Highlights
-
•
‘The Mask’ is the current byword and a precious possession.
-
•
For healthcare workers, wearing mask is a necessity for personal protection.
-
•
For general public, the mask is perhaps the most-powerful psychological symbol.
-
•
The mask undermines all other recommended practices of infection control measures.
-
•
We present evolution, types, filtration efficiency and recommended uses of mask.
Keywords: Face mask, Personal protection equipment, Filtration efficiency, Reusability, Covid-19, Infection control
Abstract
‘The Mask’ has become a byword and a precious possession universally. Except for its use by the medical fraternity, answers to the common questions-whether it provides enough protection, which type is optimal for the general public and who really needs to don it, remain poorly understood. For a frontline healthcare worker, wearing mask is a necessity as an important person protection equipment, it is perhaps the most-powerful psychological symbol for the general public. Surprisingly, it even undermines all other recommended practices of infection control and breaking the transmission chain of Covid-19, like hand washing, personal hygiene and social distancing. ‘The mask’ has evolved with time and yet there is a need to further improve the design for safety, tolerability and comfort. In this review we present the journey of face mask, originating from the first masks aimed at stopping the bad smell to its industrial use to its all-important place in the medical field. Various types of face masks, their filtration efficiency, reusability and current recommendations for their use are presented.
1. Introduction
The Mask : You were good, kid, real good. But as long as I’m around, you’ll always be second best, see? As Stanley Ipkiss, the eponymous character in the movie “The Mask” remarked: “It (The Mask) is a power tie. It's supposed to make you feel powerful.” This movie dialogue perfectly suits the ‘center stage’ taken by the face masks during the current Covid-19 pandemic. Globally, emotions fly high and heated debates are omnipresent as ‘Mask’ becomes a byword and precious possession. Answers to the common questions-whether it provides enough protection, which type is optimal for the general public and who really needs to don it, remain barely convincing. Controversies are aplenty, exacerbated further by its acute shortage, inflated prices and hoarding for profiteering by some.
For a frontline healthcare worker, wearing mask is a necessity as it empowers him to fight the deadly Covid-19 with less fear and anxiety of contracting the illness. However, for the common man, ‘the mask’ is at present, perhaps, the most-powerful psychological symbol. Surprisingly, it even undermines all other recommended practices of infection control for breaking the transmission chain of Covid-19, like hand washing, personal hygiene and social distancing.
This review describes the evolution of mask, its types and who should wear which mask during the current COVID-19 outbreak.
2. The journey of mask
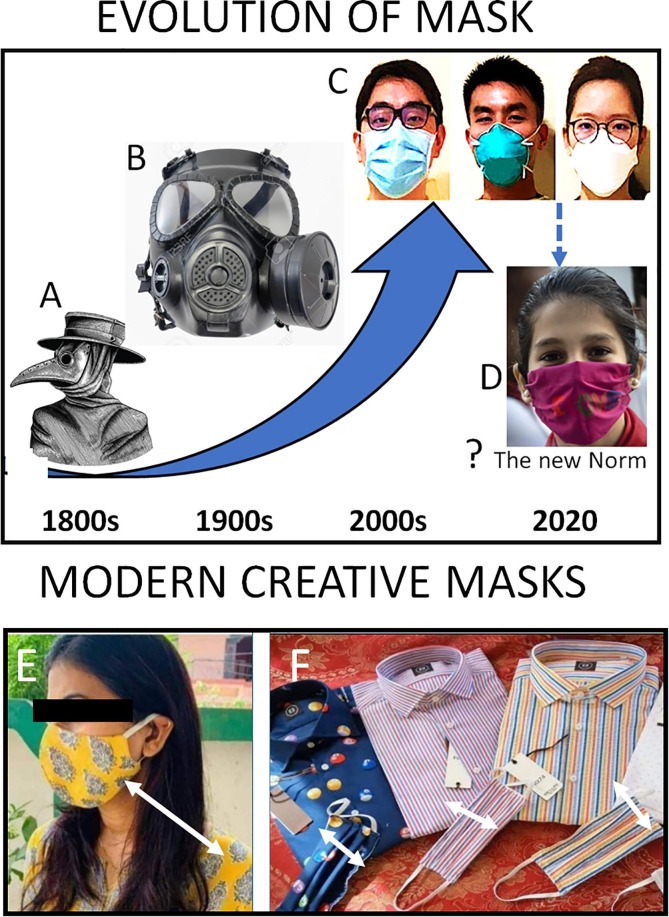
The first mask was aimed at stopping a bad smell. Only in the 1700s, mankind realized its need for medical purposes. Prevailing orthodox belief in that era was dominated by the “miasmatic” theory of disease causation, which postulated that most diseases were caused by inhaling a “miasma” - air infected through exposure to corrupting matter like corpses and exhalations of infected persons (Halliday, 2001). This popularized the notorious ‘plague doctor’ masks described by Charles de Lorme, a European physician. This mask was filled with herbal perfume, shaped like a beak, had a half-foot long nose with two holes near the nostrils, permitting sufficient breathing (Fig. 1 ).
Fig. 1.
Evolution of ‘The Mask’. Starting from a beak-shaped plague mask in 1800s (A), it has evolved from a bulky industrial mask in 1900s (B) to the simple surgical mask and N-95 medical grade respirator (C). The current scarce availability of a surgical mask and N95 respirator has prompted the governments to recommend even face covers from any available cloth (D) material!
Further developments in the field of microbiology during 1800s debunked the miasmatic theory and ‘the mask’ underwent structural transformations to suit the healthcare needs. The first study supporting the use of a mask in surgery was described in 1897 by J Miculicz, a German physician. Later in 1918, GH Weaver, a Chicago based physician, described the practice of wearing gauze masks while working with patients suffering from diphtheria, meningitis and pneumonia (Belkin, 1997).
The second phase of the industrial revolution and the threat posed by chemical warfare established the importance of ‘the mask’ and prompted rapid advances in its design. One triggering historical event was America’s industrial disaster during the construction of Hawks Nest Tunnel in 1930s, when approximately 1000 people working underground succumbed to silicosis due to the lack of suitable protective equipment. Health risks associated with asbestos inhalation were also realized among the manufacturing workers for pipes in naval vessels. Furthermore, the high risk of inhalation of toxic dust was identified among workers deployed to mining and construction industries, which led to the recommendation to use mask respirators at the workplace.
A large variety of face masks have surfaced in the market during the current COVID-19 outbreak, largely due to the limited availability of proper face masks.
3. Types of masks
3.1. Respirator mask
A respirator mask forms a tight seal around nose and mouth and protects the user from being exposed to noxious particles, gases and microorganisms including bacteria, viruses and fungi. The filter is made up of millions of microfibers of polypropylene layers that are electrostatically charged. The electrical charge retains its ability to filter microorganisms.
Initial respirator masks were made up of fibre glass and prevented fine coal dust inhalation. However, the users found it difficult to breathe through them. The first single use N95 respirator mask was introduced in 1972 by 3M. It used very thin layers of fibres by air-blasting melted polymer with added electrostatic charge to block very small particles, making it easier to breathe through. Its first medical use came in 1990s when doctors and nurses used it to protect themselves from drug resistant mycobacteria from human immune deficiency virus (HIV)-infected patients. It was subsequently used during the SARS outbreak in 2003.
Respirator masks are certified as N, R or P depending on their ability to offer
resistance to oil-based particles. ‘N’ stands for ‘not oil resistant’ and these masks can only be used for filtering particles that do not contain oil. ‘R’ and ‘P’ labelled masks are ‘somewhat resistant to oil’ and ‘strongly oil proof’, respectively.
‘N’ type respirator masks are further divided into N95, N99, N100 depending on the filtration efficacy. N95 and N99 respirator masks filter off at least 95% and 99%, respectively of the particles >0.3 µm. The 0.3 μm cut off is preferred because particles ≥0.3 µm are able to penetrate into the lung tissue. Although, coronaviruses measure 0.06–0.14 µm in diameter, their small size renders them the random Brownian motion, making them more prone for trapping by the respirator filter. Therefore, N95 respirator masks effectively filter the coronavirus effectively, provided the mask has a proper seal. A fit test is therefore necessary before donning these masks.
Each country has their own certification standard for each mask type, e.g. USA [NIOSH 42CFR Part 84], Europe [149:2001, China [GB2626]. The European Union classifies respirator masks into FFP1, FFP 2 and FFP3 where FFP stands for Filtering Face Piece. N95 is roughly equivalent to FFP2 and N99 is roughly equivalent to FFP3 masks. FFP1, FFP2 and FFP3 are also called P1, P2 and P3.
3.2. Valve versus non-valve N95 respirators
N95 respirator masks are available with a valve and without a valve. The valve N95 mask respiratory are not suitable for patients suffering with COVID-19 as during exhalation they will allow the virus to pass out easily and can potentially infect people around them.
3.3. Surgical mask
The Surgical mask is also called a ‘procedural’ or ‘medical’ mask. It was initially introduced in the 1890s for surgeons and assistants for use in the operation theatres. It was supposed to protect the surgical team from blood and body fluid splashes from the patients. It did not protect them from catching infection from the patients. On the contrary, patients undergoing operations were protected if a member of the surgical team coughed or sneezed during the surgery.
The surgical mask has three layers (3-ply). The material of the innermost layer absorbs moisture from the users’ breath, the middle melt-blown material layer acts as a filter while the outer layer repels water and other liquids. However, despite the hydrophobic nature of external layer, water droplets containing dangerous viruses can remain on it (Shen and Leonas, 2005).
The pleats on the mask increase the surface area for adequate covering of nose and mouth. Although, the surgical mask can filter the bacteria and other particles (>0.1 µm in size) with >98% efficiency, the seal around nose and mouth is not tight. Therefore, a surgical mask provides very little protection from infections. Its works efficiently for 3 to 8 h, depending on the environmental humidity and temperature. It should be disposed safely after a single use.
3.4. Dust mask
A dust mask is a moulded disposable mask made of paper pad. While it protects against non-toxic dusts during dusty house cleaning and construction works, it provides no protection against microbes.
4. Single layer face mask
Many governments have come out with varying guidelines on covering the mouth and nose with single layer face masks made up of a single layer of non-woven fabric. Such masks are commonly used by workers in the food processing industry. Such masks are only for single use, never washed or reused and provide no protection against microbes.
Indigenous masks have appeared in general public, made up of several common fabrics including cotton, silk, chiffon, flannel, various synthetics, and their combinations. Although the filtration efficiencies for various fabrics with a single layer ranged from 5 to 80% for particle sizes of >300 nm, the efficiencies improved when multiple layers were used with combination of fabrics. Cotton, the most widely used material for cloth masks performs better only at a high thread count (Konda et al., 2020). A recent randomized trial compared the cloth masks with surgical masks and reported Penetration of cloth masks by particles was almost 97% and medical masks 44% (MacIntyre et al., 2015).
5. Extended use and re-use of N95 respirator masks
Frontline healthcare workers are at highest risk of contracting the COVID-19 infection from their patients. However, the optimal N95 respirator masks are having acute shortage in various parts of the world, prompting evaluation for their extended and repeated use. It is important to note that the medical grade N95 respiratory masks are only for single use. Although, other masks, considered equivalent to the medical grade N95 respirator masks (FFP2, N99, N100 or FFP3) may filter out the dreaded coronavirus effectively, they are very uncomfortable when worn over longer periods, especially due to the difficulty of breathing through them.
Owing to the acute short supply, experiments have explored different ways of extending the use of N95 respirator masks as well as reusing them. The most import consideration is that such attempts should not compromise the protection offered by these respirator masks. During the extended use, the mask must maintain its shape and filtration efficiency. The method of sterilization must eliminate the virus threat and it should be used by the same wearer. However, when these respirator masks are used repeatedly or for longer periods, their filters may clog and make breathing through them difficult.
If for some unavoidable reasons, the N95 respirator mask is to be reused, utmost care is needed for its sterilisation. Simple drying in air for 48–72 h is the simplest way sterilising and reusing it since this method mask kills the virus. Heating the mask in an oven at 70 degrees Celsius for 30 min also kills the virus. However, it should not contain a metal and the mask should not contain an inflammable material. The mask can be hung in the oven by using a wooden clip (Kate, 2020). Alternatively, the N95 respirator mask can also be sterilised in a dry rice cooker for 3 min at 149–164 degrees Celsius (Lin et al., 2017). Importantly, the N95 respirator mask should not be washed with soap, warm water, alcohol or bleach. Even exposure to ultraviolet radiation or using a microwave oven is not advisable since these methods damage the electrostatic charge and significantly reduce the filtration capacity (Viscusi et al., 2009).
5.1. Wearing a mask to prevent COVID-19 transmission
COVID-19 is released from a patient’s body during talking, coughing, sneezing or even breathing as aerosol droplets. Airborne transmission has not been proven as the mode of transmission (Ong et al., 2020). Therefore, minimising the spread of the virus from man-to-man is the only effective way of controlling the current pandemic. Accordingly, the World Health Organization (WHO) and local governments have been advising social distancing, staying indoors, regular hand washing with water and using an alcohol based disinfectant. Historically, during the Severe Acute Respiratory Syndrome (SARS) virus outbreak, the human-to-human transmission could be reduced by 55% by hand washing alone, 68% by wearing a face mask alone while the their combined used (with gloves and a protective gear) reduced it by 91% (Jefferson et al., 2009).
The face mask appears to be an effective method of preventing the aerosol spread of COVID-19. However, the directives from various health agencies and governments regarding wearing of a face mask have been inconsistent. Initially, the WHO and Centre for Disease Control (CDC) in United States advised that mask is not needed for everybody and only people caring for a proven or suspected COVID-19 patient or a person with respiratory symptoms should wear a mask. This advisory was largely driven by the severely short supply of face masks, sparing them for frontline healthcare workers and preventing panic among the general public. Furthermore, the lack of evidence for the effectiveness of face mask against the current COVID-19 outbreak is not a reasonable explanation considering its high infection transmission rates (Leung et al., 2020).
Recent studies suggest asymptomatic transmission in the community. Moreover, an infected patient can shed the viral aerosol droplets even 2–3 days prior to developing symptoms (Ganyani et al., 2020). An interesting risk assessment model for an influenza epidemic demonstrated that around 35% of the people will catch the influenza infection if people do not wear a mask. However, wearing a mask by 50% of the general public will reduce the prevalence of infection by 50% while an 80% use of mask in the community may will make the risk of transmission negligible (Yan et al., 2019). This phenomenon has been seen in countries with a culture of wearing masks routinely, such as Hong Kong, South Korea and Taiwan, where the COVID-19 outbreak could be contained rapidly and effectively.
6. Recommended face masks for the community and healthcare workers
Wearing any mask is better than wearing no mask, both in terms of transmission and protection. This information led to a panic buying spree by general public. The acute severe shortage led to the resurgence of fake surgical and N95 respirator masks in the global markets at unbelievable prices. It even led some governments to even issue advisories on home-made cotton cloth masks, which could be washed and reused (Masks for curbing the spread of SARS-Cov-2 Coronavirus, 2020). Whether a simple cloth mask is sufficient for everybody while going outdoors in the community is debatable. The N95 respirator mask is not recommended for community use.
Surgical masks are recommended by all healthcare workers while dealing with non-COVID-19 patients. They should be used by healthcare workers deployed in high-risk hospital areas where COVID-19 patients are housed. Use of N95 respirator masks prevent frontline healthcare workers from contracting the infection from their patients (Wang et al., 2020). This is supported by the previous experiences from SARS and MERS outbreaks (Greenhalgh et al., 2020). A Cochrane review suggested that donning the N95 respirator reduces the spread of respiratory viruses (Institute, 2019). The need for a face mask has never been more critical than during the ongoing Covid-19 pandemic (Jefferson et al., 2011).
The mask design and safety have evolved over time and it remains the mainstay of the personal protective gear of a physician warrior. However, besides the current supply issues, there remains several challenges and limitations with regards to its design. Although N95 grade respirators provide excellent protection to the user, the existing designs have inherent tolerability issues. While the metal strip compresses the bony nose bridge, the tight thin straps compress various superficial sensory nerves on the scalp, causing de novo headaches or worsening the pre-existing headaches, especially when worn >4-hours at a time (Ong et al., 2020). The discomfort limits users’ compliance while frequent readjustments by the user jeopardize his own safety. Definitely, healthcare workers deserve comfortable respirators!
7. Is mask a psychological symbol for general public?
For general public, hand hygiene is a more effective strategy for preventing COVID-19 infection than donning a face mask. The general public launched huge ‘Google search’ for satisfying their curiosities even when sufficient information was provided by various government bodies. The search results for “face mask” outnumbered “washing hands”. We agree that the scarce availability of face masks might have prompted the general public to search for possible avenues of procuring them. This happened despite repeated announcement by the government health agencies that mask wearing was not necessary for the general public (National Health Service, 2020, Federal Ministry of Health, 2020).
Initially, it was a reasonable advice to the vulnerable individuals in general public to avoid crowded areas and any face masks, especially when exposed to high-risk areas. Once it was reported that COVID-19 could be transmitted even before the symptom-onset, it was advocated that community transmission might be reduced if everyone wears a mask (Zou et al., 2020). Although, there is no scientific evidence, it sounds logical to cover the mouth and nose to reduce respiratory droplet transmission (Xiao et al., 2020). Members from the general public, especially some from the younger generation had initial resentment for covering the face. However, once it became and advisory from government bodies, this generation came out with many creative ideas for face cover, giving it a fashion sense (Fig. 1). Such masks do not have the infection control value but provide the user a psychological pseudo-confidence. However, these creative mask designs certainly have the potential to become a status symbol!
In past, some sick people (especially those of chemotherapy and immunosuppression) were advised to wear a face mask for preventing infections. Also, many people in some Asian countries (Japan and Korea) used to wear a face mask as a hygienic practice Asian countries). However, this practice has induced stigmatisation and occasional racial aggravations during the current pandemic. While WHO has not recommended mass masking, we strongly feel that the universal use of face masks may prevent discrimination of individuals of certain ethnicity or facial features. We again reiterate that frequent hand-washing and social distancing are still the most potent infection control methods for general public. Mask wearing could create a false sense of security among some individuals, especially those who ignore social distancing and hand-washing. Public health education needs to emphasise these aspects to ensure a victory over the Covid-19 pandemic. The common surgical face mask worn by a Covid-19 patient prevent other people who come in his close contact. Thus, the universal use of masks in the community will be effective in reducing the infection spread in the community. Currently, amid lock-downs of various intensities, mass masking is certainly important for essential workers who cannot stay at home. As people return to work, some people with active infection would start roaming in the community. Mass masking would then become more important to reduce the transmission of infection and prevent the so-called ‘second-wave’.
Any kind of mask that covers the nose and face is being increasingly recommended for general public during the current Covid-19 pandemic, leading to the sudden arrival of multi-colored and fashionable designs of face covers-which is perhaps the NEW NORMAL!. If Covid-19 pandemic lasts longer, the United Nations may even deem access to ‘the mask’ a universal fundamental human right. For the time-being, let’s call 2020 as the “Year of The Mask”.
Funding source
None.
CRediT authorship contribution statement
Yihui Goh: Writing - original draft. Benjamin Y.Q. Tan: Writing - review & editing. Chandra Bhartendu: Conceptualization, Writing - review & editing. Jonathan J.Y. Ong: Conceptualization, Writing - review & editing. Vijay K. Sharma: Conceptualization, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Drs. Jing Mingxue, Lim Wei Yang, Tan Yi Lin and Kenneth Sooi for assisting with the photography of present-day mask use.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.05.060.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Belkin N.L. The evolution of the surgical mask: filtering efficiency versus effectiveness. Infect. Control Hosp. Epidemiol. 1997;18:49–57. doi: 10.2307/30141964. [DOI] [PubMed] [Google Scholar]
- Federal Ministry of Health, Germany, 2020. Daily updates on the coronavirus: is wearing a surgical mask, as protection against acute respiratory infections, useful for members of the general public?. https://www.bundesgesundheitsministerium.de/en/press/2020/coronavirus.html (accessed March 5, 2020).
- Ganyani T., Kremer C., Chen D. Estimating the generation interval for coronavirus disease (COVID-19) based on symptom onset data, March 2020. Eur. Surveill. 2020;25:2000257. doi: 10.2807/1560-7917.ES.2020.25.17.2000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, T., Chan, X., Khunti, K., et al., 2020. What is the efficacy of standard face masks compared to respirator masks in preventing COVID-19 type respiratory illness in primary care staff? Centre for Evidence Based Medicine. 24th March 2020; Ahead of Print.
- Halliday S. Death and miasma in Victorian London: an obstinate belief. BMJ. 2001;323:1469–1471. doi: 10.1136/bmj.323.7327.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T., Del Mar C., Dooley L. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009;339:b3675. doi: 10.1136/bmj.b3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T., Del Mar C.B., Dooley L. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2011;2011(7):CD006207. doi: 10.1002/14651858.CD006207.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kate, S., 2020. Stanford researchers develop potential method to reuse N95 respirators. Heat disinfection could be conducted in an oven. 31st March 2020. https://www.stanforddaily.com/2020/03/31/stanford-researchers-developpotential-method-to-reuse-n95-respirators/. Accessed on 4th April 2020.
- Konda, A., Prakash, A., Moss, G.A., Schmoldt, M., Grant, G.D., Guha, S., 2020. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks [published online ahead of print, 2020 Apr 24]. ACS Nano. 2020;acsnano.0c03252. doi:10.1021/acsnano.0c03252. [DOI] [PubMed]
- Leung C.C., Lam T.H., Cheng K.K. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020;395:945. doi: 10.1016/S0140-6736(20)30520-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin T.H., Chen C.C., Huang S.H., Kuo C.W., Lai C.Y., Lin W.Y. Filter quality of electret masks in filtering 14.6-594 nm aerosol particles: effects of five decontamination methods. PLoS One. 2017;12:e0186217. doi: 10.1371/journal.pone.0186217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Seale H., Dung T.C. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5:e006577. doi: 10.1136/bmjopen-2014-006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masks for curbing the spread of SARS-Cov-2 Coronavirus. A manual on homemade masks. http://164.100.117.97/WriteReadData/userfiles/FINAL%20MASK%20MANUAL.pdf Accessed on May 17, 2020.
- National Health Service, 2020. Are face masks useful for preventing coronavirus?. https://www.nhs.uk/conditions/coronavirus-covid-19/commonquestions/ (accessed March 5, 2020).
- National Institute for Occupational Safety and Health, 2020. 100 Years of Respiratory Protection History. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/niosh/npptl/Respiratory-Protection-history.html. Accessed 6 April, 2020.
- Ong J.J.Y., Bharatendu C., Goh Y. Headaches associated with personal protective equipment - a cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60:864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- Ong Sean Wei Xiang, Tan Yian Kim, Chia Po Ying, Lee Tau Hong, Ng Oon Tek, Wong Michelle Su Yen, Marimuthu Kalisvar. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H., Leonas K. Study of repellent finish of filtration ability of surgical face masks. Int. Nonwovens J. 2005;14:17–26. [Google Scholar]
- Viscusi D.J., Bergman M.S., Eimer B.C., Shaffer R.E. Evaluation of five decontamination methods for filtering facepiece respirators. Ann. Occup. Hyg. 2009;53:815–827. doi: 10.1093/annhyg/mep070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 2020;105:100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao J., Shiu E.Y.C., Gao H. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-personal protective and environmental measures. Emerg. Infect. Dis. 2020;26:967–975. doi: 10.3201/eid2605.190994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J., Guha S., Hariharan P., Myers M. Modeling the effectiveness of respiratory protective devices in reducing influenza outbreak. Risk Anal. 2019;39:647–661. doi: 10.1111/risa.13181. [DOI] [PubMed] [Google Scholar]
- Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.