Abstract
Coronavirus Disease 2019 (COVID-19) is one of the biggest challenges of the 21st century. While researchers are working on vaccine development and elucidating the mechanism of action and evolution of the harmful SARS-CoV-2, the current most important public health measure, second only to social distancing, is the obligatory wearing of facial protection. The Centers for Disease Control and Prevention recommended in April 2020 that the public wear face coverings in areas with high rates of transmission based on epidemiological evidence on the strong relationship between mask wearing and pandemic control. This protection against SARS-CoV-2 and other airborne pathogens, boost the design and production of innovative solutions by industry stakeholders. Nanoparticles, nanofibers, and other pioneering technologies based on nanomaterials have been introduced in mask production chains to improve performance and confer antiviral properties. During an emergency like COVID-19, these products directly available to the public should be carefully analyzed in terms of efficacy and possible long-term effects on the wearers’ skin and lungs as well as on the environment. This opinion paper provides a wealth of information on the role of nanotechnologies in improving the performance of facial masks and on possible future consequences caused by a poorly regulated use of nanotechnology in textiles.
Keywords: Nanotechnology, Face masks, COVID-19, Nanowaste, Droplets, Nanomaterials, Toxicity, Environment
Graphical Abstract
Introduction
As SARS-CoV-2 continues its global spread, universal mask wearing is protecting the world population. The most evident reason is of course the prevention of viral particles shedding from noses and mouths of infected and asymptomatic people as supported by model simulations [1] and data collected during the first 100 days of 2020 [2]. Further, face masks might be involved in a sort of variolation of the population. Indeed it has been recently proposed that if the severity of the disease is proportionate to the viral load, wearing masks would reduce the viral inoculum and the subsequent clinical impact by increasing asymptomatic infections [3].
Besides the touching of infected surfaces, influenza transmission can occur via large droplets, which remain suspended in the air for a short time or via small airborne particles that can be transmitted over longer distances. Indeed, in the air, respiratory particles shrink to a diameter estimated to be a little less than one-half their initial diameter, if completely desiccated [4]. These smaller droplets can penetrate the smaller bronchi [4], [5], [6].
Based on filtering efficiency, protective masks can be classified into single-use face masks, respirator masks, and surgical masks [7]. Single-use face masks and cloth masks are usually made of a single thin layer and cannot filter very small particles, however, they might still be able to block the emission of large droplets and are useful when the supply of masks is limited in the community [7].
Respirator masks (N95 masks in US and FFP2 masks in Europe) have the highest filtering capacity (at least 95% of particles of 0.3 µm for N95 respirators) and fit tightly onto the wearer's face. Respirator masks are usually made of four layers comprising a non-woven layer that filters 0.5 µm particles, an activated carbon layer that filters chemicals, a cotton layer that filters 0.3 µm particles and a second non-woven layer. They might have an optional valve for the regulation of breathing [7].
Surgical masks became the most common protective mask. They loosely fit on the face and are designed to block large respiratory droplets during routine surgical procedures but do not filter small particles. Based on their efficacy, surgical masks are classified into different levels with level 3 having the highest filtration efficacy (> 98% of particles of 3.0 µm) and maximum fluid resistance.
Surgical masks are commonly made of three layers, with a filter layer placed between two layers of non-woven fabric. The outer layer is hydrophobic, while the inner layer is absorbent and is in contact with the skin of the wearer. The middle filter layer is most commonly made of polypropylene. Other types of protective equipment, P100 respirator/gas mask, self-contained breathing apparatus and full-face respirators are not commonly used by non-healthcare workers [8].
The frontier in clothing technology is represented by nanoengineered functional textiles, where nanomaterials are embedded into textiles to confer new functions without altering the comfort of the substrate [9]. Nanomaterials have the same size as viral particles and because of their huge surface to volume ratio, exhibit physical, chemical, and biological properties that are different from larger-sized materials [10]. Surface area, melting point, fluorescence, electrical conductivity, magnetic permeability, and chemical reactivity are examples of properties that change as a function of the size of the particle. This phenomenon causes selective interactions with biological systems especially with nanosized organisms such as viruses and bacteria.
Nano-based products for vaccine against and diagnosis of SARS-CoV-2 infections have been the main focus of the last seven months of research in the nanotechnology field [11], [12], [13], [14], [15] Nanoparticle-based biosensors for coronavirus have also emerged as sensitive and selective diagnostic tools for early-stage detection [16].
Given the importance of mask-wearing health measures, the response of the nano research community to the Coronavirus Disease 2019 (COVID-19) pandemic in terms of personal protective equipment design has been prompt. Textiles companies are looking increasingly to engage nanotechnologies and specifical nanomaterials in the quest for new solutions to the pandemic challenge. Nanofibers and nanoparticles have been incorporated into respiratory masks, providing antiviral properties, high breathability and filtration capacity [10].
In the following text, we will briefly discuss the main research findings in face mask production based on nanotechnology and our concerns about nanosafety, an often-underestimated drawback in the nanotech industry. Finally, we address necessary changes in social behavior and possible regulated disposal of used face masks to reduce environmental impact caused by the use of nanotechnology-based protective equipment [17], [18].
Improved mask performance with nanotechnology
An ideal face mask possesses efficiency in the filtration of bio-aerosols and a good level of comfort. External factors affecting mask quality are humidity, temperature and frequency of respiration and the latter is influenced by comfort. Other external factors influencing mask filtration are the velocity and pattern of airflow, the charge and size of the incoming particle and the loading time.
As recently pointed out, the efficiency of face mask depends on both external factors and on the material properties such as chemical composition, thickness and packing of the fibers, number of layers, fiber diameter, and charge density [8].
Among all of these, the particle size, charge, and flow rate are the most important parameters to take into account. For small particles like viruses, in low flow rate conditions, diffusion and electrostatic mechanisms are dominant. By increasing the flow rate, interception of viral particles in mask fibers occurs.
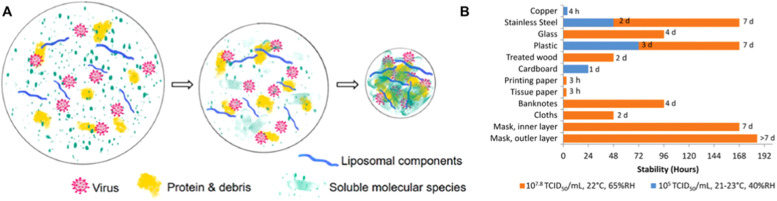
Nanomaterials already available in face masks on the market include copper dioxide, carbon, graphene, nanodiamonds, nanosilver and titanium dioxide [11], a list of patented antiviral technologies from Campos and colleagues is reported [19] ( Fig. 1).
Fig. 1.
Patents that use nanomaterials for production of Personal Protective Equipment.
Printed with permission from [19], Creative Commons CC BY.
When embedded in textile products, nanomaterials can modify mask fibers and improve filtration efficiency (or other parameters), while simultaneously nanomaterials can directly affect the viability of viruses that come in contact with the mask.
Polymers used in masks include polypropylene, that does not adsorb moisture and can be easily charged, polyethylene, polyesters, polyamides and polycarbonates [8]. Polyester woven fabrics are able to better maintain a static charge compared with natural fiber or cotton, because polyester woven fabrics are less capable of water absorption or hygroscopic [20]. Mask filters are commonly made of nonwoven fibrous materials, like wool felt, fiberglass paper, or polypropylene [8]. Several household materials (chiffon, flannel, synthetic silk, satin, cotton, paper-based products, nylon) have been used for face protection in public settings and their filtration efficiency has been compared in recent papers [20], [21].
The physical properties of masks can be modified with nanomaterials to improve performance. For example optimization of thermal comfort of face masks is required, especially for long term use by healthcare professionals and since moist warm conditions facilitate the survival of microorganisms [22]. The thermal properties are mainly determined by the thickness of the fibers, but the thickness is tightly correlated also to the particle removal efficiency (better with thick fibers) and air permeability (better with thin fibers). Using nanofiber on nanoporous polyethylene provides a cooling effect and good particle filtration to the mask [22]. Conversely, adding a silver layer to these materials provides a high infrared reflectance and a warming effect. This is particularly relevant considering the well-known antimicrobial effects of silver on surgical masks [23], [24].
If the face mask fibers are charged into electrets with quasi-permanent dipoles, the filtration efficiency improves without adding any mass or density to the structure. This allows the preservation of high air permeability [21]. Barium titanate (BaTiO3) nanomaterials possess long-term charge storage ability and have been used as the ferroelectric inorganic electret during the electrospinning process to construct filter membranes [25].
Static charge inevitably dissipates through the adsorption of water molecules from the air, or through contact with other surfaces. For example, at 22 °C and 40% relative humidity, the charge of polyester and silk decays relatively quickly (30 min) compared to nylon and spun bound polypropylene [21]. Hydrophilic polymers can also adsorb water molecules in environmental humid conditions and discharge. Moreover textiles like cotton are hygroscopic and retain water. Recently our group has demonstrated that the addition of graphene nanoplatelets can reduce cotton hygroscopy [26].
When viral particles reach the surface of the mask and are not destroyed, they can penetrate the mask textile. This becomes a microorganism collector in a warm and humid microenvironment [8]. For this reason, nanoparticles that inactivate the virus when it passes through the mask could pre-sanitize the inhaled/exhaled droplets, as recently proposed [5]. Graphene and graphene oxide are capable of decreasing the infectivity of solutions containing SARS-CoV-2 when filtered through textiles (cotton and polyurethane) functionalized with these nanomaterials [26]. Graphene incorporation into fabrics can also improve mechanical strength, flame-resistance, conductivity, resistance to abrasion, and UV-protectivity [27].
Polyethyleneimine polymer coatings seem to induce irreversible adhesion of the viral particles onto surfaces and cause viral structural damage [28]. Specifically, virus particles adhere to the hydrophobic polycationic coatings via electrostatic and hydrophobic interactions and a leakage of viral RNA from the viral particles occurs, caused by damage to the viral structure. Possibly, upon interactions with polycations, as observed with model lipid vesicles, lateral segregation and flip-flopping of phospholipids could fluidize viral envelope membrane and disrupt the ordered lipid rafts.
Similarly, quaternized chitosan nanofibers display antiviral activity upon contact thanks to the positive charge and hydrophobicity [29]. Generally, antiviral polysaccharide coatings that recognize pathogen mucopolysaccharides could be exploited as an environmentally friendly solution to improve mask antiviral activity [30]. Comprehensive reviews on nanotechnologies that can be exploited against viruses have been published recently [12], [19], [31], [32].
The possibilities offered by nanotechnology are endless [12], however we want to reiterate an important concern raised by Huang and colleagues [5] during the early emergency phase: the composition of the infecting respiratory droplet.
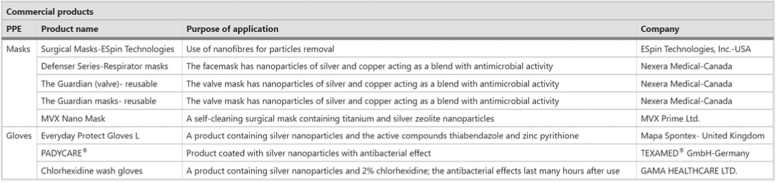
As shown in Fig. 2A, droplets are not made of individual uncoated viral particles but contain a variety of other mucus components, such as proteins, enzymes, bacteria and cell debris from the upper respiratory tract, lipidic matter such as lung surfactants and cholesterol, and soluble species like salt and lactate. Once semi-dried, this biological mass is called droplet nuclei and protects virions from disinfectants and desiccation by holding condensed water [5], [33]. This is the main reason for the SARS-CoV-2 viability on different surfaces (Fig. 2B). On one side broad-spectrum molecules active against several type of microorganism and capable of dispersing organic matter are more desirable to avoid mask contamination. On the other hand, one can envisage a draining system that leads to a fast water loss from the mask to reduce viral survival. Indeed water is necessary for the assembly of the viral envelope and its absence or its loss through capillary compression could mechanically deform virions [5].
Fig. 2.
(A) Components of the droplet and formation of droplet nuclei. Further permissions related to the material excerpted should be directed to the ACS. (B) Stability of SARS-CoV-2 on different surfaces, viral titers are indicated in blue or orange.
(A) Printed with Permission from [5] Copyright © 2020 American Chemical Society. (B) Printed with permission from [12] Creative Commons CC © 2020 The Authors. Published by Wiley‐VCH GmbH.
Broad-spectrum antimicrobial molecules have already been used to functionalize textiles and are been commercialized [9], [19]. Carbon materials like graphene and graphene-based materials, quantum dots, nanodiamonds, multiwall or single wall carbon nanotubes have been tested on several types of microorganisms, including viruses [31], [34]. Graphene has also been screen printed in textiles to obtain flexible impedance biosensors to report the location of positives and identify sources of the outbreak [35], [36]. Silver, zinc and copper are well-known antibacterial species and can interfere with several stages of the virus reproductive cycle. Some of these elements have been successfully incorporated into textile fibers [19], [24].
Importantly, semiconductors like titanium dioxide (TiO2) and organic photosensitizing nanoparticles (like curcumin and riboflavins) can photo-dynamically kill viruses and bacteria: when these nanomaterials are exposed to light, they generate radical oxygen species that damage membranes, proteins and nucleic acids [12], [31]. Nanofibers containing TiO2 nanoparticles have been produced to create antimicrobial filters [37], also in combination with silver [23] and graphene [27]. For this photocatalytic activation, the textile layer containing semiconducting species or photosensitizing agents must be reached by light at appropriate wavelength.
Environmental safety, nanosafety and skin damages
Nanoparticle coatings on face masks should be durable against rubbing and washing, long-lasting, and non-toxic [5]. Fate of the nanoparticles embedded in textiles remains questionable, most likely they will be washed out as “nanowaste” with environmental consequences.
This is a problem because the huge surface to volume ratio of nanomaterials induces a dramatic increase in their toxicology, and most of the risks to human health and the environment are poorly understood at the moment, due to scarce epidemiological studies [10].
The concentration of nanoparticles released in washing liquid from functionalized textiles depends on the nanomaterial, the composition of the washing liquid, the washing procedure. Silver-containing textiles release significant amounts of dissolved and particulate silver depending on the manufacturing processes and on the use of ultrapure water or tap water for washing, which is less aggressive [9].
Copper and silver nanoparticles can induce important toxic health and environmental effects, such as immunotoxicity in both dams and offspring in mice [38], and toxic effects on marine species [39]. Although originally classified as biologically inert, there is a growing body of evidence on the toxicity of TiO2 to humans and non-target organisms, as recently outlined by Luo and colleagues [40]. A type of multiwalled carbon nanotube (MWCNTs) has also been classified as possibly carcinogenic to humans [10]. Importantly the toxicity of nanomaterials both in the environment and the human body strictly depends on their aggregative state [41], [42].
Nanotechnological products made to have direct contact with facial skin should be extensively dermatologically tested [43]. The use of protective equipment, especially when tightly sealed for a prolonged time on healthcare workers, has already raised dermatological concerns [7]. It has been pointed out that more skin-friendly materials and interface design are needed to take in consideration the changing skin conditions that arise from perspiration [5]. As an example, TiO2 cannot penetrate the deeper layers of skin and can be considered a skin-friendly nanomaterial [40]. A panel of graphene-based materials, including few-layer graphene, graphene, graphene oxide, and reduced GO did not induce irritation unless they were prepared with irritant surfactants such as sodium dodecyl sulfate and sodium dodecyl-benzenesulfonate [44]. Nanoparticles could also reach the lungs if nanoparticles are not firmly embedded in the face mask material. Acute effects in humans arising from inhalation of silver nanoparticles include lung failure, increased heart rate and decreased arterial blood oxygen pressure [45]. Due to their increased reactivity, nanomaterials may require additional testing to ensure that their impact on human health is low. New bioprinting techniques used to recreate skin or lung alveoli might be used for testing [46]. Artificial sweat was also used to test the concentration of the silver and TiO2 released from fabrics. The release rate was found to depend on the concentration of nanomaterials in the fabric and the pH of sweat [9].
Since no specific guidelines for the testing of nanomaterials at the skin level are currently available, Fusco and colleagues have proposed the use of SkinEthic™ Reconstructed human Epidermis (RhE), following the Organisation for Economic Co-operation and Development Test Guideline 439, validated only for chemicals. RhE is a fully differentiated three-dimensional epidermal tissue constituted of normal human keratinocytes in a chemically defined medium grown at the air–liquid interface.
To summarize the current issues, in Scheme 1 we propose a step-by-step process to account for both environmental and health risks, with possible guidelines for suppliers and consumers of nanomaterial-based products.
Scheme 1.
A step-by-step guide for interventions and behavior related to the use of protective equipment based on nanomaterials.
The control of exposure to nanomaterials should be carried out both by governments and suppliers. Government agencies should establish guidelines for production of nanomaterial-based products and ensure that companies comply with these rules.
Main regulatory issues go from the creation of harmonized nanoparticles nomenclature to the development of protocols for the characterization and control of nanomedicines. More sophisticated nanostructured designs are emerging and this requires careful understanding of pharmacokinetic and pharmacodynamic, determined by chemical composition and physicochemical properties, which thus poses additional challenges for regulatory bodies [47].
The ever-increasing amount of nanoparticles released into the environment demands new strategies for detection and removal from human waste, by coagulation, flotation, filtration, ozonation or other processes from the human waste [48], [49]. Protective equipment companies’ number has increased, together with the risk of poorly controlled placing of nanomaterials in the market. Therefore, it should be mandatory that national health systems inform consumers of the health risks related to nanowaste. From the suppliers’ perspective, precise control of release of nanomaterials from products and instructions for safe disposal and washing should be provided to users. Finally, consumers should comply with regulations that protect themselves and the environment [50].
Summary and outlook
While vaccine trials are still ongoing, the design of antiviral face masks based on nanotechnology could be the fundamental ally in the war against SARS-CoV-2 infections. Nanotechnology holds huge potential in various ways: (a) in the design of personal protective equipment and surface coatings able to inactivate the virus and prevent its spread; (b) in the design of highly specific sensors for virus and/or immunological response; (c) in the development of new drugs, (d) in the development of nano-based vaccines.
The nanoresearch community is having the chance to accelerate the translation of nanotechnology advances but should be aware of several ethical and nanosafety concerns. Specifically, nanoparticles in wastewater can represent a serious environmental issue that should be added up to the ocean pollution driven by the massive usage and wrong disposal of single use masks. Considering the ability of SARS-CoV-2 to spread through aqueous media, a strategy that envisages the sanitization of used masks should be urgently implemented. When designing and launching new face masks on the market, users should be made aware of self-contamination during removal and reuse, associated health and environmental risks, and correct waste disposal. The gravity of the pandemic and the urgency of finding effective solutions is hastening the rhythm of product development. For this reason, there is a high risk in the coming years of causing unexpected negative health and/or environmental problems by the incorrect use of nanotechnology. COVID-19 is putting a huge strain on the world population. Like the Spanish ‘flu pandemic of 1918, social and behavioral challenges are considerable. The discomfort of wearing facial masks has led to reduced adherence by the general public, lowering the protective effect or even increasing infection risk. Further, face masks disposal is not sufficiently well regulated and global health crisis is putting extra pressure on regular waste management practices.
A huge amount of money has been invested globally to boost nanotechnological research during the pandemic but we also urgently need effective interventions by governments to (i) increase the adherence of individuals to engaging to behaviors that protect themselves and the environment (ii) encourage nanosafety studies and (iii) promote the establishment of guidelines for the recycling of nanotech products and control of nanomaterials in the environment (Scheme 1).
A coordinated approach to reduce nanoparticle risk for the general public and environment by governments and companies should be mandatory during the pandemic and for the future.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Biography

Dr. Valentina Palmieri is researcher at Institute for Complex Systems (ISC) at National Research Council (Italy). VP is a medical biotechnologist and obtained a Ph.D. in Oncobiology and Medical Oncology in 2014. She worked in collaboration with several national and international groups and obtained National awards and International Grants such as Fondazione Umberto Veronesi Post-Doctoral Grant (2018), European Society of Clinical Microbiology and Infectious Diseases Grant (2017). Valentina Palmieri is expert in nanomaterial synthesis and characterization and nanoparticle research, and her work is focused on graphene antimicrobial and diagnostics applications.
References
- 1.Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., Kostelich E., Gumel A.B. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020;5:293–308. doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng V.C.C., Wong S.-C., Chuang V.W.M., So S.Y.C., Chen J.H.K., Sridhar S., To K.K.W., Chan J.F.W., Hung I.F.N., Ho P.-L. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gandhi M., Rutherford G.W. Facial masking for Covid-19—potential for “variolation” as we await a vaccine. N. Engl. J. Med. 2020;383 doi: 10.1056/NEJMp2026913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicas M., Nazaroff W.W., Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J. Occup. Environ. Hyg. 2005;2:143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang H., Fan C., Li M., Nie H.-L., Wang F.-B., Wang H., Wang R., Xia J., Zheng X., Zuo X. COVID-19: a call for physical scientists and engineers. ACS Nano. 2020;14:3747–3754. doi: 10.1021/acsnano.0c02618. [DOI] [PubMed] [Google Scholar]
- 6.van der Sande M., Teunis P., Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3 doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li D.T.S., Samaranayake L.P., Leung Y.Y., Neelakantan P. Facial protection in the era of COVID‐19: a narrative review. Oral Dis. 2020 doi: 10.1111/odi.13460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tcharkhtchi A., Abbasnezhad N., Seydani M.Z., Zirak N., Farzaneh S., Shirinbayan M. An overview of filtration efficiency through the masks: mechanisms of the aerosols penetration. Bioact. Mater. 2020;6:106–122. doi: 10.1016/j.bioactmat.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yetisen A.K., Qu H., Manbachi A., Butt H., Dokmeci M.R., Hinestroza J.P., Skorobogatiy M., Khademhosseini A., Yun S.H. Nanotechnology in textiles. ACS Nano. 2016;10:3042–3068. doi: 10.1021/acsnano.5b08176. [DOI] [PubMed] [Google Scholar]
- 10.Valdiglesias V., Laffon B. The impact of nanotechnology in the current universal COVID-19 crisis. Let’s not forget nanosafety! Nanotoxicology. 2020;14:1013–1016. doi: 10.1080/17435390.2020.1780332. [DOI] [PubMed] [Google Scholar]
- 11.Statnano, 〈https://statnano.com/technology-against-covid-19-nano-insights〉.
- 12.E. Ruiz‐Hitzky, M. Darder, B. Wicklein, C. Ruiz‐Garcia, R. Martín‐Sampedro, G. Del Real, P. Aranda, Nanotechnology responses to COVID‐19, Adv. Healthc. Mater. 2000979. [DOI] [PubMed]
- 13.Nasrollahzadeh M., Sajjadi M., Soufi G.J., Iravani S., Varma R.S. Nanomaterials and nanotechnology-associated innovations against viral infections with a focus on coronaviruses. Nanomaterials. 2020;10:1072. doi: 10.3390/nano10061072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan W.C.W. Nano research for COVID-19. ACS Nano. 2020;14:3719–3720. doi: 10.1021/acsnano.0c02540. [DOI] [PubMed] [Google Scholar]
- 15.K. Kostarelos, Nanoscale nights of COVID-19 (2020). [DOI] [PubMed]
- 16.Mujawar M.A., Gohel H., Bhardwaj S.K., Srinivasan S., Hickman N., Kaushik A. Aspects of nano-enabling biosensing systems for intelligent healthcare; towards COVID-19 management. Mater. Today Chem. 2020 doi: 10.1016/j.mtchem.2020.100306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bootsma M.C.J., Ferguson N.M. The effect of public health measures on the 1918 influenza pandemic in US cities. Proc. Natl. Acad. Sci. USA. 2007;104:7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campos E.V.R., Pereira A.E.S., de Oliveira J.L., Carvalho L.B., Guilger-Casagrande M., de Lima R., Fraceto L.F. How can nanotechnology help to combat COVID-19? Opportunities and urgent need. J. Nanobiotechnol. 2020;18:1–23. doi: 10.1186/s12951-020-00685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- 21.Zhao M., Liao L., Xiao W., Yu X., Wang H., Wang Q., Lin Y.L., Kilinc-Balci F.S., Price A., Chu L. Household materials selection for homemade cloth face coverings and their filtration efficiency enhancement with triboelectric charging. Nano Lett. 2020;20:5544–5552. doi: 10.1021/acs.nanolett.0c02211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang A., Cai L., Zhang R., Wang J., Hsu P.-C., Wang H., Zhou G., Xu J., Cui Y. Thermal management in nanofiber-based face mask. Nano Lett. 2017;17:3506–3510. doi: 10.1021/acs.nanolett.7b00579. [DOI] [PubMed] [Google Scholar]
- 23.Li Y., Leung P., Yao L., Song Q.W., Newton E. Antimicrobial effect of surgical masks coated with nanoparticles. J. Hosp. Infect. 2006;62:58–63. doi: 10.1016/j.jhin.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 24.Kharaghani D., Khan M.Q., Shahzad A., Inoue Y., Yamamoto T., Rozet S., Tamada Y., Kim I.S. Preparation and in-vitro assessment of hierarchal organized antibacterial breath mask based on polyacrylonitrile/silver (PAN/AgNPs) nanofiber. Nanomaterials. 2018;8:461. doi: 10.3390/nano8070461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang N., Cai M., Yang X., Yang Y. Electret nanofibrous membrane with enhanced filtration performance and wearing comfortability for face mask. J. Colloid Interface Sci. 2018;530:695–703. doi: 10.1016/j.jcis.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 26.F. De Maio, V. Palmieri, G. Babini, A. Augello, I. Palucci, G. Perini, A. Salustri, M. De Spirito, M. Sanguinetti, G. Delogu, L.G. Rizzi, G. Cesareo, P. Soon-Shiong, M. Sali, M. Papi, medRxiv, in press, 10.1101/2020.09.16.20194316. [DOI]
- 27.Bhattacharjee S., Joshi R., Chughtai A.A., Macintyre C.R. Graphene modified multifunctional personal protective clothing. Adv. Mater. Interfaces. 2019;6 doi: 10.1002/admi.201900622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsu B.B., Wong S.Y., Hammond P.T., Chen J., Klibanov A.M. Mechanism of inactivation of influenza viruses by immobilized hydrophobic polycations. Proc. Natl. Acad. Sci. USA. 2011;108:61–66. doi: 10.1073/pnas.1017012108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bai B., Mi X., Xiang X., Heiden P.A., Heldt C.L. Non-enveloped virus reduction with quaternized chitosan nanofibers containing graphene. Carbohydr. Res. 2013;380:137–142. doi: 10.1016/j.carres.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 30.Otto D.P., De M.M. Layer-by-layer nanocoating of antiviral polysaccharides on surfaces to prevent coronavirus infections. Molecules. 2020;25:3415. doi: 10.3390/molecules25153415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss C., Carriere M., Fusco L., Capua I., Regla-Nava J.A., Pasquali M., Scott J.A., Vitale F., Unal M.A., Mattevi C. Toward nanotechnology-enabled approaches against the COVID-19 pandemic. ACS Nano. 2020;14:6383–6406. doi: 10.1021/acsnano.0c03697. [DOI] [PubMed] [Google Scholar]
- 32.Palestino G., García-Silva I., González-Ortega O., Rosales-Mendoza S. Can nanotechnology help in the fight against COVID-19? Expert Rev. Anti-infect. Ther. 2020;18:849–864. doi: 10.1080/14787210.2020.1776115. [DOI] [PubMed] [Google Scholar]
- 33.Dhand R., Li J. Coughs and sneezes: their role in transmission of respiratory viral infections, including SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020;202:651–659. doi: 10.1164/rccm.202004-1263PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmieri V., Papi M. Can graphene take part in the fight against COVID-19? Nano Today. 2020;33 doi: 10.1016/j.nantod.2020.100883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kinnamon D.S., Krishnan S., Brosler S., Sun E., Prasad S. Screen printed graphene oxide textile biosensor for applications in inexpensive and wearable point-of-exposure detection of influenza for at-risk populations. J. Electrochem. Soc. 2018;165:B3084–B3090. [Google Scholar]
- 36.Parupudi T., Panchagnula N., Muthukumar S., Prasad S. Evidence-based point-of-care technology development during the COVID-19 pandemic. Biotechniques. 2020 doi: 10.2144/btn-2020-0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee B.-Y., Behler K., Kurtoglu M.E., Wynosky-Dolfi M.A., Rest R.F., Gogotsi Y. Titanium dioxide-coated nanofibers for advanced filters. J. Nanopart. Res. 2010;12:2511–2519. [Google Scholar]
- 38.Adamcakova-Dodd A., Monick M.M., Powers L.S., Gibson-Corley K.N., Thorne P.S. Effects of prenatal inhalation exposure to copper nanoparticles on murine dams and offspring. Part Fibre Toxicol. 2015;12:30. doi: 10.1186/s12989-015-0105-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baker T.J., Tyler C.R., Galloway T.S. Impacts of metal and metal oxide nanoparticles on marine organisms. Environ. Pollut. 2014;186:257–271. doi: 10.1016/j.envpol.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 40.Luo Z., Li Z., Xie Z., Sokolova I.M., Song L., Peijnenburg W.J.G.M., Hu M., Wang Y. Rethinking nano‐TiO2 safety: overview of toxic effects in humans and aquatic animals. Small. 2020 doi: 10.1002/smll.202002019. [DOI] [PubMed] [Google Scholar]
- 41.Palmieri V., Perini G., De Spirito M., Papi M. Graphene oxide touches blood: in vivo interactions of bio-coronated 2D materials. Nanoscale Horiz. 2019;4:464–471. doi: 10.1039/c8nh00318a. [DOI] [PubMed] [Google Scholar]
- 42.Zhang D., Qiu J., Shi L., Liu Y., Pan B., Xing B. The mechanisms and environmental implications of engineered nanoparticles dispersion. Sci. Total Environ. 2020;722 doi: 10.1016/j.scitotenv.2020.137781. [DOI] [PubMed] [Google Scholar]
- 43.Hashempour S., Ghanbarzadeh S., Maibach H.I., Ghorbani M., Hamishehkar H. Skin toxicity of topically applied nanoparticles. Ther. Deliv. 2019;10:383–396. doi: 10.4155/tde-2018-0060. [DOI] [PubMed] [Google Scholar]
- 44.Fusco L., Garrido M., Martín C., Sosa S., Ponti C., Centeno A., Alonso B., Zurutuza A., Vázquez E., Tubaro A. Skin irritation potential of graphene-based materials using a non-animal test. Nanoscale. 2020;12:610–622. doi: 10.1039/c9nr06815e. [DOI] [PubMed] [Google Scholar]
- 45.Hadrup N., Sharma A.K., Loeschner K., Jacobsen N.R. Pulmonary toxicity of silver vapours, nanoparticles and fine dusts: a review. Regul. Toxicol. Pharmacol. 2020;115 doi: 10.1016/j.yrtph.2020.104690. [DOI] [PubMed] [Google Scholar]
- 46.Matai I., Kaur G., Seyedsalehi A., McClinton A., Laurencin C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials. 2020;226 doi: 10.1016/j.biomaterials.2019.119536. [DOI] [PubMed] [Google Scholar]
- 47.Soares S., Sousa J., Pais A., Vitorino C. Nanomedicine: principles, properties, and regulatory issues. Front. Chem. 2018;6:360. doi: 10.3389/fchem.2018.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang M., Yang J., Cai Z., Feng Y., Wang Y., Zhang D., Pan X. Detection of engineered nanoparticles in aquatic environments: current status and challenges in enrichment, separation, and analysis. Environ. Sci. Nano. 2019;6:709–735. [Google Scholar]
- 49.Park C.M., Chu K.H., Her N., Jang M., Baalousha M., Heo J., Yoon Y. Occurrence and removal of engineered nanoparticles in drinking water treatment and wastewater treatment processes. Sep. Purif. Rev. 2017;46:255–272. [Google Scholar]
- 50.West R., Michie S., Rubin G.J., Amlôt R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat. Hum. Behav. 2020;4:451–459. doi: 10.1038/s41562-020-0887-9. [DOI] [PubMed] [Google Scholar]