Abstract
The coronavirus disease 2019 (COVID-19) pandemic is a major threat to global health. Relevant studies have shown that ambient temperature may influence the spread of novel coronavirus. However, the effect of ambient temperature on COVID-19 remains controversial. Human mobility is also closely related to the pandemic of COVID-19, which could be affected by temperature at the same time. The purpose of this study is to explore the underlying mechanism of the association of temperature with COVID-19 transmission rate by linking human mobility. The effective reproductive number, meteorological conditions and human mobility data in 47 countries are collected. Panel data models with fixed effects are used to analyze the association of ambient temperature with COVID-19 transmission rate, and the mediation by human mobility. Our results show that there is a negative relationship between temperature and COVID-19 transmission rate. We also observe that temperature is positively associated with human mobility and human mobility is positively related to COVID-19 transmission rate. Thus, the suppression effect (also known as the inconsistent mediation effect) of human mobility is confirmed, which remains robust when different lag structures are used. These findings provide evidence that temperature can influence the spread of COVID-19 by affecting human mobility. Therefore, although temperature is negatively related to COVID-19 transmission rate, governments and the public should pay more attention to control measures since people are more likely to go out when temperature rising. Our results could partially explain the reason why COVID-19 is not prevented by warm weather in some countries.
Keywords: COVID-19, Temperature, Human mobility, Suppression effect, Mediation analysis
Author contribution
Wenjing Shao, Data curation, Writing- Original draft preparation, Visualization, Investigation. Jingui Xie, Conceptualization, Methodology, Supervision. Yongjian Zhu, Methodology, Validation, Writing-reviewing and editing.
1. Introduction
The COVID-19 outbreak was first detected in Wuhan, China. In recent weeks, the outbreak in China has been effectively contained, while novel coronavirus pneumonia has spread around the world. On January 13, 2020, novel coronavirus pneumonia was first diagnosed in a country (Thailand) other than China. According to the statistics of the World Health Organization, there have been more than 20 million confirmed cases of COVID-19 and more than 735,000 deaths worldwide as of August 5, 2020 (World Health Organization, 2020).
There are many factors that influence the spread of the COVID-19. In particular, temperature is an important factor. Both epidemiological and laboratory studies indicated that the effect of ambient temperature on the survival and transmission of coronavirus could not be ignored (Chan et al., 2011; Van Doremalen et al., 2013; Xie and Zhu, 2020). Thus, it is necessary to explore the effect of temperature on novel coronavirus transmission. Some studies have explored the connection between temperature and novel coronavirus. But the conclusion is controversial. On the one hand, temperature can influence the spread of COVID-19 (Tobias and Molina, 2020; Holtmanna et al., 2020; Wu et al., 2020). A study suggested that rising temperatures could reduce the number of COVID-19 cases (Mandal and Panwar, 2020). The results of Prata et al. (2020) also showed that there was a negative linear relationship between temperature and the number of confirmed cases for all 27 state capital cities in Brazil from February 27, 2020 to April 1, 2020, which was characterized by tropical temperature. On the other hand, some studies have reported the opposite finding that the transmission of novel coronavirus does not depend on temperature. Compared with temperature, a recent study showed that the rate of COVID-19 transmission was more susceptible to other factors, such as population density, population by age and number of travelers (Briz-Redón et al., 2020). Another study showed no association of COVID-19 transmission with temperature or UV radiation in 224 Chinese cities from early January to early March (Yao et al., 2020). Jahangiri et al. (2020) confirmed that novel coronavirus transmission rate had low sensitivity to temperature in different Iranian provinces from February 15, 2020 to March 22, 2020.
Moreover, previous studies have verified the relationships between weather conditions including temperature and outdoor activities or travel behaviors (Matthews et al., 2001; Bocker et al., 2016; Liu et al., 2014). It is commonly believed that people may prefer to participate in outdoor activities or travel in warm weather. For example, in the urban transport system, Arana et al. (2014) showed that warm weather was conducive to transit ridership and cold weather reduced ridership in Spain on all weekends (Saturdays and Sundays) journeys in 2010 and 2011. Good weather conditions could conduce individuals’ travel to leisure destinations. Cools et al. (2010) suggested that warm, cold and snowy days significantly affected travel planning, and the choice of travel mode was mainly influenced by fog and storms based on a survey of 586 Flanders respondents. People tend to choose a closer destination for activities in severe weather conditions, especially in the case of heavy rain and extremely cold temperatures.
There are also some studies that have examined the impact of human mobility on the COVID-19 transmission. The analysis of Zhu et al. (2020a, 2020b) showed that there was a significant positive relationship between the human mobility and daily COVID-19 confirmed cases in 120 cities from China between January 23, 2020 and February 29, 2020. A study by Oztig and Askin (2020) observed a positive correlation between a country's air passenger volume and the number of COVID-19 patients in 144 countries. It was further found that countries with more airports had a higher number of COVID-19 cases. The results of Badr et al. (2020) showed that mobility patterns were closely related to the growth rate of COVID-19 cases in the worst-affected counties in the United States. A study by Cartenì et al. (2020) believed that mobility habit was one of the variables, along with the number of daily tests and environmental variables, that explained the number of COVID-19 infections. The details about the above studies are summarized in Table S1.
Therefore, human mobility is not only closely related to the pandemic of COVID-19, but also affected by temperature at the same time. Explore the underlying mechanism of the association of temperature with COVID-19 transmission by linking human mobility may be useful to explain the controversial conclusion in the literatures. In this study, we aimed to investigate the relationship between ambient temperature and COVID-19 transmission, and the mediation by human mobility in 47 countries.
2. Materials and methods
2.1. Data collection
The effective reproductive number (R) is often used as the primary indicator of COVID-19 transmission rates and plays an important role in epidemiology (Xiao et al., 2020). It measures the average number of people infected by a single infected person during the period of infection. We collected the data for the estimates of R from February 22, 2020 to June 22, 2020 (time span varies by country and the starting point is the date when the number of confirmed cases in a country reaches 100) from a previous work by Arroyo-Marioli et al. (2020). To construct this proxy, they used data on new cases, recoveries, and deaths and estimated the growth rate by Kalman-filtering techniques. Arroyo-Marioli et al. (2020) believed that “the method is robust in the sense that the estimates of R remain fairly accurate even when new cases are imperfectly measured, or the true dynamics of the disease do not follow the SIR model”. Readers are referred to Arroyo-Marioli et al. (2020) for the details of estimating the reproductive number.
The meteorological data were obtained from the National Oceanic and Atmospheric Administration Center (https://www.ncdc.noaa.gov/isd). Based on previous studies on the effects of climate on influenza viruses and coronaviruses (Chan et al., 2011; Van Doremalen et al., 2013; Zhu et al., 2020a, 2020b), we selected three major meteorological factors, namely mean temperature, air pressure and wind speed. For each country, we averaged meteorological data at different meteorological stations to calculate the average daily data during the observation period. Table S2 reportes the number of meteorological stations in each country.
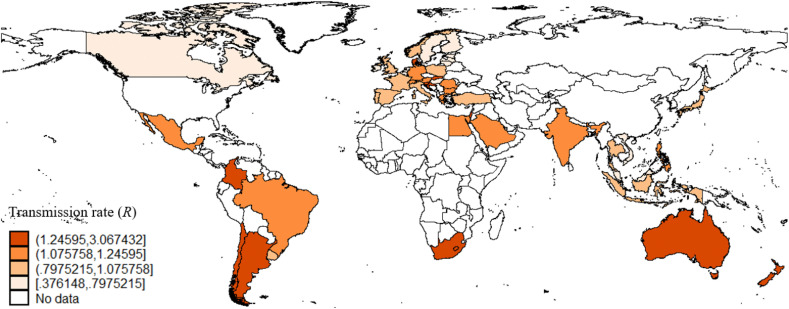
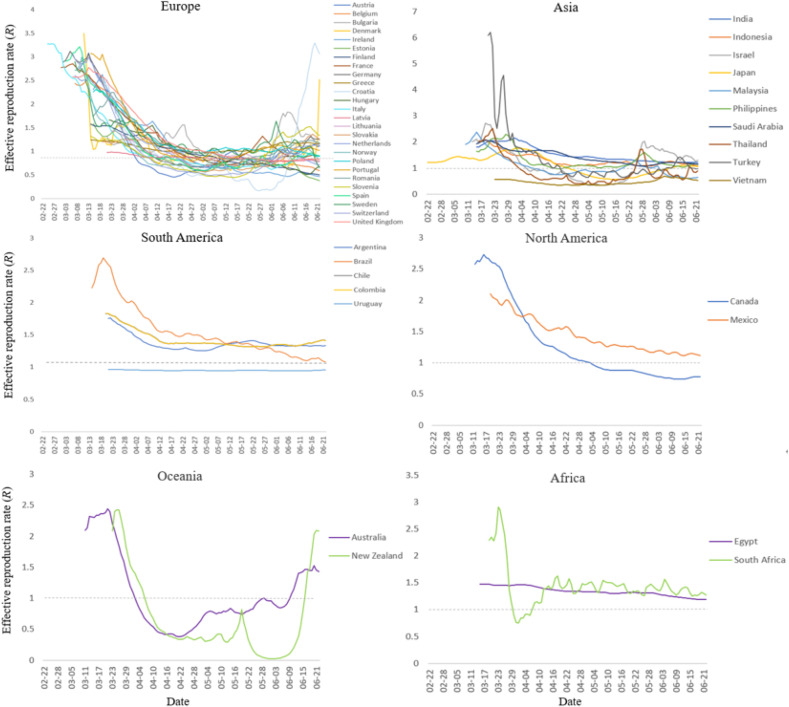
Human mobility data were collected from the Mobility Trends Reports provided by Apple, which reflects the relative volume of directional requests (the baseline is the volume on January 13, 2020) through the Apple Maps app. Apple's data include three kinds of mobility: driving, walking, and transit. These three types of mobility data are highly correlated with each other (Table 2). Therefore, we analyzed each mobility data separately to avoid the influence of collinearity. The final sample studied in our analysis includes 4056 observations from 47 countries during the 122-day observation period from February 22, 2020 to June 22, 2020 (Fig. 1 ). Fig. 2 plots the trend of R for 47 countries on six continents.
Table 2.
Spearman correlation coefficients between meteorological variables and human mobility.
| Mean |
Air |
Wind |
Driving |
Walking |
Transit |
|
|---|---|---|---|---|---|---|
| temperature | pressure | speed | mobility | Mobility | Mobility | |
| Mean temperature | 1.000 | |||||
| Air pressure | −0.180* | 1.000 | ||||
| Wind speed | −0.407* | 0.096* | 1.000 | |||
| Driving mobility | −0.064* | −0.059* | 0.251* | 1.000 | ||
| Walking mobility | −0.135* | −0.002 | 0.263* | 0.940* | 1.000 | |
| Transit mobility | −0.054* | −0.089* | 0.154* | 0.915* | 0.898* | 1.000 |
*p < 0.05.
Fig. 1.
Locations of 47 countries and transmission rate (R) in each country as of June 22, 2020.
Fig. 2.
The time trend of the effective reproduction rate (R) of COVID-19 for 47 countries on six continents.
2.2. Statistical analysis
We used panel data models with fixed effects to study the association between daily mean temperature, human mobility and transmission rates. Considering the incubation period of COVID-19 (typically 2–14 days) (Lombardi et al., 2020), we applied the moving-average approach to investigate the moving average lag effect of mean temperature and human mobility on transmission rates, with a lag of 3 days, 7 days and 14 days, respectively. Our analyses include two parts. In the first part, we examined the relationship between temperature and transmission rates. The model is as follows:
| (1) |
where and represent the country and the date, respectively. is the effective reproductive number (a proxy for COVID-19 transmission rates) in on . denotes the l day moving average term (lag1-l) of daily mean temperature in country i. X il represents other meteorological variables as confounding factors including air pressure and wind speed for the same period. β 1 identifies the impact of temperature on transmission rates. We controlled time-invariant countries characteristics by including the country fixed effect captures time fixed effect. is an error term.
In the second part, the mediation analysis is conducted to test the mediation by human mobility of the association between temperature and transmission rates. That is, temperature not only has a direct effect on transmission rates but may also affects transmission rates indirectly through human mobility. Specifically, the suppression effect occurs when direct and mediated effects of temperature have opposite signs, which is also called the inconsistent mediation effect (McFatter, 1979). According to the process of mediation analysis (Wen et al., 2014), two models are defined as follows:
| (2) |
| (3) |
where M il denotes the l day moving average of Apple human mobility (driving, walking, or transit) in country i.
Equations (1), (2), (3) constitute a complete mediation analysis. The first step is to test whether the regression coefficient β 1 is statistically significant in Equation (1); the second step is to test whether the regression coefficient α 1 in Equation (2) is statistically significant; the third step is to test whether the regression coefficients γ1, γ2 in Equation (3) are statistically significant. If β 1, α 1, γ 1 and γ 2 are all significant, and the indirect effect (α 1 × γ 2) has the opposite sign of the direct effect (γ 1), the suppressing effect of human mobility is confirmed. Including a suppressor in Equation (3) could make the absolute value of the total effect of temperature on the transmission rate (β 1) less than the absolute value of the direct effect (γ 1) (Mackinnon et al., 2000).
In the sensitivity analysis, we further added country-specific linear time trend in our models, which could control the unobservable country-level factors that evolved over time (Liu and Bharadwaj., 2020). The details about the models and equations are reported in the online supplement.
3. Results
3.1. Descriptive analysis
Table 1 summarizes the descriptive statistics of meteorological variables, human mobility, and transmission rate in the study. During the observation period (February 22, 2020 to June 22, 2020), the average of transmission rate is 1.212. Average daily mean temperature, air pressure and wind speed are 15.352 °C, 1014.524 hPa and 9.629 m/s, respectively. The average of driving mobility, walking mobility and transit mobility are −33.614, −42.898 and −55.825, respectively.
Table 1.
Descriptive statistics of transmission rate, meteorological variables and human mobility.
| Mean |
SD |
Min |
Percentile |
Max |
|||
|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | |||||
| Effective reproductive number | 1.212 | 0.571 | 0.025 | 0.830 | 1.104 | 1.439 | 6.202 |
| Mean temperature (◦C) | 15.352 | 8.330 | −10.970 | 9.714 | 14.553 | 21.329 | 34.183 |
| Air pressure (hPa) | 1014.524 | 7.222 | 982.047 | 1009.990 | 1013.811 | 1018.869 | 1046.942 |
| Wind speed (m/s) | 9.629 | 4.091 | 2.665 | 6.356 | 8.953 | 11.142 | 24.682 |
| Driving mobility | −33.614 | 36.061 | −91.260 | −60.890 | −40.610 | −10.260 | 130.560 |
| Walking mobility | −42.898 | 31.570 | −94.180 | −67.220 | −48.790 | −25.810 | 120.670 |
| Transit mobility | −55.825 | 28.316 | −92.960 | −77.735 | −64.280 | −40.480 | 60.560 |
Table 2 shows the spearman correlation coefficients between the meteorological variables and mobility data in Apple's reports. Mean temperature have significantly negative correlations with air pressure (r = −0.180, p < 0.05), wind speed (r = −0.407, p < 0.05), driving mobility (r = −0.064, p < 0.05), walking mobility (r = −0.135, p < 0.05) and transit mobility (r = −0.054, p < 0.05). Correlations between three types of mobility data are high.
3.2. Regression results
The columns (1), (4) and (7) in Table 3 show the moving average lag effects (lag1-3, lag1-7, lag1-14) of temperature on transmission rate of COVID-19 using Equation (1). We observed significant negative relationships between temperature and transmission rate of COVID-19 at all three lag levels. One degree increase in temperature is associated with a 0.012 (95% CI: −0.015 to −0.008) decrease in COVID-19 transmission rate at lag1-3, a 0.015 (95% CI: −0.019 to −0.011) decrease in transmission rate at lag1-7 and a 0.021 (95% CI: −0.025 to-0.017) decrease in transmission rate at lag1-14. These results indicated that the negative moving-average effect of temperature became stronger as the lag days accumulated, which is possibly caused by the incubation period of COVID-19.
Table 3.
Suppressing effects of walking mobility on the association between mean temperature and COVID-19 transmission rate.
| Lag1-3 |
Lag1-7 |
Lag1-14 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Effective reproductive number (1) | Walking mobility (2) | Effective reproductive number (3) | Effective reproductive number (4) | Walking mobility(5) | Effective reproductive number (6) | Effective reproductive number (7) | Walking mobility (8) | Effective reproductive number (9) |
| Mean temperature | −0.012*** | 1.529*** | −0.025*** | −0.015*** | 1.531*** | −0.031*** | −0.021*** | 1.312*** | −0.036*** |
| (-0.015,-0.008) | (1.368,1.691) | (-0.029, −0.022) | (-0.019, −0.011) | (1.362,1.701) | (-0.034,-0.027) | (-0.025,-0.017) | (1.136,1.488) | (-0.040,-0.033) | |
| Walking mobility | 0.009*** | 0.010*** | 0.012*** | ||||||
| (0.008,0.010) | (0.010,0.011) | (0.011, 0.013) | |||||||
| Control variablesObservations | YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
YES 4056 |
The rest of the columns in Table 3 show the estimated results of our mediation analysis. The temperature is positively associated with walking mobility, and walking mobility is positively related to COVID-19 transmission rate. So, the indirect effect has the opposite sign of the direct effect. The regression results strongly support our hypothesis that walking mobility has a statistically significant suppression effect on the association between temperature and COVID-19 transmission rate.
The estimated results of the other two human mobility indicators (driving and transit) are shown in Tables S3–S4 separately, which are similar to the results of walking mobility. In the sensitivity analysis, the results are still robust (Tables S5–S7).
4. Discussion
The purpose of this paper is to explore the underlying mechanism of the association of temperature with COVID-19 transmission by assessing the suppression effect of human mobility. In this study, we observed that temperature was negatively associated with transmission rate. The mediation analysis showed that human mobility had a suppression effect on the relationship between temperature and COVID-19 transmission rate, providing evidence that temperature could influence the spread of COVID-19 by affecting human mobility.
Our results are consistent with previous studies. First, for the relationship between temperature and the transmission of COVID-19. A laboratory study found that SARS-CoV-2 was highly stable at 4 °C, but sensitive to heat. As temperature rose to 70 °C, the virus inactivation time decreased to 5 min (Chin et al., 2020). Biryukov et al. (2020) observed that SARS-CoV-2 decayed more rapidly when temperature was increased. Li et al. (2020) believed that temperature was an important meteorological parameter that maintains a well negative correlation with COVID-19 incidence in Wuhan and Xiaogan. Most studies suggest that high temperatures are detrimental to the virus ability to survive.
Second, for the association of temperature with human mobility, previous studies have found a significant relationship between outdoor activities and temperature (Suminski et al., 2008; Xi et al., 2020). A study has shown that physical activity during adolescence is higher in the warmer months (Belanger et al., 2009), which is consistent with our finding. Temperature could be associated with behavioral patterns that increase human exposure to coronavirus, and accelerate the spread of COVID-19.
Third, for the relationship between human mobility and COVID-19 transmission rate. Since COVID-19 could be transmitted by aerosols and could travel a certain distance along air currents, leading to long-distance transmission of the disease (Wax and Christian, 2020; Van Doremalen et al., 2020), most people are susceptible to infection through respiratory droplets and direct contact (Shi et al., 2020). Zhou et al. (2020) revealed that mobility reduction had a significant impact on controlling the spread of COVID-19 across the ten regions of Shenzhen. Besides, a study suggested that asymptomatic carriers could also spread the virus (Gabutti et al., 2020). Thus, there is a positive relationship between population mobility and transmission rate. According to an article (Lai et al., 2020), timely and effective quarantine measures and travel restrictions in China are the key to controlling the epidemic. The number of cases would have increased 67 times without these measures. These features of novel coronavirus infection also highlight the need to strengthen physical isolation by increasing social distance to reduce the chance of transmission of novel coronavirus.
Our research has some implications. First, we found that temperature was negatively related to the transmission rate of COVID-19. However, governments should still take necessary human mobility restrictions during warm weather since people are more likely to go out when temperature rising. Besides, the suppression effect of human mobility could partially explain the current controversial conclusions in studies about the effect of temperature on COVID-19 transmission, which may also give us the reason why COVID-19 is not prevented by warm weather in some countries.
However, this paper also has some limitations. First, the average mean temperature in all available meteorological stations is used to represent the temperature of each country. So, exposure measurement error is inevitable in this study. Second, human mobility indicators from Apple are generated by the number of navigation requests made to Apple maps. On a country-level study, these variables could be largely biased. Third, although we added fixed effects in our models, a large number of confounders were still not controlled, which may affect the results.
5. Conclusion
This paper provides evidence that temperature can influence the spread of COVID-19 by affecting human mobility. Therefore, although temperature is negatively related to COVID-19 transmission rate, governments and the public should pay more attention to control measures since people are more likely to go out when temperature rising. Our results could partially explain the reason why COVID-19 is not prevented by warm weather in some countries.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research was supported by the National Natural Science Foundation of China (NSFC) with grant Nos: 71921001 and 71571176.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110608.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Arroyo-Marioli F., Bullano F., Kucinskas S., Rondón-Moreno C. Tracking R of COVID-19: a new real-time estimation using the kalman filter. 2020. [DOI] [PMC free article] [PubMed]
- Arana P., Cabezudo S., Peñalba M. Influence of weather conditions on transit ridership: a statistical study using data from Smartcards. Transport. Res. Pol. Pract. 2014;59:1–12. doi: 10.1016/j.tra.2013.10.019. [DOI] [Google Scholar]
- Bocker L., Dijst M., Faber J. Weather, transport mode choices and emotional travel experiences. Transport. Res. Pol. Pract. 2016:360–373. doi: 10.1016/j.tra.2016.09.021. [DOI] [Google Scholar]
- Badr H.S., Du H., Marshall M., Dong E., Squire M.M., Gardner L.M. The Lancet Infectious Diseases. 2020. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belanger M., Graydonald K., Oloughlin J., Paradis G., Hanley J.A. Influence of weather conditions and season on physical activity in adolescents. Ann. Epidemiol. 2009;19(3):180–186. doi: 10.1016/j.annepidem.2008.12.008. [DOI] [PubMed] [Google Scholar]
- Biryukov J., Boydston J.A., Dunning R.A., Yeager J.J., Wood S., Reese A.L., Ferris A., Miller D., Weaver W., Zeitouni N.E., Phillips A., Freeburger D., Hooper I., Ratnesar-Shumate S., Yolitz J., Krause M., Williams G., Dawson D.G., Herzog A., Dabisch P., Wahl V., Hevey M.C., Altamura L.A. Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on surfaces. mSphere. 2020;5(4):20. doi: 10.1128/mSphere.00441-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redón A., Serrano-Aroca A. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cools M., Moons E., Creemers L., Wets G. Changes in travel behavior in response to weather conditions: do type of weather and trip purpose matter? Transport. Res. Rec. 2010;2157(1):22–28. doi: 10.3141/2157-03. [DOI] [Google Scholar]
- Cartenì A., Francesco L.D., Martino M. How mobility habits influenced the spread of the COVID-19 pandemic: results from the Italian case study. Sci. Total Environ. 2020;741:140489. doi: 10.1016/j.scitotenv.2020.140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K., Peiris J.S., Lam S.Y., Poon L.L., Yuen K., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Advances in Virology. 2011:734690. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A., Chu J., Perera M., Hui K., Yen H., Chan M., Peiris M., Poon L. Stability of SARS-CoV-2 in different environmental conditions. Lance. 2020 doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabutti G., d'Anchera E., Sandri F., Savio M., Stefanati A. Coronavirus: update related to the current outbreak of COVID-19. Infect. Dis. Ther. 2020;9:241–253. doi: 10.1007/s40121-020-00295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtmanna M., Jonesb M., Shahc A., Holtmann G. Low ambient temperatures are associated with more rapid spread of COVID-19 in the early phase of the endemic. Environ. Res. 2020;186:109625. doi: 10.1016/j.envres.2020.109625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangiri M., Jahangiri M., Najafgholipourb M. The sensitivity and specificity analyses of ambient temperature and population size on the transmission rate of the novel coronavirus (COVID-19) in different provinces of Iran. Sci. Total Environ. 2020;728:138872. doi: 10.1016/j.scitotenv.2020.138872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Susilo Y.O., Karlstrom A. Examining the impact of weather variability on non-commuters’ daily activity–travel patterns in different regions of Sweden. J. Transport Geogr. 2014:36–48. doi: 10.1016/j.jtrangeo.2014.06.019. [DOI] [Google Scholar]
- Liu J., Bharadwaj A. Drug abuse and the internet: evidence from craigslist. Manag. Sci. 2020;66(5):2040–2049. doi: 10.1287/mnsc.2019.3479. [DOI] [Google Scholar]
- Li H., Xu X., Dai D., Huang Z., Ma Z., Guan Y. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai S., Ruktanonchai N.W., Zhou L., et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020 doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi A., Bozzi G., Mangioni D., Muscatello A., Peri A.M., Taramasso L., Gori A. Duration of quarantine in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a question needing an answer. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon D.P., Krull J.L., Lockwood C.M. Equivalence of the mediation, confounding and suppression effect. Prev. Sci. 2000;1(4):173–181. doi: 10.1023/A:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFatter R.M. The use of structural equation models in interpreting regression equations including suppressor and enhancer variables. Appl. Psychol. Meas. 1979;3(1):123–135. doi: 10.1177/014662167900300113. [DOI] [Google Scholar]
- Mandal C.C., Panwar M.S. Can the summer temperatures reduce COVID-19 cases? Publ. Health. 2020;185:72–79. doi: 10.1016/j.puhe.2020.05.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oztig L.I., Askin O.E. Human mobility and coronavirus disease 2019 (COVID-19): a negative binomial regression analysis. Publ. Health. 2020;185:364–367. doi: 10.1016/j.puhe.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suminski R.R., Poston W.C., Market P., Hyder M.L., Sara P.A. Meteorological conditions are associated with physical activities performed in open-air settings. Int. J. Biometeorol. 2008;52(3):189–197. doi: 10.1007/s00484-007-0110-y. [DOI] [PubMed] [Google Scholar]
- Shi Y., Wang G., Cai X., et al. An overview of COVID-19. J. Zhejiang Univ. - Sci. B. 2020;21:343–360. doi: 10.1631/jzus.B2000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A., Molina T. Is temperature reducing the transmission of COVID-19? Environ. Res. 2020;186:109553. doi: 10.1016/j.envres.2020.109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N., Bushmaker T., Munster V. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18:20590. doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M., Gamble A., Williamson B.N., Tamin A., Harcourt J., Thornburg N., Gerber S., Lloyd-Smith J., Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z., Ye B. Analyses of mediating effects: the development of methods and models. Adv. Psychol. Sci. 2014;22(5):731–745. doi: 10.3724/SP.J.1042.2014.00731. [DOI] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., Du M., Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Canadian Journal of Anaesthesia-journal Canadien D Anesthesie. 2020:1–9. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200805-covid-19-sitrep-198.pdf?sfvrsn=f99d1754_2
- Xiao Y., Tang B., Wu J., Cheke R.A., Tangg S. Linking key intervention timing to rapid decline of the COVID-19 effective reproductive number to quantify lessons from mainland China. Int. J. Infect. Dis. 2020;97:296–298. doi: 10.1016/j.ijid.2020.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi T., Wang Q., Qin H., Jin H. Influence of outdoor thermal environment on clothing and activity of tourists and local people in a severely cold climate city. Build. Environ. 2020;173:106757. doi: 10.1016/j.buildenv.2020.106757. [DOI] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55(5):2000517. doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. The mediating effect of air quality on the association between human mobility and COVID-19 infection in China. Environ. Res. 2020;189:109911. doi: 10.1016/j.envres.2020.109911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Xu R., Hu D., Yue Y., Li Q., Xia J. Effects of human mobility restrictions on the spread of COVID-19 in Shenzhen, China: a modelling study using mobile phone data. Lance. 2020 doi: 10.1016/S2589-7500(20)30165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L., Liu X., Huang H., Avellán-Llaguno R.D., Llaguno Lazo M.M., Gaggero A., Zhu Y. Meteorological impact on the COVID-19 pandemic: a study across eight severely affected regions in South America. Sci. Total Environ. 2020;744:140881. doi: 10.1016/j.scitotenv.2020.140881. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.