Abstract
Preeclampsia (PE) is a gestational-related disease presented with hypertension, peripheral edema, and proteinuria after 20 weeks of gestation. In PE, there are various metabolic changes like dyslipidemia. In addition, both PE and dyslipidemia are associated with changes of platelet indices. Thus, objective of the current study was to illustrate the potential role of dyslipidemia and platelet changes in pregnant women with PE. This case–control study involved 37 preeclamptic pregnant women as compared to 24 healthy pregnant women as controls. Blood pressure profile, lipid profile, proteinuria, and platelet indices were measured. Blood pressure profile was higher in preeclamptic pregnant women as compared to the controls (P < 0.01). There was a significant dyslipidemic status in preeclamptic pregnant women compared with the controls (P < 0.01). Platetetcrit (PCT) and platelet count (PC) were lower in preeclamptic pregnant women compared with the controls (P = 0.001). On the other hand, platelet distribution width (PDW), mean platelet volume (MPV), and platelet-large cell ratio (P-LCR) were higher in the pregnant women with PE as compared with the controls (P = 0.001). PCT and PC were insignificantly linked, while P-LCR, MPV and PDW were significantly correlated with total cholesterol, triglyceride, low-density lipoprotein (LDL)/high-density lipoprotein (HDL) ratio, systolic blood pressure, DBP, and MAP in preeclamptic patients compared with women of normal pregnancy. Both dyslipidemia and alterations in the platelet indices are correlated with blood pressure profile in PE. High MPV and PDW in association with high LDL/HDL ratio in pregnant women herald risk of PE.
Key words: Blood pressure, dyslipidemia, platelet indices, preeclampsia
INTRODUCTION
Preeclampsia (PE) is a gestational-related disease presented with hypertension, peripheral edema, and proteinuria after 20 weeks of gestation.[1] The risk factors of PE are extreme maternal age, nulliparity, obesity, insulin resistance, diabetes mellitus, chronic hypertension, gestational hypertension, twin and multiple gestation, previous preeclamptic pregnancy, and black race.[2]
The pathogenesis of PE is linked to the different etiopathological factors, including vascular, oxidative stress, genetic, and immune. However, the pathogenesis of PE remains obscure, making management and prevention of PE a current of challenge. There is unanimity of opinion concerning the standpoint in the pathogenesis of PE, Al-Maiahy et al. illustrate that poor placental invasion and trophoblastic neovascularization are the initial pathological changes with subsequent development of PE due to inflammation and oxidative stress-induced-vasoconstrictions.[3]
In PE, there are various metabolic changes like dyslipidemia, which is one of metabolic changes linked with high body mass index (BMI) during pregnancy. Physiologic hyperlipidemia is not atherogenic; however, hyperlipidemia is associated with the severity of hypertension in PE since; dyslipidemia in PE is highly prevalent in women with elevated BMI and obesity, that linked with placental dysfunction in PE.[4]
There is opinion unanimity, that both PE and dyslipidemia are associated with changes of platelet indices. Jäger et al.[5] found that platelets hyper-reactivity in patients with dyslipidemia, as well, Thalor et al.,[6] observed that changes in the platelet indices are linked with the severity of PE. Moreover, there are significant interactions between dyslipidemia and alteration in the platelet indices during PE, which together contribute in the development of PE.[7]
Thus, objective of the current study was to illustrate the potential role of dyslipidemia and platelet changes in pregnant women with PE.
MATERIALS AND METHODS
Study design
The current study involved 37 preeclamptic pregnant women aged 28–36 (31.85 ± 5.94) years compared with matched 24 healthy pregnant women as controls were recruited consecutively from the primary health center during routine visits of the antenatal care unit, during the period of June-October 2019. Selection of pregnant women was in harmony with the diagnostic criteria of Global Obstetrician and Gynecologist recommendation.[8] Written and informed verbal consents were attaining from all patients and controls. Subsequent of the comprehensive full history concerning parity, pregnancy-related complications, current and previous pharmacotherapy, the recruited pregnant women and controls were recruited into two groups: Group A: Preeclamptic women (n = 37) and Group B: healthy controls (n = 24).
Any pregnant women with chronic hypertension, gestational hypertension, cardiovascular complications, endocrine disorders, metabolic disorders, gestational diabetes mellitus, chronic sepsis, urinary tract infections (UTIs), multiple pregnancy, hepatic disorders, and chronic kidney disorders were excluded from this study.
Assessment of anthropometric variables
In the present study, BMI was estimated by explicit method, also blood pressure of patients and controls were measured at the supine position by digital sphygmomanometer 2 h apart.[9]
Gestational age was determined by the calculation the pregnancy period from the 1st day of the last menstrual cycle in addition to the ultrasonographic imaging measurements.
Assessment of biochemical parameters
Throughout the routine visiting, 10 mL of blood from all cases and controls, were centrifuged and stored for afterward investigation. Measurement of blood urea and serum creatinine was done by colometric assay. Besides, lipid profile such as triglyceride (TG), total cholesterol (TC), and high-density lipoprotein (HDL) were estimated by colorimetric kits. Both low-density lipoprotein (LDL) and very LDL were estimated in harmony to Al-kuraishy et al. method.[10] The second 5 ml of blood was stored in ethylenediaminetetraacetic acid (EDTA) tubes and used for the assessment of complete blood count (CBC) by automated hematology analyzer system (Abbot Diagnostics Santa Clara, USA). Parameters of CBC such as packed cell volume, white blood cell, mean platelet volume (MPV), platelet distribution width (PDW), and pleteletcrit (total platelet mass) were estimated.[11]
Measurement of proteinuria
Mid-stream urine from each patient and controls were collected in a special container and the amount of proteinuria was assessed by urinary dipstick method.[12]
Data analysis
Data analysis was performed using SPSS (IBM SPSS Statistics for Windows version 21.00,2017, Amonk, NY, IBM, CORP, USA) and presented as means ± standard deviation. Correlation of coefficient was done to find the correlation of different variables. The level of significance was considered when value of P < 0.05.
RESULTS
Study flow
Consort flow-diagram [Figure 1], illustrates that 4 (6.15%) of patients were excluded due to gestational diabetes and UTI, and hence, only 61 pregnant women were involved in this study.
Figure 1.
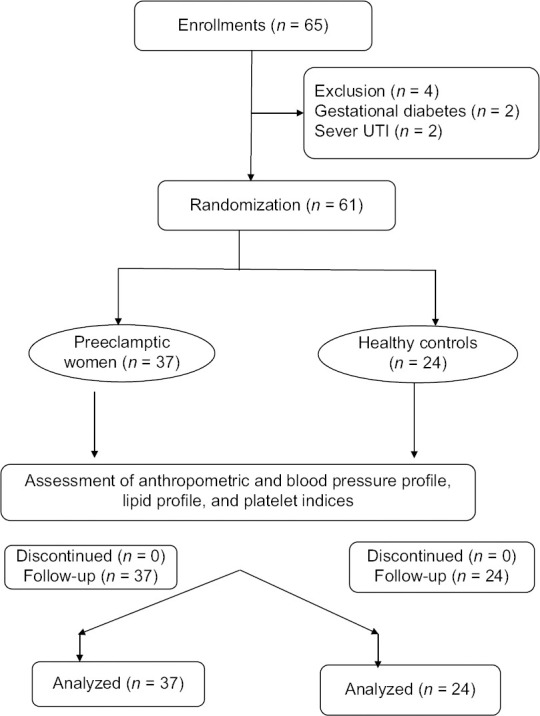
Consort flow-chart
Demographic characteristics
In this study, age and BMI of pregnant women with PE were comparable and were not differed from that of controls (P > 0.05) and (P > 0.05) correspondingly. Percentage of primigravida was superior in PE (40.54%) as compared to the controls (12.50%), (P < 0.05). Cesarean section (CS) to normal vaginal delivery ratio was high (27:10) compared with healthy controls (4:20), (P = 0.008). Moreover, 81.08% of preeclamptic patients used folic acid 1 mg/day compared with 54.17% of the controls (P = 0.02). Other characteristics are described in Table 1.
Table 1.
Characteristics of the present study
| Characteristics | Controls | PE | 95% CI | P |
|---|---|---|---|---|
| n | 24 | 37 | ||
| Age (years) | 30.71±5.93 | 31.85±5.94 | −2.013–4.213 | 0.48 |
| BMI (kg/m2) | 28.77±2.45 | 29.94±2.81 | −0.273–2.533 | 0.11 |
| GA (weeks) | 27.69±2.31 | 28.94±3.05 | −0.210–2.710 | 0.09 |
| Primigravida (%) | 3 (12.50) | 15 (40.54) | 4.719–45.975 | 0.02* |
| CS:NVD ratio | 4:20 | 27:10 | 4.411–39.454 | 0.008# |
| History of abortion% | 2 | 39 | 16.477–53.129 | 0.001# |
| White race | 23 (95.83) | 33 (89.19) | −10.710–20.954 | 0.35 |
| Black race | 1 (4.17) | 4 (10.81) | −10.710–21.856 | 0.31 |
| Smoking | 2 (8.33) | 7 (18.91) | −9.314–27.005 | 0.25 |
| Medications | ||||
| Anti-hypertensive | 32 (86.47) | |||
| Ferrous sulphate | 19 (79.17) | 29 (78.38) | −21.353–20.201 | 0.94 |
| Folic acid | 13 (54.17) | 30 (81.08) | 3.339–48.208 | 0.02* |
*P<0.05, #P<0.01. BMI: Body mass index, GA: Gestational age, CS: Cesarean section, NVD: Normal vaginal delivery, CI: Confidence interval, PE: Preeclampsia
Biochemical variables in preeclamptic patients
Regarding biochemical parameters, which was higher in the pregnant women with PE as compared with controls TC, TG, and LDL serum levels were higher preeclamptic patients as compared to the controls (P = 0.001), whereas HDL serum level was lower in preeclamptic patients compared with the controls (P = 0.03). As well, atherogenic profile and LDL/HDL were elevated in the preeclamptic women compared with the controls (P < 0.01) [Table 2]. In preeclamptic patients, proteinuria and blood pressure profile were higher in the preeclamptic patients compared with the controls (P < 0.01) [Table 3].
Table 2.
Lipid profile in the early-onset preeclamsia
| Parameters | Controls (n=24) | PE (n=37) | 95% CI | P |
|---|---|---|---|---|
| TC (mg/dL) | 154.29±12.81 | 174.29±19.81 | 10.864–29.135 | 0.001# |
| TG (mg/dL) | 148.73±9.74 | 186.96±13.42 | 31.874–44.585 | 0.001# |
| HDL (mg/dL) | 45.87±8.51 | 41.61±6.94 | −8.241–0.279 | 0.03* |
| VLDL (mg/dL) | 9.17±2.52 | 8.32±2.41 | −2.136–0.436 | 0.19 |
| LDL-C (mg/dL) | 78.70±9.85 | 95.30±10.62 | 11.182–22.015 | 0.001# |
| AI | 0.151±0.02 | 0.293±0.04 | 0.124–0.159 | 0.001# |
| LDL/HDL ratio | 1.71±0.75 | 2.29±0.86 | 0.150–1.009 | 0.009# |
*P<0.05, #P<0.01. TC: Total cholesterol; TG: Triglyceride; HDL: High density lipoprotein; LDL: Low density lipoprotein-cholesterol; VLDL: Very low density lipoprotein, AI: Atherogenic index, PE: Preeclampsia, CI: Confidence interval
Table 3.
Blood pressure profile and laboratory findings in the preeclamptic pregnant women
| Parameters | Controls (n=24) | PE (n=37) | 95% CI | P |
|---|---|---|---|---|
| SBP (mmHg) | 117.61±7.84 | 149.94±8.53 | 27.99–36.66 | 0.0001# |
| DBP (mmHg) | 67.95±9.33 | 97.89±6.52 | 25.88–33.99 | 0.001# |
| MAP (mmHg) | 85.00±6.41 | 115.00±9.21 | 25.68–34.31 | 0.003# |
| Blood urea (mg/dL) | 22.58±5.93 | 25.86±8.64 | −0.757–7.317 | 0.10 |
| Serum creatinine (mg/dL) | 1.12±0.56 | 1.39±0.74 | −0.084–0.624 | 0.13 |
| Hb (g/L) | 11.68±2.62 | 11.98±2.57 | −1.058–1.658 | 0.66 |
| Proteinuria (mg/dL) | 12.81±4.85 | 351.08±14.97 | 331.96–344.57 | 0.0001# |
#P<0.01. SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MAP: Mean arterial pressure, PE: Preeclampsia, CI: Confidence interval, Hb: Hemoglobin
Platelet indices in preeclamptic patients
Platetetcrit (PCT) and platelet count (PC) were reduced in preeclamptic patients compared with the controls (P = 0.001). However, MPV, PDW, and P-LCR were superior in preeclamptic women as in contrast with the controls (P = 0.001) [Table 4].
Table 4.
Platelet indices in preeclamptic patients
| Parameters | Controls (n=24) | PE (n=37) | 95% CI | P |
|---|---|---|---|---|
| PCT (%) | 0.28±0.04 | 0.25±0.03 | −0.048–0.012 | 0.001# |
| PC (×103/mm3) | 342.63±75.61 | 211.85±90.72 | −175.48–86.17 | 0.001# |
| MPV (fL) | 8.21±1.08 | 11.85±1.22 | 3.027–4.252 | 0.001# |
| PDW (fL) | 15.89±1.42 | 17.39±1.99 | 0.561–4.438 | 0.002# |
| P-LCR (%) | 22.96±7.93 | 29.96±9.51 | 2.321–11.678 | 0.004# |
#P<0.01. PCT: Platetetcrit, PC: Platelet count, MPV: mean platelet volume, PDW: Platelet distribution width, P-LCR: Platelet-large cell ratio
Correlations of platelet indices in preeclamptic patients
P-LCR, PDW, and MPV were correlated with LDL/HDL, TG, and AI in preeclamptic patients compared with the controls [Table 5]. As well, P-LCR, PDW, and MPV were correlated with blood pressure profile [Table 6]. Besides, all lipid profiles correlated positively with blood pressure profile (systolic blood pressure [SBP], diastolic blood pressure [DBP], and mean arterial pressure [MAP]) significantly, with exception of HDL serum level which was negatively correlated with MAP only and not with SBP or DBP [Table 7].
Table 5.
Correlation of atherogenic indices with the platelet indices in the preeclamptic pregnant women
| Platelet indices | AI |
LDL/HDL |
TC |
TG |
||||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | r | P | |
| PCT (%) | 0.31 | 0.06 | 0.29 | 0.08 | 0.30 | 0.07 | 0.28 | 0.09 |
| PC (×103/mm3) | 0.22 | 0.19 | 0.23 | 0.17 | 0.31 | 0.06 | 0.27 | 0.10 |
| MPV (fL) | 0.48 | 0.002# | 0.56 | 0.0003# | 0.43 | 0.007# | 0.41 | 0.01* |
| PDW (fL) | 0.55 | 0.004# | 0.52 | 0.0009# | 0.48 | 0.002# | 0.58 | 0.0001# |
| P-LCR (%) | 0.49 | 0.002# | 0.76 | 0.00001# | 0.66 | 0.00001# | 0.47 | 0.003# |
*P<0.05, #P<0.01. PCT: Platetetcrit, PC: Platelet count, MPV: Mean platelet volume, PDW: Platelet distribution width, P-LCR: Platelet-large cell ratio, TC: Total cholesterol, TG: Triglyceride, HDL: High density lipoprotein, LDL: Low density lipoprotein, AI: Atherogenic index, r: Correlation, P: Significance of difference
Table 6.
Correlation of platelet indices with blood pressure profile in preeclamptic pregnant women
| Platelet indices | SBP |
DBP |
MAP |
|||
|---|---|---|---|---|---|---|
| r | P | r | P | r | P | |
| PCT (%) | 0.22 | 0.19 | 0.30 | 0.07 | 0.31 | 0.06 |
| PC (×103/mm3) | 0.31 | 0.06 | 0.31 | 0.06 | 0.31 | 0.06 |
| MPV (fL) | 0.48 | 0.002# | 0.46 | 0.0003# | 0.43 | 0.007# |
| PDW (fL) | 0.55 | 0.004# | 0.72 | 0.0009# | 0.49 | 0.002# |
| P-LCR (%) | 0.43 | 0.007# | 0.86 | 0.00001# | 0.69 | 0.00001# |
#P<0.01. PCT: Platetetcrit, PC: Platelet count, MPV: Mean platelet volume, PDW: Platelet distribution width, P-LCR: Platelet-large cell ratio, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MAP: Mean arterial pressure, r: Correlation, P: Significance of difference
Table 7.
Correlation of blood lipid with blood pressure profile in preeclamptic pregnant women
| Platelet indices | SBP |
DBP |
MAP |
|||
|---|---|---|---|---|---|---|
| r | P | r | P | r | P | |
| TC (mg/dl) | 0.43 | 0.007# | 0.39 | 0.017* | 0.31 | 0.06 |
| TG (mg/dl) | 0.60 | 0.0001# | 0.66 | 0.0001# | 0.72 | 0.00001# |
| HDL (mg/dl) | −0.21 | 0.21 | −0.29 | 0.081 | −0.3 | 0.04* |
| VLDL (mg/dl) | 0.55 | 0.0004# | 0.39 | 0.017* | 0.49 | 0.002# |
| LDL (mg/dl) | 0.43 | 0.0007# | 0.86 | 0.00001# | 0.69 | 0.00001# |
| AI | 0.65 | 0.00001# | 0.76 | 0.00001# | 0.64 | 0.00001# |
| LDL/HDL ratio | 0.58 | 0.00001# | 0.62 | 0.00001# | 0.55 | 0.0001# |
*P<0.05, #P<0.01. TC: Total cholesterol, TG: Triglyceride, HDL: High density lipoprotein, LDL: Low density lipoprotein, VLDL: Very low density lipoprotein, AI: Atherogenic index, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MAP: Mean arterial pressure, r: Correlation, P: Significance of difference
DISCUSSION
Findings of this study illustrated that preeclamptic pregnant women demonstrated an advanced BMI but not significantly differed from that of the controls since; high BMI and obesity are regarded as possible risk factor in the progression of PE.[13] As well, our findings showed that there was a higher percentage of a primigravida with history of previous CS and abortion, which together increase the risk and incidence of subsequent PE. As well, there were 18.91% of our preeclamptic patients were cigarette smoking, this low percentage of smoking might increase the risk of PE since; smoking is observed paradoxically to be a protective cause alongside the progress of PE through carbon monoxide induced-vasodilatation.[14]
Moreover, the present study demonstrated the typical presentation of PE in the pregnant women; as there were significant hypertension and proteinuria in the preeclamptic pregnant women compared with healthy controls. This type of PE is called early-onset PE since the gestational age of all recruited preeclamptic women started after 20 and before 34 weeks of gestation.[15]
Furthermore, in the present study, preeclamptic patients showed dyslipidemic status with high atherogenic index and LDL/HDL ratio. Wojcik-Baszko et al.,[16] found a positive association and interrelated relationship between dyslipidemia and PE. Recent emerging evidence regarding the development of PE suggests that deregulations of feto-maternal lipid metabolism is linked with the pathogenesis of PE.[17] However, not all preeclamptic pregnant women develop dyslipidemia and some pregnant women with profound dyslipidemia had normal pregnancy outcomes. Nevertheless, high TG and FFA serum levels lead to induction of vasoconstriction and endothelial dysfunction through suppression of endothelial prostacyclin and nitric oxide (NO) with induction of oxidative stress.[18] Indeed, Aragon-Charris et al.[19] corroborate that pregnant women with PE have a high atherogenic index.
Besides, the current findings confirmed that preeclamptic pregnant women were associated with significant alterations in the platelet indices, as PCT and PC were lower, while P-LCR, PDW, and MPV were advanced in preeclamptic pregnant women compared with healthy pregnant women as disclosed previously.[20] In addition, elevation of PDW and MPV are detected earlier in patients with PE before rise of blood pressure, and then low PC, high PDW and MPV proportionally correlate with level of hypertension in PE. Thus, these indices reflect the underlying the severity of PE. It was evident that P-LCR, PDW and MPV are increased after 20 weeks of pregnancy and correlated with the severity of PE; however, in the present study, these indices were increased in mild PE of our patients. In reviewing different literatures, we found that MPV and PDW are independent indices correlated with level of hypertension and proteinuria in nonthrombocytopenic preeclamptic patients as conducted by Reddy and Prasad study.[21] As evident in the present study, a cutoff value of PDW >13.4 predicts the development of PE.
The reason behind altered platelet indices in PE is related to abnormal trophoblastic invasion in early pregnancy. Placental hypoxia in pregnant women with PE activates the release of erythropoietin from renal and hepatic tissue, which stimulates the bone marrow for production of large megakaryocyte.[22] Chulkov et al.[23] confirmed that placental erythropoietin mRNA gene expression is up-regulated in severe PE, causing more increase in erythropoietin serum and subsequent abnormal platelet indices. Besides, the erythropoietin serum level is increased by 2–4 folds and reaches a plateau in 20 weeks of gestation. Regrettably, the erythropoietin serum level was not evaluated in the current study.
Concerning the association between platelet indices and dyslipidemia, the present study illustrated that PCT and PC were not significantly correlated, while MPV, PDW, and P-LCR were significantly correlated with AI, LDL/TC ratio, TC and TG in the pregnant women with PE as compared with controls. Susilowati et al. showed that oxidized LDL (oxLDL) promotes platelet aggregations through reduction of platelet NO; in turn, the activated platelets activate the uptake of oxLDL by macrophages.[24] This interaction leads to significant changes in the platelet indices as shown in the current study. Different studies have been shown that dyslipidemia may affect the metabolic activity of platelets, as oxLDL activates while HDL inhibits the atherogenic activity of platelets.[25] Indeed, LDL/HDL ratio is more important than LDL or HDL alone, as it reflects the metabolic equilibrium since; LDL/HDL ratio is more correlated with platelet indices[26] as illustrated in the present study. Therefore, dyslipidemic status in the preeclamptic pregnant women contributes to the significant platelet changes, which in turn increase the risk of cardio-metabolic complications in PE. Furthermore, the present found a strong relationship between platelet indices and lipid profile in pregnant women with PE.
This study had some limitations, which were the small sample size, variability of platelet size, serial measurements of MPV were not done, and plasma erythropoietin concentration was not evaluated. Nevertheless, this study is considered as a pilot study for extended forthcoming study to assess the potential link between platelet alterations and their association with the dyslpidemic status in the preeclamptic pregnant women.
CONCLUSION
Initial or early-onset PE is linked with remarkable changes in the platelet indices and lipid profile. Both dyslipidemia and alterations of platelet indices are correlated with blood pressure profile in PE.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge all postgraduated medical staff members for their participations in this study.
REFERENCES
- 1.Al-Kuraishy HM, Al-Gareeb AI, Al-Maiahy TJ. Concept and connotation of oxidative stress in preeclampsia. J Lab Physicians. 2018;10:276–82. doi: 10.4103/JLP.JLP_26_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmadi F. A comparative study on infusion of usual dose of oxytocin and 80 units dose of oxytocin in the prevention of postpartum hemorrhage in cesarean section. J Adv Pharm Technol Res. 2018;9:102–6. doi: 10.4103/japtr.JAPTR_297_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Maiahy T, Al-Gareeb A, Al-Kuraishy H. Prolactin and risk of preeclampsia: A single institution, cross-sectional study. Asian Pac J Reprod. 2019;8:112. [Google Scholar]
- 4.Darghahi R, Mobaraki-Asl N, Ghavami Z, Pourfarzi F, Hosseini-Asl S, Jalilvand F. Effect of cell-free fetal DNA on spontaneous preterm labor. J Adv Pharm Technol Res. 2019;10:117–20. doi: 10.4103/japtr.JAPTR_371_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jäger B, Piackova E, Haller PM, Andric T, Kahl B, Christ G, et al. Increased platelet reactivity in dyslipidemic patients with coronary artery disease on dual anti-platelet therapy. Arch Med Sci. 2019;15:65–71. doi: 10.5114/aoms.2018.81035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thalor N, Singh K, Pujani M, Chauhan V, Agarwal C, Ahuja R. A correlation between platelet indices and preeclampsia. Hematol Transfus Cell Ther. 2019;41:129–33. doi: 10.1016/j.htct.2018.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang H, Zhang Y, Wang Z, Yan J. Platelet count and mean platelet volume predict atypical pre-eclampsia. Pregnancy Hypertens. 2019;18:29–34. doi: 10.1016/j.preghy.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Blue NR, Beddow ME, Savabi M, Katukuri VR, Mozurkewich EL, Chao CR. A comparison of methods for the diagnosis of fetal growth restriction between the royal college of obstetricians and gynaecologists and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2018;131:835–41. doi: 10.1097/AOG.0000000000002564. [DOI] [PubMed] [Google Scholar]
- 9.Al-Kuraishy HM, Al-Gareeb AI. Effects of Rosuvastatin Alone or in Combination with Omega-3 Fatty Acid on Adiponectin Levels and Cardiometabolic Profile. J Basic Clin Pharm. 2016;8:8–14. doi: 10.4103/0976-0105.195080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Kuraishy HM, Al-Gareeb AI, Shams HA, Al-Mamorri F. Endothelial dysfunction and inflammatory biomarkers as a response factor of concurrent coenzyme Q10 add-on metformin in patients with type 2 diabetes mellitus. J Lab Physicians. 2019;11:317–22. doi: 10.4103/JLP.JLP_123_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Correa ME, Côté AM, De Silva DA, Wang L, Packianathan P, von Dadelszen P, et al. Visual or automated dipstick testing for proteinuria in pregnancy.? Pregnancy Hypertension. 2017;7:50–3. doi: 10.1016/j.preghy.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Al-Maiahy TJ, Al-Gareeb AI, Al-kuraishy HM. Testosterone is a surrogate and proxy biomarker for severity of late-onset preeclampsia: A cross-sectional study. Asian Pac J Reprod. 2020;9:1. [Google Scholar]
- 13.Rasheed HA, Al-Kuraishy HM, Al-Gareeb AI, Hussien NR, Al-Nami MS. Effects of diabetic pharmacotherapy on prolactin hormone in patients with type 2 diabetes mellitus: Bane or boon. J Adv Pharm Technol Res. 2019;10:163. doi: 10.4103/japtr.JAPTR_65_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tran DT, Preen DB, Einarsdottir K, Kemp-Casey A, Randall D, Jorm LR, et al. Use of smoking cessation pharmacotherapies during pregnancy is not associated with increased risk of adverse pregnancy outcomes: A population-based cohort study. BMC Med. 2020;18:15. doi: 10.1186/s12916-019-1472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yung HW, Colleoni F, Dommett E, Cindrova-Davies T, Kingdom J, Murray AJ, et al. Noncanonical mitochondrial unfolded protein response impairs placental oxidative phosphorylation in early-onset preeclampsia. Proc Natl Acad Sci U S A. 2019;116:18109–18. doi: 10.1073/pnas.1907548116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wojcik-Baszko D, Charkiewicz K, Laudanski P. Role of dyslipidemia in preeclampsia-A review of lipidomic analysis of blood, placenta, syncytiotrophoblast microvesicles and umbilical cord artery from women with preeclampsia. Prostaglandins Other Lipid Mediat. 2018;139:19–23. doi: 10.1016/j.prostaglandins.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Maierean SM, Mikhailidis DP, Toth PP, Grzesiak M, Mazidi M, Maciejewski M, et al. The potential role of statins in preeclampsia and dyslipidemia during gestation: A narrative review. Expert Opin Investig Drugs. 2018;27:427–35. doi: 10.1080/13543784.2018.1465927. [DOI] [PubMed] [Google Scholar]
- 18.Patra S, Bhattacharya S, Bala A, Haldar PK. Antidiabetic effect of Drymaria cordata leaf against streptozotocin-nicotinamide-induced diabetic albino rats. J Adv Pharm Technol Res. 2020;11:44–52. doi: 10.4103/japtr.JAPTR_98_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aragon-Charris J, Reyna-Villasmil E, Guerra-Velasquez M, Mejia-Montilla J, Torres-Cepeda D, Santos-Bolívar J, et al. Atherogenic index of plasma in patients with preeclampsia and in healthy pregnant women. Med Clin (Barc) 2014;143:104–8. doi: 10.1016/j.medcli.2013.05.037. [DOI] [PubMed] [Google Scholar]
- 20.Al-Naimi MS, Hussien NR, Rasheed HA, Al-Kuraishy HM, Al-Gareeb AI. Levothyroxine improves Paraoxonase (PON-1) serum levels in patients with primary hypothyroidism: Case-control study. J Adv Pharm Technol Res. 2018;9:113–8. doi: 10.4103/japtr.JAPTR_298_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reddy SG, Rajendra Prasad CSB. Significance of platelet indices as severity marker in nonthrombocytopenic preeclampsia cases. J Lab Physicians. 2019;11:186–91. doi: 10.4103/JLP.JLP_161_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dutta S, Lai A, Scholz-Romero K, Shiddiky MJA, Yamauchi Y, Mishra JS, et al. Hypoxia-induced small extracellular vesicle proteins regulate proinflammatory cytokines and systemic blood pressure in pregnant rats. Clin Sci (Lond) 2020;134:593–607. doi: 10.1042/CS20191155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chulkov V, Syundyukova E, Medvedev B, Sashenkov S. Peculiarities of placental expression of erythropoietin in preeclampsia. Pregnancy Hypertension. 2018;13:S125–6. [Google Scholar]
- 24.Susilowati R, Jannah J, Maghfuroh Z, Kusuma MT. Antihyperlipidemic effects of apple peel extract in high-fat diet-induced hyperlipidemic rats. J Adv Pharm Technol Res. 2020;11:128. doi: 10.4103/japtr.JAPTR_28_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Urakov AL, Mustafin IG, Samorodov AV, Kamilov FK, Khaliullin FA. The off-label use of drugs for parenteral nutrition as a solvent of substances slightly soluble in water in pharmacological research. J Adv Pharm Technol Res. 2018;9:9–14. doi: 10.4103/japtr.JAPTR_280_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shih CM, Lin FY, Yeh JS, Lin YW, Loh SH, Tsao NW, et al. Dysfunctional high density lipoprotein failed to rescue the function of oxidized low density lipoprotein-treated endothelial progenitor cells: A novel index for the prediction of HDL functionality. Transl Res. 2019;205:17–32. doi: 10.1016/j.trsl.2018.09.005. [DOI] [PubMed] [Google Scholar]


