Abstract
Purpose
To examine the impact of the COVID-19 pandemic on the presentation and care provided to patients with acute ischemic stroke (AIS) at the emergency department (ED).
Method
A retrospective-archive study was conducted between January-April 2020, compared with the parallel months in 2017–2019, in a comprehensive stroke center. We compared the time from symptoms onset to ED arrival, the number of neurologic consultations completed in the ED, patients diagnosed with AIS, patients receiving acute treatment and hospital mortality.
Results
During January-April 2020, we found an increase in the proportion of stroke patients arriving at the ED within 6 h of symptom onset: 68–100% per month during the study period, compared with 28–42% per month in the previous years. The number of patients admitted to the ED with suspected AIS declined by 41%, compared to the parallel period in 2019. An increase was noted in the number of patients diagnosed with AIS who underwent treatment, with the number of s endovascular thrombectomy increasing throughout the examined year.
Conclusion
During the COVID-19 pandemic, we observed a significant decline in the number of AIS patients admitted to the ED. Paradoxically, we have seen an increase in the proportion of patients who arrived shortly after the onset of symptoms and received timely treatment. Future studies might investigate the medical mechanism and ramifications of this phenomenon.
Keywords: Acute ischemic stroke, COVID-19, Critical care, Emergency department, In-hospital mortality
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has resulted in public health measures, aimed at reducing viral spread. Those measures ranged from complete lockdown in Italy during March and April 2020 to stay-at-home orders and social distancing measures [[1], [2], [3]]. Soon after those measures were implemented, the toll of avoiding timely care for urgent medical conditions has become evident, for example the sharp decline (20–43% relative change) in emergency department (ED) visits [4]. The case of timely treatment is of special interest in the case of stroke, since it may decrease the incidence of poor outcomes, including disability and death [5,6].
Optimizing outcomes matters even more during the pandemic since affected patients may be at greater risk of in-patient morbidity and mortality [7], and the hospital system needs to allocate a designated pathway for patients with large vessel occlusion [8,9]. In the US, the Northern Ohio region demonstrated a ≈30% decline in stroke presentation across all EDs in the region [10]. Kansagra and his colleagues reported a 39% decrease in the number of patient who received imaging for the evaluation of stroke, across 856 US hospitals, from the pre-pandemic to the early-pandemic period. The authors referred to this decrease as a collateral effect of the pandemic [11].
In Israel, public health interventions included a national lockdown imposed on the entire population during two weeks in April, and social distancing measures, including the wearing of face masks and keeping a 2-m-distance from each other. Policy makers urged the elderly (65+) and people with medical risk factors to stay at home even when the lockdown was removed. Healthcare providers asked the public to avoid physical encounters with the healthcare system and use telemedicine, whenever possible, instead. The latter measures were explained by the overload on the medical teams as well as fear of being infected due to close contact with the healthcare teams or with other patients. This atmosphere resulted in a sharp decline in referrals to the ED with acute life-threatening medical conditions, including stroke [13].
The aim of the current study is to examine the impact of the COVID-19 pandemic on the number of acute ischemic stroke (AIS) patients admitted and treated in the emergency department of a large tertiary medical center.
2. Research hypotheses
-
1.
The number of patients arrived to the ED with symptoms suggestive of AIS declined during the COVID-19 pandemic, compared with previous years.
-
2.
The number of patients diagnosed and treated for AIS declined during the COVID-19 pandemic, compared with previous years.
3. Method
3.1. Study design and setting
A retrospective archive study was conducted in May 2020 in a comprehensive stroke center serving the northern parts of Israel. This medical center serves as a referral center for 12 district hospitals, the Northern Command of the Israel Defense Forces, the US’ Sixth Fleet and the United Nations peacekeeping forces. Its ED, with 105 beds, serves a yearly average of 136,819 adult (18+) patients. Of these, approximately 5000 patients with symptoms suggestive of AIS are assessed by neurologists each year.
The study was approved by the institutional review boards of the hospital (#3023-18-RMB).
3.2. Data collection
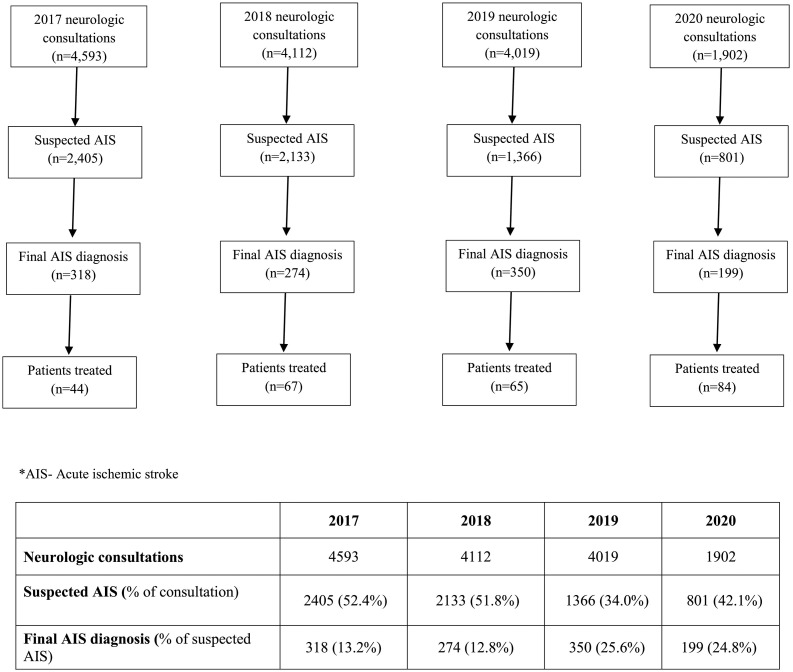
Data was collected for the months January-April in 4 consecutive years: 2017–2020. Data collection was conducted in the four following steps (Fig. 1 ): (1) Extraction of all neurological consultations which took place in the ED and were documented in the electronic medical records (EMR), in order to evaluate the number of patients admitted with symptoms suggestive of AIS. Neurologic consultation could be requested either by the triage nurse or by an ED physician. (2) Suspected AIS was defined by the following key-words: confusion, loss of consciousness, vision abnormalities, dysarthria, facial paralysis, loss of balance, lack of coordination, numbness, weakness, hemiparesis, sensory abnormalities, headaches with abnormalities of gait and diplopia. Neurological consultations of Traumatic head injury, Drug use, Alcohol intoxication, Epileptic seizures, Meningitis, Post herpetic neuralgia, Trigeminal neuralgia, Multiple sclerosis, Parkinson's disease, Psychosis, Malignancy and Migraine as initial diagnosis were all excluded. (3) In order to identify those patients with a final AIS diagnosis, all reports of CT examination performed during the study period to patients referred from the ED, whether admitted later to the hospital or discharged from the ED to their homes, were reviewed. Cases of in-hospital stroke were excluded. Inclusion criteria – the following International Classification of Diseases (ICD) 9 codes for AIS: 433.01, 433.10, 433.11, 433.21, 433.31, 433.81, and 433.91 (occlusion and stenosis of pre-cerebral arteries), 434.00, 434.01, 434.11, and 434.91 (occlusion of cerebral arteries), 436 (acute but ill-defined cerebrovascular disease). Hemorrhagic stroke codes - 430,431,432 - were not included in the analysis. (4) Two experts - the first and third authors - composed a final patient list by cross-linking the records, matching patient's identification numbers with case number and excluding duplicate records.
Fig. 1.
The flow chart of the process of care for AIS patients, by year: January-April 2017–2020.
3.3. Statistical analysis
Continuous variables were reported as means and standard deviations (SD) or medians and interquartile ranges (IQR), as appropriate. Dichotomous variables were reported as proportions. The data analysis was performed using SAS® software (SAS Enterprise Guide 7.1) and Python 3.6.5 software version 2019a.
4. Results
The analysis included a total of 14,626 neurological consultations during the months January through April, in the years 2017, 2018, 2019 and 2020, representing 31.4%, 28.1%, 27.5% and 13.0% of the overall number of neurologic consultations in the study period, respectively. A relative decrease of 67% of suspected AIS patients admitted to the ED was noted during the months of January-April of the year 2020 compared to the parallel period of 2017, supporting hypothesis one. Final AIS diagnosis was given to 24.8% of all suspected AIS patients in 2020, a rate similar to 2019 (25.6%) and twice higher compared with the rate in 2017 and 2018 (13.2% and 12.8%, respectively) (Table 1 ).
Table 1.
Presentation and care processes of stroke patients at the ED: January-April 2017–2020.a
| 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| Neurologic consultations | 4593 | 4112 | 4019 | 1902 |
| Suspected AIS | 2405 | 2133 | 1366 | 801 |
| % of consultation | 52.4% | 51.8% | 34.0% | 42.1% |
| Final AIS diagnosis | 318 | 274 | 350 | 199 |
| % of suspected | 13.2% | 12.8% | 25.6% | 24.8% |
| Treatment | ||||
| tPA | 19 | 26 | 20 | 28 |
| EVTc | 21 | 32 | 42 | 47 |
| Combined | 4 | 9 | 3 | 9 |
| Total | 44 | 67 | 65 | 84 |
| No treatment | 274 | 207 | 285 | 115 |
| In-hospital death (all-cause mortality) | 15 | 32 | 26 | 17 |
| In-hospital death (ICHb) | 10 | 8 | 8 | 11 |
| % of death | (66.7%) | (25%) | (30.7%) | (64.7%) |
AIS – acute ischemic stroke; tPA- tissue plasminogen activator.
ICH-intra-cranial hemorrhage.
EVT- endovascular thrombectomy.
The number of patients receiving treatment, either administration tPA or EVT, increased during the year of 2020 (n = 84), compared with 44–67 in previous years. Based on these findings, hypothesis 2 is rejected.
Most of the increase in the number of patients receiving treatment, resulted from increase in the number of patients who underwent EVT. While EVT performance gradually increased during the course of the examined years (2017, n = 21; 2018, n = 32; 2019, n = 42; 2020, n = 47), tPA exhibited milder, less consistent, increase (2017, n = 19; 2018, n = 26; 2019, n = 20; 2020, n = 28).
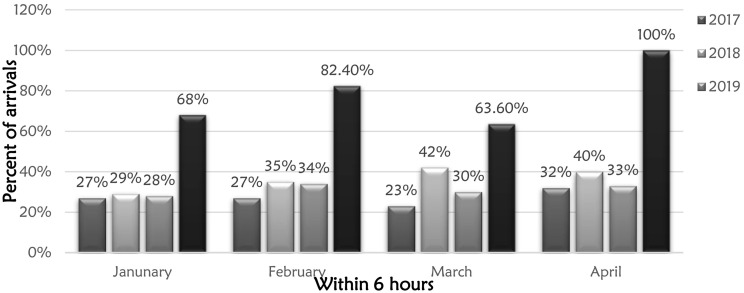
Analysis of the proportion of patient arriving at the ED within six hours from symptom onset (Fig. 2 ), demonstrated similar trends with mild fluctuations for the examined months during the 3 years prior to the pandemic: 2017 (January-27%; February-27%; March-23% and April-32%), 2018 (January-29%; February-35%; March-42% and April-40%) and 2019 (January-28%; February-34%; March-30% and April-33%). The arrival rate within 6 h in 2020 was higher during all the months examined (Januray-68%, February-82.4%, March-63.6% and April-100%), compared with the parallel months in the previous years.
Fig. 2.
Proportion of patients diagnosed with AIS arriving at the ED within six hours of symptom onset, by month and year.
In-hospital mortality from all causes demonstrated an increase from 2017 to 2018–2019, followed by decrease in 2020. Intracranial hemorrhage (ICH) was responsible for two thirds of all deaths in 2017 and in 2020, with lower proportions noted in 2018 and 2019 (Table 1).
5. Discussion
The current study examined the presentation, management and mortality of AIS patients arriving at the ED during the first four months of the COVID-19 pandemic, compared with the same months in 3 years preceding that period. A considerable decrease was observed during the pandemic in the number of neurologic consultations, suspected and approved AIS diagnoses, compared with previous years.
However, a moderately decreasing trend has already started back in 2017, with each consecutive year seeing less consultations and suspected cases, compared with the year before. In final AIS diagnosis, the trend was fluctuating. The first 4 months of 2020 demonstrated a steep decrease from 2019 to 2020, in all three variables (consultations, suspected AIS and confirmed AIS) which was different from the moderate change between 2017 and 2018 or 2018–2019. The moderate trend of decreased numbers of consulations or decreased proportion of consultations ending in “suspected AIS” could be explained by improved triage process that allows for better identification of true stroke.
The current study suggests that patients avoided seeking medical care at the ED with diverse neurologic symptoms, including those indicative of stroke. In the first months of the COVID-19 pandemic, public health policies, aimed at reducing viral spread in the population, were the leading strategy adopted globally. Special emphasis was dedicated to populations at risk, such as the elderly and patients with known morbidities [14]. Risk of severe infection and mortality was demonstrated to increase with advancing age and some co-morbidities like hypertension and diabetes – both know to be also risk factors for stroke [15]. Simultaneously, the medical staff and health services campaigns urged people to stay at home, encouraging the use of telemedicine, to reduce the infectious risk for patients and to alleviate the pressure on the healthcare system, being forced to channel huge resources into COVID-19 patient care [16]. Avoiding ED referrals could result from patients fear of being infected at the hospital, particularly after the media reports about infection spread across hospitalized patients and healthcare personnel. The above-mentioned measures resulted in a significant reduction in the number of urgent referrals to the ED, one of which is AIS. Indeed, analysis of data from 227 Chinese hospitals demonstrated a 40% in stroke admissions in February 2020 compared with February 2019. The authors suggested that patients not coming to the hospital constituted the main contributing factor to that decrease [17].
The study demonstrated that the absolute number of patients undergoing treatment increased from 2017 to 2020. The increase from 2018 and on could be explained by change of clinical guidelines concerning the criteria for treatment: In January 2018, the window for endovascular therapy (ET) for patients with AIS was extended from 6 to 24 h from symptom onset [18]. However, since in 2020 most patients arrived within the first 6 h, this explanation is less relevant to the study findings. One might suggest that patients arriving at the ED experienced more severe stroke symptoms, that they could no longer ignore, despite the warnings and fears related to arriving at the ED. Those patients naturally would be sicker, with higher chance of the clinical presentation suggestive of AIS, and with a higher proportion requiring interventional treatment, especially since they arrived on time. As reported by Diegoli et al., admissions to the ED were noted to decrease for mild and moderate, but not for severe stroke, creating a relatively higher proportion with more severe presentation, compared to the pre-pandemic period [12].
Higher treatment rates are not in accordance with the Chinese study that demonstrated a 25% decrease in thrombolysis and thrombectomy during February 2020, compared with February 2019 [19]. In Northern Ohio, rate of thrombolysis decreased but the rate of thrombectomy remained unchanged [10].
During the peak of the pandemic, in April 2020, a remarkably increased proportion (up to 100%) of stroke patients arrived at the ED within 6 h of symptom onset, 2.5–3.0 more than in the prior years. It is possible ate that more severe symptoms of patients arriving during the COVID-19 could serve as an explanation for early presentation. However, due to the unavailability of data on the severity of the disease (e.g. National Institute Health Stroke Scale-NIHSS) we were unable to examine this assumption.
Although no significant increase in the in-hospital mortality rate was noted, the proportion of in-hospital mortality due to ICH was higher than parallel periods in the years 2018 and 2019. Perhaps the increased in-hospital mortality from ICH reflects the increased treatment measures (both tPA and EVT), taken in this time period. Also, the surgical management of patients presenting with a ICH or developing this complication during hospitalization, may be different during the pandemic.
5.1. Limitations
This study has several limitations. First, retrospective analysis of medical records depends on full and accurate record keeping of many health professionals involved. Second, data availability allows to analyze only records of patients arriving to the ED, while we were not able to reach data on patients who were not referred to the ED, nor were we able to analyze the clinical outcomes of those patients. Also, NIHSS data for patients presenting during the pandemic was not available, precluding the analysis and comparison of symptom severity. Third, long-term mortality (30 days, 90 days, and one year following the discharge) beyond the hospitalization period was lacking. Fourth, we cannot rule out the effect of unexamined variables, like more time out of work, due to the lockdown or unpaid leave, on the incidence of acute cardiovascular events. Those variables could have contributed lower incidence and decreased ED admissions due to stroke. Finally, outcome data on stroke among patients who stayed away or were discharged from the ED is not available for analysis. This could have an impact on both the number of stroke cases and on its outcomes.
6. Conclusion
Despite decreased volume of patients arriving at the ED with neurologic symptoms and receiving the relevant evaluation, the number of patients being treated did not decrease and even increased during the first 4 months of the COVID-19 pandemic, compared with previous years. Additional findings, such as the decreased numbers and rates of confirmed AIS diagnoses or in-hospital mortality, require future research in order to investigate the precise reasons as well as the medical ramifications of those phenomena.
Author contributions
All authors interpreted the data and edited and approved the final article. MS, RWM, RSH and TS drafted and conceived the study. AR performed data collection, MS and TS analyzed the data and designed the study. MS and RWM take responsibility for the paper as a whole.
The research has not been presented.
No financial support was received for this research.
None of the authors have any conflicts of interest.
References
- 1.Niedzwiedz C.L., O’Donnell C.A., Jani B.D., Demou E., Ho F.K., Celis-Morales C., et al. Ethnic and socioeconomic differences in SARS-CoV2 infection in the UK Biobank cohort study. MedRxiv. 2020 doi: 10.1101/2020.04.22.20075663. 2020.04.22.20075663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. Coronavirus Disease (COVID-19) Weekly Epidemiological Update 1 Global Epidemiological Situation. [Google Scholar]
- 3.Gt Walker P., Whittaker C., Watson O., Baguelin M., Ainslie K.E.C., Bhatia S., et al. 2020. The Global Impact of COVID-19 and Strategies for Mitigation and Suppression. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butt A.A., Azad A., Kartha A., Masoodi N., Bertollini R., Abou-Samra A.-B. Volume and acuity of emergency department visits before and after COVID-19. J Emerg Med. 2020 doi: 10.1016/j.jemermed.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albers G.W., Marks M.P., Kemp S., Christensen S., Tsai J.P., Ortega-Gutierrez S., et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718. doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khosravani H., Rajendram P., Notario L., Stroke M.C. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Am Hear Assoc. 2020 doi: 10.1161/STROKEAHA.120.029838. (2020 undefined) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baracchini C, Pieroni A, Viaro F.… . Springer; 2020. Acute Stroke Management Pathway During Coronavirus-19 Pandemic. (n.d, VC-N, 2020 undefined) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegler J, Heslin M, Thau L.… . Elsevier; 2020. Falling Stroke Rates During COVID-19 Pandemic at a Comprehensive Stroke Center: Cover Title: Falling Stroke Rates During COVID-19. (n.d, AS-J of S and, 2020 undefined) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uchino K., Kolikonda M.K., Brown D., Kovi S., Collins D., Khawaja Z., et al. Decline in Stroke presentations during COVID-19 surge. Stroke. 2020:2544–2547. doi: 10.1161/STROKEAHA.120.030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diegoli H., Magalhães P.S.C., Martins S.C.O., Moro C.H.C., França P.H.C., Safanelli J., et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Am Hear Assoc. 2020;51:2315–2321. doi: 10.1161/STROKEAHA.120.030481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bullrich M.B., Fridman S., Mandzia J.L., Mai L.M., Khaw A., Gonzalez J.C.V.…Sposato L.A. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montero-Odasso M, Goens S.… Canadian Geriatrics Society COVID-19 Recommendations for older adults—What do older adults need to know? CgjonlineCa. 2020 doi: 10.5770/cgj.23.443. (NK-CG, 2020 undefined) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guzik T, Mohiddin S, Dimarco A.… COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. NcbiNlmNihGov. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. (n.d, VP-C, 2020 undefined) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020:1–6. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu R., Shen Y., Zhao J., Li H., Kung D., Fisher M. Impact of the COVID-19 epidemic on Stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powers W.J., Rabinstein A.A., Ackerson T., Adeoye O.M., Bambakidis N.C., Becker K., et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e99. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 19.Zhao J., Rudd A., Liu R. Challenges and potential solutions of Stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke. 2020 doi: 10.1161/STROKEAHA.120.029701. [DOI] [PMC free article] [PubMed] [Google Scholar]