Abstract
The California Bridge Program supports expansion of medications for opioid use disorder (MOUD) in emergency departments (EDs) and hospital inpatient units across the state. Here, we describe the change in activity before and after the coronavirus disease 2019 (COVID-19) California statewide shutdown. Of the 70 participating hospitals regionally distributed across California, 52 report MOUD-related activity monthly. We analyzed data on outcomes of OUD care and treatment: identification of OUD, acceptance of referral, receipt of buprenorphine prescription, administration of buprenorphine, and follow-up linkage to outpatient OUD treatment, from May 2019 to April 2020. In estimating the expected number of patients who met each outcome in April 2020, we found decreases in the expected to observed number of patients across all outcomes (all p-values<0.002): 37% (from 1053 to 667) decrease in the number of patients identified with OUD, 34% (from 632 to 420) decrease in the number of patients who accepted a referral, 48% (from 521 to 272) decrease in the number of patients who were prescribed buprenorphine, 53% (from 501 to 234) decrease in the number of patients who were administered buprenorphine, and 33% (from 416 to 277) decrease in the number of patients who attended at least one follow-up visit for addiction treatment. The COVID-19 California statewide shutdown was associated with an abrupt and large decrease in the progress toward expanded access to OUD treatment.
Keywords: Emergency services, Opiate substitution treatment, Buprenorphine, Administration and dosage, Opioid-related disorders
1. Introduction
On March 4, 2020, California proclaimed a state of emergency due to the threat of COVID-19, which was followed by an executive order to shelter-in-place on March 19. These events created an unprecedented challenge to hospital-based efforts to increase access to medication for opioid use disorder (MOUD). Suffering from mental health and substance use disorders increased significantly with the stress and isolation of the COVID-19 pandemic (Raj et al., 2020). Preliminary data suggest an increase in drug overdose deaths related to opioid use disorder (OUD; Alter & Yeager, 2020; D'Onofrio et al., 2020). Yet U.S. emergency department (ED) visits dropped sharply during COVID-19 (Baum & Schwartz, 2020; Volkow, 2020b).This raised concerns for a dual crisis of an exacerbated opioid epidemic combined with restricted access to behavioral health and MOUD (Volkow, 2020a, Volkow, 2020b).
The California Bridge Program (CA Bridge) is a large statewide initiative with 70 participating hospitals that implemented best practices for initiation of buprenorphine for OUD (D'Onofrio et al., 2015; D'Onofrio et al., 2018; Herring et al., 2019; Houry et al., 2018; National Institute on Drug Abuse, 2020; Substance Abuse and Mental Health Services Administration, 2017; Wax et al., 2019). CA Bridge provides participating sites with funding to support implementation of hospital-based MOUD teams that feature a clinical champion, on-site substance use navigator (SUN), best practice guidelines, and ongoing training and support (see http://www.CAbridge.org). The objective of this study was to use the scale and reach of CA Bridge to characterize changes in utilization of buprenorphine access for OUD prior to COVID shelter-in-place orders (https://www.Cabridge.org).
2. Material and methods
The CA Bridge includes a subset of 52 hospitals—of which 12 are in a rural setting and 13 are from a hospital with a teaching program—that report aggregate monthly data of key outcomes. Staff who track and treat patients for OUD at each hospital tallied and submitted on a monthly basis numbers of patients identified with and treated for OUD (primarily from EDs but can include inpatient units). The number of patients in each month is unique. The study also counted patients who use CA Bridge for additional treatments during the period in the month(s) of their new treatment(s).
To quantify the impact of COVID-19 on the activities of the CA Bridge, we compared program outcomes from the pre-COVID period (May 2019 to March 2020) to those immediately following in April 2020. Since the California statewide shelter-in-place began on March 19, 2020, March was considered as part of the pre-COVID period as the effect of the shutdown on hospital utilization likely lagged by several days (Executive Department, State of California, 2020). First, we calculated the following outcomes for each month from May 2019 to April 2020: total number of patients identified with OUD, number of patients who accepted a referral, number of patients who received a buprenorphine prescription, number of patients who were administered buprenorphine within the hospital, and the number of patients who attended at least one follow-up visit (outside the hospital) for addiction treatment within 30 days. We then performed a separate linear regression for each outcome on time (month) to estimate the average monthly increase (resulting β 95% confidence interval (CI), p-value) in the number of patients who met each outcome from May 2019 to March 2020. We used the average monthly increase in the number of patients from each linear regression model to estimate the expected number of patients for each outcome. We assumed continuation of a linear trend in April 2020 based on data from May 2019 to March 2020. The study then calculated the percent decrease from the expected to the observed number of patients for each outcome. Additionally, we calculated both the proportion of patients who were prescribed buprenorphine and the proportion of patients who were administered buprenorphine in the ED out of the total number of patients identified with OUD in each month.
During the study period there were no changes in the data reporting methodology that could affect the expected number of patients observed for each outcome. The Public Health Institute Institutional Review Board and California's Office of Statewide Health Planning and Development Committee for the Protection of Human Subjects approved the study procedures.
3. Results
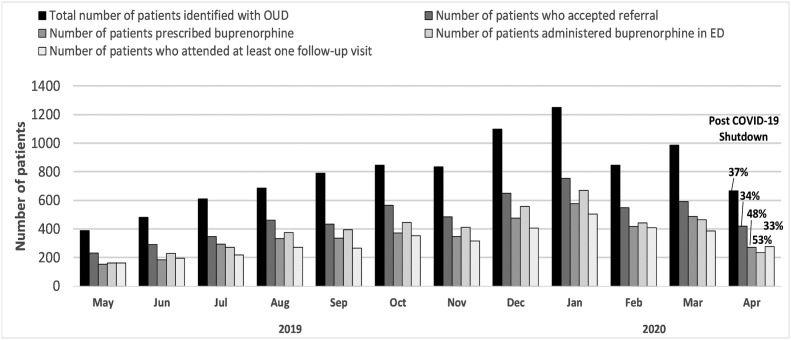
From May 2019 to Mar 2020, there was an average linear increase in the number of patients who met each of the five main CA Bridge outcomes; 66 patients (95% CI: 36–96, p<0.01) who were identified with OUD, 41 patients (95% CI: 23–59, p<0.01) who accepted a referral, 34 patients (95% CI: 21–47, p<0.01) who were prescribed buprenorphine, 36 patients (95% CI: 17–54, p<0.01) who were administered buprenorphine, and 29 patients (95% CI: 18–39, p<0.01) who attended a follow-up visit for addiction treatment within 30 days (see Fig. 1 ). Then in April 2020, the observed number of patients was lower than the expected for each outcome. The following percent decrease from the expected to the observed number of patients was estimated for each outcome: 37% (from 1053 to 667) decrease in the number of patients identified with OUD; 34% (from 632 to 420) decrease in the number of patients who accepted a referral; 48% (from 521 to 272) decrease in the number of patients who were prescribed buprenorphine; 53% (from 501 to 234) decrease in the number of patients who were administered buprenorphine; and 33% (from 416 to 277) decrease in the number of patients who attended at least one follow-up visit for addiction treatment.
Fig. 1.
CA Bridge hospital reports of emergency department identification of patients with opioid use disorder, initiation of buprenorphine, and linkage to long-term addiction treatment, May 2019 to April 2020.
Note: Percentages listed above each outcome in April represent the decrease in the observed compared to the expected for that month based on the linear trend observed for the prior 11 months.
During the study period of interest, the monthly percentage of patients identified with OUD who received a prescription for buprenorphine and/or were administered buprenorphine within the hospital ranged between 39 and 49% and 35–54%, respectively. With the exception of one month between May 2019 to February 2020, the proportion of patients who were administered buprenorphine within the hospital either equaled or exceeded the proportion who received a buprenorphine prescription; the reverse occurred in both March and April. The proportion who were administered buprenorphine in the hospital in April was the lowest observed over the entire 12-month period.
4. Discussion
The CA Bridge—the largest ED-initiated buprenorphine for OUD program in the US—reported 9 months of steady expansion of buprenorphine use in the ED and hospital setting. We observed that the timing of the imposed COVID-19 state-of-emergency orders was associated with a rapid drop in ED initiation of buprenorphine in California (53%). Given preliminary concerns about increases in opioid overdose deaths during the COVID-19 pandemic, reductions in ED-initiated buprenorphine post-COVID-19 restrictions emphasizes the need for intentional redundancy through the maintenance of multiple low-threshold MOUD access points to ensure access to this essential medication.
In the initial phases of the response to COVID-19 in California, hospitals lacked protocols and equipment to ensure safety of staff who were not absolutely required to be present in the hospital, such as social workers and substance use navigators and most were removed from the EDs (Internal communication). Patients experienced transportation disruptions, fear of contracting coronavirus at hospitals, and concerns of not being treated or worse—not being treated well (Czeisler, Marynak, & Clarke, 2020; Spagnolo et al., 2020). Most EDs developed tight screening procedures and triage processes including external tents staffed with medical personnel in head-to-toe personal protective equipment, which created a natural disincentive to seek MOUD from the ED (Noble et al., 2020).
The Drug Enforcement Agency relaxed regulatory burdens for providing buprenorphine treatment in response to the COVID-19 crisis. Our data show that patients are able to use the ED in a unique 24–7, low-threshold capacity to increase access to MOUD, for patients unable or unwilling to present to traditional medical settings (Anderson et al., 2016). As hospitals pivoted to focus on COVID-19, this high-volume access point was temporarily disrupted and utilization decreased. We observed during the initial months of the shelter-in-place (March and April 2020) an increased proportion of prescribed versus administered buprenorphine. This difference may indicate that patients were less likely to present in acute opioid withdrawal and/or clinicians were more likely to simplify the encounter by providing a prescription for an out-of-hospital self-initiation.
4.1. Limitations
The geographic distribution of CA Bridge hospitals is diverse with urban, suburban, and rural hospitals across all major geographic regions of California. However, these data are not representative of all ED visits in California. Data reporting from hospitals is verified through site visits and regular audits, but our independent confirmation of all data is not feasible. Outcome data are reported monthly in aggregate, and treatment categories are not mutually exclusive. We could not confirm reported services by electronic health records at all sites. Additionally, patient-level data were not available at the time of this analysis, so we cannot specifically describe the patient population that these hospitals served.
5. Conclusions
The infectious disease pandemic of COVID-19 had an initial negative impact on buprenorphine initiated in EDs across California. All markers of outcomes for ED and hospital treatment of OUD using buprenorphine in California showed initial reductions. We must use this time now to explore opportunities for systems to work together, to reduce regulation, to increase ED OUD treatment access (both in-person and telehealth), and to develop alternate sites for 24–7 low-barrier access to MOUD.
CRediT authorship contribution statement
Andrew Herring Conceptualization, Investigation, Methodology, Writing - Original draft preparation, Writing - Review & editing
Mariah Kalmin Conceptualization, Investigation, Methodology, Writing - Original draft preparation, Formal analysis, Writing - Review & editing
Melissa Speener Conceptualization, Investigation, Methodology, Writing - Original draft preparation, Formal analysis, Writing - Review & editing
David Goodman-Meza Conceptualization, Investigation, Methodology, Writing - Review & editing
Hannah Snyder Conceptualization, Investigation, Writing - Review & editing
Arianna Sampson Conceptualization, Investigation, Writing - Review & editing
Aimee Moulin Conceptualization, Investigation, Writing - Review & editing
Steve Shoptaw Supervision, Conceptualization, Methodology, Writing - Review & editing.
References
- Alter A., Yeager C. Overdose Detection Mapping Application Program; 2020. The consequences of Covid-19 on the overdose epidemic: Overdoses are increasing. http://www.odmap.org/Content/docs/news/2020/ODMAP-Report-May-2020.pdf Retrieved from.
- Anderson E.S., Hsieh D., Alter H.J. Social emergency medicine: Embracing the dual role of the emergency department in acute care and population health. Annals of Emergency Medicine. 2016;68(1):21–25. doi: 10.1016/j.annemergmed.2016.01.005. [DOI] [PubMed] [Google Scholar]
- Baum A., Schwartz M.D. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Marynak K., Clarke K.E. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G., McCormack R.P., Hawk K. Emergency departments - A 24/7/365 option for combating the opioid crisis. New England Journal of Medicine. 2018;379(26):2487–2490. doi: 10.1056/NEJMp1811988. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G., O’Connor P.G., Pantalon M.V., Chawarski M.C., Busch S.H., Owens P.H., et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G., Venkatesh A., Hawk K. 2020. The adverse impact of Covid-19 on individuals with OUD: Highlights the urgent need for reform to leverage emergency department–based treatment. NEJM Catalyst Innovations in Care Delivery. [DOI] [Google Scholar]
- Executive Department, State of California Executive Order N-33-20. 2020. https://www.gov.ca.gov/wp-content/uploads/2020/03/3.19.20-attested-EO-N-33-20-COVID-19-HEALTH-ORDER.pdf
- Herring A.A., Perrone J., Nelson L.S. Managing opioid withdrawal in the emergency department with buprenorphine. Annals of Emergency Medicine. 2019;73(5):481–487. doi: 10.1016/j.annemergmed.2018.11.032. [DOI] [PubMed] [Google Scholar]
- Houry D.E., Haegerich T.M., Vivolo-Kantor A. Opportunities for prevention and intervention of opioid overdose in the emergency department. Annals of Emergency Medicine. 2018;71(6):688–690. doi: 10.1016/j.annemergmed.2018.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse Opioid overdose crisis. 2020. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
- Noble J., Degesys N.F., Kwan E., Grom E., Brown C., Fahimi J., et al. Emergency department preparation for COVID-19: Accelerated care units. Emergency Medicine Journal. 2020;37(7):402–406. doi: 10.1136/emermed-2020-209788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj A., Johns N.E., Barker K.M., Silverman J.G. Time from COVID-19 shutdown, gender-based violence exposure, and mental health outcomes among a state representative sample of California residents. EClinicalMedicine. 2020;26:100520. doi: 10.1016/j.eclinm.2020.100520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spagnolo P.A., Montemitro C., Leggio L. New challenges in addiction medicine: COVID-19 infection in patients with alcohol and substance use disorders—The perfect storm. American Journal of Psychiatry. 2020;177(9):805–807. doi: 10.1176/appi.ajp.2020.20040417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2017. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS publication no. SMA 17-5044, NSDUH series H-52)https://www.samhsa.gov/data/ Retrieved from. [Google Scholar]
- Volkow N.D. Collision of the COVID-19 and addiction epidemics. Annals of Internal Medicine. 2020;173(1):61–62. doi: 10.7326/M20-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N. National Institute on Drug Abuse; 2020. COVID-19: Potential implications for individuals with substance use disorders. https://www.drugabuse.gov/about-nida/noras-blog/2020/04/covid-19-potential-implications-individuals-substance-use-disorders
- Wax P.M., Stolbach A.I., Schwarz E.S., Warrick B.J., Wiegand T.J., Nelson L.S. ACMT position statement: Buprenorphine administration in the emergency department. Journal of Medical Toxicology. 2019;15(3):215–216. doi: 10.1007/s13181-019-00712-3. [DOI] [PMC free article] [PubMed] [Google Scholar]