Abstract
Introduction
During the SARS-CoV-2 pandemic, the majority of healthcare resources of the affected Italian regions were allocated to COVID-19 patients. Due to lack of resources and high risk of death, most cancer patients have been shifted to non-surgical treatments. The following reports our experience of a Gynaecologic Oncology Unit's reallocation of resources in a COVID-19 free surgical oncologic hub in order to guarantee standard quality of surgical activities.
Materials and methods
This is a prospective observational study performed in the Gynaecologic Oncology Unit, on the outcomes of the reallocation of surgical activities outside the University Hospital of Bologna, Italy, during the Italian lockdown period. Here, we described our COVID-19 free surgical oncologic pathway, in terms of lifestyle restrictions, COVID-19 screening measures, and patient clinical, surgical and follow up outcomes.
Results
During the lockdown period (March 9th – May 4th, 2020), 83 patients were scheduled for oncological surgery, 51 patients underwent surgery. Compared to pre-COVID period, we performed the same activities: number of cases scheduled for surgery, type of surgery and surgical and oncological results. No cases of COVID-19 infection were recorded in operated patients and in medical staff. Patients were compliant and well accepted the lifestyle restrictions and reorganization of the care.
CONCLUSIONSonclusions
Our experience showed that the prioritization of oncological surgical care and the allocation of resources during a pandemic in COVID-19 free surgical hubs is an appropriate choice to guarantee oncological protocols.
Keywords: Ovarian cancer, Gynaecological cancers, SARS-CoV-2, COVID-19, Pandemic, Allocation resources
1. Introduction
A new infection identified as SARS-CoV-2 (COVID-19) by the World Health Organization (WHO) has rapidly spread worldwide since the first case was reported on December 31st, 2019 from China [1]. The COVID-19 infection had its initial epidemic manifestations in Italy on January 31st, 2020, when two Chinese tourists tested positive in Rome. An outbreak of COVID-19 infections was subsequently detected on February 21st, 2020 from 16 confirmed cases in the Lodi area of Lombardy. Very quickly, cases increased to 60 the following day when the first deaths were reported. From there the virus spread rapidly in the nearby Emilia Romagna Region (RER) especially in the cities of Piacenza and Parma. On March 4th, there were around 2700 positive cases in Italy with an infection spread in all regions of the country. On March 8th, the decree of the President of the Italian Council of Ministers sanctioned the isolation of Lombardy and 14 other Italian provinces, which were classified as “red zones”. Several cities of the RER: Parma, Piacenza, Rimini, Reggio Emilia, Modena, Medicina (Bologna), were included in the red zones (S1). On March 9th, the entire Italian territory became a “protected area” until May 8th (lockdown period). A few days later, on March 11th, the WHO declared a pandemic state. The rules of conduct to be adhered by Italians were promoted in the social media campaign #iorestoacasa (”I'm staying home”). It was possible to leave home only for proven reasons of necessity: to buy food or prescription drugs, for essential work needs or health reasons.
The sudden and progressive flow of COVID 19 patients in hospitals became a priority in terms of use of healthcare resources: healthcare workers and, in particular, anesthesiologists and nurses in intensive care units (ICUs) and wards [[2], [3], [4]]. The National Healthcare System was the first in the western world to deal with this health emergency with few and sometimes conflicting available information on how to manage the pandemic [[5], [6], [7], [8]]. Patients and healthcare workers had to be protected and a reorganization was required to provide essential forms of healthcare at least for the most relevant diseases, such as surgery for cancer patients. The few data in the literature in surgical patients infected by COVID-19 reported an increased risk of death of about 25–30%, a high risk of complications in the post-operative course with the frequent need of intensive care treatment for severe breathing difficulties [9,10]. Based on these data and to preserve health resources, in the initial stages of the pandemic the elective procedures were suppressed, ensuring surgical interventions only for high-risk and emergency cases [11].
Surgery is a cornerstone in the treatment of cancer patients. In many cases it represents the first and only approach in achieving survival improvement [12,13]. On the other hand, cancer patients are a population more susceptible to infections due to poor general conditions, coexisting comorbidities, and immunosuppression caused by the tumor itself and/or by anticancer treatments [14,15].
In this framework, contention was emerging: healthcare workers were faced with either continuing to ensure surgery to cancer patients or to shift patients towards non-surgical therapies (chemotherapy and radiotherapy) [16] until the end of the emergency. During the COVID-19 pandemic, the need to preserve maximum resources and to protect patients and healthcare professionals from exposure to contagion prompted surgical and oncological international societies to provide indications towards a reduction in the number of surgical procedures and to consider alternative treatments [[5], [6], [7], [8]]. Even for gynaecological cancers the indications were to avoid surgery. For example, the European Society of Gynaecological Oncology (ESGO) suggested, for newly diagnosed patients with advanced ovarian cancer, to perform only tissue biopsy and to start neoadjuvant chemotherapy. For those already undergoing chemotherapy the suggestion was to continue the systemic therapy until the crisis had been resolved [5].
Postponing or avoiding surgery can theoretically lead to a declining of cure probability and of quality of life of cancer patients, especially those with ovarian cancer [12,17]. From March 1st, the University Hospital of Sant'Orsola in Bologna, RER, drastically reduced all surgical activity and structural resources reassigned to the COVID-19 patients in a fast emergency reorganization. Following this drastic reduction, including the complete interruption of all oncological surgical treatments, the organization of Oncological Surgical hubs (OSH) outside the University Hospital was then considered.
The aim of this report is to describe how the Regional Health System (RHS) organized surgical treatments of Gynaecologic Oncology Unit (GO), the Regional Ovarian Cancer hub, to ensure its regular activity, all the measures taken to preserve patients and healthcare professionals, and the outcomes of this choice.
2. Materials
2.1. Objectives
The main objective of this study was to analyse the results of allocation of surgical activities of the GO in a COVID-19-free OSH. Type and number of treated cases, differences in the therapeutic choices due to the pandemic, complications and risks of COVID-19 infection were evaluated. The secondary endpoint was patient's compliance and satisfaction with this new COVID-19 free care setting.
2.2. Study design
This is a prospective observational study performed at GO, University Hospital of Bologna, Italy, on the outcomes of the allocation of surgical activities outside during the Italian lockdown period. All patients undergoing surgical evaluation and treated for gynaecological cancers were enrolled. The study was approved by the institutional review board (CE:639/2020/Oss/AOUBo).
2.3. Population
Inclusion criteria were: suspected or ascertained gynaecological malignancies potentially amenable to surgical treatment.
Exclusion criteria were: diagnostic tests or biopsy excluding the presence of gynaecological neoplasia even if only suspected; refusal of patients for surgical treatment; contraindications to surgery [12,13,18,19].
2.4. Data collection
Data on COVID-19 epidemic in RER and Italy was collected from the official Italian Civil Protection website:
http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1.
Data on reallocation of institutional healthcare resources to Covid-19 patients were collected from the official documents of our University Hospital. Patients' data were daily archived in a database on an Excel file by the team of doctors who took care of patients. The collected information included: demographic data (age, BMI, place of residence), medical and surgical history (comorbidity and previous surgical interventions), the events during the clinical path from the first access to the last post-surgical check-up, procedures related to COVID-19 screening (nasopharyngeal swab, “ad hoc” interviews, temperature measurement), surgical and oncological data (final histology and tumor staging, Peritoneal Cancer Index [20,21], Completeness of Cytoreduction Score (CC) [22], anaesthesiological data (ICU, P-Possum score, general and epidural anaesthesia), post-operative complications [[23], [24], [25]] up to 30 days after surgery, and number of patients infected by COVID-19.
2.5. Resource's allocation and perioperative care programs of GO during epidemic
The RHS, in agreement with the Italian Association of Private Hospitals, planned two different pathways of which one for COVID-19 patient care and another for cancer surgery. The RHS hospitals of the city of Bologna were completely dedicated to managing COVID-19 patients and urgent outpatient activities while private hospitals were reorganized as OSH for surgical treatment. GO activity was divided into two locations. Patient's selection for surgery, pre-operative assessment and post-surgical activities remained in the outpatient clinic and in pre-operative section of the University Hospital, while surgical activities and ICU were planned and performed in one of the OSHs. The latter provided anaesthesiologists, nurses and paramedics, as well as instruments and consumables. The GO medical team worked in the two facilities without interactions with the COVID departments activities and staffs (S2).
2.6. General measures
General measures were planned to limit access to all therapeutic facilities with check points and dedicated personnel to ensure compliance with restrictive measures. These measures included individual (unaccompanied) patient access, different entry and exit routes, temperature measurement and lifestyle restrictions such as social distancing, use of hand sanitizer gels and surgical mask, and advice to limit contact. The distances to be respected were also indicated through signs positioned on chairs and floors. Moreover, using a questionnaire, region of residence, presence of suspected flu symptoms and any risk of contact with COVID-19 positive subjects were assessed (S3). Online training courses were proposed for healthcare professionals on symptoms recognition, correct swabs execution and dressing of protective equipment. Moreover, restrictive lifestyles were recommended to medical staff and paramedics. Healthcare workers had the opportunity to isolate themselves in hotel rooms made available to protect families in cases of suspected COVID-19 infection or contact with positive subjects.
2.7. Patient's selection for surgery, pre-operative patient's assessment (University Hospital)
The patients were divided into three priority classes: class A, certain or strongly suspected malignant cancer; class B, precancerous lesions; class C, benign tumours.
Only class A patients started the surgical pathway. No changes were made to protocols related to patients' selection for surgery and to surgical technique, except for candidates for robotic surgery (patients with endometrial cancer, BMI> 30) who were shifted to laparoscopic surgery or, as an alternative, radiation therapy.
Patients unsuitable for surgery, but eligible for radiotherapy or chemotherapy, were discussed in the weekly virtual multidisciplinary team meetings. Patients with benign lesions requiring only follow-up were contacted after the end of the emergency.
Patients selected for surgery received detailed information on pathology, type of surgery and surgical procedures to be performed elsewhere due to the pandemic. All the measures planned both in the OSH and at home were discussed. Access to the University Hospital ended with laboratory tests and with surgical-anaesthesiologic risk estimation carried out using a specific score. The latter was carried out on the same day of the surgical visit or during a subsequent visit according to the staff availability and the treatment urgency. All patients underwent nasopharyngeal swab within 48 h before admission to the OSH surgical ward. Surgery was postponed or cancelled only if patients had fever >37.5 °C, showed suspected flu symptoms (dry cough, dyspnoea, diarrhoea), or in case of positive swab tests.
2.8. Surgery department and surgical theatre (OSH)
Admission to the ward took place the day before the operation when the team of anaesthesiologists performed the last patient's check. An entire floor of the OSH building was dedicated only to patients with gynaecological cancers who were accommodated in single rooms. Access to relatives was prohibited and information on intervention and patients' conditions was given by telephone from the surgical staff. The operating room was upgraded with surgical instruments provided by the University hospital, such as a laparoscopic column equipped with a sentinel lymph node identification system, an ultrafiltration system for laparoscopic gas, an argon beam coagulator and mechanical staplers. The surgical activity was performed three times a week from 8 AM to 7 PM.
At discharge, patients were advised to comply with lifestyle restrictions (surgical mask for relatives and contacts limitations). In addition, they completed a questionnaire including 8 items on lifestyle restrictions due to pandemic and 4 items on the pandemic impact on their treatments (S4).
2.9. Post-surgery measures (University Hospital)
Surgical specimens were transferred to and examined by the University Hospital pathologists. In cases of frozen section, a vehicle with dedicated personnel was available to transport surgical specimen. Once the pathological report was made available, all cases were discussed by the multidisciplinary team, some members were connected remotely. Post-surgical management was planned while patients received a copy of the multidisciplinary team report with indications for adjuvant therapies. In cases of benign lesions found on pathological examination, patients were contacted by telephone and further checks were postponed in asymptomatic patients.
2.10. Statistical analysis
Demographic and other categorical clinical data were analysed using descriptive statistics and presented as numbers and percentages while continuous variables were presented as median and range. Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS) software Version 20.0 (SPSS, Chicago, Illinois, USA).
3. Results
3.1. COVID-19 infection and University hospital situation
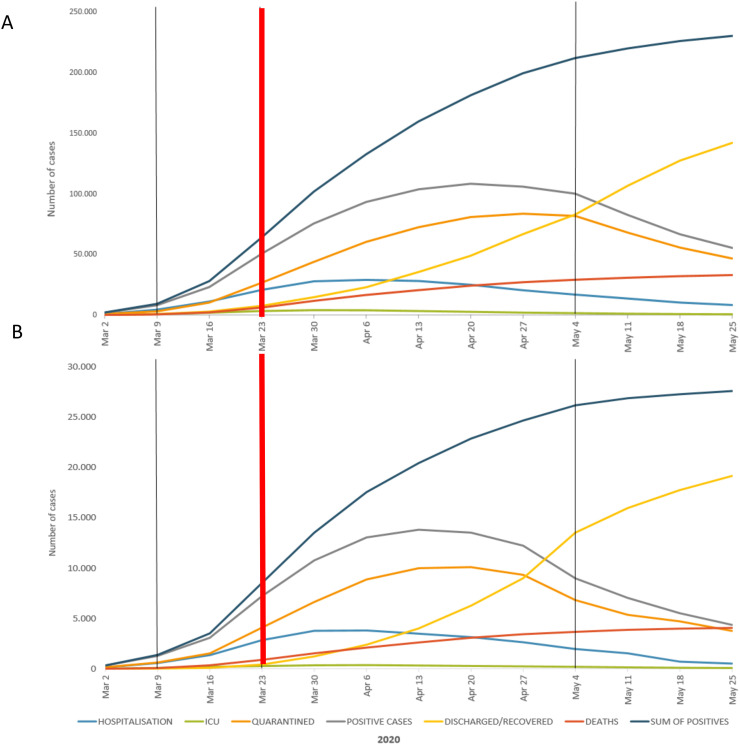
The trend of COVID infection in Italy and in RER during the lockdown are shown in Fig. 1A and B, respectively. The peak of patients who were symptomatic, hospitalized, admitted to intensive care units, quarantined, and who died within 24 h was reached in late March and April. In fact, in RER, the maximum number of these categories was as follows: 3944 cases hospitalized with symptoms on April 2nd, 375 cases hospitalized in ICU on April 5th, and 10,097 cases quarantined on April 19th. From March 23rd to 31st, the number of deaths within 24 h was approximately 100, with a peak of 109 patients who died on March 23rd. From March 9th to 23rd, in the Bologna University Hospital, 433 beds were gradually converted from other specialty units into COVID-19 dedicated bedsides, thereby increasing those already available in the infectious diseases department. These beds were divided as follows: 78 for COVID-19 ICU, 77 for COVID-19 sub intensive care, 43 for patients with suspected COVID-19 infection, and 235 for patients with COVID-19 symptoms. Planned non-oncological surgical activity was quickly suspended. Surgical oncological activity was progressively reduced until closure and transferred to six private or regional health system-affiliated hospitals. From March 9th to 23rd our GO reduced the operating sessions by 50% until closure due to lack of available beds in the ward, operating room, medical staff (anaesthesiologists) and nurses. In fact, all these resources have been committed to COVID-19 infected patients.
Fig. 1.
Epidemiological data about COVID-19 infection in Italy (Fig. 1A) and In Emilia Romagna Region (Fig. 1B).
Legend: The black lines delimit the lockdown period, while the red line indicates the data of the allocation at the COVID-19 free oncologic surgical hub. Hospitalization: number of patients infected with symptoms in the hospitals; ICU: number of admitted in intensive care units; quarantined: subjects isolated for proven or suspected COVID-19 infection; discharged/recovered: number of patients with previous COVID-19 infection; deaths: number of patients dead of COVID-19; sum of positives: total number of infected subject. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2. Patient's and health care screening
Social distancing measures, use of personal protective equipment and lifestyle restrictions were carefully respected by patients and healthcare professionals. All patients underwent active SARS-CoV-2 nasopharyngeal swab screening, using the reverse transcription polymerase chain reaction method, 48 h prior to surgery at the University Hospital. In two patients the test was repeated after one week and the intervention was postponed for 15 days. The first case concerned a patient whose mother died of COVID-19. The second case regarded a patient with mild flu symptoms: fever (38 °C) and dry cough. No positive swabs were recorded in any of surgical patients. Seven patients living in the “red zones” (S1 and Table 1) received two nasopharyngeal swabs: one in the residence area and another in pre-hospitalization centre. In April, all healthcare professionals of the RHS underwent a blood test-based screening for COVID-19 infection. No staff member of GO tested positive. An operating room nurse was quarantined for a week as his wife tested positive for COVID-19. He was asymptomatic and went back to work after two negative nasopharyngeal swabs.
3.3. GO outpatient clinic activities during lockdown
From March 9th to May 4th, 2020, 93 outpatient clinical evaluations were performed for established or suspected diagnosis of gynaecological tumor. Requests for clinical evaluation were carried out by telephone (45), emails (9), contacts from other health facilities (30), and from medical oncology (7) and radiotherapy (2) departments of the Bologna University Hospital.
In 10 patients (11%), the ultrasound and clinical examination did not confirm the suspected cancer. Therefore, four patients were scheduled for a new ultrasound check at the end of emergency and six were referred to annual checks. The 83 patients with suspected or confirmed cancer were scheduled for surgery (56, 68%), radiation (16, 19%), and chemotherapy alone (11, 13%), respectively. Radiotherapy was indicated in two obese patients with endometrial carcinoma and severe comorbidities, in seven cases of locally advanced cervical carcinoma, in two cases of locally recurrent cervical carcinoma, in three cases of locally recurrent endometrial carcinoma, and in two cases of lymph node recurrence. Patients referred to medical oncologists for chemotherapy included six ovarian stage IVB tumours and five multifocal recurrences of ovarian cancer. The treatment choice was modified compared to the non-COVID period only in the two cases of endometrial carcinoma due to lack of robotic surgery and anesthesiologic issues contraindicating laparoscopy. Both patients were treated with radiotherapy instead of surgery.
3.4. GO operating theatre and ward activities during lockdown
During the lockdown period, 63 surgical procedures were performed (seven patients had been planned before March 9th. Resected tumours were as follows: 23 (36%) uterine, 4 vulvar (7%), 23 ovarian (36%) tumours, and one breast cancer associated with uterine cancer (2%). In 13 cases (19%), the frozen section did not confirm the tumor suspicion. Sixty-three percent of patients lived outside the Bologna area and 14% came from the “red zones”. Patient characteristics and place of residence are shown in Table 1 .
Table 1.
Patients' characteristics. General, anesthesiologic and post-operative parameters of the patients scheduled for surgery.
| Variables | Data |
|---|---|
| All patients | 51 |
| General Parameters | mean (± SD) |
| Age, years | 58 (± 11.5) |
| BMI | 25.2 (± 5.5) |
| ECOG Performance Status | n (%) |
| Grade 0 | 25 (49%) |
| Grade 1 | 18 (35%) |
| Grade 2 | 8 (16%) |
| Grade 3–4-5 | 0 (0%) |
| Residence | |
| Bologna | 19 (37%) |
| Emilia-Romagna | 15 (29%) |
| Extra-region | 10 (20%) |
| Red Zones | 7 (14%) |
| Anesthesiological parameters | n (%) |
| ASA Physical Status Classification System | |
| Grade 1 | 1 (2%) |
| Grade 2 | 44 (86%) |
| Grade 3 | 6 (12%) |
| Grade 4–5 | 0 (0%) |
| Epidural analgesia | |
| Yes | 26 (51%) |
| No | 25 (49%) |
| Use of Amines | |
| Yes | 5 (10%) |
| No | 46 (90%) |
| Intensive care admission | |
| Yes | 13 (25%) |
| No | 38 (75%) |
| Possum Score | mean (±SD) |
| Possum mortality | 7.5 ± (8.9) |
| Possum morbidity | 31.7 ± 20.7 |
| Physiological score | 16 (± 2.6) |
| Operative severity score | 13 (± 5.1) |
| Post-operative parameters | n (%) |
| Clavien-Dindo Classification | |
| Grade 0 | 34 (67%) |
| Grade I | 5 (10%) |
| Grade II | 9 (17%) |
| Grade IIIa | 2 (4%) |
| Grade IIIb | 1 (2%) |
| Grade IV-V | 0 (0%) |
| Blood transfusions | |
| Yes | 11 (22%) |
| No | 40 (78%) mean (±SD) |
| Hospital stay, days | 6 ± (4.2) |
wFor cases of ovarian tumours with risk of carcinosis, the first approach was laparoscopic for the evaluation of operability and subsequent laparotomy if the patient was considered optimally cytoreductive. Complete cytoreduction was achieved in 70% of patients with ovarian carcinosis (Table 2 ). No changes in the decision-making process on surgical strategies (reduction of surgical resection extension, referral to neoadjuvant chemotherapy in candidate for cytoreduction patients, or other changes of the surgical approach) due to the risk of COVID-19 infection were recorded. A laparotomic access was used in advanced ovarian tumours, cervical cancers, and sarcomas. The laparoscopic access was preferred in endometrial cancers managed with the sentinel lymph node protocol. A fume extractor to reduce the diffusion of intra-abdominal gases in the operating room was used in both laparoscopic and laparotomic cases.
Table 2.
Surgical parameters in patients with ovarian and endometrial cancer.
| Variables | Ovarian Cancer |
Endometrial Cancer |
||
|---|---|---|---|---|
| n | % | n | % | |
| All | 23 | 100 | 16 | 100 |
| Patients with primary diagnosis | 21/23 | 91 | 16/16 | 100 |
| Up-front Surgery | 14/21 | 67 | 15/16 | 94 |
| Interval Debulking Surgery | 7/21 | 33 | 1/16 | 6 |
| After 3–4 cycles of chemotherapy | 4/7 | 57 | 0/16 | 0 |
| After 6 cycles of chemotherapy | 3/7 | 43 | 1/16 | 6 |
| Patients with relapse | 2/23 | 9 | 0/16 | 0 |
| Surgical complexity score (Aletti's Score) | ||||
| Low (≤ 3) | 11/23 | 48 | 15/16 | 94 |
| Intermediate (4–7) | 11/23 | 48 | 1/16 | 6 |
| High (≥ 8) | 1/23 | 4 | 0/16 | 0 |
| Type of surgery | ||||
| Laparoscopic surgery | 2/23 | 9 | 14/16 | 88 |
| Diagnostic Laparoscopy for operability | 3/23 | 13 | 0/16 | 0 |
| Diagnostic Laparoscopy + laparotomic surgery | 14/23 | 61 | 0/16 | 0 |
| Laparotomic surgery | 4/23 | 17 | 2/16 | 12 |
| Completeness of cytoreduction score (CC) | ||||
| CC-0 (no macroscopic residual disease) | 16/23 | 70 | 16/16 | 100 |
| CC-1 (residual disease <2.5 mm) | 1/23 | 4 | 0 | 0 |
| CC-2 (residual disease >2.5 mm and < 25 mm) | 6/23 | 26 | 0 | 0 |
| CC-3 (residual disease >25 mm) | 0/23 | 0 | 0 | 0 |
| FIGO stage | ||||
| I | 5/23 | 22 | 15/16 | 94 |
| II | 0/23 | 0 | 0/16 | 0 |
| III | 18/23 | 78 | 1/16 | 6 |
| IV | 0/23 | 0 | 0/16 | 0 |
Surgical parameters results (Table 2) showed medium to high surgical complexity and required ICU in 25% of patients in ovarian cancer cases. On the second post-operative day, fever higher than 38 °C was recorded in four patients without flu symptoms, successfully treated with antibiotic therapy. Two patients underwent an additional nasopharyngeal swab, with negative results, due to >37.5 °C fever associated to mild flu symptoms (dry cough). In anticipation for the swab's results, patients were isolated and prudentially considered as COVID-19 positive. Serious complications were observed in three (6%) cases: two patients with ovarian cancer and one with cervical cancer. In detail, seven days after resection of a pelvic recurrence from clear cell carcinoma of the ovary, one patient developed a pelvic abscess. This complication did not require surgery and was resolved with a CT guided drainage and intravenous antibiotic therapy. Three days after surgery for stage IIIC ovarian cancer, severe anaemia due to intra-abdominal bleeding occurred in a second patient. The third patient was readmitted one week after discharging due to suprafascial hematoma and a wound toilet was considered. Finally, a mild complication was observed in a patient requiring a re-evaluation in the emergency room five days after discharging due to fever and cutaneous rush produced by an allergic reaction to painkillers.
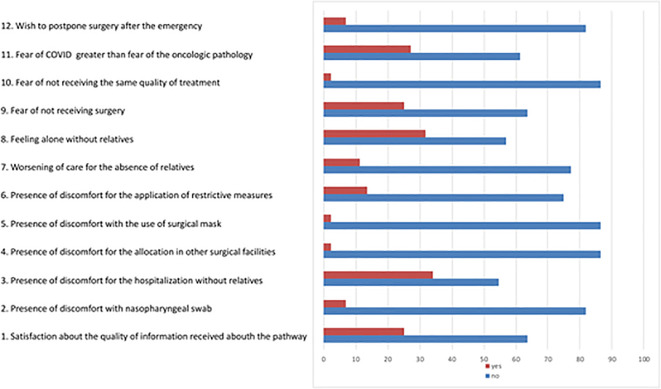
The compliance questionnaire was completed by 41 patients (80%). The relocation of surgical activities in the COVID-19-free OSH and the adopted restrictive measures were positively accepted in more than 65% of patients, as shown in Fig. 2 .
Fig. 2.
Results of the questionnaire filled by patients admitted to COVID-19 free oncologic surgical Hub. The graphic reports the percentage of patients' acceptance of the newpath. Legend: numbers represent the 12 items of the questionnaire. Blue lines represent the percentage of negative answers, red lines represent the percentage of positive answers. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.
We reviewed patients in the outpatient clinic for post-operative check after an average of 25 days from discharge. All patients claimed to have respected the restrictive lifestyle and no COVID-19 infection was recorded.
3.5. Epidemic versus non-epidemic period
After careful clinical evaluation, we excluded surgery in two patients with endometrial cancer potentially amenable to robotic surgery. In fact, severe comorbidities and obesity contraindicated laparoscopic surgery and patients were referred to the radiotherapy department. We also excluded palliative surgery (pelvic exenteration) in a 39-year-old patient with locally advanced cervical carcinoma and metastatic lymph node recurrent after concurrent chemoradiation.
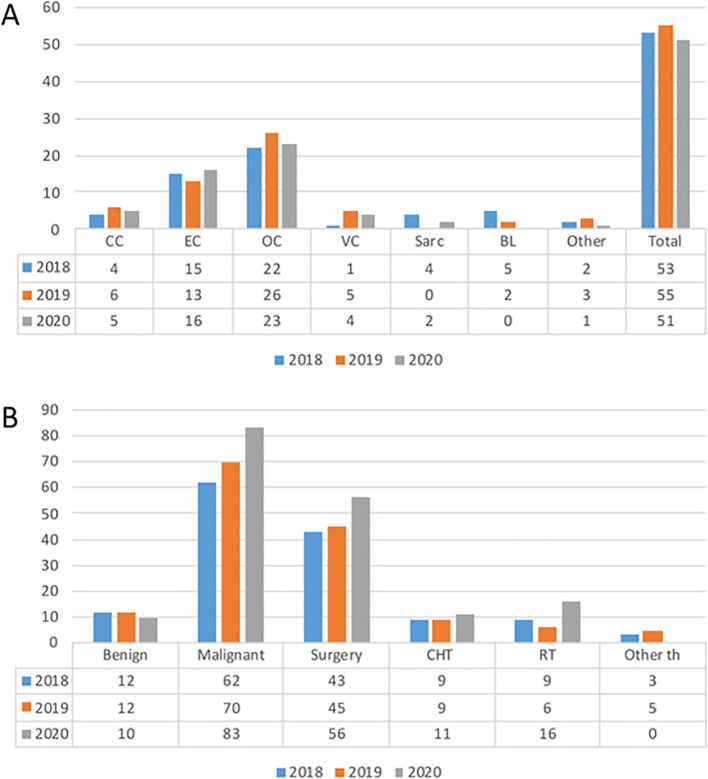
The comparison of outpatient and surgical activity at our gynaecological oncology unit did not show differences in terms of number and type of treated tumours compared to the same periods of the two previous years (Fig. 3A and 3B).
Fig. 3.
Oncological activity of the Gynaecologic Oncolgy Unit from March 9th to May 4th in 2018, 2019, 2020.Legend: CC: cervical cancer, EC: endometrial cancer, OC:ovarian cancer, VC: vulvar cancer, Sarc: sarcomas, CHT: chemotherapy, RT: radiotherapy, th: therapies.
4. Discussion
Our study represents a practical application of how the reallocation of resources in a COVID-19 free OSH can provide a correct application of surgical-oncological protocols without resorting, if not marginally, to alternative treatments entrusted to medical and radiation oncologists even in a pandemic period. To our knowledge, this is the first report on the results of this type of reorganization tested in one of the Italian regions most affected by COVID-19.
Between March and April 2020, the pandemic spread increased exponentially and no clear references on how to manage COVID-19 and non-COVID-19 patients were available. The few indications from international societies advised to postpone or cancel surgical interventions and to refer cancer patients to alternative (mainly neoadjuvant) therapies. Three main problems were related to surgical activity during this pandemic period. The first concerned the higher mortality risk, up to 39%, in cancer patients compared to the general population (2.3%) [10]. The second was the exhaustion of resources due to COVID-19 patients care, while the third was the risk of infecting patients during hospitalization [26]. The above-mentioned recommendations are based on logical rational bases. However, they were mainly based on expert opinions and not confirmed by clinical trials. Moreover, they posed two challenges: first, are the same survival rates guaranteed to patients? Second, how long would the pandemic last? In fact, at the time of the pandemic outbreak, nobody could have predicted its duration, particularly considering the progressively worsening trend of the infections. Considering these risks, we were apprehensive that full adherence to these recommendations could have had negative effects in terms of worsening patient's outcome, especially in case of ovarian cancer. In particular, our opinion was that in a period of potentially long-lasting outbreak pandemic the access to surgery should have been guaranteed to all oncologic patients. The possibility to refer cancer patients to a COVID-19 free OSH was a choice of our regional health authorities. Given this opportunity, our decision was not to establish priority categories among cancer patients being particularly difficult to choose who to prioritize among oncologic subjects. However, we agreed that a reasonable delay in the management of particularly low-risk neoplasms (initial stage of low-grade or borderline tumours) may only marginally influence both probability of cure and quality of life. Therefore, surgical procedures were offered based on booking priority and organization of the operating room. This strategy allowed us to keep our activity at a similar pace to the pre-COVID period despite an expected reduction of the number of patients referred to our department due to fear of infection in health facilities and to interruption of screening. In fact, comparing our surgical and outpatient activities with the same period of the two previous years, we did not find any difference. These findings, together with the results of the questionnaires, suggest that oncologic patients were more worried about cancer than about the risk of COVID-19 infection. Since the questionnaires were anonymous, we could not evaluate any variation among different tumours.
Our surgical activity maintained the quality standards required by guidelines also for ovarian cancer which represents the setting with the most complex surgery [27]. The proportion of primary debulking surgery was 67%, with absence of residual disease in 70% of cases achieved with medium-high surgical complexity in half of the cases (52%). In endometrial tumours, recent surgical innovations were guaranteed such as the sentinel node procedure [28,29] and the immunohistochemical analyses on the surgical specimen for microsatellite instability. All genetic analyses performed at the University Hospital Units were maintained, such as the genetic analysis pathways for BRCA and Lynch syndrome. Moreover, the multidisciplinary team continued its consultancy activity, mainly via web, with weekly sessions.
We did not have to manage infected patients either before or after surgery. In the first case, even if at the University Hospital there were operating rooms dedicated to COVID-19 patients, we would have probably shifted patients to radiotherapy or chemotherapy, because of the highest risk of death. The absence of post-operative COVID-19 infection suggests the good performance of our path. Moreover, it is possible that patient awareness about the risk of infection was important in managing our specific situation. In fact, the consciousness of the risks associated with COVID-19 favoured the acceptance of an isolation lifestyle including the absence of relatives during the hospitalization.
One of the limitations of the study is the lack of a comparison group from other institutions using different strategies in the same setting. Obviously, this does not allow to evaluate possible differences in terms of impact on quality of life and survival.
5. Conclusions
In epidemic conditions, most of the resources must be used to deal with the emergency, however, without neglecting other diseases requiring timely management. Our analysis suggests that relocating oncological surgery in COVID-19 free hubs, may be an appropriate strategy. This, in turn, once the pandemic subsides, could allow healthcare professionals to add to the count of “direct” deaths from COVID-19 also “indirect” deaths caused by lack of resources for the treatment of other fatal diseases.
: S1. North of Italy regions. The red outlined areas represent the “red zones” for COVID-19 infection. The red dot represents the town of Medicina near Bologna.
S2. Resource allocation during outbreak pandemic.
Legend: Dark blue represents the resources remained at University hospital, light blue the resources allocated at COVID-19 free surgical Hub. Class A, B, C represent the classification of the pathologies based on the time of expected treatment. The black arrows represent the type of interaction between the units, sections and wards.
S3. Questionnaire of risk of infection assessment (region of residence, presence of suspected flu symptoms and any risk of contact with COVID-19 positive subjects) in Italian and translated in English.
S4. Questionnaire filled by patients admitted to COVID-19 free oncologic surgical Hub, Italian version and translated in English.
Authors contribution
Conceptualization, A.M.P. P.D.I.; investigation, G.D., S.G., E.D.C., S.B., M.T R.D.A A.D.L., C.Z. and A.D.P.; formal analysis, G.D. and E.D.C; data curation AMP and G.D.,; writing—original draft preparation, A.M.P., A.D.P, P.D.I.; supervision, A.G.M. and P.D.I. All authors have read and agreed to the published version of the manuscript.
Declaration of Competing Interest
Authors declared no conflict of interest.
Acknowledgements
The authors are grateful to the Regional Health System, in particular to Chiara Gibertoni, MD, General Director of the University Hospital for the reorganization of health facilities and surgical paths during the emergency period for COVID-19 infection.
References
- 1.Guan W., Ni Z., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perrone A.M., De Palma A., De Iaco P. COVID-19 global pandemic: options for management of gynecologic cancers. The experience in surgical management of ovarian cancer in the second highest affected Italian region. Int. J. Gynecol. Cancer. 2020;30:902. doi: 10.1136/ijgc-2020-001489. [DOI] [PubMed] [Google Scholar]
- 3.Denys A., Chevallier P., Digklia A., et al. Interventional oncology at the time of COVID-19 pandemic: problems and solutions. Diagn. Intervent. Imag. 2020;101:347–353. doi: 10.1016/j.diii.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brethauer S.A., Poulose B.K., Needleman B.J., et al. Redesigning a Department of Surgery during the COVID-19 Pandemic. J. Gastrointest. Surg. 2020 doi: 10.1007/s11605-020-04608-4. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramirez P.T., Chiva L., Eriksson A.G.Z., et al. COVID-19 Global Pandemic: Options for Management of Gynecologic Cancers. Int J Gynecol Cancer. 2020 doi: 10.1136/ijgc-2020-001419. ijgc–2020–001419. [DOI] [PubMed] [Google Scholar]
- 6.Akladios C., Azais H., Ballester M., et al. Recommendations for the surgical management of gynecological cancers during the COVID-19 pandemic - FRANCOGYN group for the CNGOF. J. Gynecol. Obstetrics Human Reprod. 2020;49:101729. doi: 10.1016/j.jogoh.2020.101729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID 19: Elective Case Triage Guidelines for Surgical . 2020. Care. COVID-19 Guidelines for Triage of Cancer Surgery Patients. [Google Scholar]
- 8.Specialty guides for patient management during the coronavirus pandemic Clinical guide to surgical prioritisation during the coronavirus pandemic. Specialty guides for patient management during the coronavirus pandemic Clinical guide to surgical prioritisation during the coronavirus pandemic. 2020. [Google Scholar]
- 9.Cortiula F., Pettke A., Bartoletti M., et al. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann. Oncol. 2020;31:553–555. doi: 10.1016/j.annonc.2020.03.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Assaad S., Avrillon V., Fournier M.-L., et al. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur. J. Cancer. 2020 doi: 10.1016/j.ejca.2020.05.028. S0959804920303142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020 doi: 10.1136/bmj.m1106. m1106. [DOI] [PubMed] [Google Scholar]
- 12.Colombo N., Sessa C., du Bois A., et al. ESMO–ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease††These consensus statements were developed by the European Society for Medical Oncology (ESMO) and the European Society of Gynaecological Oncology (ESGO) and are published jointly in the Annals of Oncology and the International Journal of Gynecological Cancer. The two societies nominated participants who attended the consensus conference and co-authored the final manuscript. Ann. Oncol. 2019;30 doi: 10.1093/annonc/mdz062. 672–705. [DOI] [Google Scholar]
- 13.Colombo N., Creutzberg C., Amant F., et al. ESMO-ESGO-ESTRO consensus conference on endometrial cancer: diagnosis, treatment and follow-up†. Ann. Oncol. 2016;27:16–41. doi: 10.1093/annonc/mdv484. [DOI] [PubMed] [Google Scholar]
- 14.Raymond E., Thieblemont C., Alran S., et al. Impact of the COVID-19 Outbreak on the Management of Patients with Cancer. Target. Oncol. 2020;15:249–259. doi: 10.1007/s11523-020-00721-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen W., Zheng R., Baade P.D., et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 16.Pezzulla D., Macchia G., Taccari F., et al. Radiotherapy in Southern Italy at the time of COVID-19: options for radiation oncology units. Int. J. Gynecol. Cancer. 2020 doi: 10.1136/ijgc-2020-001523. ijgc–2020–001523. [DOI] [PubMed] [Google Scholar]
- 17.Eisenhauer E.L., Chi D.S. Ovarian cancer surgery — heed this LION’s roar. N. Engl. J. Med. 2019;380:871–873. doi: 10.1056/NEJMe1900044. [DOI] [PubMed] [Google Scholar]
- 18.Cibula D., Pötter R., Planchamp F., et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients with Cervical Cancer. Virchows Arch. 2018;472:919–936. doi: 10.1007/s00428-018-2362-9. [DOI] [PubMed] [Google Scholar]
- 19.Oonk M.H.M., Planchamp F., Baldwin P., et al. European Society of Gynaecological Oncology Guidelines for the Management of Patients With Vulvar Cancer. Int. J. Gynecol. Cancer. 2017;27:832. doi: 10.1097/IGC.0000000000000975. [DOI] [PubMed] [Google Scholar]
- 20.Halkia E., Spiliotis J., Sugarbaker P. Diagnosis and management of peritoneal metastases from ovarian cancer. Gastroenterol. Res. Pract. 2012;2012:541842. doi: 10.1155/2012/541842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lampe B., Kroll N., Piso P., et al. Prognostic significance of Sugarbaker’s peritoneal cancer index for the operability of ovarian carcinoma. Int. J. Gynecol. Cancer. 2015;25:135. doi: 10.1097/IGC.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 22.Look M., Chang D., Sugarbaker P.H. Long-term results of cytoreductive surgery for advanced and recurrent epithelial ovarian cancers and papillary serous carcinoma of the peritoneum. Int. J. Gynecol. Cancer. 2004;14:35. doi: 10.1136/ijgc-00009577-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Bodea R., Hajjar N.A., Bartos A., et al. Evaluation of P-POSSUM Risk Scoring System in Prediction of Morbidity and Mortality after Pancreaticoduodenectomy. chr. 2018;113:399. doi: 10.21614/chirurgia.113.3.399. [DOI] [PubMed] [Google Scholar]
- 24.Rapsang A.G., Shyam D.C. Scoring systems in the intensive care unit: a compendium. Indian J Crit Care Med. 2014;18:220–228. doi: 10.4103/0972-5229.130573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clavien P.A., Sanabria J.R., Strasberg S.M. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 26.Dexter F., Parra M.C., Brown J.R., et al. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth. Analg. 2020;131:37–42. doi: 10.1213/ANE.0000000000004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fagotti A., Ferrandina G., Vizzielli G., et al. Phase III randomised clinical trial comparing primary surgery versus neoadjuvant chemotherapy in advanced epithelial ovarian cancer with high tumour load (SCORPION trial): final analysis of peri-operative outcome. Eur. J. Cancer. 2016;59:22–33. doi: 10.1016/j.ejca.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 28.Perrone A.M., Di Marcoberardino B., Rossi M., et al. Laparoscopic versus laparotomic approach to endometrial cancer. Eur. J. Gynaecol. Oncol. 2012;33:376–381. [PubMed] [Google Scholar]
- 29.Perrone A.M., Casadio P., Formelli G., et al. Cervical and hysteroscopic injection for identification of sentinel lymph node in endometrial cancer. Gynecol. Oncol. 2008;111:62–67. doi: 10.1016/j.ygyno.2008.05.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
: S1. North of Italy regions. The red outlined areas represent the “red zones” for COVID-19 infection. The red dot represents the town of Medicina near Bologna.
S2. Resource allocation during outbreak pandemic.
Legend: Dark blue represents the resources remained at University hospital, light blue the resources allocated at COVID-19 free surgical Hub. Class A, B, C represent the classification of the pathologies based on the time of expected treatment. The black arrows represent the type of interaction between the units, sections and wards.
S3. Questionnaire of risk of infection assessment (region of residence, presence of suspected flu symptoms and any risk of contact with COVID-19 positive subjects) in Italian and translated in English.
S4. Questionnaire filled by patients admitted to COVID-19 free oncologic surgical Hub, Italian version and translated in English.