surgeons in these discussions, allowing the surgeons to work as a part of the counseling team. This modification could help ensure that patients and their families take full advantage of multidisciplinary weight management programs, in which primary providers, lifestyle program specialists, and surgeons participate in coordinated discussions with patients and their parents. Finally, more up-to-date education for primary providers on surgical management of severe obesity in adolescence could be accomplished through continuing medical education lecture materials at conferences and grand rounds.
Supplementary Material
HIGHLIGHTS.
Only half of parents concerned for their child’s future health would consider MBS.
Most parents who would consider MBS would wait until their child was over age 18.
Exposure to MBS does not make parents more likely to consider MBS for their child.
Provider counseling significantly increases parents’ likelihood to consider MBS.
Acknowledgments:
The authors would like to acknowledge the contributions of Hong Chang, Ph.D., and Debra Lerner, M.S., Ph.D. (Tufts CTSI UL1TR002544) for their assistance in the statistical analysis of data and survey methodology and Walter J. Chwals, M.D., for his assistance, expertise, and critical review during the preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
The authors report no conflicts of interest regarding the content of this article.
REFERENCES
- 1.Kelly AS, Barlow SE, Rao G, et al. Severe Obesity in Children and Adolescents: Identification, Associated Health Risks, and Treatment Approaches. Circ 2013;128(15):1689–1712. [DOI] [PubMed] [Google Scholar]
- 2.Karnik S, Kanekar A. Childhood obesity: a global public health crisis. Int J Prev Med 2012;3(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Khudairy L, Loveman E, Colquitt JL, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev 2017;6:CD012691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA 1990; 264:2519–2523. [PubMed] [Google Scholar]
- 5.Reinehr T, Widhalm K, l’Allemand D, et al. Two-year follow-up in 21,784 overweight children and adolescents with lifestyle intervention. Obesity (Silver Spring) 2009; 17:1196–1199. [DOI] [PubMed] [Google Scholar]
- 6.Savoye M, Nowicka P, Shaw M, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. J Pediatr 2011;127:402–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berthoud HR, Münzberg H, Morrison CD. Blaming the Brain for Obesity: Integration of Hedonic and Homeostatic Mechanisms. Gastroenterology 2017;152(7):1728–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherafat-Kazemzadeh R, Yanovski SZ, Yanovski JA. Pharmacotherapy for childhood obesity: present and future prospects. Int J Obes (Lond) 2012;37(1): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev 2016;11:CD012436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srivastava G, Fox CK, Kelly AS, Jastreboff AM, Browne AF, Browne NT, et al. Clinical Considerations Regarding the Use of Obesity Pharmacotherapy in Adolescents with Obesity. Obesity (Silver Spring) 2019;27:190–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelleher D, Merrill CT, Cottrell LT, Nadler EP, Burd R. Recent National Trends in the Use of Adolescent Inpatient Bariatric Surgery 2000 Through 2009. JAMA Pediatr 2012;167(2):1–7. [DOI] [PubMed] [Google Scholar]
- 12.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA 2004;292(14):1724–1737. [DOI] [PubMed] [Google Scholar]
- 13.Sjostrom CD, Peltonen M, Wedel H, Sjostrom L. Differentiated long-term effects of intentional weight loss on diabetes and hypertension. Hypertension 2000;36:20–25. [DOI] [PubMed] [Google Scholar]
- 14.Stefater MA, Inge TH. Bariatric surgery for adolescents with type 2 diabetes: an emerging therapeutic strategy. Curr Diab Rep 2017;17:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inge TH, Jenkins TM, Xanthakos SA, et al. Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): a prospective follow-up analysis. Lancet Diabetes Endocrinol 2017;5:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inge TH, Courcoulas AP, Jenkins TM, et al. Five-Year Outcomes of Gastric Bypass in Adolescents as Compared with Adults. N Engl J Med 2019;380(22):2136–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inge TH, Courcoulas AP, Jenkins TM, Michalsky MP, Helmrath MA, Brandt ML, et al. Weight Loss and Health Status 3 Years after Bariatric Surgery in Adolescents. N Engl J Med 2016;374:113–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olbers T, Beamish AJ, Gronowitz E, Flodmark C-E, Dahlgren J, Bruze G, et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol 2017;5:174–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanguri P, Lanning D, Wickham EP, Anbazhagan A, Bean MK. Pediatric health care provider perceptions of weight loss surgery in adolescents. Clin Pediatr (Phila) 2014;53:60–65. [DOI] [PubMed] [Google Scholar]
- 20.Pratt JS, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis 2018;14(7):882–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woolford SJ, Clark SJ, Gebremariam A, Davis MM, Freed GL. To cut or not to cut: physicians’ perspectives on referring adolescents for bariatric surgery. Obes Surg 2010;20:937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beamish AJ, Reinehr T. Should bariatric surgery be performed in adolescents?. Eur J Endocrinol 2017;176:D1–D15. [DOI] [PubMed] [Google Scholar]
- 23.Iqbal CW, Kumar S, Iqbal AD, Ishitani MB. Perspectives on pediatric bariatric surgery: Identifying barriers to referral. Surg Obes Relat Dis 2009;5(1): 88–93. [DOI] [PubMed] [Google Scholar]
- 24.Griggs CL, Perez NP, Goldstone RN, et al. National Trends in the Use of Metabolic and Bariatric Surgery Among Pediatric Patients with Severe Obesity. JAMA Pediatr 2018;172(12):1191–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Etelson D, Brand DA, Patrick PA, Shirali A. Childhood Obesity: Do Parents Recognize This Health Risk?. Obes Res 2003;11:1362–1368. [DOI] [PubMed] [Google Scholar]
- 26.van Geelen SM, Bolt IL, van der Baan-Slootweg OH, van Summeren MJ. The controversy over pediatric bariatric surgery: an explorative study on attitudes and normative beliefs of specialists, parents, and adolescents with obesity. J Bioeth Inq 2013;10:227–237. [DOI] [PubMed] [Google Scholar]
- 27.Lydecker JA, O’Brien E & Grilo CM Parents have both implicit and explicit biases children with obesity. J Behav Med 2018;41:784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr 1998;67(6):1130–1135. [DOI] [PubMed] [Google Scholar]
- 29.Woolford SJ, Clark SJ, Gebremariam A, Davis MM, Freed GL. Physicians’ Perspectives on Referring Obese Adolescents to Pediatric Multidisciplinary Weight Management Programs. Clin Pediatr 2010;49(9), 871–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imoisili OE, Goodman AB, Dooyerna CA, Harrison MR, Belay B, Park S. Screening and Referral for Childhood Obesity: Adherence to the U.S. Preventive Services Task Force Recommendation. Am J Prev Med 2019;56(2):179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Inge TH, Xanthakos SA, Zeller MH. Bariatric surgery for pediatric extreme obesity: now or later. Int J Obes (Lond) 2007;31:1–14. [DOI] [PubMed] [Google Scholar]
- 32.Khidir N, El-Matbouly MA, Sargsyan D, Al-Kuwari M, Bashah M, Gagner M. Five-year outcomes of laparoscopic sleeve gastrectomy: a comparison between adults and adolescents. Obes Surg 2018:28:2040–2045. [DOI] [PubMed] [Google Scholar]
- 33.Kao CM, Schneyer RJ, Bocchini JA. Child and adolescent immunizations: selected review of recent U.S. recommendations and literature. Curr Opin Pediatr 2014:26(3):383–395. [DOI] [PubMed] [Google Scholar]
- 34.Ventola CL. Immunization in the United States: Recommendations, Barriers, and Measures to Improve Compliance: Part 1: Childhood Vaccinations. Pharm Ther 2016;41(7):426–436. [PMC free article] [PubMed] [Google Scholar]
- 35.Provider Resources for Vaccine Conversations with Parents. Centers for Disease Control and Prevention, 2016. (Accessed June 26, 2019 at https://www.cdc.gov/vaccines/hcp/conversations/index.html.)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


