Abstract
SARS-CoV-2 is a novel beta-coronavirus causing over 200.000 lethal cases within six months of first infecting humans. SARS-CoV-2 causes COVID-19, a form of severe acute respiratory syndrome (SARS). COVID-19 is characterized by two phases: the first resembles the flu with pneumonia, but after about seven or eight days the disease suddenly worsens to a sepsis-like syndrome. It is difficult to explain this virus-immune-pathology sequence from virology or immunology only. This paper hypothesizes that host-produced anti-spike protein antibodies are responsible for immune-induced viral dissemination. Subsequently, systemic distribution of virus-antibodies complexes activates the immune pathology observed in severe COVID-19.
This hypothesis may be counterintuitive to immunologist that consider many anti-spike antibodies to be virus-neutralizing antibodies. Although anti-spike antibodies may hinder infection of epithelial cells, antibody binding to the spike protein may facilitate virus infection of myeloid leukocytes. If myeloid leukocytes reenter the circulation, they could spread the virus from a locoregional infection to a systemic disease. Disseminated virus in combination with antibodies results in dispersed virus-antibody complexes that overstimulate the immune system.
The hypothesis aligns with the sequences of virus, immune and pathological events in COVID-19. The delay in onset from both syndromes results from an immune system still naïve to the non-cross-reactive spike protein. Details of this hypothesis are in concordance with many clinical characteristics of COVID-19, including its predominant lethality for the elderly, and the mostly asymptomatic course of disease in children. It predicts putative detrimental effects of vaccines that induce virus-neutralizing antibodies against the spike protein, as has been shown for other coronaviruses.
This hypothesis has consequences for treatment of patients, evaluation of personal and herd immunity and vaccine development. In patients, cellular immunity should be stimulated. Neutralizing antibodies might not be indicative for immunity. Vaccines should aim to stimulate cellular immunity COVID-19 and/or stimulate humoral immunity against viral proteins except for the immunodominant spike protein.
Introduction
SARS-hCoV-2 (SARS-2) is a zoonotic beta-coronavirus that emerged from bats, probably through an intermediate host, and should now be considered as a serious human pathogen [1]. Human beta-coronaviruses consists of three lineages. The A-lineage contains HCoV-OC43 and HCoV-HKU1, two causative agents of the common cold. The C-lineage contains MERS-CoV, a virus of zoonotic origin that caused a severe disease in humans with 800 fatalities in 2500 cases in Saudi Arabia from 2012. SARS-2 belongs to the B-lineage, and is most related to SARS-CoV, the causative agent for SARS. SARS caused 800 fatalities in 8000 cases in South-China in 2002–2003.
SARS-2 is a rapidly spreading pandemic virus infecting over 3.4 million people, causing a novel disease (COVID-19). COVID-19 has a mortality of over 240 thousand people worldwide within half a year of infecting the first human [2]. Thus the disease is rightfully considered a severe pandemic by the WHO. The pathogenesis of COVID-19, and especially its sudden immune-mediated disease aggravation, is only partially understood. Improved understanding of the mechanisms might help to improve medical intervention to achieve a relevant reduction in mortality and morbidity per case.
From a clinical perspective COVID-19 appears to be the sequence of two syndromes. After the incubation period, a serious pneumonia-like disease might develop. In a later stage, about 7–8 days after onset of the disease, some patients suffer from a serious local and systemic immune response, e.g. a form of sepsis. Physicians have great difficulties in predicting and controlling disease progression. The clinical deterioration is often fatal and has strong an immunological component [3]. However it is unclear why and how suddenly a severe systemic immune activation would be triggered [4].
Simple virologic and immunologic mechanisms of disease fail to explain the delayed progression of disease and other observations, including the sequence of events, epidemiologic data, observed differences in disease severity and immunological parameters. Based on integration of virologic and immunologic mechanisms, this paper proposes an integrated model for a virus-immune-pathology sequence.
Virology shows that coronaviruses have four essential structural proteins: the spike (S), the nucleocapsid (N), the membrane (M), and the envelope (E) protein. Coronaviruses infect new cells after binding of their spike protein to a target cell. The spike protein is at the outside of the virus, dominant for antibody responses [5]. Many antibodies against the spike protein are neutralizing antibodies which prevent virus infection of epithelial cells. These neutralizing antibodies are considered crucial in immunological protection against SARS-2 [6].
The spike protein is the site of major antigenic variation and has low amino acid sequence homology between coronaviruses. From an immunological and evolutionary perspective, cross-reactivity between epitopes of the spike protein of different coronaviruses is extremely unlikely. Thus each host should be regarded as immunologically naïve with respect to neutralizing antibodies against the spike protein. Other structural proteins and the RNA directed RNA polymerase are more likely to yield cross-reactive immune responses resulting from other coronavirus infections [7]. The appearance of antibodies is delayed compared to the onset of first clinical symptoms [8]. Its timing seems to coincidence with the extravagation of the disease. Merging these immunological events with known virological mechanisms in the sequence of the pathology gave rise to the hypothesis of this paper.
Outline of the hypothesis
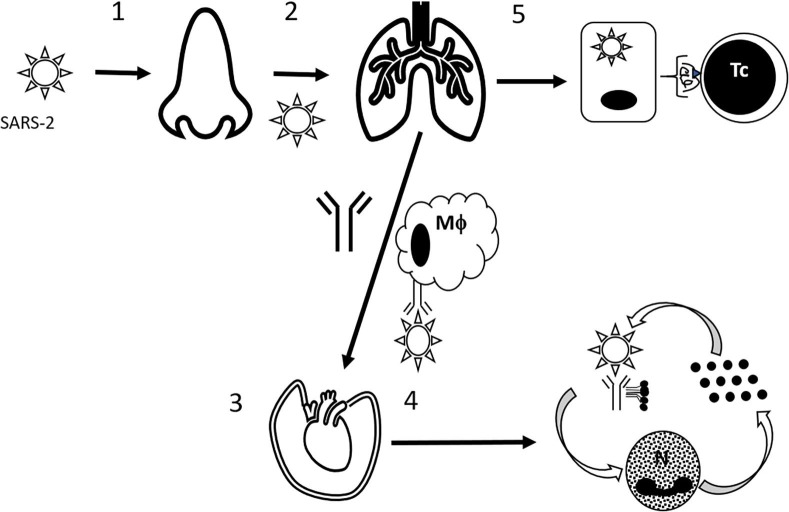
SARS-CoV-2 probably has an easy and efficient entry in the human body, like in nasal epithelial cells [10] as has been suggested by its very high reproduction number, i.e. R0 between 4.7 and 6.6 [9]. During this asymptomatic phase, local virus production will yield increase intranasal virus titres. After some days, the virus may spread regionally to the lung causing the symptomatic pneumonia (see Fig. 1 ).
Fig. 1.
Hypothesis of virus-immune pathology of COVID-19. Sequence of events. 1. SARS-CoV-2 infects nasal epithelial cells to produce virus titres. 2. The virus spreads locoregional to infect the lungs. 3. When antivirus antibodies are present, antibody-dependent infected myeloid leukocytes could transport the virus through the lymph and blood circulation, resulting in a disseminated infection. 4. Disseminated virus-antibody complexes results in amplification of activation cycles of the complement system, innate immune cells and cytokines resulting in systemic immune pathogenesis. Because of high virus titres in the lungs, this will also result in sever acute respiratory syndrome. 5. The alternative route would be effective clearance of the virus by cytotoxic T lymphocytes (and/or antibodies devoid of the capability to induce antibody-dependent infection).
When the host has generated SARS-CoV-2 spike-protein-specific IgG antibodies, FcγRII-mediated antibody-dependent infection of human macrophages may occur. This antibody-dependent infection has been described for the spike protein of similar beta-coronaviruses, i.e. SARS-CoV-1 [11], [12] and MERS [13]. The FcγRII receptor is widely expressed on myeloid leukocytes. Infected myeloid cells might return to circulation in the peripheral blood and transport the virus to distant organs of the host. Thus, antibodies directed against the SARS-2 spike protein could cause viremia and disseminate virus particles through the whole host.
In various organs of the body some cells express the ACE2 receptor [10], where the virus might replicate after transportation by myeloid immune cells. At the dispersed locations throughout the body, antivirus-virus immune complexes could activate the innate immune system by compliment activation, binding to platelets, or by binding to myeloid immune cells. This would cause disseminated inflammation and thrombosis, as a systemic disease with a major impact on the lungs, i.e. the main site of virus replication.
Evaluation of the hypothesis
Integrating virology and immunology allows the explanation of a sudden unexpected increase in disease severity of COVID-19. A central role for neutralizing antibodies has been suggested.
Patients with agammaglobulinemia lack B lymphocytes and antibodies, and they are vulnerable to many infections that could be resolved by antibodies. In contrast to the expectations yielded by their immunodeficiency, these patients have only a mild form of COVID-19, indicating the detrimental role of antibodies in COVID-19 [14]. Studies with a feline coronavirus causing infectious peritonitis, showed decreased survival after vaccination related to antibody-mediated enhancement of infection [22].
Immune cross reactivity
The spike protein has very limited amino acid homology between coronaviruses [15], making cross-reactivity for anti-spike antibodies between viruses highly unlikely. In serological assays cross-reactivity between anti-SARS-2 and other corona-virus antibodies shows up. Most likely this cross-reactivity could be attributed to other virus proteins, that have an amino acid homology that is high enough to allow immunological cross reactivity. This could be the viral RNA polymerase or structural proteins like the nucleocapsid, the membrane protein and the envelope protein. Although these antibodies may not directly neutralize the virus, they may synergize with the innate immune to eliminate viral particles.
Many beta-coronaviruses cause frequent infections like the common cold, and especially in children [16], [17]. Research on SARS infection, showed that T-cell immunity remained for at least ten years post infection, while antibodies are lost within two years [18], [19]. If some antibodies and cytotoxic T lymphocytes against other beta-coronaviruses might cross react against SARS-2, these would not include immune responses against the spike protein. Such non-neutralizing antibodies might offer some protection in children and others that have recently encountered a common cold coronavirus.
Cellular immunity
Neutralizing IgG antibodies can prevent virus infection of epithelial cells, by blocking the spike protein in its entry though the ACE2 receptor. But anti-spike antibodies might also be the mediators of antibody-dependent infections of myeloid leukocytes. In a study, neutralizing antibody titres correlated negatively with blood lymphocyte counts and positively with blood CRP levels in COVID-19 patients. This suggests that the humoral response might play an important role when cellular response was dysfunction or impaired [20]. It yields the unexpected conclusion that stimulating cellular immunity might avoid immune overstimulation.
Virus infections cause antibody responses and cytotoxic T lymphocytes. Both immune responses have been reported to be important for virus clearance of the related SARS-CoV-1. Cytotoxic T lymphocytes can eliminate infected cells by recognizing viral peptides in MHC I (HLA) context. Killing the cells that produce new virus particles would effectively avoiding virus release. Elderly people have decreased cellular immunity [21]. Most likely their immune responses shift towards antibody-mediated immunity to eliminate virus particles. The proposed hypothesis would predict that elderly would suffer more often from the lethal form of COVID-19.
Consequences of the hypothesis
This hypothesis considers virus neutralizing antibodies to be not beneficial but even detrimental for COVID-19 patients. Such a view has major consequences for the strategy against COVID-19 regarding therapy of patients, evaluation of personal and herd immunity, and for the development of SARS-2 vaccines.
Firstly, viral diseases are cured by antigen-specific immunity of the patients. Because of the dangerous side effects of neutralizing antibodies, stimulating cellular immunity seems like a wise strategy. In elderly and other patients with diminished immune functions cellular immunity might be stimulated using vitamin D or low doses of interleukin-2 (IL-2). Restoring normal levels of vitamin D could be crucial for the elderly to restored their immune functions [23], [24]. Indeed, vitamin D3 supplementation has been advised for respiratory RNA virus infections [25], [26]. Cellular immunity could also be boosted by subcutaneous application of low dose IL-2 in the early stages of disease, as has been shown for other viruses like HIV [27], and the DNA and RNA viruses causing hepatitis B and C, respectively [28].
Secondly, antibodies after a COVID-19 infection might be no more than an epiphenomenon that might occur in the development of antivirus immunity. The SARS-2 virus would be eliminated by successful cellular immune responses. Antibody titres might be associated more with disease severity than with immunological efficacy. Thus patients that recovered a low or asymptomatic COVID-19 infection might have low or even no neutralizing antibodies [29]. This would be a contraindication for the the approach to measure antibodies to indicate personal or herd immunity against SARS-2. The WHO correctly stated that “no study has evaluated whether the presence of antibodies to SARS-CoV-2 confers immunity to subsequent infection by this virus in humans” [30].”
Lastly, this hypothesis implies rethinking our vaccine strategy against the SARS-2 virus. Default vaccination wisdom says: the spike, nucleocapsid and membrane protein are most abundant in SARS [31] and akin SARS-2 and thus should be incorporated in the vaccine. Injecting inactivated viruses or viral proteins would mainly trigger antibody responses. Since antibodies against the viral spike protein might be detrimental, immune responses might be triggered to other viral proteins. The nucleocapsid [32] and the membrane protein are also immunodominant for antibodies, and these could be a good candidate for a vaccine.
Alternatively, vaccination could focus at cellular immunity, as has been done against other coronaviruses, like SARS [33]. Cellular immunity builds on antigen processing in the context of MHC class I and II. This facilitated by protein production within an infected cell, but some cross-priming of dendritic cells may occur. In vaccine technology, this would imply strategies that allow vaccine RNA transcription in the host. That would imply strategies like attenuated viruses or genetically modified vaccines, i.e. conditionally infectious vectors, DNA or RNA vaccines. A cytotoxic T lymphocyte response could be induced by structural or non-structural virus proteins, as has been shown in the immunity to SARS [34], [19].
Grants
This research has not been supported by any grants.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zhou P., Yang X.-L., Wang X.-G. A pneumonia outbreak associated with a new coronavirus of probably bat origen. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. https://www.nature.com/articles/s41586-020-2012-7.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymus COVID-19 coronavirus pandemic. Assessed 02-05-2012. https://www.worldometers.info/coronavirus/.
- 3.C. Huang, Y Wang, X Li et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (10223) (2020), p. 497–06. https://reader.elsevier.com/reader/sd/pii/S0140673620301835. [DOI] [PMC free article] [PubMed]
- 4.Giamarellos-Bourboulis E.J., Netea M.G., Rovina N. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;27:1–9. doi: 10.1016/j.chom.2020.04.009. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7172841/pdf/main.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallagher T.M., Buchmeier M.J. Coronavirus spike proteins in viral entry and pathogenesis. Virology. 2001;279:371–374. doi: 10.1006/viro.2000.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou G., Zhao Q. Perspectives on therapeutic neutralizing antibodies against the Novel Coronavirus SARS-CoV-2. Int J Biol Sci. 2020;16(10):1718–1723. doi: 10.7150/ijbs.45123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7098029/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharmin R., Islam A.B. A highly conserved WDYPKCDRA epitope in the RNA directed RNA polymerase of human coronaviruses can be used as epitope-based universal vaccine design. BMC Bioinf. 2014;15:161–170. doi: 10.1186/1471-2105-15-161. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/24884408/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo L, Ren L, Yang S, et al. Profiling early humoral response to diagnose novel Coronavirus Disease (COVID-19). Clin Inf Dis. (2020). In press. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184472/pdf/ciaa310.pdf. [DOI] [PMC free article] [PubMed]
- 9.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. The novel Coronavirus, 2019-nCoV, is highly contagious and more infectious than initially estimated. MedRXIV. (2020). Preprint. https://www.medrxiv.org/content/10.1101/2020.02.07.20021154v1.
- 10.Sungnak W, Huang N, Bécavin C et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. (2020). In press. https://www.nature.com/articles/s41591-020-0868-6.pdf. [DOI] [PMC free article] [PubMed]
- 11.Yip M.S., Leung N.H.L., Cheung C.Y. Antibody-dependent infection of human macrophages by severe acute respiratory syndrome coronavirus. J Virol. 2014;11:82–92. doi: 10.1186/1743-422X-11-82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4018502/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang S.F., Tseng S.P., Yen C.H. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun. 2014;451(20):208–214. doi: 10.1016/j.bbrc.2014.07.090. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/25073113/L [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wan Y., Shang J., Sun S. Molecular mechanism for antibody-dependent enhancement of coronavirus entry. J Virol. 2020;94(5) doi: 10.1128/JVI.02015-19. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinti I., Lougaris V., Milito C. A possible role for B cells in COVID-19?: Lesson from patients with Agammaglobulinemia. J Allergy Clin Immunol. 2020 doi: 10.1016/j.jaci.2020.04.013. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7175894/pdf/main.pdf In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srinivasan S., Cui H., Gao Z. Structural Genomics of SARS-CoV-2 Indicates Evolutionary Conserved Functional Regions of Viral Proteins. Viruses. 2020;12(4):360–376. doi: 10.3390/v12040360. https://www.mdpi.com/1999-4915/12/4/360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corman V.M., Muth D., Niemeyer D., Drosten C. Hosts and sources of endemic human coronaviruses. Adv Virus Res. 2018;100:163–188. doi: 10.1016/bs.aivir.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monto A.S., DeJonge P., Callear A.P. Coronavirus occurrence and transmission over 8 years in the HIVE cohort of households in Michigan. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184402/ In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Channappanavar R., Zhao J., Perlman S. T cell-mediated immune response to respiratory coronaviruses. Immunol Res. 2014;59(1):118–128. doi: 10.1007/s12026-014-8534-z. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4125530/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu W.J., Zhao M., Liu K. T-cell immunity of SARS-CoV: Implications for vaccine development against MERS-CoV. Antiviral Res. 2017;137:82–92. doi: 10.1016/j.antiviral.2016.11.006. https://www.ncbi.nlm.nih.gov/pubmed/27840203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tan C., Huang Y., Shi F. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 2020 doi: 10.1002/jmv.25871. https://onlinelibrary.wiley.com/doi/full/10.1002/jmv.25871 In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ventura M.T., Casciaro M., Gangemi S., Buquicchio R. Immunosenescence in aging: between immune cells depletion and cytokines up-regulation. Clin Mol Allergy. 2017;15:21–28. doi: 10.1186/s12948-017-0077-0. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5731094/pdf/12948_2017_Article_77.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott F.W. Evaluation of Risks and Benefits Associated with Vaccination against Coronavirus Infections in Cats. Adv Vet Med. 1999;41:347–358. doi: 10.1016/S0065-3519(99)80026-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7149311/pdf/main.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Watkins R.R., Lemonovich T.L., Salata R.A. An update on the association of vitamin D deficiency with common infectious diseases. Can J Physiol Pharmacol. 2015;93(5):363–368. doi: 10.1139/cjpp-2014-0352. [DOI] [PubMed] [Google Scholar]
- 24.Jiménez-Sousa M.Á., Martínez I., Medrano L.M., Fernández-Rodríguez A., Resino S. Vitamin D in human immunodeficiency virus infection: influence on immunity and disease. Front Immunol. 2018;9:458–468. doi: 10.3389/fimmu.2018.00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bergman P., Lindh A.U., Björkhem-Bergman L., Lindh J.D. Vitamin D and respiratory tract infections: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2013;8(6) doi: 10.1371/journal.pone.0065835. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/23840373/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant W.B., Lahore H., McDonnell S.L. Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988–1006. doi: 10.3390/nu12040988. http://www.mdpi.com/resolver?pii=nu12040988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Temesgen Z. Interleukin-2 for the treatment of human immunodeficiency virus infection. Review. Drugs Today. 2006;42(12):791–801. doi: 10.1358/dot.2006.42.12.1025703. https://journals.prous.com/journals/servlet/xmlxsl/pk_journals.xml_summaryn_pr?p_JournalId=4&p_RefId=1025703 [DOI] [PubMed] [Google Scholar]
- 28.Tomova R., Antonov K., Ivanova A. Low-dose IL-2 therapy reduces HCV RNA and HBV DNA: case report. Anticancer Res. 2009;29(12):5241–5244. [PubMed] [Google Scholar]
- 29.Wu F, Wang A, Liu M, et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. medRxiv (2020): 2020.03.30.20047365. https://www.medrxiv.org/content/10.1101/2020.03.30.20047365v2.
- 30.Anonymus. “Immunity passports” in the context of COVID-19. Scientific brief.Pubished online 24 April 2020. https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19.
- 31.Zin M. SARS Immunity and Vaccination. Cell Mol Immunol. 2004;1:193–198. http://www.cmi.ustc.edu.cn/1/3/193.pdf [PubMed] [Google Scholar]
- 32.Shang B., Wang X.-Y., Yuan J.-W. Characterization and application of monoclonal antibodies against N protein of SARS-coronavirus. Biochem Biophys Res Commun. 2005;336(1):110–117. doi: 10.1016/j.bbrc.2005.08.032. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092910/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gu J., Gong E., Zhang B. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415–424. doi: 10.1084/jem.20050828. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2213088/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kohyama S., Ohno S., Suda T. Efficient induction of cytotoxic T lymphocytes specific for severe acute respiratory syndrome (SARS)-associated coronavirus by immunization with surface-linked liposomal peptides derived from a non-structural polyprotein 1a. Antiviral Res. 2009;84(2):168–177. doi: 10.1016/j.antiviral.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]