To the Editor:
The COVID-19 pandemic has caused an abrupt shift in the way care is delivered in cardiovascular intensive care units (CICUs). One example of this drastic change has been the limitations placed on family visitation. In many hospitals across Canada and beyond, a strict "no visitor" policy has been implemented. Governments and hospital administrators have instituted this policy to prevent the spread of infection and preserve protective equipment. However, physical distancing may lead to social isolation and emotional distress for both patients and their families. In addition, overstretched health care workers may prioritize life-saving work over communication with family members, leading to a breakdown in the physician-patient-family care axis. Cultural and language barriers may further exacerbate this disconnect. As result, family members may have concerns regarding the potential for health care workers to transmit infection to their loved ones and whether their care needs (physical, emotional, and spiritual) are being met.
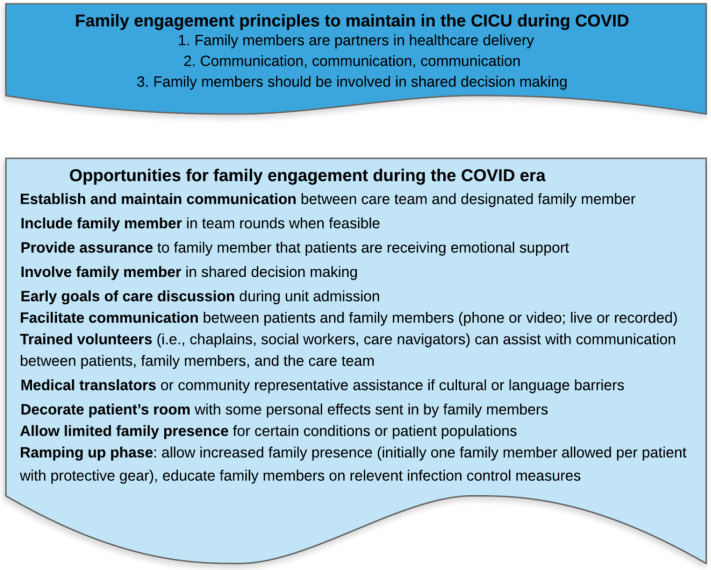
We recently described opportunities to engage family members in care in the CICU.1 Yet despite the new challenges to family engagement in the COVID-19 era, there are still opportunities to engage patients and family members while providing optimal cardiovascular critical care (Fig. 1 ). An effective and regular system for communication between the CICU team and a designated family member is likely the best way to keep family members engaged. For example, semistructured communication sessions between the family and health care members can be scheduled on a regular basis. Facilitating communication between patients and their families via phone or videoconferencing can help bridge the distance. Specially designed patient communication apps can facilitate patient-family-clinician interactions.2 Family members could participate virtually in daily team rounds. A designated family member could even be allowed to be present at the bedside as an “essential care partner” in specific CICUs (ie, in regions with low rates of COVID-19) or for certain patients (ie, older adults with or without dementia, those with cultural or language barriers, and for the compassionate care of critically ill patients and those on palliative care).
Figure 1.
Family engagement principles and opportunities in the cardiac intensive care unit during COVID-19.
Although the nature of the partnership may have changed temporarily, family members are not merely “visitors” in the CICU but rather are key partners in the delivery of health care. Although family members may not be present at the bedside, their role and contribution to patient care can be, and should be, maintained to provide optimal patient- and family-centred care. When the pandemic wanes and health care delivery returns to a “new-normal,” it will be important to increase and strengthen family engagement in CICU care.
Funding Sources
The authors report no funding sources relevant to the contents of this paper.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Goldfarb M, Bibas L,Burns K. Patient and family engagement in care in the cardiac intensive care unit. Can J Cardiol. 10.1016/j.cjca.2020.03.0.37. [DOI] [PubMed]
- 2.Society of Critical Care Medicine Patient Communicator App. https://www.sccm.org/Education-Center/Clinical-Resources/Patient-and-Family Available at: