Shared accommodation, equipment, and staff movement enhance healthcare transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Pre- or asymptomatic coronavirus disease 2019 (COVID-19) poses a silent risk. In our adult tertiary hospital, with more than 800 beds, mostly multi-occupancy, capacity often exceeds 100%. There are just 136 single (77% en suite) and 12 airborne isolation rooms. Emergency department (ED) admissions with suspected COVID-19 are assigned to the COVID-19 pathway, with infection prevention and control (IPC) precautions. Where COVID-19 is not suspected (i.e. asymptomatic nor a contact of a COVID-19 case), a ‘non-COVID-19 pathway’ is assigned, with multi-occupancy accommodation, unless an alternative reason for IPC precautions exists. Daily on-site testing commenced on March 16th, 2020 using the CerTest ViaSure SARS-CoV-2 real-time polymerase chain reaction (PCR) or Cepheid Xpert® Xpress SARS-CoV-2. On March 31st, universal staff mask use in clinical areas was implemented, and extended to communal spaces on August 10th.
Concerns about an undetected asymptomatic COVID-19 admission to multi-occupancy accommodation resulting in onward transmission prompted implementation of SARS-CoV-2 universal admission testing (UAT). From June 1st, 2020 nasopharyngeal swabs were taken in the ED upon admission decision. IPC and occupational health determination of acquisition, risk assessment and contact tracing was performed if COVID-19 was newly confirmed in an inpatient (e.g. delayed recognition of community or hospital infection) or a staff member (e.g. community or occupational infection).
We describe our experience of UAT for SARS-CoV-2 in non-COVID-19 pathway emergency admissions (June 1st to September 20th, 2020), to assess (i) the UAT detection rate and (ii) the impact on patient and staff contact tracing. Patients with COVID-19 already confirmed before admission and beyond their period of infectiousness were excluded [2]. Close contacts were tested for SARS-CoV-2 on day zero and day seven [2]. Staff were advised to restrict their movements and remain off work for 14 days and patients were either isolated or cohorted with other close contacts for 14 days, or advised to restrict movements if discharged within 14 days.
Statistical analysis was performed using Stata version 15.0 (Statacorp, College Station, TX, USA). Independent sample t-test was used to compare the average number of contacts between the pre-UAT and UAT periods; P < 0.05 was considered significant.
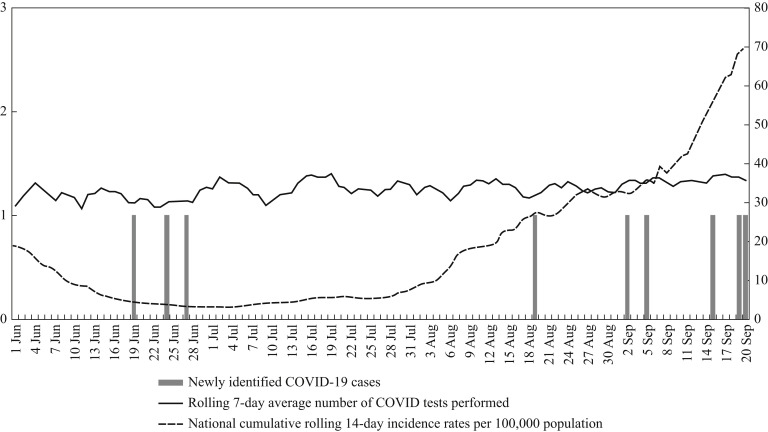
From June 1st to September 20th, 3393 PCR tests for SARS-CoV-2 were performed on non-COVID-19 pathway emergency admissions, with a stable testing rate throughout (Figure 1 ). Results were returned same day for 1945 (57%), next day for 1416 (42%), and ≥2 days later for 32 (1%) patients.
Figure 1.
National cumulative rolling 14-day incidence of COVID-19 expressed as a rate per 100,000 population (scale 0–80) (source: HPSC). Local rolling seven-day average number of COVID-19 tests performed in non-COVID pathway emergency department admissions (scale 0–80), along with the number of newly identified COVID-19 cases (scale 0–3) (June 1st to September 20th, 2020) in Beaumont Hospital, Dublin.
SARS-CoV-2 RNA was newly detected from nine (0.26%) patients (June (N = 3), July (N = 0), August (N = 1) and to September 20th (N = 5)) as described in Figure 1. Five were female and the mean age was 49.6 years. None became symptomatic. The most common presentation was an abdominal complaint (N = 5). Four (44%) were admitted under surgical specialties. The median length of stay (LOS) was five days (range: 1–28). There were 23 patient and 21 staff close contacts. Before June 1st, the mean number of contacts per case was 4.5 patients (range: 0–17) and 4.9 staff (range: 1–37), falling to 2.5 patients (range: 0–5; P = 0.061) and 2.3 staff (range: 0–6; P < 0.05), respectively, during the study period. All close contacts remained asymptomatic, with none having SARS-CoV-2 detected on follow-up testing.
Timely COVID-19 diagnosis protects patients and staff, especially where asymptomatic or pre-symptomatic admissions present with another complaint. While UAT on a non-COVID-19 pathway yielded a few detections, the value lies in preventing transmission, early implementation of IPC measures, identification and minimization of close contacts in a hospital with high occupancy and limited isolation facilities. After UAT implementation, a significant reduction in the mean number of staff contacts was observed, with a reduction in the mean number of patient contacts. Increased detection of COVID-19 cases from late August to September 20th was contemporaneous with an increased national incidence.
SARS-CoV-2 testing strategies include: testing those with symptoms, those who are contacts of a COVID-19 case, and UAT. Some centres adopted UAT during the first wave [3]. UAT is costly and consumes laboratory resources. In one centre, along with universal masking, UAT decreased high-risk exposures to SARS-CoV-2 among healthcare staff by 77% [4].
As 44% of the asymptomatic COVID-19 patients were surgical admissions, UAT may have prevented cross-transmission to other perioperative patients, where severe outcomes have been reported [5]. Universal surgical face mask use in clinical areas also protected staff, provided that standard precautions were also meticulously applied.
Limitations include a single-centre setting and timing of the study during a period of low incidence of SARS-CoV-2. Staff compliance with universal mask-wearing and other IPC measures were not systematically evaluated.
However, this study was undertaken where occupancy frequently exceeds capacity and the majority of inpatient accommodation is multi-occupancy, with limited isolation rooms. SARS-CoV-2 resurgence mandates rapid identification of cases and close contacts and we believe that a UAT strategy can prevent transmission of this potentially fatal virus.
Acknowledgements
With thanks to COVID-19 Epidemiology Team, Health Protection Surveillance Centre (HPSC), Dublin, Ireland, for 14-day national incidence data.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Rickman H.M., Rampling T., Shaw K., Martinez-Garcia G., Hail L., Coen P. Nosocomial transmission of coronavirus disease 2019: a retrospective study of 66 hospital-acquired cases in a London teaching hospital. Clin Infect Dis. 2020 Jun 20 doi: 10.1093/cid/ciaa816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health Protection Surveillance Centre . 2020. COVID-19: guidance for healthcare settings.https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/guidanceforhealthcareworkers/ Available from: [last accessed October 2020] [Google Scholar]
- 3.Sutton D., Fuchs K., D’Alton M., Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163–2164. doi: 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker J., Fleece M.E., Griffin R.L., Leal S.M., Alsip J.A., Stigler W.S. Decreasing high risk exposures for healthcare-workers through universal masking and universal SARS-CoV-2 testing upon entry to a tertiary care facility. Clin Infect Dis. 2020 Sep 8 doi: 10.1093/cid/ciaa1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [Erratum in: Lancet 2020;396(10246):238.] [DOI] [PMC free article] [PubMed] [Google Scholar]