Abstract
Aim
This study aimed to investigate and monitor the mental health status of pregnant women during the COVID-19 pandemic.
Materials and methods
The meta-analysis was used to study the literatures on the psychology of pregnant women in four databases until Sep 27, 2020.
Results
A total of 19 articles were included in the final meta-analysis. The overall prevalence of anxiety was 42 % (95 %CI 26 %–57 %) with substantial heterogeneity (I2 = 99.6 %). The overall prevalence of depression was 25 % (95 %CI 20 %–31 %) with substantial heterogeneity (I2 = 97.9 %). Age, family economic status, social support, and physical activity seem to correlate with the mental health status of pregnant women.
Conclusion
The prevalence of anxiety and depression among pregnant women increased significantly during the COVID-19 epidemic. Pregnant women are more concerned about others than themselves during COVID-19, and younger pregnant women seem to be more prone to anxiety, while social support and physical activity can reduce the likelihood of anxiety and depression. It is necessary to take some psychological intervention measures for pregnant women to help them go through this special period safely and smoothly.
Keywords: COVID-19, Pregnant women, Anxiety, Depression, Psychological intervention
1. Introduction
Till now COVID-19 has caused a pandemic worldwide. This has had a significant negative impact on the economy, health, and other sectors like the human mind. COVID-19 rapidly spread, widespread and powerful infectiousness, which has caused a degree of panic around the world. Currently, relevant papers indicated that COVID-19 has caused corresponding psychological disorders to many groups in the society (such as medical workers, ordinary people, etc.), and the related negative psychological emotions (such as anxiety and depression) are increased (da Silva and Neto, 2020; Salari et al., 2020; Pappa et al., 2020; Luo et al., 2020). Besides guidelines of treatment for COVID-19, relevant policies have been introduced in various countries, which show that psychological problems during COVID-19 are a problem that cannot be ignored.
Pregnant women are undergoing subtle changes both mentally and physically as their roles change from ordinary women to mothers. The World Health Organization (WHO) says that worldwide about 10 % of pregnant women and 13 % of women who have just given birth experience a mental disorder, primarily depression. In developing countries, this is even higher, i.e. 15.6 % during pregnancy and 19.8 % after childbirth (WHO, 2020). It has been reported that women are more likely to experience anxiety and depression symptoms during COVID-19 than men (Al-Rabiaah et al., 2020; Wang et al., 2020). Pregnant women are likely to be more affected during this particular period. Besides, there is much evidence that prenatal psychological problems adversely affect the babies. In a follow-up study of about 20 years, the offspring of depressed parents have about three times the risk of anxiety disorders, major depression, and substance dependence as the offspring of non-depressed parents (Weissman et al., 2006).
Therefore, more attention should be paid to the psychological changes in pregnant women during this period. As far as we know, many papers study the psychological changes of pregnant women during the COVID-19 epidemic have been published and no relevant meta-analysis, so the purpose of this study is to conduct a systematic review and meta-analysis of the papers in this field to analyze the impact of the COVID-19 pandemic on the psychological and mental status of pregnant women.
2. Method
2.1. Search strategy
To perform a systematic review and meta-analysis on studies evaluating the psychological impact of COVID-19 on pregnant women, we used the retrieval expression to retrieve systematically searched for related published articles from the three databases: Web of Science, Embase, PubMed. And the last retrieval was on September 27, 2020. Search time was limited to 2020. The study was approved by the Ethics Committee of the Eighth People’s Hospital of Xinjiang Uygur Autonomous Region.
Published papers were searched in PubMed using the following retrieval expression: ((pregnant women OR pregnancy OR perinatal) AND (SARS-CoV-2 OR COVID-19 OR coronavirus) AND (stress OR psychological OR mental OR anxiety OR depression OR depressive OR psychology)). Published papers were searched in Embase using the following retrieval expression: ('pregnant women':abstract,title OR pregnancy:abstract,title OR perinatal:abstract,title) AND (' SARS-CoV-2':abstract,title OR 'COVID-19':abstract,title OR coronavirus:abstract,title) AND (stress:abstract,title OR psychological:abstract,title OR mental:abstract,title OR anxiety:abstract,title OR depression:abstract,title OR depressive:abstract,title OR psychology:abstract,title). Published papers were searched in Web of Science using the following retrieval expression: theme: ((pregnant women OR pregnancy OR perinatal)) AND theme: ((SARS-CoV-2 OR COVID-19 OR coronavirus)) AND theme: ((stress OR psychological OR mental OR anxiety OR depression OR depressive OR psychology)).
2.2. Selection criteria
We consider that papers included in the systematic review analysis should meet the following criteria: 1) original studies about pregnant women's psychological response to COVID-19; 2) describing the results of psychological reactions related to pregnant women; 3) Not a case report. Papers included in the final meta-analysis need to meet additional following criteria: 1) rates of anxiety and/or depression are reported; 2) the outcomes of pregnant women and puerperal women were described separately.
All retrieved papers go through the review process. Initially, all duplicate papers were deleted. Then, abstracts and titles of the remaining papers were read to determine if they are relevant to this study. Finally, the full text of the remaining papers after Browsing the abstract and title were reviewed carefully according to the inclusion criteria. Papers still included after the above steps will be used in the analysis of this study. Papers included in the meta-analysis used a cross-sectional study literature quality assessment tool to assess literature quality. We consider papers with a total score of more than 10 to be of higher quality.
2.3. Statistical analysis
In this meta-analysis, the Stata SE 15.1 version was used. Each value of the results is represented by a 95 % confidence interval (95 %CI) in a random effects model. The heterogeneity between studies was assessed by the I2 (%) test. In Stata 12.0 software, Egger and Begg tests were used to find publication bias. P < 0.05 was considered to be a significant publication bias. And a sensitivity analysis was performed to test result stability.
3. Results
3.1. Search results
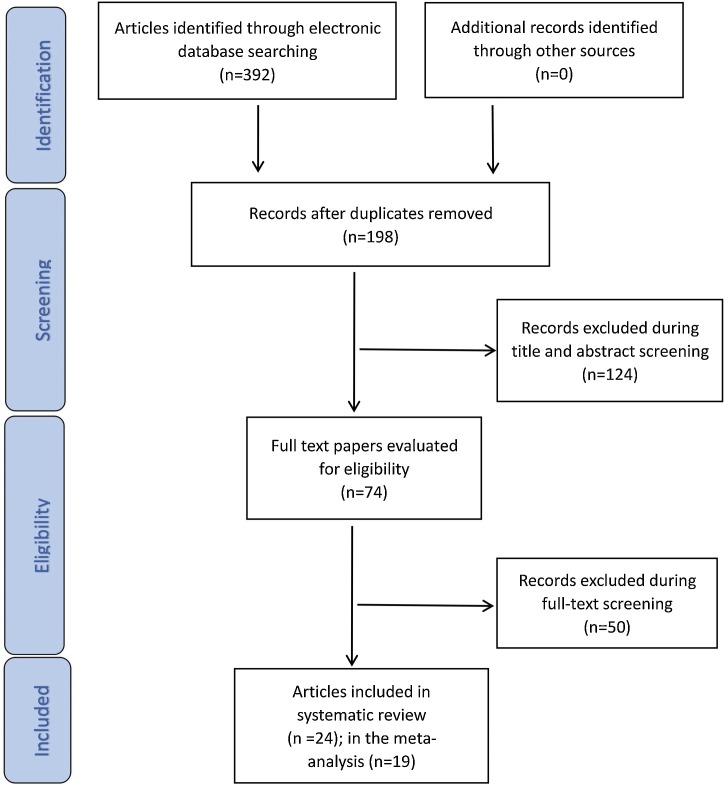
The detailed steps of the paper filtering process were shown in Fig. 1 . A total of 392 papers were obtained. After deleting repeated papers, 198 papers were obtained. After analyzing the title and abstract of the paper, 124 papers were excluded and 74 papers were included in the subsequent review. Finally, after careful review of the full text (we excluded a paper for which the full text was not available), a total of 24 papers were included in the systematic review, and 19 papers were included in the meta-analysis.
Fig. 1.
Flowchart of literature search.
3.2. Features of the papers included in the meta-analysis
The following basic characteristics of the included in the meta-analysis were extracted: Author and year, country, study population, assessment, cut-off, results (anxiety and depression rates). These results were documented in detail in Table 1 . All 19 papers from ten different countries were published in 2020. The number of subjects of the included studies ranged from 63 to 2,421. Different psychological questionnaires were used in different studies. According to the Egger and Begg tests, there was no obvious publication bias, and the sensitivity analysis found that the results were stable. In the paper quality evaluation, 16 articles scored more than 10 points, and 3 articles scored less than 11 points (Table 2 ). Four studies have specifically excluded pregnant women infected with COVID-19, while other studies have not addressed the issue.
Table 1.
Summary of basic information of the studies included for meta-analysis based on the PRISMA method.
| Author and Year | Country | Study Population | Assessment | Cut-off | Results |
|
|---|---|---|---|---|---|---|
| Depression % (n) | Anxiety % (n) | |||||
| Sade et al. (2020) | Israel | 84 | EPDS | EPDS≥10 | 25.0 %(21) | N.A. |
| Patabendige et al. (2020) | Sri Lanka | 257 | HADS | A total score of on the depression or Anxiety ≥8 | 19.5%(50) | 17.5 %(45) |
| Yue et al. (2020) | China | 308 | SAS | SAS>50 | N.A. | 14.3 %(44) |
| Gu et al. (2020) | China | 126 | N.A. | N.A. | 38.1 %(48) | 28.6 %(36) |
| Liu et al. (2020) | China | 1947 | SAS | SAS≥50 | N.A. | 17.2 %(334) |
| Durankuş and Aksu (2020) | Turkey | 260 | EPDS | EPDS>13 | 35.4%(92) | N.A. |
| Lebel et al. (2020) | Italy | 1987 | EPDS | EPDS≥13 | 37.0%(653) | Unable to get |
| Wu et al. (2020) | China | 1285 | EPDS | EPDS≥10 | 29.6%(381) | N.A. |
| Mappa et al. (2020) | Italy | 178 | STAI | STAI-S≥40 | N.A. | 77.0 %(137) |
| Ceulemans et al. (2020) | Belgium | 2421 | EDS; GAD-7 | EDS≥13 | 25.3 %(612) | 53.0 %(1275) |
| GAD-7 ≥ 5 | ||||||
| Parra-Saavedra et al. (2020) | Colombia | 941 | self-created questionnaire | N.A. | 25.0 %(235) | 49.9 %(469) |
| Suzuki (2020) | Japan | 117 | the tale of Whooley two questions; GAD-2 | at least one of the two questions is ‘yes’ | 29.9 %(35) | 25.6 %(30) |
| Matsushima and Horiguchi (2020) | Japen | 1777 | EPDS | EPDS≥13 | 17.0%(302) | N.A. |
| Thayer and Gildner (2020) | the United States | 2099 | EPDS | EPDS≥15 | 23.6%(496) | N.A. |
| Effati-Daryani et al. (2020) | Iranian | 205 | DASS-21 | N.A. | 32.7 %(67) | 43.9 %(90) |
| Silverman et al. (2020) | the United States | 485 | DPDS | EPDS≥9 | 15.1%(73) | N.A. |
| Zhou et al. (2020) | China | 544 | PHQ-9 | PHQ>10; GAD-7 ≥ 7 | 5.3 %(29) | 6.8 %(37) |
| GAD-7 | ||||||
| Preis et al. (2020) | the United States | 788 | GAD-7 | GAD-7 ≥ 5 | N.A. | 78.8 %(621) |
| Ayaz et al. (2020) | Turkey | 63 | BAI | BAI≥10 | N.A. | 90.5 %(57) |
EPDS: Edinburgh Postpartum Depression Scale; HADS: Hospital Anxiety and Depression Scale; SAS: Self-Rating Anxiety Scale; STAI: State-trait anxiety inventory; STAI-S: one separate sub-scales of STAI; PHQ-2: the Patient Health Questionnaire-2; GAD-7 and GAD-2: Generalized Anxiety Disorder 7-item Scale; DASS-21: Depression, Anxiety and Stress Scale-21; BAI: Beck Anxiety Inventory.
Table 2.
The JBI PACES and total score of each study.
| Studies | Year | The JBI PACES |
Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| Sade | 2020 | 2 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 15 |
| Patabendige | 2020 | 1 | 1 | 2 | 1 | 2 | 0 | 2 | 2 | 1 | 1 | 13 |
| Yue | 2020 | 2 | 1 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 1 | 12 |
| Gu | 2020 | 2 | 1 | 0 | 0 | 2 | 0 | 2 | 0 | 1 | 1 | 9 |
| Liu | 2020 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Durankuş | 2020 | 2 | 1 | 2 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 14 |
| Lebel | 2020 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 16 |
| Wu | 2020 | 2 | 1 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 15 |
| Mappa | 2020 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 1 | 14 |
| Ceulemans | 2020 | 2 | 1 | 0 | 0 | 2 | 0 | 2 | 0 | 1 | 0 | 8 |
| Parra-Saavedra | 2020 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 14 |
| Suzuki | 2020 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 2 | 1 | 0 | 10 |
| Matsushima | 2020 | 2 | 1 | 0 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 13 |
| Thayer | 2020 | 2 | 1 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 14 |
| Effati-Daryani | 2020 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 15 |
| Silverman | 2020 | 2 | 1 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | 1 | 11 |
| Zhou | 2020 | 1 | 1 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 13 |
| Preis | 2020 | 2 | 1 | 1 | 1 | 2 | 0 | 2 | 1 | 1 | 1 | 12 |
| Ayaz | 2020 | 1 | 1 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 14 |
The JBI PACES:The Joanna Briggs Institute, Practical Application of Clincial Evidence System.
3.3. The result of psychological influence
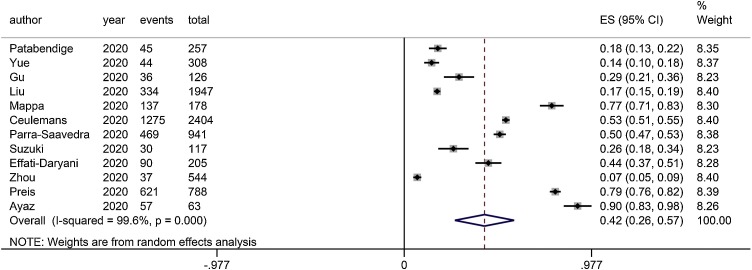
According to the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5TM), anxiety disorders include disorders that share features of excessive fear and anxiety and related behavioral disturbances. Anxiety is more often associated with muscle tension and vigilance in preparation for future danger and cautious or avoidant behaviors (Am. Psychiatr. Assoc., 2013). There are 12 studies reported anxiety rates as indicators of psychological impact. Ten studies reported specific scale form, one study did not clarify what scale was used, and one study used a homemade scale. Some papers reported the proportions of different levels of anxiety. The overall prevalence of anxiety was 42 % (95 %CI 26 %–57 %), with significant heterogeneity (I2 = 99.6 %), so a random-effect model was used (Fig. 2 ).
Fig. 2.
Meta-analysis of anxiety in pregnant women during the COVID-19 pandemic. The overall prevalence of anxiety was 42 % (95 %CI 26 %-57 %) with substantial heterogeneity (I2 = 99.6 %). ES: effect size. CI: confidence interval.
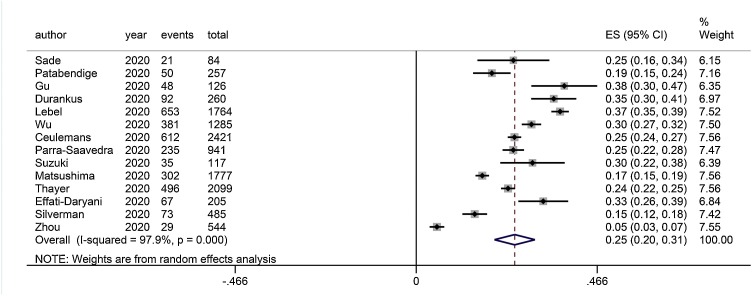
According to the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5TM), the Characteristics of depressive disorders are feeling sad, empty, or irritable, accompanied by physical and cognitive changes, which significantly affect an individual's ability to function (Am. Psychiatr. Assoc., 2013). There are 14 studies reported depression rates as indicators of psychological impact. Twelve studies reported specific scale form, one study did not clarify what scale was used, and one study used a homemade scale. Some papers reported the proportions of different levels of depression. The overall prevalence of depression was 25 % (95 %CI 20 %–31 %), with significant heterogeneity (I2 = 97.9 %), so a random-effect model was used (Fig. 3 ).
Fig. 3.
Meta-analysis of depression in pregnant women during the COVID-19 pandemic. The overall prevalence of depression was 25 % (95 %CI 20 %-31 %) with substantial heterogeneity (I2 = 97.9 %). ES: effect size. CI: confidence interval.
In addition to the two common psychiatric symptoms of anxiety and depression, other symptoms have been reported in pregnant women. Fear and stress are the most reported psychological symptoms after depression and anxiety. The mean stress score of 126 pregnant women was 8.50 ± 5.06 (Gu et al., 2020). In a study of the psychological reactions among pregnant women to the early stages of the COVID-19 pandemic, most of pregnant women reported increased financial stress (69.3 %), work stress (62.9 %), and home stress (59.6 %) (Zhang and Ma, 2020). Besides, a descriptive-analytical cross-sectional study reported mild stress symptoms (16/205, 7.8 %), moderate stress symptoms (32/205, 15.6 %), and high stress symptoms (16/205, 7.6 %), extremely severe stress symptoms (3/205, 1.5 %), and the mean (standard deviation,SD) score of stress was 6.22 (4.25) (Effati-Daryani et al., 2020). In a cohort study, Post-traumatic Checklist for DSM-5 (PCL-5), Dissociative Experiences Scale (DES-II), and Positive and Negative Affect Schedule (PANAS) were also used to evaluate Prenatal distress and psychiatric symptomatology; finally, dissociative symptoms (effect size,ES = 0.2 and 0.25), symptoms of post-traumatic stress disorder (ES = 0.19), negative emotions (ES = 0.96), and less positive emotions (ES = 0.95) in COVID-19 women were observed to be higher than in the pre−COVID-19 cohort (Berthelot et al., 2020). Insomnia (2.6 %), post-traumatic stress disorder(PTSD) (0.9 %), and somatic symptoms (2.5 %) were also reported in a study comparing pregnant women with non-pregnant women (Zhou et al., 2020). Besides, more than half of the pregnant women reported experiencing fear (67.5 %, 59.5 %), apprehensive (57.0 %), and helpless feelings (67.5 %) (Gu et al., 2020; Zhang and Ma, 2020).
4. Discussion
The main purpose of this paper is to learn about the psychological effects of COVID-19 on the mental health of pregnant women. In our current systematic review and meta-analysis, the overall reported anxiety rate was 42 % and anxiety rates documented in the papers included in the analysis ranged from 6.8%–90.5%. The overall reported depression rate was 25 % and depression rates documented in the papers included in the analysis ranged from 5.3%–38.1%. Mental disorders are common in pregnant women. Among the articles included in our meta-analysis, two studies showed that anxiety symptoms increased and one study showed that depression symptom increased in pregnant women before and after COVID-19 (Ayaz et al., 2020; Suzuki, 2020). So we have seen an increased incidence of psychological problems among pregnant women during COVID-19, consistent with what has been observed during previous epidemics of infectious diseases such as SARS (Lee et al., 2005). Pregnant women have a higher mixed prevalence of anxiety and depression than healthcare workers during COVID-19 (Pappa et al., 2020). Compared with the general population, pregnant women had a higher mixed prevalence of anxiety and a lower prevalence of depression (Luo et al., 2020).
We found that age may be associated with the likelihood of psychological problems in pregnant women. It appears the older a pregnant woman is, the less likely she is to experience anxiety and depression (Lebel et al., 2020; Wu et al., 2020; Matsushima and Horiguchi, 2020). In a survey of 257 participants, the youngest age group (18–25 years) accounts for the largest proportion (10/22, 45.5 %) of people with both depression and anxiety, and this was consistent among depressed people (17/50, 34.0 %) (Patabendige et al., 2020). The younger the woman is, the higher anxiety concerning delivery (Taubman-Ben-Ari et al., 2020). The authors concluded that younger age was associated with increased anxiety and depression scores in pregnant women, and that anxiety scores were more likely to be affected (Matsushima et al., 2020). Multiple regression analyses also indicated that younger age was associated with higher maternal psychological distress (Berthelot et al., 2020).
Besides, pregnant women's family economic situation is also a point of concern. Low socioeconomic status was confirmed one of several risk factors for depressive symptoms (Wu et al., 2020). Pregnant women who worry about their finances were more likely to have higher clinical depression scores (adjusted Odds Ratio [aOR]: 2.23, 95 %CI = 1.80,2.77, P < 0.001, adjusted model R2 = 0.06). Pregnant women with both high and low incomes were at risk of developing depression if they experienced COVID-19-associated financial stress (Thayer et al., 2020). In the unadjusted general linear model, stress scores were significantly correlated with household income (p<0.05). In the adjusted general linear model, there was still a significant correlation between family economic situation and stress score (Effati-Daryani et al., 2020).
In a variety of psychological changes that occur in pregnant women, we found that pregnant women seemed to care more about others than about themselves. Likert scale was used to assess the concerns of pregnant women and it was found that they cared more about their elders, partners, baby, and baby’s future than their health (p<0.05) (Ravaldi et al., 2020). Among the eight anxiety items related to COVID-19, the causes of anxiety (rated ‘much’ or ‘very much’) rank from highest to lowest: the use of public transportation (87.5 %), followed by the potential infection of other family members (71.7 %), being in public places (70.0 %), concern for the fetus (70.0 %), going for pregnancy check-ups (68.7 %), being infected themselves (59.2 %), and the delivery (55.4 %) (Taubman-Ben-Ari et al., 2020). In another study, although over half of women (50.7 %, 36/71) worried about their health often or all the time, they had heightened anxiety regarding their older relatives’ health (83.3 %,55/66), their other children (66.7 %, 28/42), and their unborn baby (63.4 %, 45/71) (Corbett et al., 2020). It is worth noting that when women devote more energy to caring for others. It may lead to a lack of attention to themselves, which can lead to the neglect of their health. This could also be one of the reasons why mental problems increase in pregnant women during COVID-19.
COVID-19 also seriously affects pregnant women's expectations of childbirth and obstetric decisions. Regarding birth experience, the primary emotions of more than half of pregnant women before COVID-19 were joy (63.0 %), less fear (7.5 %), and almost no sadness (0.5 %). After COVID-19, sadness (10.5 %) and fear (49 %) are greatly increased, while joy (17 %) is greatly decreased. Besides, although fear is commonly used by pregnant women to describe birth expectations before and after COVID-19, positive words (such as joy, happiness, sharing, and tranquility) are associated with fear before COVID-19, and negative words (such as restriction, sadness, loneliness, pain, anxiety, and incompetence) are associated with fear after COVID-19 (Ravaldi et al., 2020). Due to COVID-19, most pregnant women reported changed obstetric decisions. In a study from Italy, pregnant women changed prenatal care (89.0 %) and birth plan (35.0 %) (Lebel et al., 2020). In another study from China, only 16.3 % scheduled prenatal care as planned and 25.2 % scheduled Hospitalized delivery as planned; besides, the choice of hospital preference, delivery mode, infant feeding, the postnatal resting place has also changed (Liu et al., 2020).
According to a systematic review, factors most associated with prenatal anxiety or depression include lack of partner or social support, adverse life events, and high levels of perceived stress (Biaggi et al., 2016). This is consistent with the conclusions of the included papers. Taking appropriate measures can alleviate the adverse mental reactions of pregnant women. Pregnant women who received more social support and engaged in more physical work were less likely to experience Psychological problems (Yue et al., 2020; Gu et al., 2020; Lebel et al., 2020). The antenatal medical needs of pregnant women should be met as much as possible while measures are taken to prevent infection (e.g. regular telephone visits by doctors). The network can be used to spread COVID-19 knowledge to pregnant women to reduce the wrong perception and excessive panic of pregnant women about COVID-19. At the same time, family members should give pregnant women more care and support, always pay attention to the psychological changes of pregnant women, if necessary, can seek psychological counseling help.
There is strong evidence that prenatal psychological distress is harmful to the mother, the fetus, and the development of the child. In the context of COVID-19, pregnant women may experience additional psychological distress from worrying about their unborn child. In particular, there is no clear conclusion on vertical transmission of COVID-19, which may increase the psychological burden of pregnant women.
This study has a few limitations. First, different questionnaires are used in different papers to assess the psychological status of pregnant women, and the cut-offs of the same questionnaire were sometimes different. Second, the questionnaire is only a preliminary screening tool and could not clarify every. The results may not reflect the real psychological state of the pregnant woman. Third, using online questionnaire survey is likely to have a sampling error. Fourth, only two studies included in the analysis compared anxiety and depression symptoms in pregnant women before and after COVID-19, so we did not compare anxiety/depression of pregnant women before and during the COVID-19 pandemic. We can do this analysis when there are enough similar studies in the future. Fifth, all of the studies only reflected the psychological state of pregnant women at the time of the survey, and no long-term follow-up was conducted. Different attitudes towards the coronavirus and the corresponding measures taken in different countries may lead to different results.
5. Conclusion
COVID-19 has a significant impact on pregnant mental health, and meta-analysis shows an increased incidence of maternal anxiety and depression, which should attract the attention of obstetricians and gynecologists and become a priority in the field of public health. There is a need to provide women and women with psychological support during the epidemic to mitigate the adverse psychological effects of COVID-19.
CRediT authorship contribution statement
Si Fan: Data curation, Writing - original draft, Writing - review & editing. Jianping Guan: Investigation, Data curation. Li Cao: Investigation, Data curation. Manli Wang: Investigation, Data curation. Hua Zhao: Investigation, Data curation. Lili Chen: Supervision, Writing - review & editing. Lei Yan: Funding acquisition, Conceptualization, Methodology.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgment
This study was supported by the National Key Research and Development Program of China (2018YFC1004800).
References
- Al-Rabiaah A., Temsah M.H., Al-Eyadhy A.A., Hasan G.M., Al-Zamil F., Al-Subaie S., Alsohime F., Jamal A., Alhaboob A., Al-Saadi B., Somily A.M. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J. Infect. Public Health. 2020;13(5):687–691. doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Am. Psychiatr. Assoc . 5th ed. Am. Psychiatr. Publ.; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Ayaz R., Hocaoğlu M., Günay T., Yardımcı O.D., Turgut A., Karateke A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J. Perinat. Med. 2020;48(9):965–970. doi: 10.1515/jpm-2020-0380. [DOI] [PubMed] [Google Scholar]
- Berthelot N., Lemieux R., Garon-Bissonnette J., Drouin-Maziade C., Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet. Gynecol. Scand. 2020;99(7):848–855. doi: 10.1111/aogs.13925. [DOI] [PubMed] [Google Scholar]
- Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J. Affect. Disord. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceulemans M., Hompes T., Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: a call for action. Int. J. Gynaecol. Obstet. 2020;151(1):146–147. doi: 10.1002/ijgo.13295. [DOI] [PubMed] [Google Scholar]
- Corbett G.A., Milne S.J., Hehir M.P., Lindow S.W., O’connell M.P. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;249:96–97. doi: 10.1016/j.ejogrb.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva F.C.T., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020;104 doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durankuş F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J. Matern. Fetal. Neonatal. Med. 2020:1–7. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- Effati-Daryani F., Zarei S., Mohammadi A., Hemmati E., Ghasemi Yngyknd S., Mirghafourvand M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020;8(1):99. doi: 10.1186/s40359-020-00464-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu X.X., Chen K., Yu H., Liang G.Y., Chen H., Shen Y. How to prevent in-hospital COVID-19 infection and reassure women about the safety of pregnancy: experience from an obstetric center in China. J. Int. Med. Res. 2020;48(7) doi: 10.1177/0300060520939337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.H., Huang N., Chang H.J., Hsu Y.J., Wang M.C., Chou Y.J. The immediate effects of the severe acute respiratory syndrome (SARS) epidemic on childbirth in Taiwan. BMC Public Health. 2005;5:30. doi: 10.1186/1471-2458-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Chen M., Wang Y., Sun L., Zhang J., Shi Y., Wang J., Zhang H., Sun G., Baker P.N., Luo X., Qi H. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG. 2020;127(10):1229–1240. doi: 10.1111/1471-0528.16381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mappa I., Distefano F.A., Rizzo G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: a prospectic observational study. J. Perinat. Med. 2020;48(6):545–550. doi: 10.1515/jpm-2020-0182. [DOI] [PubMed] [Google Scholar]
- Matsushima M., Horiguchi H. The COVID-19 pandemic and mental well-being of pregnant women in Japan: need for economic and social policy interventions. Disaster Med. Public Health Prep. 2020:1–6. doi: 10.1017/dmp.2020.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-Saavedra M., Villa-Villa I., Pérez-Olivo J., Guzman-Polania L., Galvis-Centurion P., Cumplido-Romero Á, Santacruz-Vargas D., Rivera-Moreno E., Molina-Giraldo S., Guillen-Burgos H., Navarro E., Flórez-Lozano K., Barrero-Ortega A., Sanz-Cortes M., Miranda J. Attitudes and collateral psychological effects of COVID-19 in pregnant women in Colombia. Int. J. Gynaecol. Obstet. 2020;151(2):203–208. doi: 10.1002/ijgo.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patabendige M., Gamage M.M., Weerasinghe M., Jayawardane A. Psychological impact of the COVID-19 pandemic among pregnant women in Sri Lanka. Int. J. Gynaecol. Obstet. 2020;151(1):150–153. doi: 10.1002/ijgo.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2(3) doi: 10.1016/j.ajogmf.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravaldi C., Wilson A., Ricca V., Homer C., Vannacci A. Pregnant women voice their concerns and birth expectations during the COVID-19 pandemic in Italy. Women Birth. 2020;(20) doi: 10.1016/j.wombi.2020.07.002. S1871-5192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sade S., Sheiner E., Wainstock T., Hermon N., Yaniv Salem S., Kosef T., Lanxner Battat T., Oron S., Pariente G. Risk for depressive symptoms among hospitalized women in high-risk pregnancy units during the COVID-19 pandemic. J. Clin. Med. 2020;9(8):2449. doi: 10.3390/jcm9082449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global. Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman M.E., Medeiros C., Burgos L. Early pregnancy mood before and during COVID-19 community restrictions among women of low socioeconomic status in New York City: a preliminary study. Arch. Womens Ment. Health. 2020:1–4. doi: 10.1007/s00737-020-01061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki S. Psychological status during the first trimester of pregnancy under the COVID-19 epidemic in Japan. J. Matern. Fetal. Neonatal. Med. 2020:1–2. doi: 10.1080/14767058.2020.1793319. [DOI] [PubMed] [Google Scholar]
- Taubman-Ben-Ari O., Chasson M., Abu Sharkia S., Weiss E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J. Reprod. Infant Psychol. 2020;38(3):340–348. doi: 10.1080/02646838.2020.1786037. [DOI] [PubMed] [Google Scholar]
- Thayer Z.M., Gildner T.E. COVID-19-related financial stress associated with higher likelihood of depression among pregnant women living in the United States. Am. J. Hum. Biol. 2020:e23508. doi: 10.1002/ajhb.23508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M.M., Wickramaratne P., Nomura Y., Warner V., Pilowsky D., Verdeli H. Offspring of depressed parents: 20 years later. Am. J. Psychiatry. 2006;163(6):1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- WHO Maternal Mental Health. https://www.who.int/teams/mental-health-and-substance-use/maternal-mental-health
- Wu Y., Zhang C., Liu H., Duan C., Li C., Fan J., Li H., Chen L., Xu H., Li X., Guo Y., Wang Y., Li X., Li J., Zhang T., You Y., Li H., Yang S., Tao X., Xu Y., Lao H., Wen M., Zhou Y., Wang J., Chen Y., Meng D., Zhai J., Ye Y., Zhong Q., Yang X., Zhang D., Zhang J., Wu X., Chen W., Dennis C.L., Huang H.F. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am. J. Obstet. Gynecol. 2020;223(2) doi: 10.1016/j.ajog.2020.05.009. 240.e1-240.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue C., Liu C., Wang J., Zhang M., Wu H., Li C., Yang X. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: the mediating effect of risk perception. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020941567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020952116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Shi H., Liu Z., Peng S., Wang R., Qi L., Li Z., Yang J., Ren Y., Song X., Zeng L., Qian W., Zhang X. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl. Psychiatry. 2020;10(1) doi: 10.1038/s41398-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]