The coronavirus disease-2019 (COVID-19) pandemic has prompted a dramatic reorganization of health care systems and medical training programs across the United States. At many hospitals, cardiovascular fellows-in-training (FITs) provide front-line clinical care. The traditional cardiovascular fellowship training paradigm has undergone significant upheaval as a result of physical distancing mandates as well as staffing redeployment strategies (1). The impacts of COVID-19 on physicians, specifically cardiovascular medicine trainees, have not been fully assessed.
In this context, we conducted a national survey of cardiovascular FITs. The objectives of the survey were to describe evolving daily activities of cardiovascular FITs; current strategies to reduce occupational risk; and the educational, social, and psychological implications of working during the COVID-19 pandemic.
The Beth Israel Deaconess Medical Center Fellowship Program, in conjunction with the American College of Cardiology (ACC) Fellows-in-Training Section Leadership Council, developed an online survey of adult and pediatric cardiology FITs which focused on 3 key areas: 1) policies with respect to personal protective equipment (PPE) and concerns about risks of exposure; 2) staffing practices during the pandemic, including redeployment of FITs to noncardiology services and the role of FITs in outpatient clinics and procedures; and 3) the impact of COVID-19 on FIT education.
Invitations to participate in the survey were administered via email to adult and pediatric cardiology fellows through the ACC and Accreditation Council for Graduate Medical Education (ACGME) program fellowship directors. Survey responses were collected from April 6 through April 17, 2020. Respondents completed an online questionnaire using the Qualtrics Online Survey Tool (Provo, Utah). Responses were kept anonymous and de-identified. Authors P.R., J.D, and N.R. undertook an initial review of narrative comments to identify emerging themes. The study was approved by the Institutional Review Board of the Beth Israel Deaconess Medical Center.
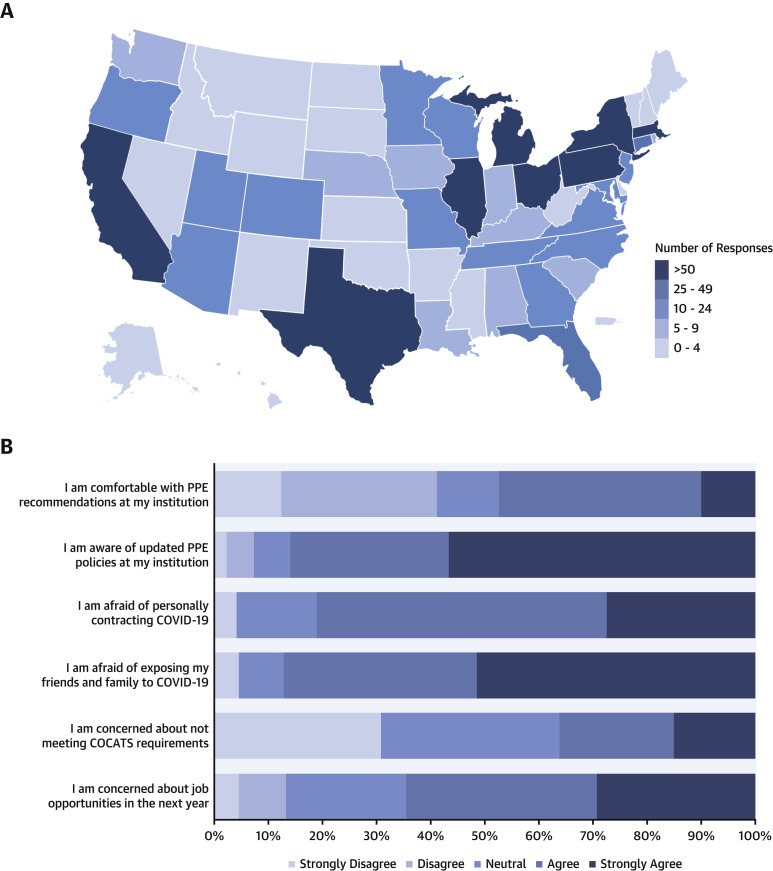
Basic demographic information is shown in Figure 1 . Of the approximately 3,500 FITs at ACGME-accredited pediatric and adult cardiology programs in the United States eligible to participate, 997 responded to the survey. All 50 states, the District of Columbia, and the territory of Puerto Rico are represented (Figure 1). Eighty-seven percent of respondents were general cardiology fellows. The remaining survey participants were advanced fellows representing interventional cardiology (6%), electrophysiology (3%), heart failure (2%), cardiac imaging (2%), and adult congenital heart disease (<1%).
Figure 1.
COVID-19 Impact on Cardiovascular Fellows-in-Training
(A) The geographic distribution of United States survey respondents. Notable in this presentation is the high number of responses from fellows-in-training in fellowship programs in New York, Texas, and California, which are also 3 of the 4 states with the largest number of fellowship programs. (B) Summary of survey responses to key questions regarding PPE, personal exposure and risk of COVID-19 transmission, and career trajectory. COCATS = Core Cardiovascular Training Statement; COVID-19 = coronavirus disease-2019; PPE = personal protective equipment.
Personal Protective Equipment
Eighty-one percent of respondents reported wearing surgical masks for all patient contact, with approximately one-half (51%) reporting wearing N95 masks for all suspected and confirmed COVID-19 patients, whereas 37% using N95 masks only if these patients were intubated or required an aerosol generating procedure. Most FITs were using the same PPE for multiple patients, including N95 masks (74%), surgical masks (50%), and eye protection (55%). Eight percent of fellows reported using homemade masks, scarves, or bandanas when facemasks were unavailable. The majority of respondents (93%) believed that PPE recommendations were affected by current or anticipated supply shortages, and nearly one-third of participants (29%) found it difficult to access PPE at their institution. Of note, 41% were uncomfortable with the current PPE recommendations at their institutions.
Personal Exposure and Risk of Transmission
A majority of fellows were anxious about contracting COVID-19 (81%) and exposing their family or roommate(s) to COVID-19 (87%). Forty-two percent reported changing living circumstances to reduce risk of exposure to family or roommate(s). Sixty-one percent of respondents received guidance on reducing occupational transmission risk out of the hospital. Eighty-six percent identified a known mechanism for notifying senior officials, such as program directors or chief fellows, regarding concerns related to current job responsibilities.
Staffing
COVID-19 has changed the on-call schedule for the majority (69%) of FITs who completed the survey. Respondents reported a decrease in FIT staffing in the echocardiography laboratory (88%), catheterization laboratory (90%), and on cardiology consultation services (43%). There was heterogeneity with regard to cardiac intensive care unit FIT scheduling, with 30% of respondents reporting a decrease and 20% stating an increase in fellow staffing. Many FITs (38%) have been asked to cover noncardiology services. Such redeployment was mandatory for 69% of respondents. Redeployment was more common in states with higher COVID-19 case counts. In states with ≥15,000 reported cases by mid-April 2020, 47% of respondents had been redeployed to cover noncardiology services, whereas 21% of respondents had been redeployed in states with <15,000 reported cases (2). Of those redeployed, approximately one-half (53%) were serving in “back up” roles and had not yet been required to cover noncardiology services. Of those actively working on noncardiology services, the majority were managing both intensive care unit and floor patients (63%), and the remaining were covering either critical care (30%) or floor patients (7%).
With respect to cardiology services, the majority of FITs were performing fewer transthoracic echocardiography studies (69%). While most FITs (62%) were not participating in face-to-face outpatient clinic visits, 66% were engaged in providing care through telemedicine. Nearly three-quarters of respondents (74%) agreed that additional training in performing telemedicine visits would be helpful.
FIT Education
Most respondents (69%) voiced concerns about fulfilling ACC Core Cardiovascular Training Statement (COCATS 4) requirements in advance of graduation. Eighty-eight percent of FITs reported a transition to virtual conferences with 78% reporting an increase in online education content. Of note, 73% of FITs expressed interest in using complementary educational resources such as virtual didactic lessons, board reviews, echocardiography tutorials, procedural simulations, and multicenter collaborative webinars to replace traditional learning modalities.
Career Trajectories
The majority (60%) of FITs were concerned that the economic impact of COVID-19 would jeopardize their future job prospects, and nearly one-half of respondents (48%) believed that the cancellation of national meetings and scientific conferences due to COVID-19 would compromise career and advanced fellowship applications.
Conclusions
Our work represents the most comprehensive assessment of cardiology FITs’ perceptions regarding the impact of the COVID-19 pandemic on cardiovascular fellowship training. Overall, there has been a marked change in training roles and schedules during this period, and FITs are concerned about their personal safety, education, and career prospects.
FITs and institutional leaders acknowledge that the PPE supply shortage has been a critical component of this health crisis (3). In this context, personal safety has been a major concern among FITs. Overwhelmingly, respondents believed that PPE protocols have been affected by shortages or potential shortages and voiced concerns regarding PPE distribution, reuse, rationing, and the institutional communication surrounding these decisions. Many FITs reported following universal masking policies at their institutions, although most would feel more comfortable wearing N95 masks with all patient encounters. Because of the fear of exposing family or roommate(s), many FITs are adjusting their living circumstances during an already uncomfortable and isolating time.
During the COVID-19 pandemic, the ACGME has allowed institutions to self-declare Pandemic Emergency Status, which permits suspension of program requirements—with the exception of mandating adherence to specific training, supervision, and work hour policies—for at least 30 days. Through this provision, traditional rotation schedules created to fulfill COCATS 4 and ACGME requirements have been modified. Many FITs have found themselves in atypical roles such as primary providers or attending physicians and believed that they may incur significant personal risk without commensurate compensation or legal protection. FITs reported fewer procedural training opportunities due to reduced staffing levels and the cancellation of elective and nonurgent procedures. Fellows responding to this survey expressed concerns over a decline in experience in echocardiography, interventional cardiology, electrophysiology, inpatient cardiology, and outpatient clinical care. As a result, almost three-quarters of cardiology FITs surveyed were anxious about not being able to fulfill COCATS 4 requirements.
While many FITs have been asked to use their critical care experience to care for COVID-19 patients, fellows also believed that the current situation affected their opportunities to pursue their career and research goals. Although this trade-off supports advancement of FITs’ skills in critical care medicine, it may come at a cost to their core cardiology career aspirations. Future employers across private, integrated, federal, and academic institutions should remain mindful of the obstacles COVID-19–era FITs may experience during fellow-to-faculty transitions. Formal mentorship programs to nurture FIT development in their early practice should be instituted.
Efforts to continue cardiology-specific training during the pandemic have inspired significant innovation in fellowship medical education and delivery of clinical care. Fellows have newly engaged in the practice of telemedicine, gaining valuable skills that they will use and develop in the future. Many programs have replaced traditional in-person conferences with virtual meetings using web conference technologies (4). In our survey, FITs repeatedly requested increased access to online didactics focused on board review topics and procedural training. The provision of additional virtual didactic content and telemedicine training, either provided by institutions or national cardiology societies, would likely benefit current FITs during COVID-19 pandemic and in the future.
Leaders in cardiovascular medical education will need to re-evaluate current standards of competency and readiness for independent practice. Moreover, the perceptions elicited in this survey highlight an opportunity to improve FIT education and wellbeing. Proactive exploration of educational adaptations and implementing rapid feedback cycles may help to accomplish these goals (5).
We acknowledge limitations with this study. First, although the absolute number of respondents is high, the survey participation rate was approximately 30%; however, this is nearly double the response rate of prior surveys of FITs. Second, sampling bias may have occurred due to the nature of survey administration. Third, the survey was conducted for a 2-week period in early April 2020, during a time when program strategies were evolving which may affect the enduring applicability of these results. Finally, participants were not asked to identify their specific institutions but rather the states in which they are training in order to maintain anonymity. It is possible that these results may not be representative of all training programs across the United States; however, the majority of survey respondents were from programs in New York, Texas, and California, which are 3 of 4 states with the largest number of fellowship programs (30, 18, and 17, respectively).
Cardiology fellowship programs across the country have undergone dramatic changes during the COVID-19 pandemic. It is imperative to ensure that cardiovascular medicine FITs feel adequately protected and supported in their current roles in order to provide high-quality care while maintaining their personal safety. In addition, the implementation of virtual learning opportunities in cardiology has been an important innovation to supplement the FIT educational experience. Programs should continue to harness the feedback from FITs to ensure their ongoing safety, welfare, and education as we navigate this pandemic.
Acknowledgment
The authors thank Kristin West, BA, for her assistance with survey dissemination.
Footnotes
The views expressed in this paper by the American College of Cardiology’s Fellows-in-Training Section Leadership Council do not necessarily reflect the views of the Journal of the American College of Cardiology or the American College of Cardiology.
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 2.COVID-19 Updates: April 17, 2020. American Heart Association Center for Health Metrics and Evaluation. https://healthmetrics.heart.org/wp-content/uploads/2020/04/COVID-19-Updates_4-17-2020.pdf Available at:
- 3.Artenstein A.W. In pursuit of PPE. N Engl J Med. 2020;382:e46. doi: 10.1056/NEJMc2010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almarzooq Z., Lopes M., Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in graduate medical education. J Am Coll Cardiol. 2020;75:2635–2638. doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeFilippis E.M., Stefanescu Schmidt A.C., Reza N. Adapting the educational environment for cardiovascular fellows-in-training during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2630–2634. doi: 10.1016/j.jacc.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]