Abstract
The COVID-19 pandemic has highlighted the difficulties of countries and healthcare systems in preparing for major emergency situations. In the first month of the pandemic there was a global shortage of personal protective equipment (PPE), thereby causing a rise in infection cases and deaths among healthcare workers (HCWs) in some countries. Moreover, the PPE used in hospitals today is not designed for prolonged use, and causes problems such as headaches and vision difficulties. To address these problems, a case study of an active PPE system for HCWs that is based on 3D printing and the use of ready-made parts is presented here. This case study demonstrates a new approach toward the design and manufacturing of PPE in emergency situations that relies on rapid development and domestic manufacturing of products through 3D printing technologies. The system was developed during the first months of the pandemic under restrictive quarantine conditions, and was fabricated and then tested by HCWs at several hospitals. Apart from sterilization difficulties, the system received positive feedback in user testing.
Keywords: COVID-19, Medical device 3D printing, 3D printed PPE, Emergency situations, PPE design, Personal protective equipment
1. Introduction
The COVID-19 virus, which was declared to be a global pandemic by the World Health Organization (WHO) on March 11, 2020 (World Health Organization, 2020b), highlights the difficulties in preparing for large-scale global crises. During the first months of the pandemic, many countries reported having a shortage of personal protective equipment (PPE) (McMahon et al., 2020). In many cases, healthcare workers (HCWs) have had to reuse disposable PPE, for example: due to a guidance published by Public Health England, workers were obliged to reuse PPE because of the acute shortage of new PPE (Rimmer, 2020). Only six months later, the supply grew and the guidance was withdrawn (“Guidance [WITHDRAWN]: Considerations for Acute Personal Protective Equipment (PPE) Shortages,” 2020). In some case, such as in Peru, improvised PPE was used, which led to many cases of infections and deaths among HCWs (Gonzales-Tamayo et al., 2020). In China, the pandemic itself caused the production to stop, in some cases, and the supply chain was disrupted, causing manufacturing halts in many places over the world (Cohen & van der Meulen Rodgers, 2020), which contributed even more to the global shortage of PPE. In addition, because the PPE is produced in advance in mass quantities, for use and distribution worldwide in cases of crisis, it may reach its expiration date, after which it cannot be used, for example, in preparing for a crisis that never arrives (Brennan et al., 1999).
In terms of quality, the PPE currently used by HCWs is not designed according to the specific characteristics of the COVID-19 virus and the treatment that patients need. The current PPE is limited in its comfort and safety, especially when used over extensive periods of time (Vidua et al., 2020). The WHO recommendation for PPE for HCWs includes a certified N-95 face mask (or equivalent), eye or facial protection, a long-sleeve gown, and gloves (World Health Organization, 2020a). This equipment was designed to be used for a maximum of two or three hours. Studies show that working with this equipment for more than four hours may lead to headaches or to the exacerbation of pre-existing headaches (Ong et al., 2020). However, pressure on the healthcare system due to the large number of severe COVID-19 cases demands longer working hours. Additionally, HCWs report that PPE causes skin irritation, hair pulling, increased temperature sensation, and problems with fit that result in a loose seal (Locatelli et al., 2014), which significantly reduce the effectiveness of the PPE. The intensive use of PPE during the COVID-19 pandemic may also cause sensory problems, such as visibility and hearing problems, which may hinder the performance of HCWs and put their health and the health of their patients at risk (Shenal et al., 2012).
Here, a novel method of manufacturing PPE for emergency situations is presented. According to this method, after an emergency event, PPE and other emergency equipment is rapidly developed locally by multidisciplinary teams that assess the problems and issues to be solved and the available resources. The equipment is then produced using 3D printing methods and additive manufacturing (AM). The local development and production enables the equipment to be used immediately, without depending on shipping or long supply chains. The advantage of this method lies in its dependence on 3D printing and domestic manufacturing, which is available worldwide and enables the rapid development of products without expensive tooling and logistics. This method makes it possible to assess the special circumstances of emergency events and the needs that arise during such events, develop rapid prototype solutions, test them in real time, and receive feedback. The PPE described here may be manufactured locally by domestic 3D printers and shared digitally with workers in other locations.
This approach has already partially been shown to be useful during the first months of the pandemic through academic research on PPE and parts of PPE that were designed and manufactured by local workers in the private sector for domestic HCWs, such as the Oxyframe PPE (Maracaja et al., 2020) and the Air-Wave Protector (“How a Re-Fitted Snorkel Mask Can Save Lives: ‘Air-Wave.org Protector™,’” n.d.). However, for hospitals to adopt these devices and integrate them into their daily treatment routine, there is a need to provide them with a comprehensive protection solution that takes into account the availability of all the components, comfort and ease of use, dressing and undressing, the sterilization requirements between uses, human factors, and maximal protection from infection.
To solve these problems, made-on-demand PPE is suggested here. This method is demonstrated through the Air-Shade project, which was developed in Israel for use by HCWs in COVID-19 departments in hospitals. The Air-Shade PPE was developed by a team of designers and engineers during the first months of the pandemic. The system was designed in collaboration with medical staff at COVID-19 departments at several hospitals in Israel and the US. Feedback and evaluation of the system was received.
2. Method
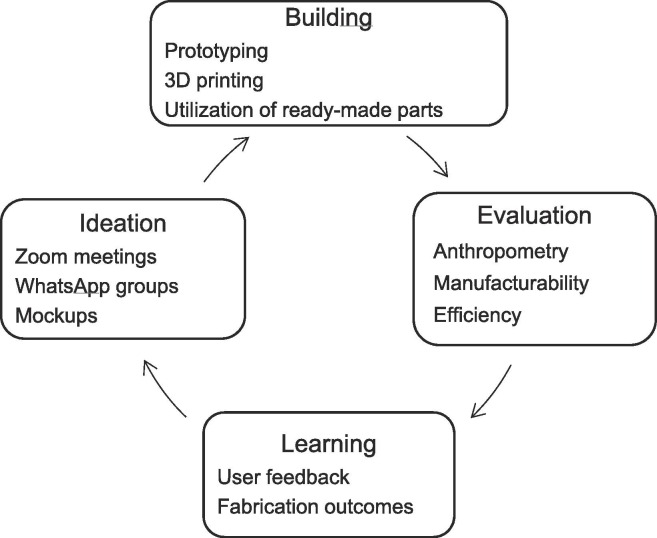
The Air-Shade project was developed by a multidisciplinary team under quarantine restrictions that prevented the team from physical interaction. To overcome this, and because of the need for fast correspondence, the short continuous “lean learning cycle” (Ries, 2011, p. 27) was used (Fig. 1 ). This helped to quickly define different design approaches and behaviors related to fluid efficiency, anthropometry, and usability based on the experience of medical staff.
Fig. 1.
Lean learning cycle. The diagram shows the process used to collaboratively analyze various aspects of design without physically meeting.
The team communicated through two platforms: WhatsApp, which was used mainly for short updates, sharing of media, and open discussion; and Zoom, which was used mainly for comprehensive ideation, problem-solving, and decision-making. Zoom meetings took place every evening to report on the work that was accomplished and define new targets for the following day. Files containing 3D models designed by the team members were shared using an online collaborative CAD tool that enables virtual review and sharing of 3D files. Fused filament fabrication (FFF) desktop 3D printers, owned by the team members and located at their homes, were used to 3D print prototypes and test physical samples. This allowed the team members to share their designs and to print and evaluate designs by other members, without the need to meet physically (Fig. 2 ).
Fig. 2.
Physical models of the Air-Shade system. These models were printed on the personal 3D printers of the design team members, as part of the development process.
2.1. System description
The system was designed based on knowledge and previous work done by team members in protecting civilians against chemical and biological warfare. The chemical weapon particles are much smaller than the COVID-19 virus, so repurposing and redesigning PPE intended to protect against chemical warfare may also provide maximal protection for medical staff against the COVID-19 virus. The main concept of the system is to create a stream of filtered air flowing over the face of the HCW, using a headband with nozzle vents. The air flowing over the user’s face creates a positive-air-pressure shield that prevents contaminated particles from reaching the user’s face. A headband is connected with a tube to a filter, and a compressor unit hangs from a belt over the wearer’s pelvis. The system was designed based on repeated feedback from hospital crews focusing on the cleaning process after a shift ends in closed COVID-19 departments. It includes a transparent visor film; a low-density polyethylene (LDPE) skin that completely covers the Air-Shade system, making it easier for the crew to clean any contaminated area of the product; and a hood that completely covers the head of the user (Fig. 3 ).
Fig. 3.
The Air-Shade system. The design is based on user feedback and is easy to clean.
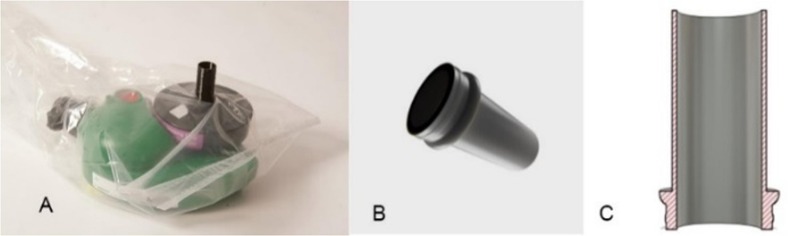
Tests were performed to track the behavior of the air going out of the nozzles and ensure that no air suction from the outside enters into the Air-Shade system. To keep the system wrapped in plastic but still allow air to enter the filter, a 3D printed disposable inlet connector is used. The connector allows air to flow into the filter without contaminating the blower. The inlet connector was designed in the shape of a tube, with an increment around the edge that snaps into the filter’s inlet hole. This assures that the airway stays clear (Fig. 4 ).
Fig. 4.
Inlet connector in the Air-Shade system. (A) Filter. (B) Inlet connector—designed to keep the system safe and sterilized. The connector connects to the filter shown in (A). (C) Cross section of the inlet connector, showing the stopper that snaps securely into filter.
2.2. Human factors
From the very first stage, the need arose to incorporate ergonomic principles into the design to solve problems of inconvenience in using PPE of this type and, moreover, to improve the user experience. Ergonomic adjustments for prolonged convenient use were made in the areas of anthropometry, usability, and thermal comfort.
2.2.1. Anthropometry
Under the case-study limitations, the headband was designed to fit the faces and heads of a substantial range of users, from the 5th to 95th percentiles of the Israeli population, including both men and women, using a “one size fits all” approach. Since there is no anthropometric data on the facial structure of the Israeli general population, head and face anthropometric data were obtained from the Henry Dreyfuss database (Tilley, 2001). Because of the importance of a good fit to a wide range of head dimensions, a flexible self-fit mechanism was used. The self-adjustment system uses stretch straps at the back of the mask and an adjustable waist belt for the high-efficiency particulate air (HEPA) unit. The accurate adjustment of the headband, which contains the air nozzles, to the forehead curve, is done by using a soft layer foam that creates good coupling by lightly stretching the head straps.
2.2.2. Usability
Easy and quick assembly of the system was taken into consideration in the design. Materials that are easy to clean and disinfect after use were chosen. To provide the necessary protection with minimal discomfort, lightweight components and flexible attachments were chosen. An important issue was finding the correct size and shape for the transparent visor screen and its desirable position over to the face. Screen dimensions that are too small may reduce protection, while an oversized screen may interfere with free head movement. Finally, to simplify the logistics, a commercial printable A4 clear sheet was chosen. The role of the airflow is to provide an effective “shield of air” preventing the entrance of polluted air and, at the same time, supplying an adequate amount of fresh air with minimal unwanted air suction from the thin foam head mediator.
Another important goal was to plan a non-turbulent air flow providing effective protection. This was achieved following several flow analyses concerning the desired shape, number, and arrangement of the flow nozzles. Activation of the HEPA produces two different sounds, created by the air compressor and the outlet nozzles. The airflow is audible but relatively undisturbing—no negative feedback was received on this issue. Importantly, the airflow was designed to provide the basic need for a protection shield along with the need for the visor to be clean from breath vapor. Breathing under a transparent visor causes condensation on the inner surface and, especially in cold conditions, creates a very disturbing fog. An effective way to prevent this is to allow a very small airflow to reach the surface of the visor. For users who wear eyeglasses, using the visor together with a surgical or N95 protective mask may blur vision through the eyeglasses, but the flow of air prevents this, as well.
2.2.3. Thermal comfort
Thermal comfort is a condition of feeling satisfied with the thermal environment, and this is highly determined by physical factors. In addition to the ambient temperature itself, thermal comfort is affected by four other factors, over which the medical staff has very little control:
-
(a)
Body insulation: Thermal insulation is measured in CLO units, and each item of clothing adds to the total CLO value. Protective clothing is worn above the regular clothing and contributes to the total CLO, thereby affecting body thermoregulation.
-
(b)
Self-metabolism: Physical activity raises the body temperature. In a hospital environment there is a conflict between the appropriate ambient temperature for patients, whose low metabolic rate in lying down requires a relatively high ambient temperature, and the desired temperature for the medical staff, whose physical activity is greater (Del Ferraro et al., 2015).
-
(c)
Relative humidity: This is another important factor in human thermoregulation and thermal comfort. Relative humidity determines the ability of the body to lower its temperature by sweating. High relative humidity prevents the sweat from evaporating and does not enable the body to cool down.
-
(d)
Airflow: A gust of air on the skin allows the temperature to be lowered by thermal convection. In addition, it improves the ability of sweat to evaporate. The head, which is usually the only organ that is not wrapped in protective clothing, plays an important role in heat transfer, and directivity determines the whole-body thermal sensation and thermal comfort (Chen et al., 2015).
The use of protective clothing in COVID-19 departments causes a significant decrease in thermal comfort, which is one of the most common complaints of medical staff (Karim et al., 2020). The protective clothing causes great discomfort and exhaustion, which may necessitate shortening the length of shifts. Active airflow may significantly improve thermal comfort and is important in solving this problem. In conclusion, active air filtering plays an important role in supplying fresh clean-filtered breathing air, eliminating the condensation of breath on the visor, and improving thermal comfort.
2.3. Manufacturing
Safety-on-demand PPE is created by a rapid process of development based on local needs and for local users, and it relies on two manufacturing methods. The first method is 3D printing. In this method, the printed parts are optimized in terms of printing time and in terms of quality and repeatability. The second method uses available off-the-shelf ready-made parts that may be integrated into the product with minimal need for assembly or processing. In this method, the product may be developed without depending on sourcing or supply chains, because only parts that are available locally are used. The 3D parts used in the Air-Shade system were designed using Fusion 360 software by Autodesk, a CAD program that enables remote collaboration by multiple users.
2.3.1. Readymade parts and improvisations
2.3.1.1. Compressors and filters
The compressor was obtained from a system used by the Israeli army for protection against chemical and biological warfare, available from the army’s emergency inventory. The system uses a HEPA filter. The compressor was modified to enable it to work with rechargeable batteries.
2.3.1.2. Air pipes and air-pipe connectors
The air pipe was disassembled from a siphon hand fuel pump. Before fixing it to the compressor, the original connector between the pipe and pump was cut out and heated to expand it temporarily, then attached to the blower outlet and reinforced with a zip tie. The original connector was used for exact fit and sealing. The outlet of the pipe fits the headband perfectly, since the headband inlet was designed in the shape of a cone to fit the pipe.
2.3.1.3. Textiles
The hood was developed from beginning to end, because off-the-shelf parts were unavailable. First, a half-hood version was developed. As the development of the system proceeded, the design of the hood was modified accordingly. At the time, there was a shortage of non-woven fabric, since manufacturers of medical garments held all the available stock. However, a roll of non-woven material with a waterproof membrane was obtained from a manufacturer of diapers. This material was used for sampling and manufacturing the final version of the hood.
2.3.2. Printing of 3D parts
In the manufacturing process, 3D printing is the technology that enables success. The fact that the parts are manufactured immediately on demand within a reasonable time, and the capability of making changes from one model to another without additional manufacturing changes, boosts productivity and allows developing the system while continuing to manufacture it. Two different types of 3D printers are used. The first is the 3D Platform 300 Series Workbench Pro 3D printer, which is a large-scale FFF printer with a 1-mm nozzle for fast industrial-scale printing. The second is an HP Jet Fusion 580 3D color printer, which uses HP Multi-Jet Fusion (MJF). The printer uses nylon 12 powder, which causes the product to remain intact under later autoclave sterilization by the medical staff. FFF 3D printing is used to print the inlet connector. The connector is printed using black polylactic acid (PLA) filament. The printing time for each connector is three minutes. It was designed for one-time use, with low resolution for fast printing. Using a large-scale printer for printing small parts permits fast production of multiple parts.
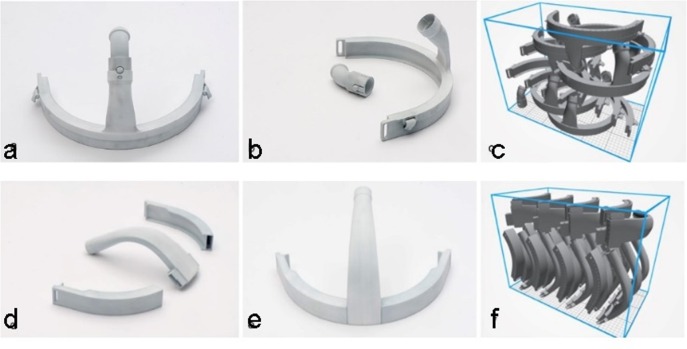
MJF 3D printing technology is used to manufacture the headband. The number of parts in the 3D printer build plates was optimized, and both the printing time and necessary post-process activities were minimized. The headband is divided into three parts that are later connected together by snap-fit for easy assembly (Fig. 5 d). By dividing the headband into parts, more units fit into the build chamber, thereby reducing the printing time of each headband from 73 to 43 min per unit (Fig. 5f). This also improves the quality of printing, since the orientation of the parts makes the post-processing (removing of the captive powder) much easier than when printing the headband as one unit.
Fig. 5.
Parts of the headband, printed from nylon on an HP Jet Fusion 580 3D color printer using HP Multi-Jet Fusion (MJF). (a) The headband, printed as one piece, with a detachable connector for the tube (attached to the top of the headband). (b) The same headband, with the detachable connector separated from the headband. (c) The arrangement of the 3D parts of the headband on the printer bed when printed as one piece. (d) The three parts of the headband when printed in parts. This optimizes the printing time and quality, and shortens the time required for post-processing. (e) The same headband after assembling the three pieces. (f) The arrangement of the 3D parts on the printer bed when printing the headband in three parts. Here, the arrangement is more efficient: more headbands are printed, and a better heat distribution reduces the number of distorted parts printed.
3. Results
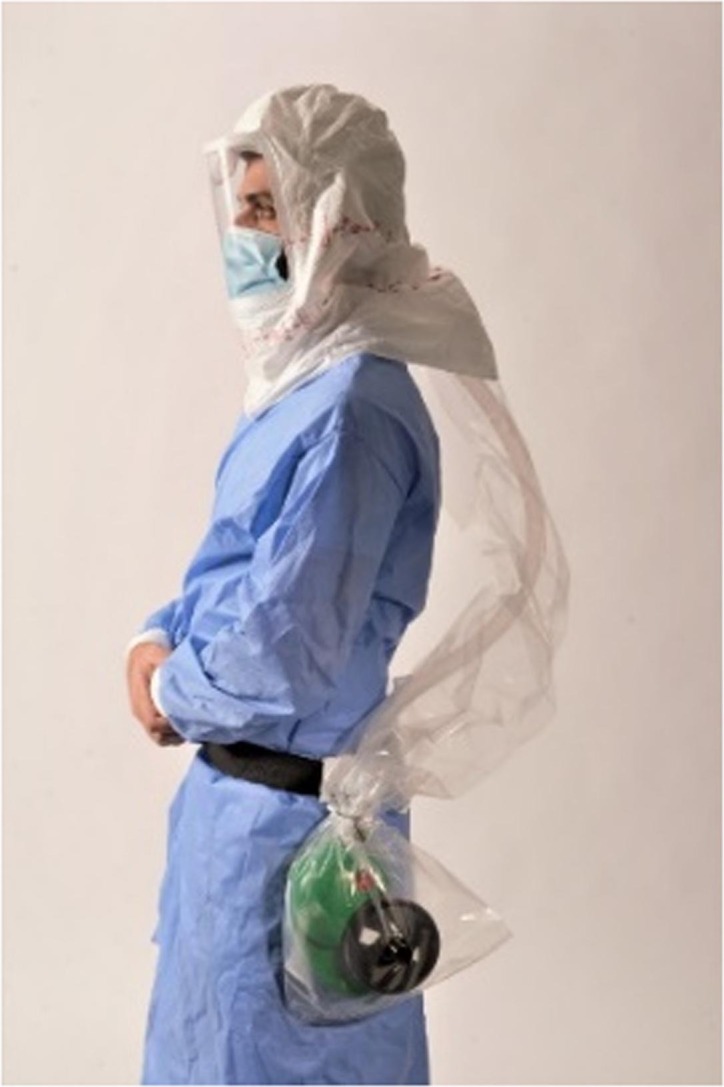
The system was used during the emergency period that was declared at the outbreak of the pandemic. Because of the emergency situation, medical teams accepted and tested the system inside COVID-19 departments at hospitals despite the fact that it did not yet undergo standard regulation and authorization. The system was tested by medical staff at the Rambam, Carmel (Fig. 6 ), and Bnei-Zion hospitals in Haifa, Israel, and the Holy Name Medical hospital in New-Jersey. The system was also tested by dentists at Hadassah hospital in Israel. A total of 15 working systems were delivered to these hospitals.
Fig. 6.

Healthcare worker (HCW) wearing the Air-Shade system. This worker is testing the device at the Carmel Hospital in Haifa, Israel.
In total, during and after the development, the system was tested by medical staff on eight occasions in COVID-19 departments at hospitals while treating patients. All testers reported a positive experience using the system and stated that wearing it made them feel more protected. The system’s ability to eliminate vapor was mentioned as a key advantage, since vapor accumulation on the visor inhibits clear sight and is a major concern for medical staff. Additionally, the testers were satisfied with the system’s ventilation. Other feedback included the ability to work smoothly while wearing the device due to the non-disturbing noise of the blower, alongside the uncomfortable position of the manifold sponge on the forehead, the difficulty in sterilizing the device between uses, the heavy weight of the device, and the lack in protection caused by the protruding pipe on the backside of the device, which hit surrounding objects in the room. It was suggested that the difficulty in sterilization may be partially solved by covering the blower and pipe with a disposable plastic sleeve. There were conflicting opinions concerning the level of difficulty in removing and sterilizing the system between uses.
In conclusion, HCWs were mostly satisfied with the new system; however, logistic challenges arose, mainly when the system was removed at the end of shifts. Usually, all PPE for HCWs is disposable and is thrown away after a shift ends. In the Air-Shade system, some parts are disposable, while others require sterilization. To ensure safety, HCWs must be aided by other workers in removing and disassembling the system after use. It is recommended for this aid to be assigned to a specific worker in a specified room. However, not all hospitals may have an extra worker and extra room available for this purpose.
4. Conclusions and discussion
Based on feedback from users at several hospitals, the Air-Shade system provides greater comfort and freedom to perform tasks than traditional PPE. However, since the system has disposable parts as well as non-disposable parts, there is a need to sanitize the non-disposable parts before each use. Removing the system at the end of a shift is challenging and requires the help of other workers in a designated room, since all of the parts are considered contaminated and must be handled with extreme care. This is the major setback of the system, since logistic operation by both the hospital and HCWs is required every time the system is removed. During the high-pressure emergency period, hospitals were willing to test and evaluate the new PPE despite the fact that it had not yet been formally approved and regulated; however, after the workload decreased, HCWs went back to using their previous PPE.
The use of new technologies that enable remote collaboration in manufacturing and communication presents a new paradigm in the design of PPE. It enables targeting problems in a more focused manner; however, it requires training, education, and openness to innovative ideas, as well as confidence and faith in proposed solutions. The 3D printing technologies are becoming cheaper and faster every day. Although 3D printing has not yet replaced traditional manufacturing, governments and policymakers may benefit from creating and training design response teams and providing them with resources for inventing and supplying solutions to emergencies, as well as creating a network of manufacturing facilities that are willing and able to produce these solutions when needed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The authors would like to sincerely thank the Systematics Ltd. team members for their guided assistance. Special thanks are offered to Prof. David Greenblat and the Flow Control lab members at the Mechanical Engineering faculty at the Technion institute of technology for the valuable contribution of design to the arduous research process.
Funding
This research was partially funded by the New York Metro Fund through the American Technion Society.
References
- Brennan R.J., Waeckerle J.F., Sharp T.W., Lillibridge S.R. Chemical warfare agents: emergency medical and emergency public health issues. Ann. Emerg. Med. 1999;34(2):191–204. doi: 10.1016/S0196-0644(99)70229-5. [DOI] [PubMed] [Google Scholar]
- Chen X., Wang Q., Srebric J. Model predictive control for indoor thermal comfort and energy optimization using occupant feedback. Energy Build. 2015;102:357–369. doi: 10.1016/j.enbuild.2015.06.002. [DOI] [Google Scholar]
- Cohen, J., van der Meulen Rodgers, Y., 2020. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prevent. Med. 141, 106263. https://doi.org/10.1016/j.ypmed.2020.106263. [DOI] [PMC free article] [PubMed]
- Del Ferraro S., Iavicoli S., Russo S., Molinaro V. A field study on thermal comfort in an Italian hospital considering differences in gender and age. Appl. Ergon. 2015;50:177–184. doi: 10.1016/j.apergo.2015.03.014. [DOI] [PubMed] [Google Scholar]
- Gonzales-Tamayo L., Arevalo-Oropeza M., Yáñez J.A. COVID-19 physician deaths in Peru: a result of an underfunded and fragmented healthcare system. SSRN. 2020 [Google Scholar]
- Guidance [WITHDRAWN]: Considerations for acute personal protective equipment (PPE) shortages. (2020, October 20). GOV.UK. Retrieved November 6, 2020, from https://www.gov.uk/government/ publications/wuhan-novel-coronavirus-infection-prevention-and-control/managing-shortages-in-personal-protective-equipment-ppe.
- How a re-fitted snorkel mask can save lives: “Air-Wave.org Protector™.” (n.d.). Air-Wave.org. Retrieved December 6, 2020, from https://www.air-wave.org/.
- Karim N., Afroj S., Lloyd K., Oaten L.C., Andreeva D.V., Carr C., Farmery A.D., Kim I.-D., Novoselov K.S. Sustainable personal protective clothing for healthcare applications: a review. ACS Nano. 2020;14(10):12313–12340. doi: 10.1021/acsnano.0c05537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locatelli, S.M., LaVela, S.L., Gosch, M., 2014. Health care workers’ reported discomfort while wearing filtering face-piece respirators. Workplace Health & Safety, 62(9), 362–368. https://doi.org/ 10.3928/21650799-20140804-03. [DOI] [PubMed]
- Maracaja L., Blitz D., Maracaja D.L.V., Walker C.A. How 3D printing can prevent spread of COVID-19 among healthcare professionals during times of critical shortage of protective personal equipment. J. Cardiothorac. Vasc. Anesth. 2020;34(10):2847–2849. doi: 10.1053/j.jvca.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon D.E., Peters G.A., Ivers L.C., Freeman E.E. Global resource shortages during COVID-19: bad news for low-income countries. PLoS Negl.Trop. Dis. 2020;14(7) doi: 10.1371/journal.pntd.0008412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.J.Y., Bharatendu C., Goh Y., Tang J.Z.Y., Sooi K.W.X., Tan Y.L., Tan B.Y.Q., Teoh H.-L., Ong S.T., Allen D.M., Sharma V.K. Headaches associated with personal protective equipment – a cross-sectional study among frontline healthcare workers during COVID-19. Headache: J. Head Face Pain. 2020;60(5):864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- Ries E. Crown Business; 2011. The lean startup: How today’s entrepreneurs use continuous innovation to create radically successful businesses. [Google Scholar]
- Rimmer A. COVID-19: Experts question guidance to reuse PPE. BMJ. 2020;369(8242) doi: 10.1136/bmj.m1577. [DOI] [PubMed] [Google Scholar]
- Shenal B.V., Radonovich L.J., Jr., Cheng J., Hodgson M., Bender B.S. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J. Occupat. Environ. Hygiene. 2012;9(1):59–64. doi: 10.1080/15459624.2012.635133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilley A.R. Rev Ed. John Wiley & Sons; 2001. The measure of man and woman: Human factors in design. [Google Scholar]
- Vidua R.K., Chouksey V.K., Bhargava D.C., Kumar J. Problems arising from PPE when worn for long periods. Med. Leg. J. 2020;88(15):47–49. doi: 10.1177/0025817220935880. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020a. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: Interim guidance. Retrieved December 6, 2020, from https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages.
- World Health Organization, 2020b. Rolling updates on coronavirus disease (COVID-19). Retrieved November 6, 2020, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.