There is growing interest in the role of thrombosis in severe acute respiratory syndrome-coronavirus 2 (SARS-Cov2) and anticoagulation including observations of pulmonary microvascular thrombi at autopsy [1] and improved survival in heparin-treated patients [2]. Abnormalities of coagulation and fibrinolysis are further suggested by SARS-Cov2-associated elevations in fibrinogen and fibrin split products (D-DIMER), which are associated with mortality [3]. In spite of this, SARS-Cov2 often presents with normal measures traditional coagulation tests such as prothrombin time (PT) despite elevated levels of fibrinogen and D-DIMER, failing to satisfy criteria for traditional coagulopathy.
Rotational thromboelastometry (ROTEM) is a point-of-care viscoelastic test of whole blood which provides analysis of multiple components of clot formation, clot firmness and fibrinolysis. ROTEM is commonly used in clinical practice to diagnose disorders of coagulation and fibrinolysis in trauma, transplant and cardiac surgery, and it can also been applied to identify hypercoagulable states. Abnormalities of ROTEM may be predictive of future thromboembolic events. In a series of 313 patients who had ROTEM prior to major non-cardiac surgery, for example, 10 patients with postoperative thromboembolic complications had significantly higher preoperative levels of maximum clot firmness (MCF) and significantly lower clot formation time (CFT) [4]. We therefore sought to evaluate coagulation status using ROTEM young, otherwise previously healthy patients who presented with mild symptoms for 3–4 days March 2020.
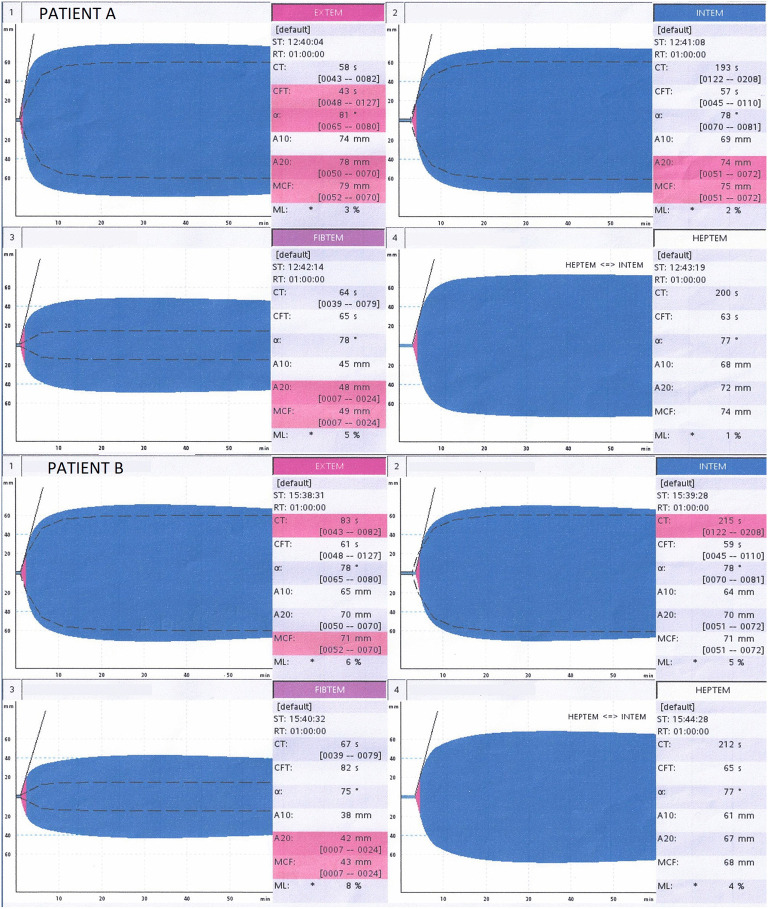
After obtaining consent from the patients, ROTEM was performed on whole blood samples collected on hospitalization day zero. Both patients complained of dyspnea and exhibited moderate hypoxemia, managed with high-flow nasal cannula and bi-level positive airway pressure, respectively. Initial laboratory studies were notable for normal levels of platelets, PT and PTT in both cases; elevated levels of fibrinogen (653 mg/dL and 820 mg/dL; normal, 212–516 mg/dL); and elevated levels of D-DIMER (0.76 μg/mL and 1.33 μg/mL; normal, <0.50 μg/mL). ROTEM findings in both cases (Fig. 1 ) indicated hypercoagulability, with elevated levels of maximum clot firmness (MCF, 71 mm and 79 mm; normal, 52–70 mm) and clot amplitude at 20 min (A20, 70 mm and 78 mm; normal, 50–70 mm) in the EXTEM; as well as elevated levels of MCF (43 mm and 48 mm; normal, 7–24 mm) and A20 (42 mm and 48 mm; normal, 7–24 mm) in the FIBTEM. Collectively, these observations raise alarm that a thrombotic diathesis is present early in the clinical course of SARS-Cov2, possibly prior to hospitalization.
Fig. 1.
ROTEM for patients A and B. EXTEM, extrinsic pathway; INTEM, intrinsic pathway; FIBTEM, fibrinogen activity with platelet inhibitor; HEPTEM, heparin inhibition with heparinase.
Both patients were started on prophylactic anticoagulation therapy. Patient A was initially placed on a heparin infusion, intubated, extubated on day 4 and transitioned to apixaban 5 mg daily until discharge on day 16. Patient B was placed on enoxaparin 60 mg daily, remained on nasal cannula oxygen therapy and was discharged on day 6.
We have received consent from both patients to publish this case. To our knowledge, this communication represents the one of the first few reports in a recently growing literature of ROTEM findings in SARS-Cov2. Our results are consistent with findings of Panigada and colleagues, who identified indices of hypercoagulability in 24 patients with SARS-Cov2 using thromboelastography (TEG) [5]. Unlike TEG, ROTEM provides simultaneous assessment of multiple channels of coagulation. In our analysis, we identified evidence of hypercoagulability as evidenced by shortened time to clot formation and increased clot integrity. Our findings are consistent with not only hyperfibrinogenemia but also hypofibrinolysis. Our findings further underscore the risks of hypercoagulability in the absence of abnormalities in standard laboratory coagulation parameters.
Further research is needed to delineate the onset and evolution of disorder of coagulation and fibrinolysis over the course of SARS-Cov2. Serial performance of ROTEM at different time points in the disease may help to elucidate the natural history of coagulopathy in SARS-Cov2 and its response to therapies.
Disclosures
The authors have received no grants, contracts or financial support for this research project.
CRediT authorship contribution statement
All the authors of the manuscript have read and approved the manuscript and have been extensively involved in formulation, analysis, authorship or revision of this manuscript. ML, MT, SG, DK and HVB designed research, performed research and wrote the paper. KD performed research. JG wrote paper and served at mentor.
Declaration of competing interest
Himani V. Bhatt discloses financial relationships with Neochord, LLC. All other authors have no conflict of interest to disclose.
References
- 1.Fox SE, Akmatbekov A, Harbert JL, Li G, Brown JQ, Vander Heide RS. Pulmonary and cardiac pathology in covid-19: the first autopsy series from New Orleans. medRxiv. doi: 10.1101/2020.04.06.20050575. [DOI] [PMC free article] [PubMed]
- 2.Paranjpe I, Fuster V, Lala A, Russak A, Glicksberg BS, Levin MA et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed]
- 3.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hincker A., Feit J., Sladen R.N., Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18(5):549. doi: 10.1186/s13054-014-0549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed]