Abstract
Background
Coronavirus disease 2019 (COVID-19) has changed the way we practice medicine. Standards of care are evolving in an effort to diagnose, manage, and treat the cause of this global pandemic, as well as to protect the health care workforce. These practices can have unexpected and potentially dangerous consequences, particularly for patient populations with confounding factors that put them at increased risk for complications and poor outcomes.
Case Report
A 52-year-old previously healthy woman presented with 4 days of nasal pain and discharge after using a home collection kit in an attempt to obtain a nasopharyngeal viral sample for COVID-19 testing.
Why Should an Emergency Physician Be Aware of This?
With treatments, policies, and procedures that are rapidly evolving and often deviating from established, evidence-based, usual care in response to the COVID-19 pandemic, emergency physicians must be cognizant of and monitor for poor outcomes and potential downstream complications, especially in underserved patient populations.
Keywords: COVID-19, unexpected complication, rhinoscopy, nasal foreign body
Introduction
The novel coronavirus 2019 (COVID-19) was first identified as the cause of a pneumonia outbreak in Wuhan, China, in December 2019 (1). The responsible pathogen, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was isolated on January 7, 2020, and the outbreak was declared a pandemic by the World Health Organization on March 11, 2020 (2,3). In the course of treating this pandemic, new methods of testing, treatment, and care have been implemented to protect the frontline health care workforce, with occasional negative consequences for patients. Taking stroke as one example, several authors have reported poorer outcomes. Naccarato et al. described a decrease in effectiveness of stroke workup during the early phases of the pandemic (4). Patient behavior has also changed in response to fears of COVID-19, also contributing to worse outcomes. Again looking at stroke, Teo et al. described a delay in hospital arrival after a stroke (5).
This case report describes an unintended adverse outcome of COVID-19 related to diagnostic testing. Nasopharyngeal swab sampling, using a nasal viral swab, remains the go-to method for widespread testing for COVID-19. As health care facilities have moved to protect employees, responsibility for obtaining viral swabs has been, in some cases, transferred to patients themselves. This case report describes an unexpected negative consequence of patient-performed testing with a self-swab kit. Similar complications have also been reported with professionally obtained viral samples, but we fear that such complications will become more and more common with increased reliance on patient self-swabbing to obtain viral samples (6).
Case Report
History and Physical Examination
A 52-year-old woman who denied significant medical history presented to the emergency department (ED) of a large, academic, level I trauma center with concerns that there was a retained foreign body in her left nostril. She had a positive COVID-19 test approximately 1 month prior to presentation and, therefore, was prohibited from working her retail job. Her employer's return-to-work policy required a negative COVID test after resolution of symptoms. Four days prior to presentation to our facility, she obtained a nasopharyngeal self-swab testing kit from a national pharmacy chain. She was personally responsible for the cost of testing, and this was the cheapest option she could find. She successfully obtained a sample from the right nare but after attempting to obtain a sample from her left nare, she withdrew the nasopharyngeal swab applicator and retrieved only part of the applicator. She presented with concern that the tip of the applicator remained in her nose, as she felt considerable discomfort in the upper region of the left nostril and excessive secretions on that side.
The patient had been evaluated twice previously for the same concerns, first at an urgent care center and next in the ED at a large, local outside community hospital. In spite of extensive efforts, as described by the patient, outside hospital providers were unable to find or remove any retained foreign body. She was therefore discharged on a 7-day course of amoxicillin and instructed to follow-up with otolaryngology (ear, nose, and throat [ENT]) as an outpatient should symptoms persist. Symptoms did not resolve, however she could not afford the fees associated with an outpatient specialty office visit and therefore presented to our ED for further evaluation. She denied any other symptoms. She specifically denied difficulty swallowing or tolerating oral intake, cough, difficulty breathing, shortness of breath or respiratory symptoms at this time. Her discomfort was localized to the left nostril, from which she also described copious white and yellow secretions.
Intake vital signs were within normal limits. External physical examination revealed no evidence of foreign body, trauma, epistaxis or other significant findings.
Diagnostic Focus and Assessment
The patient brought with her both plastic applicators that she used for self-swabbing, allowing us to clearly visualize the shape and form of the swab fragment we were searching for within her left nare (Figure 1 ). After anesthetizing the left nare with three sprays of oxymetazoline hydrochloride 0.05%, followed by 3 mL of vaporized 2% lidocaine, we used a nasal speculum but were unable to visualize any foreign object. The left internal nare appeared more erythematous than the right, but was otherwise indistinguishable distal to the turbinates. Next, we used a video rhinolaryngoscope (Figure 2 ; Karl Storz CMOS Video Rhino-Laryngoscope with 2.9 mm diameter, model 11102) attached to a CMAC monitor to attempt to better visualize the foreign body. After achieving local anesthesia with combined lidocaine, epinephrine, and tetracaine gel we were able to successfully manuever the fiber optic device past the turbinates and visualize the epiglottis and vocal chords. While retracting the scope, we could appreciate what appeared to be a foreign body approximately 3.5 cm proximal to the opening of the left nare, in the middle meatus (Figure 3 ). We were, however, unable to retrieve the suspected foreign body. We therefore consulted our ENT colleagues who agreed to come to the bedside to evaluate the patient in the ED.
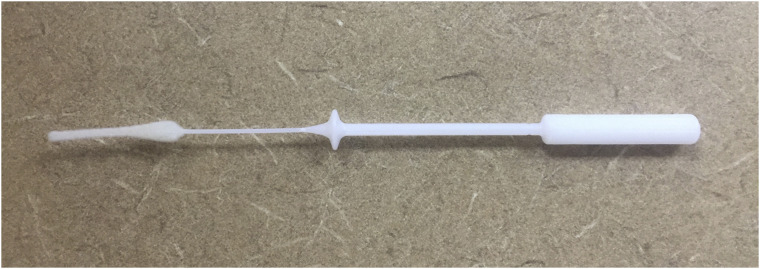
Figure 1.
The type of nasopharyngeal swab applicator used by the patient for self-swabbing.
Figure 2.

Karl Storz CMOS video Rhino-Laryngoscope with diameter 2.9 mm (model 11102).
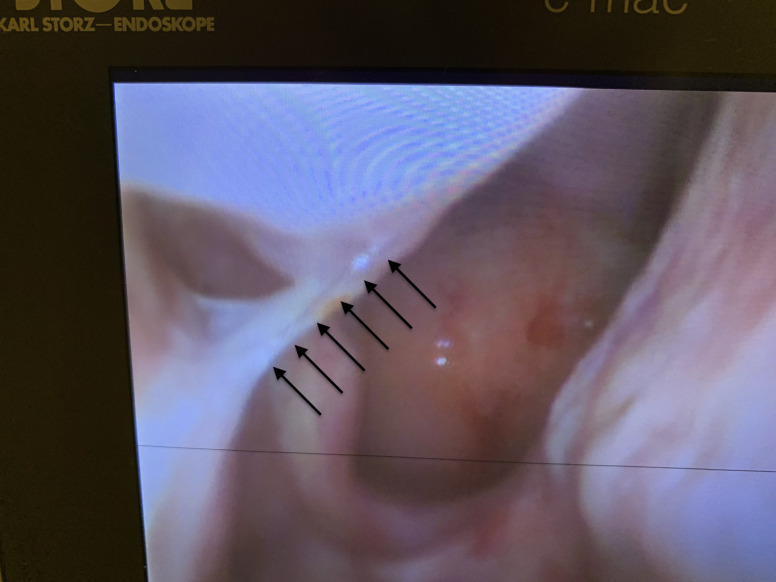
Figure 3.
Rhino-laryngoscope image showing what appears to be the nasal foreign body, indicated by the black arrows, in the upper left corner of the CMAC screen.
Therapeutic Focus and Assessment
Bedside nasal endoscopy was performed using a 30-degree rigid nasal endoscope (Figure 4 , Karl Storz 2.7-mm, 0-degree Hopkins rod scope, model 1230BA). Attempts were made at retrieving the presumed foreign body in the middle meatus using an "alligator" forceps (Figure 5 , Karl Storz Hartmann ear forceps, model 161000); however, palpation of this object revealed it to be a strand of mucus. After clarification of patient history and symptomatology, and further nasal endoscopy, the retained swab tip was ultimately found in the left olfactory fossa, a narrow space bounded medially by the nasal septum and laterally by the middle turbinate. Figure 6 shows a coronal section of noncontrast CT sinus with bony windows. This generic cross-sectional image indicates the olfactory fossa, a very narrow space between the middle turbinate and the nasal septum, where the retained swab tip was ultimately identified in our patient via repeat nasal endoscopy. The retained foreign body (Figure 7 ) was then retrieved easily from this location using the “alligator” forceps.
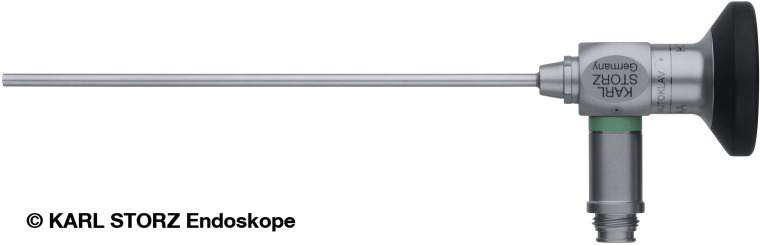
Figure 4.
Karl Storz 2.7-mm, 0-degree Hopkins rod scope (model 1230BA).
Figure 5.
“Alligator” forceps; Karl Storz Hartmann ear forceps (model 161000).
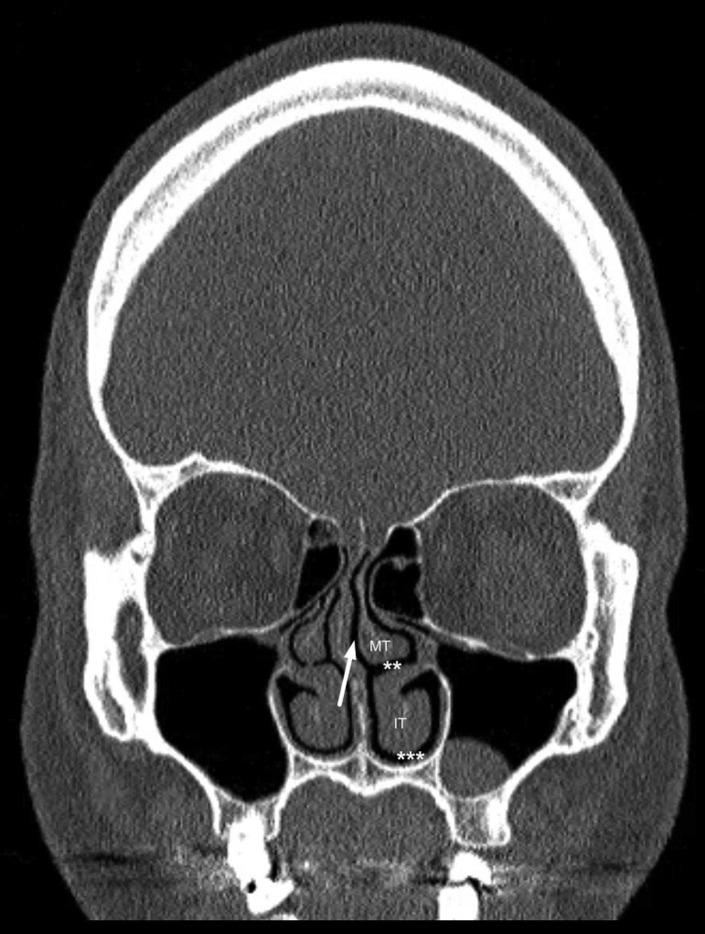
Figure 6.
Generic coronal section of noncontrast computed tomography sinus with bony windows. This slice depicts the olfactory fossa, indicated by the white arrow, where the swab tip was ultimately identified and retrieved. Home test swabs are intended to be applied through the middle meatus (∗∗) or inferior meatus (∗∗∗), which provide unobstructed paths to the nasopharynx. IT = inferior turbinate; MT = middle turbinate.
Figure 7.
The swab applicator tip that was retrieved from the patient's left nare.
After the procedure, the patient described immediate resolution of all symptoms. The patient reported 3 days remaining on her amoxicillin prescription and we recommended completing this antibiotic course. She was discharged home in stable condition with appropriate return precautions and instructions to follow-up with her primary care physician on an outpatient basis.
Follow-Up and Outcome
Ten days after our intervention, the patient reported no lingering symptoms or delayed complications. We had obtained a preprocedure COVID-19 swab on the day of presentation, following ENT's protocol for a potentially aerosolizing procedure, which was negative. An unintended benefit was that this result allowed the patient to finally return to work.
Discussion
This case highlights an unintended consequence of our current state of practice surrounding COVID-19. Persistent uncertainty and lack of clear, unifying public health policy means that employers, including hospitals and health care facilities, government agencies, schools, and all manner of institutions have developed their own return-to-work protocols. In the case of our patient, her employer had directed that she was personally responsible, at her own expense, for providing proof that she had recovered from COVID-19 and was safe to return to work. This led to an economically motivated decision to self-swab, with an unanticipated complication leading to three trips to health care facilities and three expensive bills. Exact charges are unknown, as our patient was seen at two outside hospitals prior to her visit at our facility, but a conservative estimate of total costs of treatment is somewhere in the range of $25,000.
Fortunately, the Emergency Medical Treatment and Active Labor Act assured that she could be seen and evaluated. During her ED visit, the foreign body was removed and therefore did not become a nidus for sinus infection in her inner sinuses, a potentially life-threatening complication due to proximity to her brain and subarachnoid space. Our patient's persistence ultimately led to a favorable outcome, but only after three visits to three separate health care facilities.
In terms of our intervention, the use of otologic instrumentation, such as the "alligator" forceps, in a case like this one was favorable from both patient comfort and operator ease standpoints. Situated adjacent to the nasal septum, the olfactory fossa is a highly sensitive area in most patients. It is also narrow, averaging 2–3 mm in transverse width in anatomic studies (7). Compact instrumentation is necessary to access such a small space and allows the operator to reach the foreign body and avoid collateral instrumentation, and irritation, to the adjacent nasal mucosa.
Apart from the case reported, which describes retention of a broken segment of a professionally administered nasopharyngeal swab applicator, as of October 2020, we found only one other published case report describing potential hazards of a swab test gone awry. In that instance, which did not involve self-swabbing, a patient accidentally ingested a broken-off swab applicator tip (8).
In terms of general effectiveness of self-swabbing, the location of the retained foreign body also brings to light some interesting points of concern. Nasopharyngeal samples are intended to be retrieved from the actual nasopharynx. Home test swabs are designed to be applied through the middle meatus or inferior meatus, which provide unobstructed paths to this anatomic location. In contrast, the olfactory fossa is a narrow space with a blind ending at the anterior skull base. To reach the actual nasopharynx, a patient should push the swab applicator straight back. But, the layperson's conception of where the nose "goes" is in an upward direction toward the forehead. Inserting the swab up along this trajectory will not reach the nasopharynx, but we fear this is likely the technique many at-home testers are using. In our own casual observations, we have also noted multiple instances in which health care professionals have inserted swabs in an upward, rather than backward, direction.
Inserting the swab in an upward direction also causes more pain to the patient. In addition, this technique produces more potential complications than pointing it correctly posteriorly toward the nasopharynx. Piras et al. posit that improper nasopharyngeal sampling performed by untrained operators can increase false-negative results and have a negative overall impact on attempts to monitor and control the outbreak (9). This group also reports concern that improper collection may put health care workers at risk (10).
This case highlights one specific, unnecessary risk and downstream complication that occurred as a result of evolving standards of care in the testing and treatment of COVID-19. This case suggests that efforts to protect the health care workforce can lead to increased poor outcomes in underserved populations.
Why Should an Emergency Physician Be Aware of This?
COVID-19 has resulted in policies and procedures that deviate from established, evidence-based, usual practice, with potential negative consequences for patients. Emergency physicians must be mindful of and monitor for poor outcomes and potential downstream complications that result from evolving testing and treatment in response to COVID-19, especially in underserved patient populations. Better understanding and education surrounding proper nasopharyngeal swab sampling are needed to help reduce complications and improve outcomes.
Footnotes
The patient provided verbal and written informed consent.
References
- 1.Kim J.Y., Ko J.H., Kim Y., et al. Viral load kinetics of SARS-CoV-2 infection in first two patients in Korea. J Korean Med Sci. 2020;35(7):e86. doi: 10.3346/jkms.2020.35.e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Virtual press conference on COVID-19. 11 March 2020. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2 Available at:
- 4.Naccarato M., Scali I., Olivo S., et al. Has COVID-19 played an unexpected "stroke" on the chain of survival? J Neurol Sci. 2020;414:116889. doi: 10.1016/j.jns.2020.116889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teo K.-C., Leung W.C.Y., Wong Y.-K., et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mughal Z., Luff E., Okonkwo O., Hall C.E.J. Test, test, test—a complication of testing for coronavirus disease 2019 with nasal swabs. J Laryngol Otol. 2020;134:646–649. doi: 10.1017/S0022215120001425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Savvateeva D.M., Güldner C., Murthum T., et al. Digital volume tomography (DVT) measurements of the olfactory cleft and olfactory fossa. Acta Otolaryngol. 2010;130:398–404. doi: 10.3109/00016480903283741. [DOI] [PubMed] [Google Scholar]
- 8.De Luca L., Maltoni S. Is naso-pharyngeal swab always safe for SARS-CoV-2 testing? An unusual, accidental foreign body swallowing. Clin J Gastroenterol. 2020 doi: 10.1007/s12328-020-01236-y. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piras A., Rizzo D., Uzzau S., De Riu G., Rubino S., Busso F. Inappropriate nasopharyngeal sampling for sars-cov-2 detection is a relevant cause of false-negative reports. Otolaryngol Head Neck Surg. 2020;163:459–461. doi: 10.1177/0194599820931793. [DOI] [PubMed] [Google Scholar]
- 10.Piras A., Rizzo D., Longoni E., et al. Nasopharyngeal swab collection in the suspicion of Covid-19. Am J Otolaryngol. 2020;41:102551. doi: 10.1016/j.amjoto.2020.102551. [DOI] [PMC free article] [PubMed] [Google Scholar]