Abstract
Background
The uptake of point-of-care testing (POCT) within community pharmacies at state and national levels is largely unknown despite the endorsement and advocacy efforts of pharmacy organizations, recent legislative advances, and numerous models for successful POCT implementation within individual pharmacy sites.
Objectives
The study aimed to describe the current landscape of POCT in Wisconsin community pharmacies and identify opportunities for the advancement of testing and the key factors influencing the realization of these opportunities.
Methods
A survey was administered over the telephone to pharmacy managers of community pharmacies in Wisconsin. The sites were randomly selected from predefined geographic regions to mirror pharmacy distribution across Wisconsin. The survey items evaluated provision of POCT, future direction of POCT, barriers and motivators to offering POCT, and pharmacy demographics. Descriptive statistics and thematic analysis were used to analyze data.
Results
Pharmacy managers from 147 of the 938 registered community pharmacies (15.7%) participated in the survey. Only 17.1% of the pharmacies were offering POCT; however, 48.3% of managers reported that their pharmacy would likely implement or expand POCT within the next 5 years. The most commonly reported barriers to initiating or expanding POCT were the limitations on pharmacist availability to oversee testing and workflow restrictions. Continuing to advance the pharmacy profession was a top reason for offering or expanding testing services.
Discussion
While few pharmacies are offering POCT in Wisconsin, there is motivation for expansion in coming years. Understanding, anticipating and addressing common barriers can faciliate this process.
Conclusion
This needs analysis offers a blueprint for researchers, educators, and clinicians to shape POCT efforts by examining the landscape of pharmacy-based testing in their own states and communities.
Background
Point-of-care testing (POCT) within community pharmacies is endorsed by organizations at the national level and, more recently, was included as part of the federal response to the coronavirus disease (COVID-19) pandemic. The American Pharmacists Association has had policy recognizing the value of pharmacist-provided POCT since 2003. It advocates for laws, regulations, and policies enabling testing services and facilitates implementation through education and resources.1 The National Community Pharmacists Association views POCT as an opportunity to enhance revenue and expand direct patient care within pharmacies, and it has been active in state advocacy efforts to expand the scope of practice to include these services.2 The National Association of Chain Drug Stores offers the “Community Pharmacy-based Point-of-Care Testing Certificate.”3 Most recently, the U.S. Department of Health and Human Services under the Public Readiness and Emergency Preparedness Act authorized licensed pharmacists to order and administer COVID-19 tests.4 As part of the pandemic response, pharmacies can temporarily enroll as independent clinical diagnostic laboratories, with Medicare covering COVID-19 testing at the enrolled pharmacies.5
Models of POCT within community pharmacies exist, but POCT is still an emerging area.10, 11, 12, 13, 14, 6, 7, 8, 9 Herbin et al.6 recently reviewed pharmacy-based infectious disease management programs, including POCT as well as the treatment, referral and monitoring of influenza, Group A streptococcus (GAS), human immunodeficiency virus (HIV), and hepatitis C virus (HCV). Models also exist for lipid screening and management within community pharmacy practice.13 , 14
Despite advocacy efforts, recent legislative advancements, and practice exemplars, the uptake of POCT within pharmacies at state and national levels is largely unknown. Qualitative interviews of pharmacy managers and staff pharmacists at 8 community pharmacies in New York and Pennsylvania revealed that only 3 pharmacies (37.5%) provided POCT services.15 A national survey of 485 community pharmacists found that only 12.6% engaged in POCT.16 Neither of the aforementioned studies explored which types of tests were being conducted or what the barriers or facilitators were to service implementation.
Steltenpohl et al.17 examined the successful implementation of POCT in Pennsylvania community pharmacies. Six community pharmacies offering POCT participated in qualitative interviews through which the researchers identified key tools for successful implementation. Although this illustrated the lived experience of a small sample of pharmacies, it did not depict a widespread picture of the status and direction of POCT or identify the factors contributing to the limited uptake within community pharmacies. A multistate survey of 101 independent community pharmacists addressed some of these questions as it relates to pharmacogenomic testing; however, the results are not necessarily transferable to other types of POCT.18
Identifying the current status and trajectory of community pharmacy POCT at state levels can assist pharmacies, universities, and state organizations in guiding the allocation of time, resources, and training in a manner that helps community pharmacy practice meet local societal needs.19 Nationally, calls have been made for educators to optimize training of students and practicing pharmacists, and locally in Wisconsin a strategic priority of the University of Wisconsin-Madison School of Pharmacy is to help the profession meet the needs of patients in the state.20 Understanding the local landscape of POCT can inform the training and professional development efforts of schools of pharmacy and state organizations. In Wisconsin, approximately 15% of the community pharmacies hold Clinical Laboratory Improvement Amendments (CLIA) waivers; however, it is unclear to what degree POCT services are currently offered and what direction future efforts should take.21
We conducted a statewide survey to better understand the extent of POCT services currently offered, projections of future offerings, and attitudes toward POCT within community pharmacies. The survey aimed to (1) describe the current landscape of POCT in Wisconsin community pharmacies and (2) identify opportunities for the advancement of POCT and the key factors influencing the realization of these opportunities.
Methods
The study was a cross-sectional survey of pharmacy managers at community pharmacies in Wisconsin. The pharmacy that the respondent managed was the focus of the analyses, and the study was granted exemption by the University of Wisconsin Institutional Review Board.
Pharmacies were identified using the Wisconsin Department of Safety and Professional Services (DSPS) list of credentialed sites, which was reviewed to eliminate sites meeting the exclusion criteria (sites whose primary purpose was dispensing medications to patients who had been hospitalized or institutionalized or supplying medications and products for home infusion and sites dispensing medications solely through delivery or remote dispensing).
A sample size was calculated using 95% confidence level and 10% margin of error; the study aimed to survey at least 88 pharmacies. Purposeful random sampling was used to identify a representative sample of Wisconsin pharmacies. The sites were stratified into, and randomly selected from, 6 predefined geographic regions to mirror the distribution of pharmacies across Wisconsin. Student research assistants contacted the sites via telephone to confirm edibility and offer participation using a standardized script. If a manager declined participation or was unreachable after 3 attempts, the research assistants moved down the list of the randomized sites. Recruitment continued until the list had been exhausted or until the end of the study period.
The surveys were administered over the telephone and included Likert scale and open-ended items aimed at assessing the provision of POCT and other services, intent for future involvement or expansion of services, barriers and motivators to offering services, and pharmacy demographics. The survey was grounded in the Theory of Planned Behavior (TPB) to assess the likelihood of future engagement in POCT.22 The TPB items were informed by previous survey work.13 , 22, 23 The items were drafted by the study team, reviewed by 2 outside community pharmacists, and revised based on the feedback.
Descriptive statistics were used to analyze quantitative data. The “Am I Rural? Tool” was used to determine if the pharmacies were located in a rural area, health professional shortage area, or medically underserved area.24 Thematic analysis was performed for qualitative data.25 Two student research assistants compiled and familiarized themselves with the responses and coded data separately, using an inductive approach to group the responses into categories. Once complete, a team member reviewed and reconciled the codes, which were then examined to generate and define emerging themes. A second team member independently reviewed the responses, codes, and themes, and all met to reach consensus on the final themes.
Results
Attempts were made to reach managers at 603 pharmacies, and contact was made with 429 managers, out of which 147 participated in the survey, representing 15.7% of the community pharmacies in Wisconsin. Of those surveyed, 43.5% were in rural areas, reflective of the distribution of pharmacies across Wisconsin. Chain pharmacies (32%), pharmacies within mass merchandizers (17%), and multistore independent pharmacies (17%) were most common.
Of the managers surveyed, 10.9% were very familiar with POCT, whereas 36.7% were somewhat familiar. Regarding CLIA waivers, 4.1% were very familiar, and 18.5% were somewhat familiar. The survey found that 17.1% of the pharmacies were offering POCT, 52.4% were providing physical assessment, and 78.7% were providing medication management. The most common POCT services offered were measurement of blood glucose or glycosylated hemoglobin levels and lipid monitoring, and the most common physical assessment was measurement of vitals (blood pressure, heart rate, weight or height). Of the managers surveyed, 48.3% reported that the pharmacy would likely implement or expand POCT within 5 years.
Table 1 displays the results from the TPB items. Most of the managers surveyed agreed that POCT advances the pharmacy profession (83.6%), improves care of patients (95.2%) and medication outcomes (96.6%), and establishes pharmacists as key members of interprofessional teams (91.1%). Only 47.3% of the respondents agreed that other health professionals would approve of pharmacists’ offering testing, 46.6% agreed that it would be feasible for pharmacies to offer POCT, 18.5% believed that pharmacists would have time to provide services, 23.5% believed that insurers would reimburse for POCT, and 43.5% agreed that testing would be profitable.
Table 1.
TPB survey items
| Survey item | Disagree/strongly disagree (%) | Neutral (%) | Agree/strongly agree (%) |
|---|---|---|---|
| Pharmacist participation in providing POCT services is an important step in moving the profession of pharmacy forward. | 6.9 | 9.6 | 83.6 |
| Offering POCT services in community pharmacies will allow pharmacists to provide a higher level of care to their patients. | 1.4 | 3.4 | 95.2 |
| Providing POCT services within community pharmacies will help to establish pharmacists as important members of the health care team. | 3.4 | 5.5 | 91.1 |
| Pharmacists are qualified to provide POCT services to patients. | 8.2 | 15.8 | 76.0 |
| Patients would seek POCT services in community pharmacies. | 11.0 | 18.5 | 70.6 |
| Physicians and other health care providers will approve of pharmacists providing POCT services to patients. | 19.2 | 33.6 | 47.3 |
| I know of other pharmacies currently offering POCT. | 44.8 | 7.6 | 47.6 |
| Pharmacy employers will support pharmacists providing POCT services to patients in the pharmacy. | 7.5 | 30.1 | 62.3 |
| Insurers will reimburse pharmacists for providing POCT services to patients. | 37.9 | 38.6 | 23.5 |
| Pharmacists have the necessary knowledge and skills to provide POCT services to patients. | 8.2 | 12.3 | 79.5 |
| It will be feasible for the pharmacy I work at to begin offering POCT services. | 39.0 | 14.4 | 46.6 |
| Pharmacists will have the necessary time to provide POCT services. | 56.9 | 24.7 | 18.5 |
| Pharmacists will need to offer POCT services to stay competitive. | 22.8 | 23.5 | 53.8 |
| Pharmacies will be able to identify and recruit patients for a POCT program. | 3.5 | 24.8 | 71.7 |
| Offering POCT services within community pharmacies is likely to be profitable for pharmacies. | 24.8 | 31.7 | 43.5 |
| Pharmacists can decrease health care costs by providing POCT services to patients in community pharmacies. | 3.5 | 9.7 | 86.9 |
| Providing POCT services within community pharmacies will give pharmacists the ability to improve medication outcomes for patients. | 1.4 | 2.1 | 96.6 |
| Providing POCT services within community pharmacies will increase the stress level of pharmacists at work. | 6.2 | 19.9 | 74.0 |
| Offering POCT services will attract more patients to my pharmacy. | 11.0 | 27.6 | 61.4 |
| I will actively work to ensure a role for pharmacists at my pharmacy in the provision of POCT services to patients. | 17.2 | 29.0 | 53.8 |
| I will actively work to ensure that adequate reimbursement is established for the provision of POCT services offered at my pharmacy. | 15.9 | 29.0 | 55.2 |
| I intend to seek further training on providing POCT services to patients. | 17.1 | 22.6 | 60.3 |
| I know of other pharmacies that intend to begin offering POCT services. | 62.0 | 17.2 | 21.4 |
| Students at University of Wisconsin-Madison School of Pharmacy should receive instruction on POCT to adequately prepare them for community pharmacy practice. | 6.9 | 6.9 | 86.2 |
Abbreviations used: TPB, Theory of Planned Behavior; POCT, point-of-care testing.
Note: n = 147.
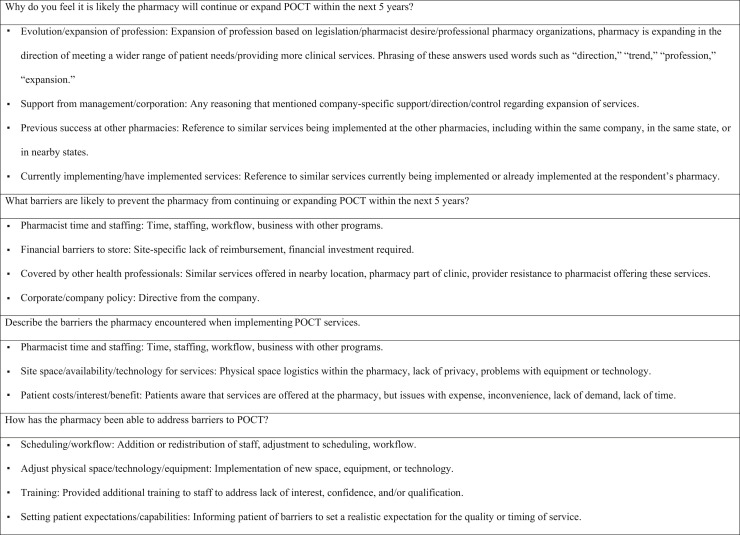
Figure 1 lists the themes that emerged from open-ended items. The motivators for continuing or expanding POCT included alignment with the evolution of community pharmacy practice, supportive leadership, observed success at other pharmacies, and investment in implementing services. Challenges with time and staffing were encountered in pharmacies currently offering POCT and were identified as barriers to expanding or first implementing services. Financial concerns and corporate policy restrictions were also recognized barriers. The managers of pharmacies embedded in clinics or affiliated with larger health systems described overlap in offering POCT services as a barrier.
Figure 1.
Emergent themes from thematic analysis of open-ended responses. Note: Themes listed in order of frequency. Abbreviation used: POCT, point-of-care testing.
Discussion
Few pharmacies in Wisconsin offer POCT, consistent with the low number holding CLIA waivers. However, most of the surveyed managers view POCT as a way to advance the profession, establish pharmacists as key team members, and improve patient care; therefore, unsurprisingly, 48.3% desire to continue, expand, or launch POCT within 5 years.
The perception that POCT overlaps with what is offered by other clinicians was cited as a reason for not implementing these services. Although only 47.3% of those surveyed believe that other health professionals approve of pharmacists’ providing POCT, these perceptions were likely influenced by where a particular pharmacy was housed and its proximity to other health care facilities. Encountering overlapping services or lack of physician support for POCT was not commonly mentioned by managers in the pharmacies already offering such services.
Needs assessment can help pharmacies develop services that fit local communities and health systems by avoiding duplicative efforts that prompt competition.17 , 26 Two studies examining community pharmacy–based GAS testing found that 43%-54% of the patients using the services did not have a primary care physician (PCP), and 38%-44% visited outside the traditional clinic hours.9 , 27 Approximately one-third of the community pharmacies in Wisconsin are located in areas with known primary care shortages, as determined by an analysis of the DSPS list. Pharmacies could fill a void by increasing access to care through collaboration with PCPs to identify services that meet community needs. Lack of access to COVID-19 testing in certain areas and populations is an example of an emergent need that pharmacies could address through POCT.
In the survey, the managers believed that patients would seek POCT within local pharmacies. A recent examination of influenza and GAS testing within a community pharmacy supports this finding. Patients embraced the service, with 98% reporting satisfaction and willingness to use it again.7 Increased awareness of the role of community pharmacists in COVID-19 testing could further enhance the acceptability of pharmacy-based POCT services to patients and providers, although this remains to be seen.
Financial factors were also identified as a barrier to the implementation or expansion of POCT. A separate study examining barriers to successful implementation of community-based pharmacy services found that lack of provider status prevents independent billing, which in turn limits the ability of pharmacies to demonstrate the value necessary for sustaining these services.28 The pharmacy managers in the current survey share this concern. Although 61.4% believe that offering POCT would attract more patients, only 23.5% believe that insurers would reimburse for POCT, and 43.5% believe that pharmacies could profit. It should be noted that the survey was conducted before the temporary ruling on Medicare coverage for COVID-19 testing in pharmacies.
Previous studies support these findings and speak to the financial challenges that community pharmacies face when launching POCT programs. An exploration of consumer willingness to pay for POCT found that patients are willing to pay out of pocket for testing in a pharmacy, but the amount that they are willing to pay is nominal, with 79% endorsing a willingness to pay only up to $50.29 Another study looking at patient willingness to receive HCV testing found that 71.7% were willing to be screened in a pharmacy, but only 34.5% were willing to pay more than $20.30
Although financial challenges exist, they are not insurmountable. Although the managers in pharmacies without an established POCT cited cost as a barrier, difficulty with financial sustainability was infrequently described by those in the pharmacies currently offering these services, suggesting that reliable financial models exist.
The impact of POCT on pharmacy workflow and resources presents another hurdle. Availability of pharmacist oversight was the most common barrier to offering or expanding POCT. Only 46.6% agreed that it would be feasible for pharmacies to offer POCT, 18.5% agreed that community pharmacists have the time, and 74.0% agreed that it would increase stress levels. Logistical challenges such as personnel and workflow were also identified in a separate qualitative study of industry leadership aimed at examining barriers and facilitators to POCT in community pharmacies.31
For a POCT program to be successful, pharmacists must balance the time spent delivering testing with competing responsibilities.8 Pharmacies should explore how testing fits into the existing practice environment. This includes identifying the staffing, pharmacy technician role, time, workflow, space requirements, and patient privacy necessary for a successful POCT program and considering how the pharmacy could be restructured to meet these needs.17 , 26 The managers spoke to the importance of this in the interviews, identifying a re-examination of schedules and workflow and a readjustment of physical space, technology, and equipment as key strategies for implementing POCT. Innovative practice models are being examined to help pharmacies grapple with the issue of how to address logistical constraints. Using certified pharmacy technicians in POCT support roles has been studied as a means to operationalize service delivery within pharmacies.14
Appropriate training and credentialing are essential to the successful implementation of POCT.32 Most of the managers agreed that pharmacists are qualified to provide testing and have the necessary knowledge and skills; however, only 47.6% endorsed familiarity with POCT and 22.6% with CLIA waivers. Other studies have reported similar results. A survey of pharmacist awareness of HIV and HCV testing found that only 22% were aware that such screenings are available through POCT.33 Overall, this speaks to the shared impact that schools/colleges of pharmacy and professional organizations can have on enhancing awareness and expanding training efforts.20 The survey found that 86.2% of the managers believe that schools of pharmacy should provide POCT training to prepare graduates for community practice.
The present study has several limitations. The COVID-19 pandemic was not explored in the survey because its onset occurred after data collection was completed. Discussion of its potential impact is therefore speculative. It is unknown how the pandemic will affect the long-term trajectory of POCT in pharmacies, but, as discussed, in the short-term it could be a motivator.
The survey was not validated and was susceptible to social desirability bias. The responses may have been influenced by what the managers perceived would be most acceptable to the interviewers or positively perceived by the pharmacy profession. It was also confined to the perspective of a sample of managers within Wisconsin.
Although the results speak to state-level community pharmacy practice, certain results seem universal and applicable at a national level. The trends in the responses identified in the survey are consistent with, and grounded in, the work done by researchers looking at POCT elsewhere. They also provide key messages for anyone involved in training the next generation of pharmacists and those engaged in efforts to grow momentum around POCT expansion.
Despite the acknowledged barriers, most of the managers believe that POCT allows pharmacists to provide a higher level of care and improve health outcomes. The managers shared various reasons for continuing, expanding, or launching POCT, but advancing practice and meeting a wider range of patient needs were highest on the list. Regional or state needs assessment can inform training efforts and allocate resources on the basis of the needs of local community pharmacies and the patients that they serve. A similar approach can be applied by others to ensure that curricular and professional development efforts around POCT support the trajectory of local, state, and regional community pharmacy practice.
Conclusion
The current survey found that few pharmacies offer POCT in Wisconsin, but there is motivation for expansion. This needs analysis offers a blueprint for researchers, educators, and clinicians to shape POCT efforts by examining the landscape of pharmacy-based testing in their own states and communities.
Acknowledgments
The authors would like to thank Robert Hetue, Allison Martin, Mark Cinquegrani, Shauna MacKenzie, and Gabriela Loveland for their work on the project. They would also like to thank University of Wisconsin-Madison School of Pharmacy for funding the project.
Biographies
Casey E. Gallimore, PharmD, MS, Associate Professor, University of Wisconsin-Madison School of Pharmacy, Madison, WI
Andrea L. Porter, PharmD, Associate Professor, University of Wisconsin-Madison School of Pharmacy, Madison, WI
Susanne G. Barnett, PharmD, BCPS, Associate Professor, University of Wisconsin-Madison School of Pharmacy, Madison, WI
Edward Portillo, PharmD, Assistant Professor, University of Wisconsin-Madison School of Pharmacy, Madison, WI
Joseph A. Zorek, PharmD, BCGP, Director, Linking Interprofessional Networks for Collaboration, Office of the Vice President for Academic, Faculty and Student Affairs, and Associate Professor, School of Nursing, The University of Texas Health Science Center at San Antonio, San Antonio, TX
Footnotes
ORCID Casey E. Gallimore: http://orcid.org/0000-0002-2626-7673.
Disclosure: The authors declare no relevant conflicts of interest or financial relationships.
References
- 1.American Pharmacists Association APhA policy manual. https://www.pharmacist.com/policy-manual Available at:
- 2.National Community Pharmacist Association Scope of practice and compensation for services. https://ncpa.org/scope-of-practice-and-compensation-for-services Available at:
- 3.National Association of Chain Drug Stores Community pharmacy-based point-of-care testing certificate program. http://nacds.learnercommunity.com/Point-of-Care-Testing-Certificate Available at:
- 4.U.S. Department of Health and Human Services HHS statements on authorizing licensed pharmacists to order and administer COVID-19 tests. https://www.hhs.gov/about/news/2020/04/08/hhs-statements-on-authorizing-licensed-pharmacists-to-order-and-administer-covid-19-tests.html Available at:
- 5.Centers for Medicare and Medicaid Services Medicare pharmacies and other suppliers may temporarily enroll as independent clinical diagnostic laboratories to help address COVID-19 testing. https://www.cms.gov/files/document/se20017.pdf Available at:
- 6.Herbin S.R., Klepser D.G., Klepser M.E. Pharmacy-based infectious disease management programs incorporating CLIA-waived point-of-care tests. J Clin Microbiol. 2020;58(5) doi: 10.1128/JCM.00726-19. e00726-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirby J., Mousa N. Evaluating the impact of influenza and streptococcal point-of-care testing and collaborative practice prescribing in a community pharmacy setting. J Am Pharm Assoc (2003) 2020;60(3S):S70–S75. doi: 10.1016/j.japh.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Dong B.J., Lopez M., Cocohoba J. Pharmacists performing hepatitis C antibody point-of-care screening in a community pharmacy: a pilot project. J Am Pharm Assoc (2003) 2017;57(4):510–515.e2. doi: 10.1016/j.japh.2017.04.463. [DOI] [PubMed] [Google Scholar]
- 9.Klepser D.G., Klepser M.E., Dering-Anderson A.M., Morse J.A., Smith J.K., Klepser S.A. Community pharmacist-physician collaborative streptococcal pharyngitis management program. J Am Pharm Assoc (2003) 2016;56(3):323–329.e1. doi: 10.1016/j.japh.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Weidle P.J., Lecher S., Botts L.W. HIV testing in community pharmacies and retail clinics: a model to expand access to screening for HIV infection. J Am Pharm Assoc (2003) 2014;54(5):486–492. doi: 10.1331/JAPhA.2014.14045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Darin K.M., Klepser M.E., Klepser D.E. Pharmacist-provided rapid HIV testing in two community pharmacies. J Am Pharm Assoc (2003) 2015;55(1):81–88. doi: 10.1331/JAPhA.2015.14070. [DOI] [PubMed] [Google Scholar]
- 12.Kugelmas M., Pedicone L.D., Lio I., Simon S., Pietrandoni G. Hepatitis C point-of-care screening in retail pharmacies in the United States. Gastroenterol Hepatol (N Y) 2017;13(2):98–104. [PMC free article] [PubMed] [Google Scholar]
- 13.Haggerty L., Tran D. Cholesterol point-of-care testing for community pharmacies: a review of the current literature. J Pharm Pract. 2017;30(4):451–458. doi: 10.1177/0897190016645023. [DOI] [PubMed] [Google Scholar]
- 14.Hill H., Cardosi L., Henson L. Evaluating advanced pharmacy technician roles in the provision of point-of-care testing. J Am Pharm Assoc (2003) 2020;60(4):e64–e69. doi: 10.1016/j.japh.2020.02.024. [DOI] [PubMed] [Google Scholar]
- 15.Bacci J.L., Coley K.C., McGrath K., Abraham O., Adams A.J., Somma McGivney M. Strategies to facilitate the implementation of collaborative practice agreements in chain community pharmacies. J Am Pharm Assoc (2003) 2016;56(3):257–265.e2. doi: 10.1016/j.japh.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Doucette W.R., Rippe J.J., Gaither C.A., Kreling D.H., Mott D.A., Schommer J.C. Influences on the frequency and type of community pharmacy services. J Am Pharm Assoc (2003) 2017;57(1):72–76.e1. doi: 10.1016/j.japh.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Steltenpohl E.A., Barry B.K., Coley K.C., McGivney M.S., Olenak J.L., Berenbrok L.A. Point-of-care testing in community pharmacies: keys to success from Pennsylvania pharmacists. J Pharm Pract. 2018;31(6):629–635. doi: 10.1177/0897190017735243. [DOI] [PubMed] [Google Scholar]
- 18.Alexander K.M., Divine H.S., Hanna C.R., Gokun Y., Freeman P.R. Implementation of personalized medicine services in community pharmacies: perceptions of independent community pharmacists. J Am Pharm Assoc (2003) 2014;54(5):510–517. doi: 10.1331/JAPhA.2014.13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Porter A.L., Portillo E.C., Gallimore C.E., Zorek J.A., Barnett S.G. Let external stakeholders be your guide to curricular revision. Am J Pharm Educ. 2020;84(8) doi: 10.5688/ajpe8021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kehrer J.P., James D.E. The role of pharmacists and pharmacy education in point-of-care testing. Am J Pharm Educ. 2016;80(8):129. doi: 10.5688/ajpe808129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Clinical Laboratory improvement amendments (CLIA) laboratory search. http://wwwn.cdc.gov/clia/Resources/LabSearch.aspx Available at:
- 22.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J., Beckman J., editors. Action-Control: From Cognition to Behavior. Springer; Heidelberg, Germany: 1985. [Google Scholar]
- 23.Herbert K.E., Urmie J.M., Newland B.A., Farris K.B. Prediction of pharmacist intention to provide medicare medication therapy management services using the theory of planned behavior. Res Social Adm Pharm. 2006;2(3):299–314. doi: 10.1016/j.sapharm.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Rural Health Information Hub Am I Rural? – Tool. https://www.ruralhealthinfo.org/am-i-rural Available at:
- 25.Maguire M., Delahunt B. Doing a thematic analysis: a practical, step-by-step guide for learning and teaching scholars. AISHE-J. 2017;9(3):3351–33514. [Google Scholar]
- 26.Rodis J.L., Thomas R.A. Stepwise approach to developing point-of-care testing services in the community/ambulatory pharmacy setting. J Am Pharm Assoc (2003) 2006;46(5):594–604. doi: 10.1331/1544-3191.46.5.594.rodis. [DOI] [PubMed] [Google Scholar]
- 27.Klepser D.G., Klepser M.E., Smith J.K., Dering-Anderson A.M., Nelson M., Pohren L.E. Utilization of influenza and streptococcal pharyngitis point-of-care testing in the community pharmacy practice setting. Res Social Adm Pharm. 2018;14(4):356–359. doi: 10.1016/j.sapharm.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen E., Holmes J.T. Pharmacist-provided services: barriers to demonstrating value. J Am Pharm Assoc (2003) 2019;59(1):117–120. doi: 10.1016/j.japh.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 29.Hohmeier K.C., Loomis B., Gatwood J. Consumer perceptions of and willingness-to-pay for point-of-care testing services in the community pharmacy. Res Social Adm Pharm. 2018;14(4):360–366. doi: 10.1016/j.sapharm.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Brewer A., Hanna C., Eckmann L., Schadler A., Divine H. Patient awareness, willingness, and barriers to point-of-care hepatitis C screening in community pharmacy. J Am Pharm Assoc (2003) 2018;58(4S):S69–S72.e1. doi: 10.1016/j.japh.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 31.Hohmeier K.C., McDonough S.L.K., Wang J. Co-creation of market expansion in point-of-care testing in the United States: industry leadership perspectives on the community pharmacy segment. Res Social Adm Pharm. 2017;13(4):746–753. doi: 10.1016/j.sapharm.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Gubbins P.O., Klepser M.E., Dering-Anderson A.M. Point-of-care testing for infectious diseases: opportunities, barriers, and considerations in community pharmacy. J Am Pharm Assoc (2003) 2014;54(2):163–171. doi: 10.1331/JAPhA.2014.13167. [DOI] [PubMed] [Google Scholar]
- 33.Min A.C., Andres J.L., Grover A.B., Megherea O. Pharmacist comfort and awareness of HIV and HCV point-of-care testing in community settings. Health Promot Pract. 2020;21(5):831–837. doi: 10.1177/1524839919857969. [DOI] [PubMed] [Google Scholar]