Abstract
Background:
Search algorithms used to identify patients with alopecia areata (AA) need to be validated prior to use in large databases.
Objectives:
The aim of the study is to assess whether patients with an International Statistical Classification of Diseases and Related Health Problems (ICD) 9 or 10 code for AA have a true diagnosis of AA.
Materials and Methods:
A multicenter retrospective review was performed at Columbia University Irving Medical Center, Brigham and Women's Hospital, and Massachusetts General Hospital to determine whether patients with an ICD 9 codes (704.01 - AA) or ICD 10 codes (L63.0 -Alopecia Totalis, L63.1 - Alopecia Universalis, L63.2 - Ophiasis, L63.8 - other AA, and L63.9 - AA, unspecified) for AA met diagnostic criteria for the disease.
Results:
Of 880 charts, 97.5% had physical examination findings consistent with AA, and 90% had an unequivocal diagnosis. AA was diagnosed by a dermatologist in 87% of the charts. The positive predictive value (PPV) of the ICD 9 code 704.01 was 97% (248/255). The PPV for the ICD 10 codes were 64% (75/118) for L63.0, 86% (130/151) for L63.1, 50% (1/2) for L63.2, 91% (81/89) for L63.8, and 93% (247/265) for L63.9. Overall, 89% (782/880) of patients with an ICD code for AA were deemed to have a true diagnosis of AA.
Conclusions:
Patients whose medical records contain an AA-associated ICD code have a high probability of having the condition.
Key words: Alopecia areata, database, international classification of diseases, positive predictive value, validation
INTRODUCTION
Large cohort studies in alopecia areata (AA) are limited by a lack of search strategies that have been developed and validated for other dermatologic disorders.[1,2] The accuracy of clinical coding derived from the International Statistical Classification of Diseases and Related Health Problems (ICD) cannot be assumed due to clinical error, uncertainty regarding diagnosis, missing information, and the nature by which the lack of robustness in coding leads to improper grouping of medical conditions. This study aims to assess the validity of using ICD codes to establish a verified list of AA patients for future epidemiological or clinical studies.
MATERIALS AND METHODS
A retrospective case series was performed at Columbia University Irving Medical Center (CUIMC), Brigham and Women's Hospital (BWH), and Massachusetts General Hospital (MGH) to determine whether patients with an ICD 9 code (704.01 - AA) or ICD 10 (L63.0 - Alopecia Totalis, L63.1 - Alopecia Universalis, L63.2 - Ophiasis, L63.8 - Other AA, and L63.9 - AA, unspecified) met the diagnostic criteria for AA. A query was submitted at CUIMC for a randomized selection of approximately 150 patients with each of the above-mentioned ICD codes from 2009 to 2019 through the Clinical Data Warehouse (CDW), facilitated by the Tripartite Request Assessment Committee. The CDW captures data from the New York-Presbyterian Hospital and Columbia Doctors, both of which are affiliated with CUIMC. At BWH/MGH, a query was submitted for 100 patients with the same ICD codes from 2015 to 2019 through the Research Patient Data Registry, which captures information from various Partners hospital systems.
There are no validated diagnostic guidelines for diagnosis of AA. The clinical criteria used to validate a diagnosis of AA was adapted from a Mayo Clinic study in conjunction with dermatologists from CUIMC and BWH who specialize in hair disorders.[3] In order for a diagnosis of AA to considered definite, it had to be the unequivocal impression of the dermatologist or had to be the unequivocal impression made by a nondermatologist with supportive documentation. Supportive documentation can include a physical examination description compatible with AA or AA variant (i.e., alopecia totalis), such as exclamation point hairs or circumscribed patches of hair loss. A set of acceptable diagnostic terms was agreed upon by both institutions in the study and applied to all patients. Biopsy data were not considered due to the limited amount of data available. For a diagnosis to be unequivocal, the diagnosis of AA or an equivalent acronym needed to be documented in an unstructured form in the assessment or plan section. A diagnosis was considered equivocal if a differential diagnosis was listed associated with AA or there was any other sign or terminology to suggest ambiguity, such as a question mark.
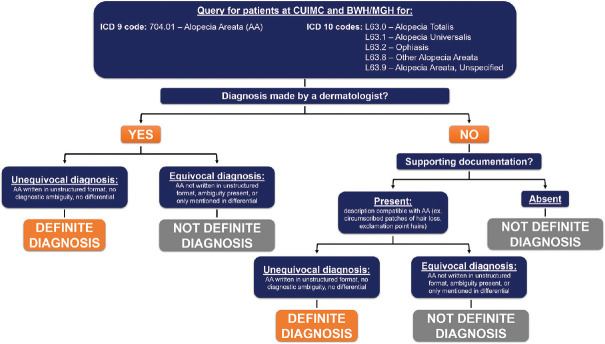
Positive predictive values (PPVs) were calculated for each ICD code as well as an overall PPV for all AA patients. Figure 1 depicts the workflow that was used for this study.
Figure 1.
Workflow for validating a diagnosis of alopecia areata based on international classification of diseases coding
This retrospective study was approved by the Human Research Protection Office and Institutional Review Board of Columbia University and the Partners Human Research Committee, which is the institutional review board of Partners HealthCare. All study procedures followed are in accordance with their standards as well as with the Helsinki Declaration of 1975, as revised in 2000.
RESULTS
Eight hundred and eighty patients with an ICD 9 or 10 code for AA were identified. We aimed to review up to 250 charts for each diagnosis code associated with AA. All records were reviewed for the major ICD 9 (704.01) and ICD 10 (L63.9) codes for AA, as well as less-utilized codes for AA subtypes [Table 1]. The majority of patients were female (61%) and had physical examination findings consistent with AA [97.5%, Table 1]. For most patients, the diagnosis of AA was unequivocal (90%). Overall, AA was diagnosed by a dermatologist in 87% of the charts reviewed.
Table 1.
Number of patient charts reviewed for each International Classification of Diseases code at each respective institutions, along with gender, physical exam, ambiguity, and provider validation findings in patients with an International Classification of Diseases code for alopecia areata*
| ICD code | Patients from BWH/MGH | Patients from CUIMC | Total | Male (%) | Female (%) | Physical exam findings consistent with AA or intended diagnosis code (/) (%) | No ambiguity in diagnosis of AA or intended diagnosis code (/) (%) | Diagnosis made by dermatologist. (/)(%) |
|---|---|---|---|---|---|---|---|---|
| L63.0 | 45 | 73 | 118 | 40 (34) | 78 (66) | 57 (52) | 75 (64) | 62 (53) |
| L63.1 | 28 | 123 | 151 | 68 (45) | 83 (55) | 136 (90) | 133 (88) | 128 (85) |
| L63.2 | 1 | 1 | 2 | 0 (0) | 2 (100) | 1/2 (50) | 1 (50) | 1 (50) |
| L63.8 | 20 | 69 | 89 | 27 (30) | 62 (70) | 78 (88) | 82 (92) | 83 (93) |
| L63.9 | 100 | 165 | 265 | 105 (40) | 160 (60) | 249 (94) | 249 (94) | 246 (93) |
| 704.01 | 100 | 155 | 255 | 99 (39) | 156 (61) | 248 (97) | 248 (97) | 244 (96) |
| Overall | 294 | 586 | 880 | 339 (39) | 541 (61) | 858 (97.5) | 788 (90) | 764 (87) |
*BWH – Brigham and Women’s Hospital; MGH – Massachusetts General Hospital;”CUIMC – Columbia University Irving Medical Center; AA – Alopecia areata (ICD 9 code: 704.01 - AA, ICD 10: L63.0 - Alopecia totalis, L63.1 - Alopecia universalis, L63.2 - Ophiasis, L63.8 - Other AA, L63.9 - AA, unspecified). ICD – International Classification of Diseases
Of the 782 patients who met definite criteria for AA, 85% (744/880) had a diagnosis by a dermatologist and 7% (63/880) had a diagnosis by another type of provider [Table 2].
Table 2.
Patients meeting criteria for alopecia areata based upon International Classification of Diseases code, subdivided by specialty of physician making a definite diagnosis of alopecia areata
| ICD code | Definite diagnosis by a dermatologist (%) | Definite diagnosis by nondermatologist (%) | Total number of patients who met definite criteria for AA | Total number of patients who did not meet definite criteria for AA | Total number of patients | PPV of ICD code for AA (%) |
|---|---|---|---|---|---|---|
| L63.0 | 65 (55) | 17 (14) | 75 | 43 | 118 | 64 |
| L63.1 | 126 (83) | 9 (6) | 130 | 21 | 151 | 86 |
| L63.2 | 1 (50) | 0 | 1 | 1 | 2 | 50 |
| L63.8 | 77 (87) | 4 (4) | 81 | 8 | 89 | 91 |
| L63.9 | 236 (89) | 15 (6) | 247 | 18 | 265 | 93 |
| 704.01 | 239 (94) | 18 (7) | 248 | 7 | 255 | 97 |
| Overall | 744 (85) | 63 (7) | 782 | 98 | 880 | 89 |
Percentages reflect definite diagnoses out of all cases identified in Table 1. A number of patients were given definite diagnoses by both a dermatologist and a nondermatologist, and this was taken into account when calculating the total number of patients who met definite criteria for AA. The total number of patients who met definite criteria for AA was used to calculate the PPV of each ICD code for AA. AA – AA (ICD 9 code: 704.01 - AA, ICD 10: L63.0 - Alopecia totalis, L63.1 - Alopecia universalis, L63.2 - Ophiasis, L63.8 - Other AA, L63.9 - AA, unspecified). ICD – International Classification of Diseases; AA – Alopecia areata; PPV – Positive predictive value
Overall, 89% (782/880) of patients with an ICD code for AA were determined to have a true diagnosis of AA based on chart review criteria. The ICD 10 codes L63.0 (Alopecia Totalis) had a lower PPV in determining whether a patient truly had true AA [75/118; 64%, Table 2]. There was insufficient data to determine the predictive value of the ICD 10 code L63.2 (Ophiasis).
DISCUSSION AND CONCLUSIONS
In this retrospective validation study, we determined the PPV of the ICD 9 and 10 codes for a diagnosis of AA among two large health-care systems in the United States. We found that ICD 9 or 10 codes associated with AA (704.01, L63.0, L63.1, L63.2, L63.8, L63.9) had an overall PPV of 88.9%. Accordingly, patients whose medical records contain an ICD code associated with AA have a high probability of having the disease. These codes can be accurately used in large databases to identify cases of AA. The most reliable ICD codes for developing a cohort as determined by this study were 704.01, L63.9, and L63.8, all of which are general ICD codes for AA as opposed to a specific subtype such as alopecia totalis (L63.0) or universalis (L63.1).
These findings cannot be extended to the identification of specific AA subtypes using ICD 10 codes. Among two large academic institutions, there were relatively few patients identified with the ICD codes L63.0 - Alopecia Totalis, L63.1 - Alopecia Universalis, L63.2 - Ophiasis, and L63.8 - other AA. In our study, several charts carried an ICD 10 code of L63.0 - Alopecia Totalis in the assessment section of the chart without any further elaboration in the history, physical examination, or plan section of the note. It remains unclear why the L63.0 ICD code was placed in these charts. These findings are likely representative of coding errors throughout electronic health records and reinforce the importance of validation studies. Although it is expected that miscoded charts would play a minor role if more charts were reviewed, a larger, multi-institution validation study is required to determine whether the above ICD 10 subtypes of AA individually have a sufficient PPV for their AA subtypes.
There are few other studies which have attempted to validate an ICD 9 or ICD 10 code for AA from clinical databases. Although Safavi et al. reported that 90% of the patients whose charts were reviewed fulfilled criteria for a definite diagnosis of AA, it is unclear whether their cohort of patients was initially identified by an ICD code for AA, and if so, whether this included codes for the specific subtypes of AA.[3] More recently, a study examining comorbidities in AA used an artificial intelligence program was used to determine which patient charts with an ICD 9 code of AA 704.01 had a true diagnosis of AA.[4] Here, approximately 60% of charts reviewed (2115 out of 3568) were determined to have a true diagnosis of AA. The sensitivity of the artificial intelligence algorithm was not reported, and it is unclear how many of the charts that did not meet inclusion criteria from the artificial intelligence model would have met criteria for AA based on a manual review. In a Korean study, 209 of the 220 patients with an ICD 10 code of L63 who had their chart reviewed were confirmed to have AA, resulting in a PPV of 95.0%.[5] The criteria used to validate the charts was not described. Overall, our PPVs lie within the range of those published by previous studies.
These results must be interpreted in the context of our study design. While AA is a clinical diagnosis, there are no validated diagnostic guidelines for AA. This can create inconsistency among which patients are considered to have a true diagnosis of AA. Although we attempted to minimize discordance by coming up with exact inclusion terminology agreed on by two dermatologists who specialize in hair loss conditions, some dermatologists may disagree about which patients meet inclusion criteria. Second, the use of medical records to confirm a diagnosis is an imperfect standard since most notes are written in the context of clinical care and may be missing details that would be used in a standardized assessment. Furthermore, inadequate clinical documentation may result in some patients not meeting the inclusion criteria, leading to an underestimation of the PPV.
A strength of this study includes the individual analysis of ICD codes for a true diagnosis of AA. This represents the first time and the largest cohort in which the various ICD 10 codes for AA, in addition to the ICD 9 codes, were individually validated across multiple institutions. In conclusion, the ICD 9 and 10 codes for AA collectively identify a cohort of patients with true AA with excellent accuracy. These data will help support future epidemiological studies in AA for which disease burden, comorbidities, and management patterns have not been adequately identified.
Financial support and sponsorship
This study was supported in part by P50AR070588-03, Alopecia Areata Center of Research Translation (AACORT) to AMC. EYL was funded by T32GM007367, Medical Scientist Training Program training grant at Columbia University.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Strunk A, Midura M, Papagermanos V, Alloo A, Garg A. Validation of a case-finding algorithm for hidradenitis suppurativa using administrative coding from a clinical database. Dermatology. 2017;233:53–7. doi: 10.1159/000468148. [DOI] [PubMed] [Google Scholar]
- 2.Lockwood SJ, Li DG, Butler D, Tsiaras W, Joyce C, Mostaghimi A. The validity of the diagnostic code for pyoderma gangrenosum in an electronic database. Br J Dermatol. 2018;179:216–7. doi: 10.1111/bjd.16446. [DOI] [PubMed] [Google Scholar]
- 3.Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton LJ., 3rd Incidence of alopecia areata in Olmsted County, Minnesota, 1975 through 1989. Mayo Clin Proc. 1995;70:628–33. doi: 10.4065/70.7.628. [DOI] [PubMed] [Google Scholar]
- 4.Huang KP, Mullangi S, Guo Y, Qureshi AA. Autoimmune, atopic, and mental health comorbid conditions associated with alopecia areata in the United States. JAMA Dermatol. 2013;149:789–94. doi: 10.1001/jamadermatol.2013.3049. [DOI] [PubMed] [Google Scholar]
- 5.Lee S, Lee YB, Kim BJ, Bae S, Lee WS. All-cause and cause-specific mortality risks associated with Alopecia Areata: A Korean nationwide population-based study. JAMA Dermatol. 2019;155:922–28. doi: 10.1001/jamadermatol.2019.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]