Just as hope for relief from the COVID-19 pandemic brightened in December, with emergency use approval for vaccines following phase 3 trials and the start of immunisation programmes, unprecedented numbers of cases, hospital admissions, and deaths have been recorded, including in countries such as Germany and Japan that were previously celebrated for their public health response. Predictions that the northern hemisphere winter would be a difficult time for control of COVID-19, as is typically the case with respiratory viral diseases, have proved to be correct. Emergence in South Africa and the UK of new variants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that are substantially more transmissible, has added to concerns that health services will be overwhelmed.
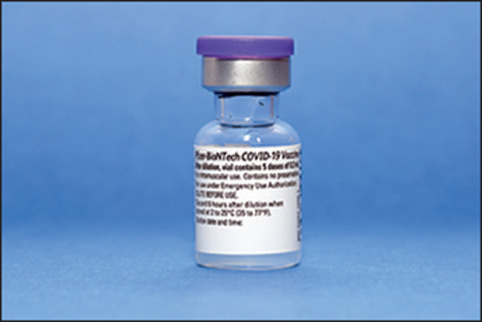
Alarm over the rapid rise in cases led to an unexpected policy twist in the UK on Dec 30: on top of a third national lockdown, the chief medical officers of the four nations of the UK announced that the second dose of vaccines against SARS-CoV-2 should be given at up to 12 weeks after the first dose rather than the recommended interval of 3–4 weeks, on the basis of advice from the Joint Committee on Vaccination and Immunisation (JCVI). While supplies of vaccine remain limited, the JCVI recommends “initially prioritising delivery of the first vaccine dose as this is highly likely to have a greater public health impact in the short term and reduce the number of preventable deaths from COVID-19”. The rationale is that if 95% of people are protected from disease after two doses (as determined in the phase 3 trial of the Pfizer-BioNTech vaccine) and 90% after one dose (JCVI estimate), then 19 of 20 people will be protected by two doses but when given as single doses to 40 people 36 will be protected. The WHO Strategic Advisory Group of Experts (SAGE) on immunisation has advised that the interval between doses of the Pfizer-BioNTech vaccine can be up to 6 weeks in “exceptional epidemiological circumstances”. The Canadian province of British Columbia will extend the vaccine interval to 5 weeks, and other countries are reported to be considering extending the dosing interval while awaiting delivery of more vaccine.
Given that vaccine approval is based on a dosing interval of 3 or 4 week, that efficacy of single doses was not formally tested in randomised trials, and that estimated efficacy of single doses is based on unplanned analyses of few data from these trials, the decision to prioritise the first dose has naturally drawn criticism. The British Medical Association described the decision as “unreasonable and totally unfair”, pointing out the logistical difficulties in rebooking vaccination appointment for the elderly and vulnerable people who have already received their first immunisation. Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases, said that the US vaccination programme would proceed with the approved two-dose schedule, noting the lack of data on extending the period to the second immunisation.
An important concern is the durability of immunity in the extended dosing interval. Some COVID-19 cases after the first vaccine dose are inevitable among people infected around the time of immunisation—as was observed in clinical trials—because protective immunity takes about 2 weeks to become established. However, if immunity wanes during the interval between doses, post-vaccination infections will be more common, thus reducing the impact of—and public confidence in—the vaccination programme. As John Roberts and colleagues point out, duration of immunity to viral spike protein induced by mRNA vaccines such as the Pfizer-BioNTech and Moderna ones is unknown, and in animal models neutralising antibody production falls at about 28 days from first vaccination. By contrast, these authors note that for viral-vector vaccines (eg, Oxford-AstraZeneca ChAdOx1), there is evidence to support an extended interval between doses. Another unknown is whether potentially suboptimal immunity will foster evolution of vaccine-escape mutants of SARS-CoV-2. In this regard, some reassurance comes from a report that the Pfizer-BioNTech vaccine produces antibodies that neutralise SARS-CoV-2 carrying the N501Y mutation found in the South African and UK variants.
Independent SAGE, a group of UK scientists not known for their support of government COVID-19 policy, has endorsed the decision “to pursue coverage of as high a proportion of the population as possible, as quickly as possible”, noting that it must be part of a comprehensive strategy that includes prospective evaluation of different dosing intervals. Given the urgent need to suppress a rise in cases caused by a new viral variant, we believe that extending the dosing interval is an expedient, short-term decision while there are constraints on vaccine supply.
© 2021 Dr P Marazzi - Science Photo Library


