Abstract
Objectives:
Genomic information will increasingly be used to aid in the prevention, diagnosis, and treatment of disease. Several national initiatives are paving the way for this new reality, while also promoting new models of participant-engaged research. We compare the opinions of research participants in a cancer registry, human genetic researchers, and institutional review board (IRB) professionals about the return of individual-level genetic results (ROR).
Methods:
Online surveys were administered to participants in a cancer registry (n = 450) and overlapping questions were compared to our previous online national surveys of human genetic researchers (n = 351) and IRB professionals (n = 208).
Results:
The majority of respondents agreed that researchers have an obligation to return individual results when they would affect a participant’s health. While 77% of registry participants favored ROR if the researcher feels the participant might be interested in the results, only 30% of the IRB professionals and 25% of the genetic researchers agreed with this statement.
Conclusions:
Significant differences emerged between the stakeholder groups in several ROR scenarios. Policies that are acceptable to participants, researchers and IRBs, and that ensure human subject protections and facilitate research are needed.
Keywords: Return of results, Genomics, Cancer, Research participant perspective, Precision medicine
Introduction
The ambitious goals of the All of Us Research Program, which is a key element of the Precision Medicine Initiative, and the parallel Cancer Moonshot Initiative (CMI) are to improve human health by tailoring medical treatment to the individual characteristics of each patient. The vision of both programs is to use an array of information to identify an individual’s susceptibility to a particular disease, such as cancer, and their response to a specific treatment [1, 2]. Genomic information is the foundation that will drive discoveries critical for the success of both of these national programs.
Genomic research has raised a number of ethical, legal and social issues, including: (1) confidentiality of information exchanged within a study; (2) potential for participant identification; (3) returning results gathered as research data to participants; (4) reconsent of existing participants into a different part of a study; and (5) data sharing processes and implications between researchers and institutions. The All of Us Research Program and parallel CMI will again require us to consider these issues, but on a much larger scale. The All of Us Research Program is also encouraging a new paradigm where participants will have greater control over their information, and the ability to determine what results they wish to receive [2–4], presumably including genomic results. While access to results has not been stated as an explicit requirement of the CMI, it is reasonable to assume it will also be encouraged under this initiative. Historically, the opinions of institutional review board (IRB) leaders and researchers have had a strong influence on these issues, including shaping policy on return of research results (ROR). However, there has not been a direct comparison of the views of these groups with those of research participants.
Our initial work measured the opinions and practices of human genetic researchers and IRB leaders regarding ROR, reconsent, data sharing, identifiability, and potential for harm [5] in the context of genomic research. The Genetics Research Review Issues Project (GRRIP), which queried both IRB professionals and genetic researchers using qualitative and quantitative methods, discovered that these groups did not agree with each other on many of these issues, including ROR, likelihood of identification from coded genomic data, and potential for harm if identified [5]. There was also a lack of consensus within the groups on a number of issues, including several scenarios around ROR [5–9]. These findings are consistent with previous results, including studies showing that although most researchers would return a clinically significant result, there was no consensus as to what constituted an appropriate threshold [10–12].
To date, arguably the most important views on these issues have not been collected in a way that allows direct comparisons with these other stakeholder groups. As we embark on large national research initiatives where participants will have greater access to their data and results, it is important to consider their views about and expectations of these issues. Currently, we do not know whether the views of research participants differ from those of other stakeholder groups. Further, we do not know whether the views of research participants with cancer will differ from those of their relatives or those research participants without cancer.
We address this gap by providing data on the views of research participants enrolled in a cancer research registry, including people with cancer, their relatives, and noncancer controls recruited from the general population, regarding returning genetic results and compare their views to genetic researchers and IRB professionals from the GRRIP study that were asked the same questions. These findings can guide policies regarding ROR as we now embark on two major national initiatives that will need to enroll and engage large numbers of individuals, including those with and without cancer and their family members.
Methods
Eligibility and Recruitment for the Participant Issues and Expectations Project
Details on the Northwest Cancer Genetics Registry (NWCGR), the source of individuals for this study, have been described previously [13, 14]. Briefly, individuals who were enrolled in the NWCGR (n = 3,352) were the source of participants for the Participant Issues and Expectations Project (PIP), and included people with cancer recruited from Western Washington (n = 2,027), first-degree relatives of cases (n = 451), noncancer controls who were recruited from a random population sample from Western Washington (n = 527), and people who self-referred in response to community awareness efforts for the NWCGR and included both people with and without cancer (n = 904 total; 340 with cancer). Noncancer controls were recruited for the NWCGR from a random population from the same geographic area to compare with participants with cancer. Self-referrals with cancer are grouped with cases and those without are grouped with the controls. All were eligible to participate in the current project. As described previously, letters, including informed consent, were sent by US mail inviting individuals to take the online, confidential survey. Up to 3 invitations were sent to participants at approximately 2-week intervals [14]. Of the 450 participants that completed the online survey in 2013–2014, 228 were from the case group, 155 were from the control group, and 67 were relatives.
Survey Methods
The purpose of the survey was to document the range and frequency of occurrence of concerns and expectations regarding participating in human research studies, including genomic studies, and to compare these findings to our previous surveys of IRB professionals and genetic researchers from the GRRIP study that was conducted in 2009 [5, 6, 8]. Detailed methods for this study, including the survey instrument, have been published previously [14]. Briefly, the confidential, online survey instrument had a total of 22 questions, including overlapping questions from the GRRIP surveys and covering 6 general topic areas: decision to participate in research; relationship between researchers and participants; reconsent and broad consent; ROR; use and security of de-identified data; and family communication of health issues. Three questions regarding the return of individual results overlapped with our previous online surveys of IRB professionals and genomic researchers developed as part of the GRRIP. These questions asked whether researchers have an ethical obligation to return individual results to each person under 3 scenarios: (1) the results would affect a participant’s health or health care, (2) a participant asks for them, (3) the researcher feels that the participant might be interested in knowing about the results. The response categories for these 3 questions were 5-point Likert scales rating the level of agreement with the statement. The 5 categories were: strongly agree, somewhat agree, neither agree nor disagree, somewhat disagree, strongly disagree.
Details on the GRRIP study and the development of the surveys have been described previously [5, 6, 9]. Briefly, parallel online surveys were used to anonymously collect information from human genetic researchers (n = 351) and IRB professionals (n = 208) regarding their views about human participant oversight of genetic protocols, and participants were allowed to skip questions they did not wish to answer. The same 3 questions on ROR with exactly the same wording were included in both the human genetic researcher and IRB surveys. However, 2 additional response categories were allowed in the GRRIP: “don’t know” and “it depends.” Respondents who answered “don’t know” were excluded from the analysis to be consistent with the PIP study (n = 7 [q8.1], n = 2 [q8.2], and n = 4 [q8.3] for researchers and n = 8 [q8.1], n = 6 [q8.2], and n = 6 [q8.3] for IRB professionals). Those who indicated that “it depends” were grouped with the neither agree nor disagree (neutral) category.
All study procedures were approved by the University of Washington’s Human Subjects Division, as well as by the University of California, Irvine Institutional Review Board. All participants provided informed consent prior to participation and were free to skip any questions that they did not wish to answer.
Statistical Analysis
Responses to all questions were first summarized using frequency distributions separately for each group (PIP and the 2 GRRIP groups). Two hypotheses were generated based on our qualitative interview data and previous findings from the GRRIP and tested in this study: (1) there would be a range of expectations within PIP with regard to ROR and these would differ by age, gender, and status (case vs. relative vs. control) and (2) PIP participants would differ in their preferences for ROR from both researchers and IRBs. To address the second hypothesis, we compared overlapping questions that were asked in the same way from the 3 surveys. Response categories were collapsed into fewer categories for testing and to facilitate interpretation. For example, the 5 categories of the Likert scales were collapsed into 3, combining the “strongly” and “somewhat” categories (e.g., strongly agree, somewhat agree and strongly disagree, somewhat disagree). Hypothesis 1 was tested using ordinal logistic regression which allows for multiple categories of the outcome variable and adjustment for potential confounders. Participant type (case, control or relative) was the independent variable. Differences in frequency of responses between PIP and GRRIP groups (hypothesis 2) were also tested using ordinal logistic regression, with stakeholder group (participants, researchers or IRBs) as the independent variable. The response categories (dependent variable) were ordered and coded as follows for all models: agree and strongly agree as 0, neutral as 1, disagree and strongly disagree as 2. With ordinal logistic regression, several cumulative logits were modeled using all possible cut points of the dependent variable, but a single summary odds ratio (OR) and 95% confidence interval describing the relationship between the dependent and independent variable was obtained. With the coding as described above the ORs are interpreted as follows: an OR greater than 1 indicates that the comparison group was more likely to be neutral or disagree when compared to the reference group; similarly, an OR less than 1 indicates that the comparison group was more likely to agree with the statement than the reference group. Comparisons within the PIP sample between cases, controls, and relatives were adjusted for age, gender, and education. Because there were no differences by participant type within the PIP sample, all participants were combined when compared to the 2 GRRIP groups. Comparisons between PIP and the 2 GRRIP groups were adjusted for gender. Odds ratios are interpreted as described above. R version 3.2.2 with the MASS package was used for all analyses [15, 16]. A p value < 0.05 was considered statistically significant for all tests. Sample sizes varied by question since participants were allowed to skip any question they did not wish to answer.
Results
Demographics of the research participants, genetic researchers, and IRB professionals are summarized in Table 1. About half of the research participants were cases, one-third of them were controls, and the remainder were relatives. Their average age was 63.6 years and 94.7% were white and well educated, with over 60% having a college degree. Melanoma was the most frequent cancer type among cases (29.5%), followed by thyroid cancer (18.3%), and breast cancer (15.5%), reflecting the focus on these cancers in the NWCGR. Compared to genetic researchers, the IRB professionals were significantly more likely to be women (76 vs. 51.9%; p < 0.0001) and have worked previously as genetic researchers (42.8 vs. 26.8%; p < 0.0001), and less likely to have worked long term (> 5 years) in their respective area (56.7 vs. 82.3%; p < 0.0001).
Table 1.
Demographics of the research participants, genetic researchers, and Institutional Review Board professionals
| a Demographics of the research participant group | |||||
| Total (n = 450) | Cases (n = 228) | Controls (n = 155) | Relatives (n = 67) | p value | |
| Age, years | 63.6±11.8 | 64.3±11.4 | 64.0±11.5 | 60.5±13.6 | 0.079 |
| Women | 292 (64.9) | 145 (63.6) | 110 (71.0) | 37 (55.2) | 0.066 |
| Race | |||||
| Asian/Pacific Islander | 7 (15.6) | 4 (1.8) | 2 (1.3) | 1 (1.5) | 0.9149 |
| Black | 4 (0.9) | 2 (0.9) | 2 (1.3) | 0 | |
| Multi-racial/other | 16 (3.6) | 8 (3.5) | 4 (2.6) | 4 (6.0) | |
| White | 423 (94.7) | 214 (93.9) | 147 (94.8) | 62 (92.5) | |
| Education | |||||
| High School or less | 40 (8.9) | 19 (8.3) | 13 (8.4) | 8 (11.9) | 0.5922 |
| Some college | 107 (23.8) | 57 (25.0) | 37 (23.9) | 13 (19.4) | |
| Bachelor’s degree | 276 (61.3) | 126 (55.3) | 105 (67.7) | 45 (67.2) | |
| Unknown | 27 (6.0) | 26 (11.4) | 0 | 1 (1.5) | |
| b Demographics of the genetic researcher (ASHG) and Institutional Review Board (PRIM&R) groups | |||||
| ASHG (n = 351) | PRIM&R (n = 208) p value | ||||
| Women | 182 (51.9) | 148 (76.0) | <0.0001 | ||
| Opposite service | 94 (26.8) | 91 (43.8) | <0.0001 | ||
| Years working in genetic research/IRB | |||||
| <5 years | 61 (17.4) | 80 (38.5) | <0.0001 | ||
| >5 years | 289 (82.3) | 118 (56.7) | |||
Values are presented as mean ± SD or n (%). Opposite service is defined as Institutional Review Board professionals previously working as genetic researchers and genetic researchers previously working as Institutional Review Board professionals.
Among research participants, no statistically significant differences were seen in any ROR scenarios when stratified by participant type (i.e., cases, controls or relatives), level of education, or a diagnosis of any type of cancer at baseline (Table 2). As a result, participant types were grouped together in subsequent analyses. Agreements related to scenario 1 differed by gender. Accordingly, comparisons in Table 3 were adjusted for gender.
Table 2.
Adjusteda ordinal regression model results comparing the strength of agreement for each return of results scenario between the PIP groups
| OR | 95% CI | p value | |
|---|---|---|---|
| Researchers have an ethical obligation to return individual research results when: | |||
| (1) The results would affect a participant’s health or health care (n = 448) | |||
| Participant type | |||
| Control vs. case | 0.69 | 0.20, 2.36 | 0.56 |
| Relative vs. case | 1.72 | 0.52, 5.75 | 0.38 |
| Gender (male vs. female) | 3.06 | 1.11, 8.43 | 0.03 |
| Education | |||
| High school or less vs. BA/BS | 2.05 | 0.54, 7.83 | 0.29 |
| Some college/AA vs. BA/BS | 0.90 | 0.50, 1.61 | 0.73 |
| Age (years) | 0.98 | 0.94, 1.02 | 0.24 |
| Cancer at baseline, yes vs. no | 0.85 | 0.31, 2.32 | 0.75 |
| (2) A participant asks for them (n = 445) | |||
| Participant type | |||
| Control vs. case | 1.56 | 0.93, 2.63 | 0.09 |
| Relative vs. case | 0.70 | 0.31, 1.62 | 0.41 |
| Gender | 1.10 | 0.65, 1.85 | 0.72 |
| Education | |||
| High school or less vs. BA/BS | 0.78 | 0.21, 2.90 | 0.71 |
| Some college/AA vs. BA/BS | 0.59 | 0.24, 1.47 | 0.26 |
| Age (years) | 0.99 | 0.97, 1.02 | 0.57 |
| Cancer at baseline | 0.78 | 0.48, 1.28 | 0.33 |
| (3) The researcher feels that the participant might be interested in knowing (n = 447) | |||
| Participant type | |||
| Control vs. case | 1.59 | 0.96, 2.62 | 0.07 |
| Relative vs. case | 0.96 | 0.46, 1.99 | 0.91 |
| Gender | 1.27 | 0.78, 2.08 | 0.34 |
| Education | |||
| High school or less vs. BA/BS | 0.80 | 0.32, 2.01 | 0.63 |
| Some college/AA vs. BA/BS | 0.72 | 0.41, 1.28 | 0.27 |
| Age (years) | 0.98 | 0.96, 1.00 | 0.11 |
| Cancer at baseline | 0.67 | 0.41, 1.07 | 0.04 |
Adjusted for gender, education, age, except for gender (adjusted for education, age), age (adjusted for education, gender), and education (adjusted for age, gender).
Table 3.
Adjusteda ordinal regression model results comparing the strength of agreement for each return of results scenario between PIP, ASHG, and PRIM&R groups
| OR | 95% CI | p value | |
|---|---|---|---|
| Researchers have an ethical obligation to return individual research results when: | |||
| (1) The results would affect a participant’s health or health care | |||
| ASHG (n = 340) vs. PIP (n = 448) | 4.21 | 2.41, 7.36 | <0.0001 |
| PRIM&R (n = 196) vs. PIP (n = 448) | 5.52 | 3.01, 10.10 | <0.0001 |
| PRIM&R (n = 196) vs. ASHG (n = 340) | 1.25 | 0.77, 2.04 | 0.37 |
| (2) A participant asks for them | |||
| ASHG vs. PIP (n = 445) | 4.26 | 3.12, 5.82 | <0.0001 |
| PRIM&R (n = 199) vs. PIP (n = 445) | 2.92 | 2.04, 4.17 | <0.0001 |
| PRIM&R (n = 199) vs. ASHG (n = 343) | 0.67 | 0.47, 0.94 | 0.023 |
| (3) The researcher feels that the participant might be interested in knowing about them | |||
| ASHG (n = 346) vs. PIP (n = 447) | 11.38 | 8.31, 15.58 | <0.0001 |
| PRIM&R (n = 199) vs. PIP (n = 447) | 7.81 | 5.51, 11.07 | <0.0001 |
| PRIM&R (n = 199) vs. ASHG (n = 346) | 0.65 | 0.46, 0.92 | 0.014 |
PIP, Participant Issues and Expectations Project; ASHG, genetic researcher; PRIM&R, Institutional Review Board members.
Adjusted for gender.
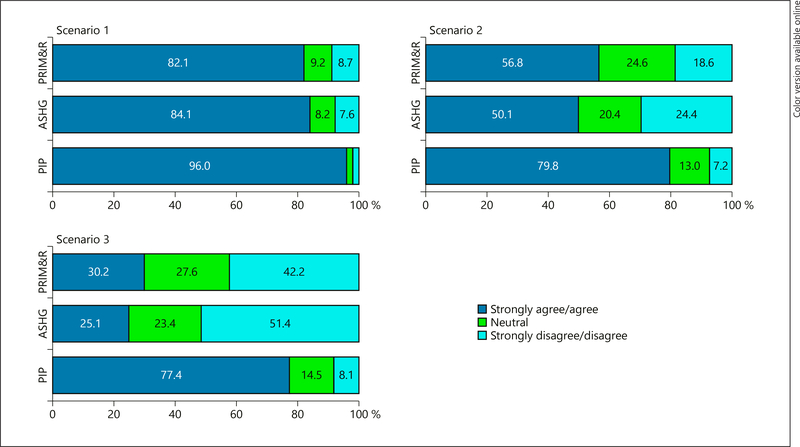
A comparison between the research participants, genetic researchers, and the IRB professionals is shown in Figure 1 for each ROR scenario. For each of the 3 scenarios, the majority of research participants agreed that individual results should be returned (Fig. 1). In scenario 1, over 80% of respondents in all 3 groups agreed that individual study results should be returned if the results would affect a participant’s health or health care, and over 50% of respondents in all 3 groups agreed that results should be returned if a participant asks for them (scenario 2), but there was a greater difference in the level of agreement between research participants and both researchers and IRB professionals. The biggest difference between research participants and the other 2 groups was seen in scenario 3. For the third scenario, while over 77% of research participants felt that results should be returned if the researcher feels the participant might be interested in knowing about the results, only about one-third of the researchers and IRB professionals agreed with this statement.
Fig. 1.
Comparison of agreement with 3 possible scenarios: genetic researcher (ASHG), Institutional Review Board member (PRIM&R), and research participant (PIP) groups. Scenario 1: researchers have an ethical obligation to return individual research results when the results would affect a participant’s health or health care. Scenario 2: researchers have an ethical obligation to return individual research results when a participant asks for them. Scenario 3: researchers have an ethical obligation to return individual research results when the researcher feels that the participant might be interested in knowing about them.
Results from the ordinal logistic regression models (Table 3) indicate that although at least 50% of respondents from all 3 groups agree with returning research results, differences between the groups are significant and indicate that for all scenarios researchers and IRB professionals are more likely to disagree or be neutral in their responses when compared to the research participants. For example, participants strongly endorsed the belief that researchers have an ethical obligation to return individual research results when the results would affect a participant’s health or health care (scenario 1), whereas genetic researchers were 4.2 times and IRB professionals were 5.2 times more likely to disagree or be neutral with this sentiment. Genetic researchers and IRB professionals were also more likely to be neutral or disagree with there being an ethical obligation to return results if a participant asked for them or if the researcher felt that a participant might be interested in knowing about them. When IRB members and genetic researchers were directly compared for these 2 scenarios, IRB professionals were more likely to agree that individual research results should be returned (OR = 0.67 and OR = 0.65, respectively).
Discussion
This study compared the perspectives of 3 important groups of stakeholders including research participants, genetic researchers, and IRB professionals regarding the return of individual research results to participants. While most respondents in each group agreed that researchers have an obligation to return individual research results when they would affect a participant’s health or health care, significant differences, reflecting the degree of agreement, were seen among these stakeholders in all of the ROR scenarios. Specifically, the researchers and to a lesser degree the IRB professionals were significantly less likely to believe that participants should receive results when they are requested. This has implications beyond communicating results. If researchers and IRBs claim that their research or oversight are serving the interests of society and research participants, participants themselves may understandably question how their interests are being represented or protected if results are not available to them, particularly when they are requested.
Most groups involved in genetic research agree that individual genetic findings that are highly penetrant (highly related to outcomes) and clinically actionable (useful in clinical practice) should be returned to the participant [17–24], although several studies have found that many researchers do not return results even if they believe that they should [25–27]. The most commonly cited reasons for not returning individual research results were expecting participants would have difficulty understanding the results, trouble contacting participants, or not considering the option [27]. Guidelines regarding informed consent language as well as the type, timing, and format of disclosed genomic research results have been suggested [28–31], but these leave a great deal of discretion to researchers. Further, guidelines around the return of genetic results with lesser penetrance or unknown significance are even less clear. Nevertheless, if participants desire results regardless of their significance, it may be prudent to consider developing proactive interpretations and communication strategies that deal with the various types of findings. Although there is no consensus on when, how or by whom results should be returned, there are 2 prevailing views from the scientific community. Those in favor of returning individual genomic results argue that the information may be valuable, it is respectful of the participant, and it increases participant autonomy [32]. Others argue that by definition, the goal of research is the advancement of knowledge, not the treatment of individual patients [33]; the original intent of the participant was altruistic [34]; harm may come from disclosure of nonvalidated results [34]; return of individual results may be perceived as undue inducement to participate [35]; and concern for legal liability [36].
While researchers have debated the question about obligation to disclose genetic results, including genetic incidental findings (GIFs), the views of IRBs on this topic are beginning to emerge. Like researchers, there is no consensus among IRBs about returning individual genetic results and disclosing GIFs. As a result, decisions about disclosing this information are typically determined at an institutional level by the IRB. In a national survey of 796 IRB professionals, Gliwa et al. [37] found that a minority of IRBs felt prepared to address issues about GIFs, but a majority believed there is an obligation to disclose GIFs. Although IRB respondents were divided when asked about what ethical principles might support an obligation to disclose GIFs, 3 principles emerged as the top-cited reasons: (1) the duty to warn a participant if the participant was in significant or imminent danger had the strongest support (84% strongly agreed or agreed), followed by (2) respect for autonomy (80% strongly agreed or agreed), and (3) beneficence (79% strongly agreed or agreed) [37]. Like researchers, the study by Gliwa et al. [37] shows that IRBs are moderately prepared to address these issues. Working to establish the ethical basis for returning results and to balance these against both practical issues and desires of participants themselves may better prepare IRBs to consider these issues and to also provide guidance to researchers. This study found that only about half of genetic researchers and IRB professionals believe that researchers should return individual results if the participant asks for them. This is in contrast to the research participant group, who were significantly more likely to agree that results should be returned if a participant asks for them. In addition, greater than three-quarters of the research participants stated that results should be returned if the researcher thinks the participant may be interested in knowing about them compared to only 25% of researchers and 30% of IRB professionals. To our knowledge, this is the first study to query research participants in a long-standing cancer registry about their attitude towards ROR in a way that directly enables comparisons with the views of other key stakeholder groups typically engaged in these discussions: researchers and IRB professionals. The degree of uniformity among this group of research participants casts doubt on some rationales for not returning results (especially the interpretation of the goal of the research and the [purely] altruistic intent of the participants).
Given the strong endorsement for the return of clinically actionable results from all 3 groups, there is a need to identify the potential barriers to ROR in the research context for this particular scenario. While the details may differ depending on the size of the research program, i.e., the 1 million All of Us Research Program versus an individual researcher’s genome-wide association study or sequencing study, there are similar issues that should be addressed. For example, what type of infrastructure will be needed to return results? Who should return results? How long should this obligation last? How much more funding will studies need to dedicate to ROR in order to be able to responsibly return results to participants? Should participants be updated as new information becomes available, and if so, over what period of time will this obligation last?
There are several limitations of this study. First, a comparison of the cases, controls, and relatives found no significant differences in attitudes towards the 3 ROR scenarios, suggesting that cancer participants feel similarly to relatives and to noncancer participants. Although 7% (n = 35) of the relatives and controls reported having had a cancer during the interval between baseline (1998) and this survey (2013), cancer status at the last follow-up was not significant in any of the scenarios (results not shown) and is unlikely to account for the lack of differences between these 3 groups. Further, our findings are similar to other studies showing that research participants favor the return of individual results [17–21]. Nevertheless, in the light of the borderline statistical significance for the case-control comparison in scenarios 2 and 3, we cannot exclude that lack of statistical power limited our ability to find case-control differences. Secondly, although the racial and ethnic diversity of our sample reflects that of the NWCGR, it is not racially or ethnically diverse. It is also possible that the online administration of this study biased these results by excluding participants who are not computer-educated or do not have access at home. Third, given their long-standing participation in this cancer registry, PIP participants may be more knowledgeable about research and have different expectations of the ROR than the general population. On the other hand, their experience may also be viewed as a strength and their preferences indicative of the factors that may be important for longer-term engagement of participants as will be required in the CMI and the All of Us Research Program. Finally, while data from researchers and IRB professionals were collected at the same time, data from participants was collected several years later. Although it is possible that the opinions of researchers and IRBs may have changed during the approximately 3.5-year interval such that the differences observed between the research participants and the researchers and IRB professionals no longer exist, these data indicate the possibility of large differences in opinion regarding 3 specific ROR scenarios. If this is true, these results indicate that one stakeholder group does not necessarily represent the views of other stakeholder groups.
Overall, our results are consistent with the body of literature indicating that we have no clear agreement between researchers, IRB members, and participants about most elements of returning research results. These results have important implications for the translation process of research to practice. For example, if researchers and IRBs do not have guidance and tools for returning results, they will likely do so less frequently and in a less standardized manner. The potential consequences may impact participants. Specifically, if participants do not receive the results they desire or request, they may feel used and underappreciated, and will likely lessen their engagement in existing and future studies. It is clear that we need to build agreement and mutual understanding between these stakeholder groups. As a start, we might consider focusing on the areas of agreement to pinpoint specific solutions, including who should return results, how long the obligation should last, how and what type of results should be returned, and who should pay for this. For areas of disagreement, it will be necessary to build consensus across stakeholder groups to bridge the divides. The goal here should be to identify solutions that are acceptable to participants, that ensure human subject protections, and that allow research to move forward. Application of these study results may also be considered for noncancer research areas in which genetic results play a role and necessitate the possible ROR [38], as well as other types of omics studies [39].
In summary, the debate surrounding the issue of ROR will take on new dimensions as we embark on 2 large national research initiatives with substantial data collection. These endeavors will require participation and engagement of large numbers of Americans. We have clearly illustrated that research participants are significantly more likely to desire the return of their individual research results than the researchers and IRB professionals desire to provide them. These differences will require careful consideration and resolution to accommodate the needs and perspectives of all stakeholders when developing policies and considering approaches for return of individual research results under the national Precision Medicine Initiatives.
Acknowledgement
This research was supported by NIH grant No. R01CA149051 to Karen L. Edwards (PI), “Identification of Issues and Expectations of Subjects Participating in Genetic Studies of Cancer.”
Footnotes
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.https://www.whitehouse.gov/the-press-of-fice/2016/02/01/fact-sheet-investing-national-cancer-moonshot (accessed August 2, 2016).
- 2.Collins FS, Varmus H: A new initiative on precision medicine. N Engl J Med 2015; 372:793–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker R, Boerwinkle E, Burke G, Collins R, Gaziano M, Lauer M, Manolio T: Building a Consortium of Cohorts – Cohort Identification and Participant Recruitment. https://www.nih.gov/sites/default/files/research-training/initiatives/pmi/building-consortium-cohorts.pdf.
- 4.http://grants.nih.gov/grants/guide/rfa-files/RFA-PM-16-002.html.
- 5.Edwards KL, Lemke AA, Trinidad SB, et al. : Genetics researchers’ and IRB professionals’ attitudes toward genetic research review: a comparative analysis. Genet Med 2012; 14: 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards KL, Lemke AA, Trinidad SB, et al. : Attitudes towards genetic research review: results from a survey of human genetics researchers. Public Health Genomics 2011; 14: 337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dressler LG, Smolek S, Ponsaran R, et al. : IRB perspectives on the return of individual results from genomic research. Genet Med 2012; 14: 215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lemke AA, Smith ME, Wolf WA, Trinidad SB; GRRIP Consortium: Broad data sharing in genetic research: views of Institutional Review Board professionals. PMC 2012; 33: 1–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Lemke AA, Trinidad SB, Edwards KL, et al. : Attitudes toward genetic research review: results from a national survey of professionals involved in human subjects protection. J Empir Res Hum Res Ethics 2010; 5: 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meacham MC, Starks H, Burke W, Edwards K: Researcher perspectives on disclosure of incidental findings in genetic research. J Empir Res Hum Res Ethics 2010; 5: 31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruiz-Canela M, Valle-Mansilla JI, Sulmasy DP: Genetics researchers’ preferences and attitudes on ethical aspects of genomics research: a comparative study between the USA and Spain. J Med Ethics 2009; 35: 251–257. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez CV, Strahlendorf C, Avard D, Knoppers BM, O’Connell C, Bouffet E, Malkin D, Jabado N, Boycott K, Sorensen PH: Attitudes of Canadian researchers toward the return to participants of incidental and targeted genomic findings obtained in a pediatric research setting. Genet Med 2013; 15: 558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Condit CM, Korngiebel DM, Pfeifer M, Renz AD, Bowen DJ, Kaufman D, Mercer Kollar LM, Edwards K: What should be the character of the researcher-participant relationship? Views of participants in a longstanding cancer genetic registry. IRB 2015; 37: 1–10. [PubMed] [Google Scholar]
- 14.Goodman D, Johnson C, Wenzel L, Bowen D, Condit C, Edwards KL: Consent issues in genetic research: views of research participants. Submitted. [DOI] [PMC free article] [PubMed]
- 15.R Core Team: R: A Language and Environment for Statistical Computing. Vienna, R Foundation for Statistical Computing, 2011. http://R-project.org/. [Google Scholar]
- 16.Venables WN, Ripley BD: Modern Applied Statistics with S, ed 4 New York, Springer, 2002. [Google Scholar]
- 17.Bollinger JM, Bridges JFP, Mohamed A, Kaufman D: Public preferences for the return of research results in genetic research: a conjoining analysis. Genet Med 2014; 16: 932–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arar N, Seo J, Lee S, et al. : Preferences regarding genetic research results: comparing veterans and nonveterans responses. Public Health Genomics 2010; 13: 431–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meulenkamp TM, Gevers SK, Bovenberg JA, Koppelman GH, van Hylckama Vlieg A, Smets EM: Communication of biobanks’ research results: what do (potential) participants want? Am J Med Genet A 2010; 152A: 2482–2492. [DOI] [PubMed] [Google Scholar]
- 20.O’Daniel J, Haga SB: Public perspectives on returning genetics and genomics research results. Public Health Genomics 2011; 14: 346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Townsend A, Adam S, Birch PH, Lohn Z, Rousseau F, Friedman JM: “I want to know what’s in Pandora’s Box:” comparing stakeholder perspectives on incidental findings in clinical whole genomic sequencing. Am J Med Genet A 2012; 158A: 2519–2525. [DOI] [PubMed] [Google Scholar]
- 22.Klitzman R, Appelbaum PS, Fyer A, Martinez J, et al. : Researchers’ views on return of incidental genomic research result: qualitative and quantitative findings. Genet Med 2013; 15: 888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleiderman E, Avard D, Besso A, et al. : Disclosure of incidental findings in cancer genomic research: investigators’ perceptions on obligations and barriers. Clin Genet 2015; 88: 320–326. [DOI] [PubMed] [Google Scholar]
- 24.Applebaum PS Fyer A, Klitzman RL, et al. : Reseachers’ views on informed consent for return of secondary results in genomic research. Genet Med 2015; 17: 644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shalowitz DI, Miller FG: Communicating the results of clinical research to participants: attitudes, practices, and future directions. PLoS Med 2008; 5:e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Partridge AH, Hackett N, Blood E, et al. : Oncology physician and nurse practices and attitudes regarding offering clinical trial results to study participants. J Natl Cancer Inst 2004; 96: 629–632. [DOI] [PubMed] [Google Scholar]
- 27.Rigby H, Fernandez CV: Providing research results to study participants: support versus practice of researchers presenting at the American Society of Hematology annual meeting. Blood 2005; 106: 1199–1202. [DOI] [PubMed] [Google Scholar]
- 28.National Heart, Lung, and Blood Institute Working Group; Fabsitz RR, McGuire A, Sharp RR, et al. : Ethical and practical guidelines for reporting genetic research results to study participants: updated guidelines from a National Heart, Lung, and Blood Institute working group. Circ Cardiovasc Genet 2010; 3: 574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simon CM, Williams JK, Shinkunas L, et al. : Informed consent and genomic incidental findings: IRB chair perspectives. J Empir Res Hum Res Ethics 2011; 6: 53–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simon C, Shinkunas LA, Brandt D, Williams JK: Individual genetic and genomic research results and the tradition of informed consent: exploring US review board guidance. J Med Ethics 2012; 38: 417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green RC, Berg JS, Grody WW, et al. ; American College of Medical Genetics and Genomics: ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med 2013; 15: 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ossorio PN: Letting the gene out of the bottle: a comment on returning individual research results to participants. Am J Bioeth 2006; 6: 24–25. [DOI] [PubMed] [Google Scholar]
- 33.Merz JF, Sankar P, Taube SE, Livolsi V: Use of human tissues in research: clarifying clinician and researcher roles and information flows. J Investig Med 1997; 45: 252–257. [PubMed] [Google Scholar]
- 34.Forsberg JS, Hansson MG, Eriksson S: Changing perspectives in biobank research: from individual rights to concerns about public health regarding the return of results. Eur J Hum Gen 2009; 17: 1544–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clayton EW, Ross LF: Implications of disclosing individual results of clinical research. JAMA 2006; 295: 37. [DOI] [PubMed] [Google Scholar]
- 36.Dressler LG: Biobanking and disclosure of research results: addressing the tension between professional boundaries and moral intuition; in Solbakk JH, et al. (eds): The Ethics of Research Biobanking. New York, Springer, 2009, pp 85–99. [Google Scholar]
- 37.Gliwa C, Yurkiewicz IR, Lehmann LS, Hull SC, Jones N, Berkman BE: IRB perspectives on obligations to disclose genetic incidental findings to research participants. Genet Med 2016; 18: 705–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Potaczek DP, Kabesch M: Current concepts of IgE regulation and impact of genetic determinants. Clin Exp Allergy 2012; 42: 852–871. [DOI] [PubMed] [Google Scholar]
- 39.Potaczek DP, Harb H, Michel S, Alhamwe BA, Renz H, Tost J: Epigenetics and allergy: from basic mechanisms to clinical applications. Epigenomics 2017; 9: 539–571. [DOI] [PubMed] [Google Scholar]