Abstract
Coronavirus 2019 disease (COVID-19) has rapidly evolved into a pandemic during the first months of 2020. The general extent of organ involvement, as well as microscopic changes in the organs of the diseased remains insufficiently documented so far.
Herein we are reporting the case of a Caucasian male who apparently died in a workplace allegedly by a fall from height and was found to be SARS-CoV-2 positive just prior to the autopsy. The circumstances of his death required a medicolegal investigation.
Gross autopsy findings included minor external injuries and focal subarachnoid hemorrhage together with ribs and sternum fractures resulting from resuscitation attempt. In addition, visceral congestion was noticed, especially visible in lungs. Traumatic findings suitable to explain sudden death were absent. However, lungs histopathology analysis revealed diffuse alveolar damage with massive capillary congestion. Pathology in other organs included myocardial fibrosis, left ventricular hypertrophy, severe generalized atherosclerosis, glomerulosclerosis, focal liver necrosis, liver microabscesses and intrahepatal cholestasis. Lab test confirmed the presence of SARS-CoV-2 in nasopharygeal swab taken postmortem. Only afterwards, the investigation brought out that he was suffering complaints consistent with respiratory infection in the days before death. Based on all findings, the death was ruled as natural, caused by COVID-19.
Learnings from this case urge medical staff in the autopsy suite to consider the presence of SARS-CoV-2 in sudden deaths during the pandemic, to enable adequate personal protection gear is worn and to ensure the proper cause of death is determined where misleading circumstances exist.
Keywords: SARS-CoV-2/COVID-19 (may be used interchangeably) death, Forensic autopsy, Histopathology, Diffuse alveolar damage, Work-related accident
Case description
The ambulance service operator received a call reporting that the body of a 51-year-old Caucasian male was found near scaffolding, in the yard of a house under construction. Upon arrival, the emergency medical service (EMS) team was informed that the patient was a construction worker who probably fell from the scaffolding installed approximately 3 m above the ground. No other useful medical information was obtained. Initial assessment revealed the absence of vital signs so the resuscitation was commenced immediately. Resuscitation efforts failed and death was pronounced shortly after. Due to the scant information on the events that preceded the death presented to EMS team by people at the scene, the police were informed about the case and the scene investigation team and the coroner arrived. External examination of the body made by the coroner revealed lacerations on both sides of his forehead, minor abrasions on the face and elbows and a bruise on the left hand. Traces of blood were present on the ground near head. A suspicion of violent death under unknown circumstances led to the order for a forensic autopsy consigned by the State Attorney’s office to the Institute of Forensic Medicine and Criminalistics in Zagreb.
Since the resuscitation at the scene had been performed, recently introduced due diligence required taking a postmortem nasopharyngeal swab of the corpse for SARS-CoV-2 analysis. Such analysis, applying the real time reverse transcriptase polymerase chain reaction (RT-PCR), was established for the purpose of risk-assessment for the responders and EMS team members at the first place.
The test result was positive, confirming the presence of SARS-CoV-2 in the postmortal sample taken from the corpse. Therefore, an autopsy was performed under controlled conditions following the recommendations [1,2] requiring the staff fully equipped with personal protective equipment including FFP3 masks, eye protection and gowns.
Additionally, the positive test for the corpse was an indication for taking nasopharyngeal swabs of all EMS team members involved in resuscitation. For all of them, the tests showed negative result meaning that transmission of the virus from the patient to medical staff did not occur.
The police investigation revealed that none of the co-workers eye-witnessed the fall but all of them uniformly stated they suddenly noticed his body lying on the ground. Initial suspicion of physical conflict between the victim and some of the co-workers, leading to victim’s fall, has been raised, but further investigation has given no support for such a scenario. In the absence of any medical records, the only available data concerning the health condition of the deceased were gathered from his co-workers who had been sharing the same accommodation with him for the last ten days. From their statements given to the police, we learned that the deceased suffered from type-2 diabetes and was a smoker for decades. During the week preceding his death, he had been complaining of headache, fatigue, fever, cough, chest discomfort and shortness of breath. He had refused the suggestion to see a doctor and had kept working until the moment he died.
Autopsy findings and cause of death
In the external examination, two linear lacerations, one on each supraorbital region, several abrasions of the face and minor bruises on the left arm, elbows and right knee were noted.
The internal examination revealed subgaleal hematoma and discrete focal subarachnoid hemorrhage in the left temporal-parietal region. There was mild bilateral pleural effusion, the lungs were heavy (L 930 g, R 935 g), voluminous, with markedly reduced air content, dark red to purple in color on cross section with reddish fluid leaking on the cutting surfaces. The heart weighed 375 g with evident left ventricular hypertrophy (1.7 cm), myocardial fibrosis and atherosclerotic changes on coronary arteries but without occlusions or critical stenoses. Severe generalized atherosclerosis was also found.
Samples of internal organs were taken for histopathological analysis and routinely stained with hematoxylin-eosin while body fluids were collected for toxicological analysis.
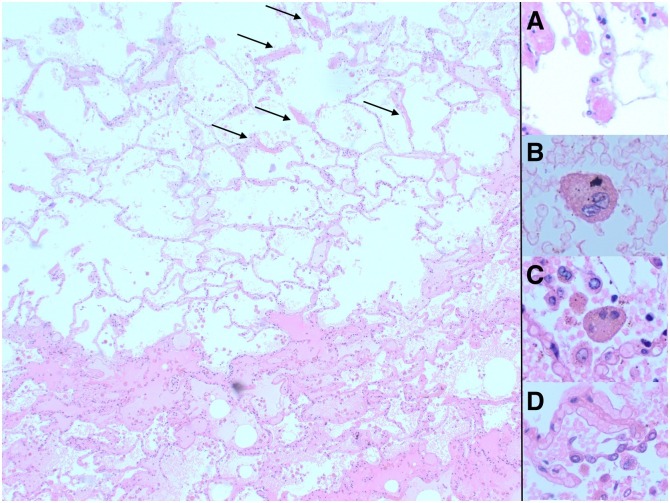
In the lungs, congestion of alveolar septal capillaries and edema within the alveoli were noted diffusely. In addition, diffuse alveolar damage was found with fibrin deposits, formation of hyaline membranes and microthrombi in the capillaries (Fig. 1 ). Alveolar spaces contained siderophages, some multinuclear giant cells and desquamated pneumocytes with regenerative changes. There were no signs of secondary infection, no definitive viral inclusions and no evidence of interstitial fibrosis.
Fig. 1.
Microscopic findings in the lungs. Edema and diffuse alveolar damage in the acute stage. Note hyaline membranes (arrow). A. Microthrombi in the capillaries. B, C. Multinuclear cells inside alveolar spaces. D. Desquamated pneumocytes with regenerative changes.
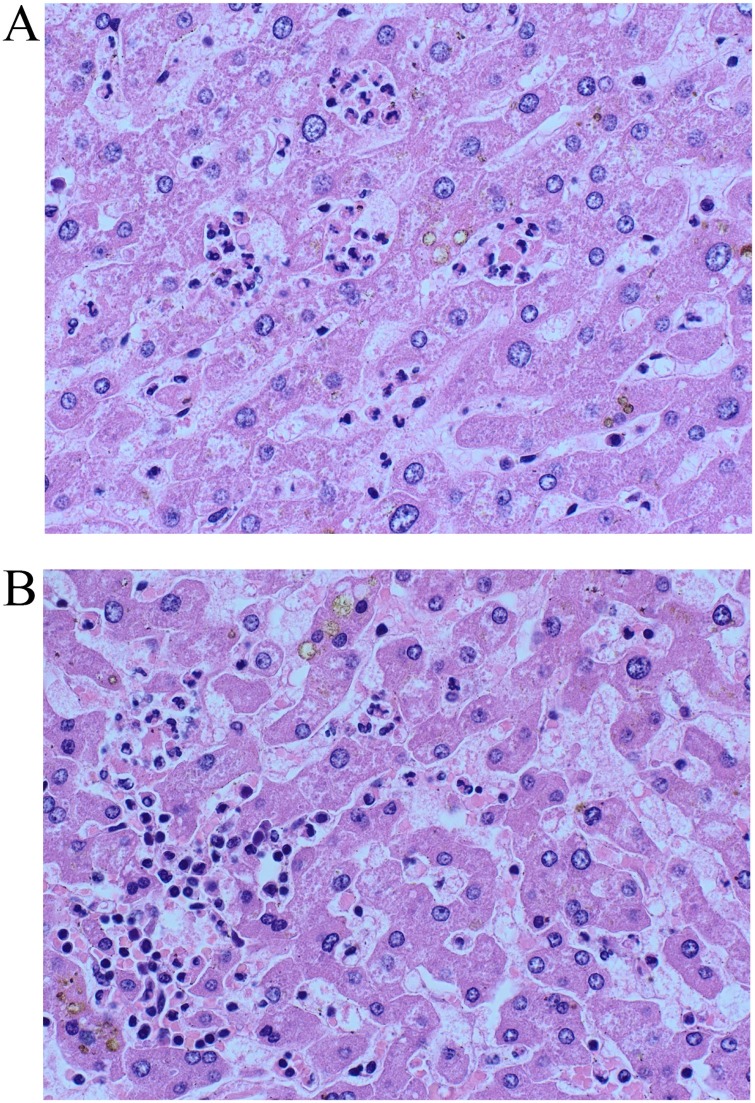
Examination of the liver revealed mild regenerative changes of the hepatocytes without significant steatosis and without cytoplasmic changes of ballooning. Focal hepatocyte necrosis and scattered microabscesses were visible in the parenchyma (Fig. 2 a). We also noticed the intrahepatal cholestasis (Fig. 2b). The portal spaces were unremarkable with no significant inflammation. The sinusoids were dilated and filled with erythrocytes. A large quantity of neutrophils were found inside the sinusoidal spaces.
Fig. 2.
A. Microscopic findings in the liver. Intrahepatal cholestasis, microabscesses and neutrophils in the sinusoidal spaces. B. Microscopic findings in the liver. Intrahepatal cholestasis and focal necrosis.
Proximal tubules of the kidneys were dilated with visible denudation of necrotic epithelial cells intracanalicularly. Some glomeruli showed segmented and global sclerosis and arteriolosclerosis.
Some of the cardiomyocytes were hypertrophic and some were being replaced by fibrous tissue. Interstitium contained focal clusters of lymphocytes in the perivascular distribution, but sections from the heart showed no evidence of myocarditis. Capillaries were filled with abundant neutrophils. In several places surrounding the fibrosis, focal ischemic changes to cardiomyocytes were noted in the form of thinned and more eosinophilic muscle fibers, but without evident neutrophilic infiltration.
Other organs showed no remarkable changes
The following histopathological diagnoses were established: diffuse alveolar damage, pulmonary edema, severe visceral congestion, myocardial fibrosis and left ventricular hypertrophy.
Toxicological analysis was negative
The cause of death was determined to be COVID-19 and the manner of death ruled as natural. By applying WHO guidelines for COVID-19 death certification [3], one should list the acute respiratory distress syndrome (immediate cause) due to COVID-19 (underlying cause), while type-2 diabetes, smoking habit, myocardial hypertrophy and fibrosis and atherosclerosis should be listed as other contributing factors.
Discussion
SARS-CoV-2 is a novel human coronavirus first detected in Wuhan, China in December 2019 [4]. Infection with this virus may progress to acute respiratory distress syndrome (ARDS), sepsis, multi-organ failure, and death [5]. From China, the virus spread globally and as of 31 August 2020 there were 25,118,689 confirmed cases of SARS-CoV-2 infection and 844,312 deaths [6]. The first case in Croatia, recorded on 25 February 2020, was 25-year-old male who arrived from Milan, Italy [7]. The preponderance of cases has led to a proliferation of papers attempting to provide insight into the clinical presentations of this novel virus. Few of these papers report complete autopsy findings because of the potential risk for SARS-CoV-2 to attending staff [1,5,[8], [9], [10], [11], [12], [13]]. The indications to perform an autopsy are also ambiguous. There are currently authors who encourage autopsies of people known to have died from SARS-CoV-2 infection [11] while the others point out that if the death is considered to be due to a confirmed SARS-CoV-2 infection, an autopsy is unlikely to be necessary [1].
The case under consideration is interesting for several reasons; the deceased was a construction worker found dead under a scaffolding, with signs of head trauma. The body was sent for a medico-legal autopsy to determine if death was due to the workplace accident. A full autopsy was performed, despite the presence of proven SARS-CoV-2 infection in the corpse. A violent death was ruled out and the autopsy revealed that death was due to natural causes, specifically by the impact of the viral infection. In addition to the evidence of the changes related and consistent with SARS-CoV-2 infection, the deceased showed histological evidence of pre-existing medical conditions including myocardial fibrosis, left ventricular hypertrophy and severe atherosclerosis, and was known to be diabetic and smoker. The presence of comorbidities in persons dying from COVID-19 is almost a rule. It has been reported that people with certain chronic diseases are prone to severe forms of the disease [[13], [14], [15]]. Recently published papers highlight diabetes mellitus as ranking second as a co-morbidity in infected patients and associated with a less favorable course of the disease [14,15]. Also, the outcome of COVID-19 infection may be more severe in smoking population [14].
Most patients with COVID-19 are asymptomatic or experience mild symptoms. However, others deteriorate progressively and develop acute respiratory distress syndrome [9]. In this particular case, histological findings of diffuse alveolar damage in the lungs were consistent with an early ARDS which appears to be a very common feature of this disease [1,5,[8], [9], [10],12,13,16]. Also, severe capillary congestion, pneumocyte hyperplasia, and the presence of multinuclear giant cells have also been reported [1,5,[8], [9], [10],12,13,16]. Consistent with current publications, there were no definitive viral inclusions or specific cytopathic changes [1,5,8,9]. In the absence of prior medical records on the deceased, we relied on witness statements to determine his condition prior to death. All declared symptoms were conclusive with gradually evolving severe respiratory infection, which removes designation of his death as sudden.
There are reports of acute tubular necrosis (ATN) in the patients who died of SARS-CoV-2 infection [13,17]. Although histologically ATN exhibits similar features to those seen in autolysis occurring post-mortem [13,17], the kidneys were of normal weight (140 g each) and devoid of specific signs of ATN so this condition was excluded and existing changes in the tubules were attributed to autolysis. Arteriosclerosis and segmental glomerulosclerosis were consistent with long-term diabetes.
Severe cyanosis, focal necrosis and microabscesses were present in the liver, together with abundance of neutrophils inside the sinusoids. The presence of neutrophils and focal liver necrosis can be attributed to sepsis, the local effects of the drugs (no known data) but also to the viral attack [18]. Since the liver injury in COVID-19 patients has been reported and liver function tests abnormalities occur in 14–53 % of them [18], microscopic changes in the liver may be related to direct viral attack. As previously reported, normal portal spaces were found on autopsy without evident portal tract inflammation [5,9,18].
There are emerging findings about myocarditis in COVID-19 patients [8] but we did not confirm any sign of myocarditis nor of the inflammatory cellular infiltration in the heart tissue.
The abundance of neutrophils were found in the liver and blood vessels of the heart and lungs. Since there are papers reporting neutrophils as potential mediators of SARS-CoV-2 infection damage [19], we speculate that the neutrophil accumulation observed in our case could be attributed to the same mechanism. Further observations in this area are needed.
Specificity of our case also lies in the fact that the only indication for virus testing was the resuscitation attempt. This is consistent with the actual policy of the Ministry of Health recommending taking a swab for SARS-Cov-2 analysis for each deceased who has been resuscitated prior to death, in order to assess the risk for occupationally-exposed health professionals. Had such a policy not been in place, the autopsy would have been performed in standard conditions so the autopsy team could have been exposed to the virus during the procedure. Delay in performing autopsy caused by waiting for the results of testing is not significant since they routinely arrive within 24 h from the sample submission.
In attempt to unify reporting of COVID-19 casualties, WHO issued the guidelines for certification of that disease as the cause of death [3]. The instructions contained in this document raised some concern among the part of the medical community routinely dealing with death certification. Some authors point out the possibility of over-estimating the number of pandemic victims: by including cases as COVID-19 deaths even when the presence of virus is unconfirmed (i.e. in patients that have not been tested for virus before or after death); and by diminishing the importance of pre-existing diseases, shifting them from the ‘underlying cause of death’ field to the ‘other significant conditions’ field on the death certification form [[20], [21], [22]]. Although the authors of this paper generally believe that the issue of death counting methodology deserves a broad academic discussion to ensure proper and honest mortality statistics in current pandemic, our case left us no doubt when it came to the cause of death determination. Namely, all the evidence collected unequivocally led to the conclusion that COVID-19 was responsible for the lethal outcome of the presented patient.
Cases of assumed natural deaths that end as violent deaths due to unexpected findings at the autopsy are well-known to each forensic medicine practitioner. Our case testifies to the opposite sequence of events, reminding us that the autopsy of putative traumatic death with obvious circumstantial data will not always confirm initial thesis of violence. Faced with the absence of significant traumatic findings, the forensic medical expert should be able to re-focus his/her attention and search for the morphological signs of natural diseases that actually caused death.
Informed by this case, we would like to send a message to healthcare providers working in autopsy suites and to coroners to be vigilant, even with suspected violent deaths, SARS-CoV-2 can be hidden as the natural cause of death. The full autopsy performed on the deceased contributes greatly to the limited data available on the pathological findings in COVID-19 cases.
Key points
-
1
If proper indication exists, SARS-CoV-2 positive status of the deceased should not be the argument against performing forensic (medicolegal) autopsy – of course, with use of appropriate protective equipment.
-
2
Complete autopsy of COVID-19 victim revealed the most prominent changes on lungs, predictably, but also the involvement of the liver, accompanied with preexisting chronic conditions mainly in heart muscle.
-
3
Since the behavior of virus is still incompletely understood so far, we advise postmortem testing of the patients who have undergone CPR attempt as a useful procedure in preventing of the virus spread via EMS team members.
-
4
Collecting of all obtainable data on the deceased should be the routine effort of forensic medicine practitioner, especially in unclear cases where such data can substantially help rounding the picture out.
Authors' contributions
All authors listed were actively involved in the preparation of manuscript and have approved the version to be published.
Declaration of Competing Interest
The authors report no declarations of interest.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
All the data and material used in this manuscript are in the possession of authors.
Code availability
Not applicable.
Ethics approval (include appropriate approvals or waivers)
The presented content completely complies with laws in Croatia and with the ethical standards of the authors’ affiliated institutions. Ethics approval is not needed.
Funding
None of the authors have received any funding for this work.
References
- 1.Hanley B., Lucas S.B., Youd E., Swift B., Osborn M. Autopsy in suspected COVID-19 cases. J. Clin. Pathol. 2020;73:239–242. doi: 10.1136/jclinpath-2020-206522. [DOI] [PubMed] [Google Scholar]
- 2.2020. Croatian Institute of Public Health. Handling of a Patient Deceased Due to COVID-19 and Autopsy Procedures.https://www.hzjz.hr/wp-content/uploads/2020/03/Rukovanje_umrlim.pdf available at. [Google Scholar]
- 3.World Health Organization . 2020. International Guidelines for Certification and Classification (Coding) of Covid-19 as Cause of Death.https://www.who.int/classifications/icd/Guidelines_Cause_of_Death_COVID-19.pdf?ua=1 available at. [Google Scholar]
- 4.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacy J.M., Brooks E.G., Akers J., et al. COVID-19: postmortem diagnostic and biosafety considerations. Am. J. Forensic Med. Pathol. 2020;41:143–151. doi: 10.1097/PAF.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . 2020. Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int available at. [Google Scholar]
- 7.Croatian Institute of Public Health . 2020. COVID-19- First Case Report.https://www.hzjz.hr/priopcenja-mediji/covid-19-priopcenje-prvog-slucaja available at. [Google Scholar]
- 8.Barton M.L., Duval E.J., Stroberg E., Ghosh S., Mukhopadhyay S. COVID-19 autopsies, Oklahoma, USA. Am. J. Clin. Pathol. 2020;153:725–733. doi: 10.1093/ajcp/aqaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wichmann D., Sperhake J.P., Lütgehetmann M., Steurer S., Edler C., Heinemann A., et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann. Intern. Med. 2020;173:268–277. doi: 10.7326/M20-2003. [published online ahead of print, 2020 May 6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pomara C., Li Volti G., Cappello F. COVID-19 deaths: are we sure it is pneumonia? Please, autopsy, autopsy, autopsy! J. Clin. Med. 2020;9:E1259. doi: 10.3390/jcm9051259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S.Y. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menter T., Haslbauer J.D., Nienhold R., Savic S., Hopfer H., Deigendesch N., et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology. 2020 doi: 10.1111/his.14134. [published online ahead of print, 2020 May 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J.J., Dong X., Cao Y.Y., Yuan Y.D., Yang Y.B., Yan Y.Q., et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 15.Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J. Endocrinol. Invest. 2020;43(6):867–869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian S., Xiong Y., Liu H., Guo J., Liao M., Xiao S.Y., et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su H., Yang M., Wan C., Yi L.X., Tang F., Zhu H.Y., et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y., Xiao S.Y. Hepatic involvement in COVID-19 patients: pathology, pathogenesis, and clinical implications. J. Med. Virol. 2020 doi: 10.1002/jmv.25973. [published online ahead of print, 2020 May 5] [DOI] [PubMed] [Google Scholar]
- 19.Barnes B.J., Adrover J.M., Baxter-Stoltzfus A., Borczuk A., Cools-Lartigue J., Crawford J.M., et al. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J. Exp. Med. 2020;217:e20200652. doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cirera L., Segura A., Hernández I. Defunciones por COVID-19: no están todas las que son y no son todas las que están [Deaths by COVID-19: Not all were registered and others should not be accounted for] Gac. Sanit. 2020 doi: 10.1016/j.gaceta.2020.06.006. S0213-9111(20)30139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 22.Newton J. GOV.UK – Public Health England; 2020. Behind the Headlines: Counting COVID-19 Deaths.https://publichealthmatters.blog.gov.uk/2020/08/12/behind-the-headlines-counting-covid-19-deaths/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data and material used in this manuscript are in the possession of authors.