Abstract
Bovine tuberculosis (TB) caused by Mycobacterium bovis is a significant health threat to cattle and a zoonotic threat for humans in many developing countries. Rapid and accurate detection of M. bovis is fundamental for controlling the disease in animals and humans, and for the proper treatment of patients as one of the first-line anti-TB drug, pyrazinamide, is ineffective against M. bovis. Currently, there are no rapid, simplified and low-cost diagnostic methods that can be easily integrated for use in many developing countries. Here, we report the development of a loop-mediated isothermal amplification (LAMP) assay for specific identification of M. bovis by targeting the region of difference 4 (RD4), a 12.7 kb genomic region that is deleted solely in M. bovis. The assay's specificity was evaluated using 139 isolates comprising 65 M. bovis isolates, 40 M. tuberculosis isolates, seven M. tuberculosis complex reference strains, 22 non-tuberculous mycobacteria and five other bacteria. The established LAMP detected only M. bovis isolates as positive and no false positives were observed using the other mycobacteria and non-mycobacteria tested. Our LAMP assay detected as low as 10 copies of M. bovis genomic DNA within 40 minutes. The procedure of LAMP is simple with an incubation at a constant temperature. Results are observed with the naked eye by a color change, and there is no need for expensive equipment. The established LAMP can be used for the detection of M. bovis infections in cattle and humans in resource-limited areas.
Author summary
Although bovine tuberculosis in humans has been eliminated in developed countries, the disease remains a challenge in many developing countries. Routine laboratory methods used to identify tuberculosis (TB) in high-burden countries do not distinguish between the two main causes of TB in humans, namely Mycobacterium tuberculosis and M. bovis. In addition, M. bovis is naturally resistant to one of the first-line drugs used to treat TB called pyrazinamide; therefore, accurate diagnosis of M. bovis is important for proper selection of anti TB drugs. In cattle, surveillance for M. bovis infection is important to obtain data on bovine TB burden and hence provide a basis for the establishment and/or improvement of control programs. In this study, a loop-mediated isothermal amplification (LAMP) based method was developed to identify M. bovis. This LAMP method detected M. bovis within 40 minutes following incubation at constant temperature (66°C) in a battery-powered incubator and results could be read with the naked eye following development of a color change. Our results elaborate a rapid and low-cost LAMP based method for detection and surveillance of M. bovis infection in cattle and humans in resource-limited, endemic areas.
Introduction
Mycobacterium tuberculosis, the archetypal member of the M. tuberculosis complex (MTC), is the principal causative agent of tuberculosis (TB) in humans [1]. Additionally, Mycobacterium bovis, which is the main causative pathogen of bovine TB, also causes TB disease in humans which is termed 'zoonotic TB'. In both hosts, M. bovis infections pose serious challenges. For instance, in cattle annual economic losses are estimated at US$3 billion [2]. The losses incurred include condemnation of carcasses at slaughterhouses, mortalities and costs involved in the implementation of disease control measures [2,3]. These challenges are immense mostly in developing and high burdened countries in comparison to developed countries. In the latter, appropriate food hygiene measures such as milk pasteurization and "test and slaughter" control programs to remove infected animals have helped reduce the disease burden. However, this is not the case in developing countries due to a lack of compliance and absence of associated control measures due to financial constraints [4]. In humans, the zoonotic transmission of M. bovis infection from animals poses challenges to standard TB diagnosis and treatment [5]. M. bovis is innately resistant to pyrazinamide (PZA), a critical first line anti-TB drug that plays a unique role in shortening the duration of TB treatment [6]. Hence, if PZA is included in a patient's regimen with M. bovis infection, the drug is ineffective while the patient is exposed to the potential side effects such as hepatotoxicity and polyarthralgia [7]. However, if M. bovis is detected during routine TB diagnosis, then the standard TB regimen can be optimized [5].
In developing countries, routine TB diagnosis is still achieved through clinical symptoms, chest radiography and sputum smear microscopy. Additionally, in referral hospitals or laboratories, BACTEC MGIT culture (Becton Dickinson (BD), USA) or GeneXpert (Cepheid, Sunnyvale, CA, USA) systems are also used. Unfortunately, these methods do not have the capacity to distinguish MTC to the species level [8]. Mycobacterial culture, being the gold standard method for TB diagnosis, takes several weeks to months to read results and thus is unable to provide timely diagnosis [9]. Testing technologies capable of identifying M. bovis have varying limitations prohibiting easy integration in resource-limited areas. For instance, biochemical based tests such as nitrate reduction and niacin accumulation [10] rely on mycobacterial growth and are hence time consuming. Nucleic acid amplification tests (NAAT) such as PCR targeting single nucleotide polymorphisms in the pncA and oxyR genes [11] involve complex procedures, use of expensive equipment and standardized laboratory infrastructure that constrains their use in many developing countries [12].
Lack of rapid, simple and low-cost methods for specific differentiation of MTC species has, to some extent, been caused by the high genetic homogeneity shared among MTC species which show 99% identity at the nucleotide level and with identical 16S rRNA sequences, a molecular marker commonly used in microbiology to distinguish species [13]. Indeed, this high level of genetic identity has led to the MTC species being recently proposed as the same species [14]. Nevertheless, MTC comparative genomic studies have revealed the distinct evolutionary trajectory of the MTC species, traced by the deletion of specific regions [15]. For instance, region of difference 4 (RD4) is a 12.7kb locus that encompasses 11 genes, from Rv1506c - Rv1516c in M. tuberculosis, which is deleted from M. bovis [15]. Therefore, the RD4 deletion could be utilized as a molecular marker to differentiate M. bovis from M. tuberculosis. Indeed, PCR approaches have previously been reported that target RD4 for differentiation of M. bovis from M. tuberculosis [16,17]. Despite being specific for detecting M. bovis, these PCR-based methods are not easily adopted for use in resource limited areas because of the aforementioned constraints mentioned above. Thus, a rapid, simple and low cost diagnostic tool is required in such areas for specific detection of M. bovis that can be easily incorporated into existing systems [18].
Loop-mediated isothermal amplification (LAMP) is a single tube NAAT technique that was developed by Notomi et. al. in 2000 [19]. LAMP doesn't require equipment such as a thermo-cycler or electrophoresis system since DNA amplification occurs under a constant temperature, and the results are visible to the naked eye. LAMP is recommended for use in resource limited areas due to its simplicity, rapidity, sensitivity and use of low cost equipment [20]. LAMP has been reported extensively for detecting several infectious diseases such as malaria [21], TB [22,23] and African trypanosomiasis [24]. In this study, we have developed and utilized a LAMP based technology for specific detection of M. bovis by targeting the deletion of RD4.
Materials and methods
Ethics statement
The ethical approval to conduct this study was granted by The University of Zambia Biomedical Research Ethics Committee for samples from Zambia and National Health Science Research Committee (NHSRC), Ministry of Health and Population, Lilongwe, Malawi for samples from Malawi. The Zambia National Health Research Ethics Committee and the Department of Animal Health and Livestock Development in Malawi approved the transfer of mycobacterial DNA to Hokkaido University (Japan) for molecular analysis.
Samples and DNA extraction
Extracted DNA from 139 mycobacteria and non-mycobacteria were used to determine the specificity of our LAMP assay comprising of seven reference MTC strains, twenty-two reference non-tuberculous mycobacteria (NTM) strains, five reference non-mycobacteria and 105 clinical or field MTC isolates or TB lesion specimens as shown in Tables 1 and S1. We included M. caprae and M. orygis, two other important causative agents of zoonotic TB associated with cattle, as they are pyrazinamide susceptible and thus differentiation from M. bovis was crucial. NTMs were selected as representative mycobacteria that would be useful for differential diagnosis relative to M. bovis infections. A further five bacterial species, that are agents of respiratory infections, were also included to represent general pathogens that would be useful for differential diagnosis of TB in humans.
Table 1. Bacteria used in this study to determine specificity.
| Bacterial species | Sample ID | |
|---|---|---|
| MTC reference strains | M. bovis BCG | 172-Tokyo |
| M. tuberculosis | H37Rv | |
| M. tuberculosis | H37Ra | |
| M. africanum | KK 13–02 | |
| M. caprae | EPDC01 a | |
| M. orygis | NepR1 b | |
| M. microti | ATCC 19422 | |
| MTC clinical isolates | M. bovis | 65 isolates c |
| M. tuberculosis | 40 isolates c | |
| NTM reference strains | M. abscessus | JATA 63–01 |
| M. asiaticum | KK 24–01 | |
| M. avium | JATA 51–01 | |
| M. chelonae | JATA 62–01 | |
| M. fortuitum | JATA 61–01 | |
| M. gastri | KK 44–01 | |
| M. gordonae | JATA 33–01 | |
| M. intermedium | JATA 9H-01 | |
| M. intracellulare | JATA 52–01 | |
| M. kansaii | KK 21–01 | |
| M. lentiflavum | JATA 9N-01 | |
| M. malmoense | JATA 47–01 | |
| M. marinum | JATA 22–01 | |
| M. mucogenicum | JATA 9P-01 | |
| M. nonchromogenicum | JATA 45–01 | |
| M. peregrinum | JATA 61–01 | |
| M. scrofulaceum | JATA 31–01 | |
| M. shimodei | JATA 54–01 | |
| M. simiae | KK 23–01 | |
| M. smegmatis | JATA 64–01 | |
| M. szulgai | JATA 32–01 | |
| M. terrae | JATA 46–01 | |
| Other bacteria | Streptococcus pneumoniae | NBRC 102642 |
| Klebsiella pneumoniae | NBRC 3318 | |
| Pseudomonas aeruginosa | NBRC 12689 | |
| Staphylococcus aureus | NBRC 100910 | |
| Mycoplasma pneumoniae | NBRC 14401 |
Sixty-five isolates of M. bovis and forty of M. tuberculosis were used. Fifty-one isolates grown on Ogawa medium (Kyokuto Pharmaceutical Industrial Co., Ltd., Tokyo, Japan) and identified as M. bovis by a MTC-discrimination multiplex PCR [25] and spoligotyping [26] were collected from cattle and wild lechwe antelope from 2004 to 2009 in Zambia [27]. Twenty clinical samples grown in mycobacterium growth indicator tubes (MGIT) (Becton, Dickinson and Company, NJ, USA) were obtained at the University teaching hospital in Lusaka, Zambia during 2011 to 2016 [28]. Four of those were confirmed as M. bovis and 16 were M. tuberculosis by Capilia TB (Tauns Laboratories Inc., Shizuoka, Japan) and spoligotyping. Ten samples were collected from cattle suspected of TB during routine postmortem at Lilongwe cold storage abattoir in Lilongwe Malawi in November 2019. Briefly, samples were homogenized, decontaminated in 4% NaOH for 15 minutes, followed by neutralization in sterile phosphate buffer saline (PBS) and centrifuged at 3200 g for 20 min at 6°C. Part of the pellets was re-suspended in PBS and DNA was isolated directly by heating at 95°C for 15 minutes and immediately cooling at -20°C for 30 minutes. Confirmation as M. bovis was done at Hokkaido University, Japan using Mycobacterium specific PCR IS6110 [29], MTC-discrimination multiplex PCR and spoligotyping. The other 24 M. tuberculosis isolates were collected in Osaka, Japan during 2000 to 2009 [30] and grown on Ogawa medium. Bacterial DNA from colonies on solid medium was extracted as previously described [29]. For liquid medium cultures, 500 μl of the MGIT contents were taken to a cryotube and DNA was extracted by boiling at 95°C for 15 minutes. All extracted DNA were stored at -30°C.
Primer design and screening
The location of RD4 deletion was determined by sequence alignment of M. bovis AF2122/97 genome sequence (GenBank accession No.: LT708304.1) against M. tuberculosis H37Rv genome sequence (GenBank accession No.: AL123456.3) using Molecular Evolutionary Genetics Analysis (MEGA) version 7 software (https://www.megasoftware.net/ Pennsylvania State University, USA). The target sequence was chosen from upstream through to downstream flanking the RD4 deletion. LAMP primers were designed using the online Primer Explorer V5 software (http://primerexplorer.jp/lampv5e/index.html, Eiken Chemical, Tokyo, Japan). A set of primers comprised of 4 primers, namely: outer primers (Forward outer primer-F3 and Backward outer primer-B3) and inner primers (Forward inner primer-FIP and Backward inner primer-BIP). Loop primers (Forward loop primer-FLP and Backward loop primer-BLP) were designed and added for the best performing primer set that was selected and optimized. In order to determine a set of primers specific for detection of M. bovis, primer design properties and position of RD4 deletions were manually adjusted with reference to the "Advanced primer design" manual [33]. Designed LAMP primers were screened by observing the specificity, cross-reactivity and reaction speed in order to select the best performing primer set. All primers were synthesized by Life Technologies Japan Ltd. (Tokyo, Japan).
Optimization of LAMP reaction
LAMP reactions were performed according to the procedures in Pandey et al [22]. Reaction tubes were incubated at 64°C for 120 minutes in a Loopamp real-time turbidimeter (LA-200: Teramecs Co. Ltd., Kyoto, Japan). M. bovis BCG Tokyo 172 genomic DNA was used as positive control while M. tuberculosis H37Rv DNA and double distilled water (DDW) were both negative controls for every run. Positive results were indicated by rising curve(s) of turbidity greater than 0.1 threshold in the real time turbidimeter (LA-200) and visual inspection of the color change by colori-fluorometric indicator (CFI) [24]. In order to improve LAMP performance, modifications to three parameters of the LAMP reaction were screened. The incubation temperature was screened at 1°C intervals from 60°C to 67°C; the concentration of loop primers was evaluated at 5.0 μM, 4.2 μM, 3.6 μM and 2.8 μM. Inner primers (FIP/BIP) and outer primers (F3/B3) were kept fixed at 4.8 μM and 0.6 μM, respectively. The primer mixture's final volume per reaction was adjusted in 0.25 μl intervals from 2.0 μl to 2.75 μl.
Specificity and sensitivity analysis
Using the optimized conditions, LAMP specificity was evaluated using bacterial genomic DNAs listed in Tables 1 and S1. To assess the specificity, the results of the newly established LAMP were compared to the initial identification and confirmation results using other conventional methods (S1 Table). Sensitivity of our new LAMP system was evaluated using serially diluted M. bovis BCG Tokyo 172 genomic DNA, 2.5pg/μl, 250fg/μl, 25fg/μl, 20fg/μl and 15fg/μl (5pg ~ 30fg/reaction). DNA concentration was measured using a Qubit 3 Fluorometer (Thermo Fisher Scientific, MA, USA) according to the manufacturer's instructions. Reactions were performed in duplicates and repeated 4 times (8 reactions). All reactions were monitored up to 120 min after the beginning of incubation by the LA-200 (Teramecs Co. Ltd.). In the specificity study, the cut-off point to determine positivity and negativity was set to 40 minutes.
Multiplex PCR reaction
Multiplex PCR targeting RD4 [16] was performed to compare its sensitivity to our new LAMP assay. The protocol of multiplex PCR was slightly modified, as follows: 4 μl 5× Go Taq buffer (Promega Co., WI, USA); 0.6 μl of 25mM MgCl2; 0.5 μl of 25mM dNTP mix; 0.5 μl of 10 μM each primer; common forward primer—CBS1 (5'-TTCCGAATCCCTTGTGA-3'); M. bovis specific reverse primer—CBS2 (5'-GGAGAGCGCCGTTGTA-3') and M. tuberculosis specific reverse primer—CBS3 (5'-AGTCGCCGTGGCTTCTCTTTTA-3'); 0.2 μl of 5U/μl GoTaq DNA polymerase (Promega Co.); 1 μl of template DNA; and finally double-distilled water (DDW) to make up to a final volume of 20 μl. The cycling parameters consisted of an initial denaturation at 94°C for 5 min, followed by 30 cycles of denaturation at 94°C (1 min), annealing at 52°C (1.5 min), and extension at 72°C (1 min), with a final elongation step at 72°C for 5 min. The amplification products were analyzed by gel electrophoresis at 100v for 20 min. The predicted PCR products were 168 bp (M. bovis) and 337 bp (M. tuberculosis).
Confirmation of LAMP products
In-silico LAMP fragment analysis (http://creisle.github.io/creisle.lamprflp/) was performed to predict LAMP product sizes. Then, LAMP products were digested by restriction enzyme EcoRI (New England Biolabs, MA, USA). Enzymatic digestion reaction mixture comprised of 1 μl of LAMP product, 1 μl of EcoRI, 2 μl of 10x enzyme buffer (New England Biolabs) and 16 μl of DDW. The mixture was incubated at 37°C for 60 min and the resultant products analyzed by 2% agarose gel electrophoresis stained with Gel-Red (Biotium, Inc., CA, USA).
Results
LAMP primers screening and selection
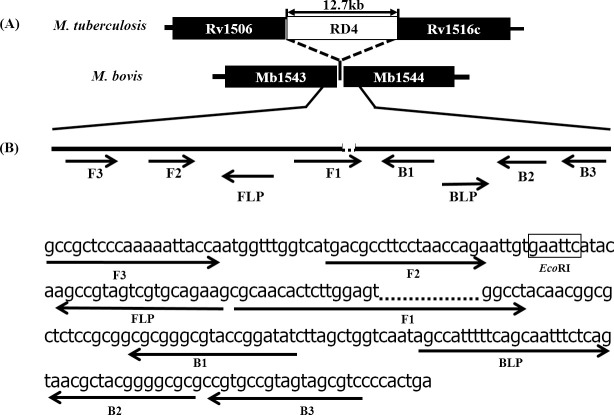
More than 40 sets of primers targeting the RD4 deletion were designed and screened. Primer design properties and position of the RD4 deletion were manually configured while screening for the best performing set of primers for specific detection of M. bovis. A primer set where the F1 primer 3-prime section was located across the RD4 deletion-junction showed high specificity and repeatability and was selected for further optimization (Table 2). The target sequence and primer binding positions are shown in Fig 1.
Table 2. Nucleotide sequences and sizes of established LAMP primers.
| Primer | Length | Sequence (5'-3') |
|---|---|---|
| F3 | 20 | GCCGCTCCCAAAAATTACCA |
| B3 | 18 | GACGCTACTACGGCACGG |
| FIP | 41 | AGGCCACTCCAAGAGTGTTGCG-TGACGCCTTCCTAACCAGA |
| BIP | 35 | GCGCGGGCGTACCGGATAT-GCGCCCCGTAGCGTTA |
| FLP | 19 | CTTCTGCACGACTACGGCT |
| BLP | 24 | AGCCATTTTTCAGCAATTTCTCAG |
FIP primer consisted of F1c and F2; BIP primer consisted of B1 and B2c.
Fig 1. LAMP primers for specific detection of M. bovis targeting the RD4 flanking region.
(A) Position of the RD4 deletion on M. bovis genome, shown with reference to M. tuberculosis. The RD4 locus is present in M. tuberculosis but deleted from M. bovis. (B) The target sequence, individual primers, annealing positions and their directions of the set of primers with RD4 deletion at 3-prime region of F1 primer are shown. Restriction enzyme EcoRI target sequence is indicated in a box between F2 and FLP.
Optimization of LAMP assay
Different incubation temperatures at 1°C intervals from 60°C to 67°C were evaluated. An increase in temperature gave an improved detection speed and specificity. However, at 67°C the LAMP assay sensitivity decreased; thus, the optimal temperature was determined as 66°C. The effect of loop primers was tested at varying concentrations (Table 3). Upon adding 5.0 μM of loop primers to the primer mixture, the assay's detection speed improved with M. bovis; however, false positives from M. tuberculosis were observed. Reducing the concentration of loop primers (4.2 μM) improved the specificity. We observed that by using the lowest concentration of loop primers (2.8 μM) LAMP specificity improved, but sensitivity was reduced. Therefore, the optimal concentration of loop primers was determined as 3.6 μM. Primer mixture volume was optimized in the same way and a 2.25μl/reaction volume was determined to be optimal. With this combination of conditions, no false positives with M. tuberculosis were observed up to 120 min incubation. Considering these adjustments, the final LAMP reaction conditions for our new assay were as follows: reaction temperature of 66°C; 2.25 μl of final primer mixture comprising of 0.6 μM of each outer primer, 4.8 μM of each inner primer, 3.6 μM of each loop primer; 20 mM Tris-HCl (pH 8.8, BIORAD); 10 mM KCl; 10 mM (NH4)2SO4; 0.1% Tween20; 6 mM MgSO4; 0.8 M betaine; 1.25 mM dNTP; 8U Bst DNA polymerase (Nippon Gene Co., Japan); 1 μl of CFI [24]; 2 μl of extracted DNA as a template and DDW up to a final volume of 25 μl.
Table 3. Optimization of primer concentrations and ratios in LAMP reaction.
| Loop Primer concentration | ||||||||
| 5.0μM | 4.2μM | 3.6μM | 2.8μM | |||||
| DNA concentration | BCG | H37Rv | BCG | H37Rv | BCG | H37Rv | BCG | H37Rv |
| 5pg | 21.0±1.3 | 82.1±5.9 | 23.8±0.6 | 95.3±2.6a | 24.8±0.6 | NA | 35.2±3 | NA |
| 500fg | 24±1.7 | NT | 24.9±1.2 | NT | 31.6±2.1 | NT | 39.9±10.1 | NT |
| 50fg | 27.1±0.9 | NT | 30.0±3.1 | NT | 36.1±4.0b | NT | NA | NT |
| NC | NA | NA | NA | NA | ||||
| Primer volume quantity | ||||||||
| 2.0μl | 2.25μl | 2.5μl | ||||||
| DNA concentration | BCG | H37Rv | BCG | H37Rv | BCG | H37Rv | ||
| 5pg | 37.6±1.6 | 117.3c | 32.8±4 | NA | 23.8±2.1 | 101.3±10.1d | ||
| 500fg | 41.9±6.2 | NT | 35.3±2.1 | NT | 31.9±7.0 | |||
| 50fg | 70±15.7e | NT | 45.1±9.0f | NT | 34.4±1.9 | |||
| NC | NA | NA | NA | |||||
LAMP reactions were performed six times (duplicate x 3). Results are shown in time (min.) to be positive presented as mean ± standard deviation. BCG: M. bovis BCG 172 Tokyo; H37Rv: M. tuberculosis H37Rv; NA: No amplification observed within 120 min of reaction; NT: Not tested; NC: Negative control (DDW); NA: No Amplification
a 2 of 6 reactions were positive
b 5 of 6 reactions were positive
c 1 of 6 reactions were positive
d 4 of 6 reactions were positive
e 3 of 6 reactions were positive
f 4 of 6 reactions were positive
Specificity of LAMP assay
An analysis of LAMP specificity was performed by testing 139 DNA samples from bacteria listed in Tables 1 and S1. The assay detected all 65 M. bovis isolates as positive, while all other bacteria tested negative. There were no false positives, which is particularly relevant when considering we tested against M. tuberculosis isolates and other MTC species. All isolates detected as M. bovis by our newly developed LAMP system were in agreement with their initial identification of the samples as M. bovis by other conventional methods (S1 Table).
Sensitivity of LAMP assay and multiplex PCR
Sensitivity analysis of our newly established LAMP was performed by determining limit of detection using diluted M. bovis BCG Tokyo 172 genomic DNA. The detection limit of our new LAMP was 50fg/reaction, equivalent to 10 copies of M. bovis genome, in 40 minutes. These results were observed both on the LAMP turbidimeter (Fig 2A) as well as visually by the naked eye under natural light (Fig 2B) and under LED light (Fig 2C). Comparatively, multiplex PCR [16] performed on the same samples detected up to 5pg/reaction (Fig 2D).
Fig 2. Sensitivity of established LAMP assay and multiplex PCR.
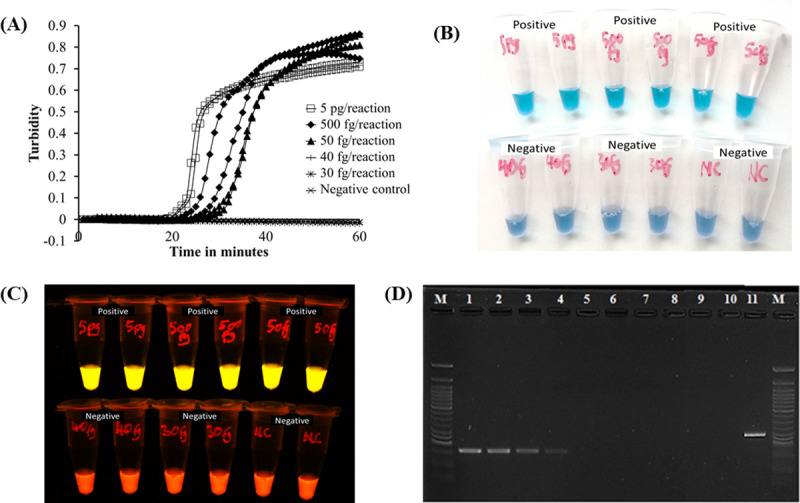
A) LAMP results observed by rising curves of turbidimeter. B) LAMP results observed by the naked eye under natural light; the colour shifts from violet to sky blue for positive samples. C) Under LED light, the color change is from orange to light yellow for positive samples. D) The gel electrophoresis result of the multiplex PCR [16]. Lane M, 50bp DNA marker (New England Biolabs); lanes 1–9, M. bovis BCG Tokyo 172 genomic DNA 500pg, 50pg, 20pg, 5pg, 500fg, 50fg, 40fg, 30fg, 20fg/reaction; lane 10, Negative Control (DDW); lane 11, M. tuberculosis H37Rv.
Confirmation of LAMP products
LAMP products were digested by restriction enzyme EcoRI to confirm successful amplification of the target sequence. Digested LAMP products gave three fragments of 124 bp, 169 bp and 239 bp (Fig 3) as predicted in-silico (S1 Fig).
Fig 3. Enzymatic digestion of target sequence by restriction enzyme EcoRI.
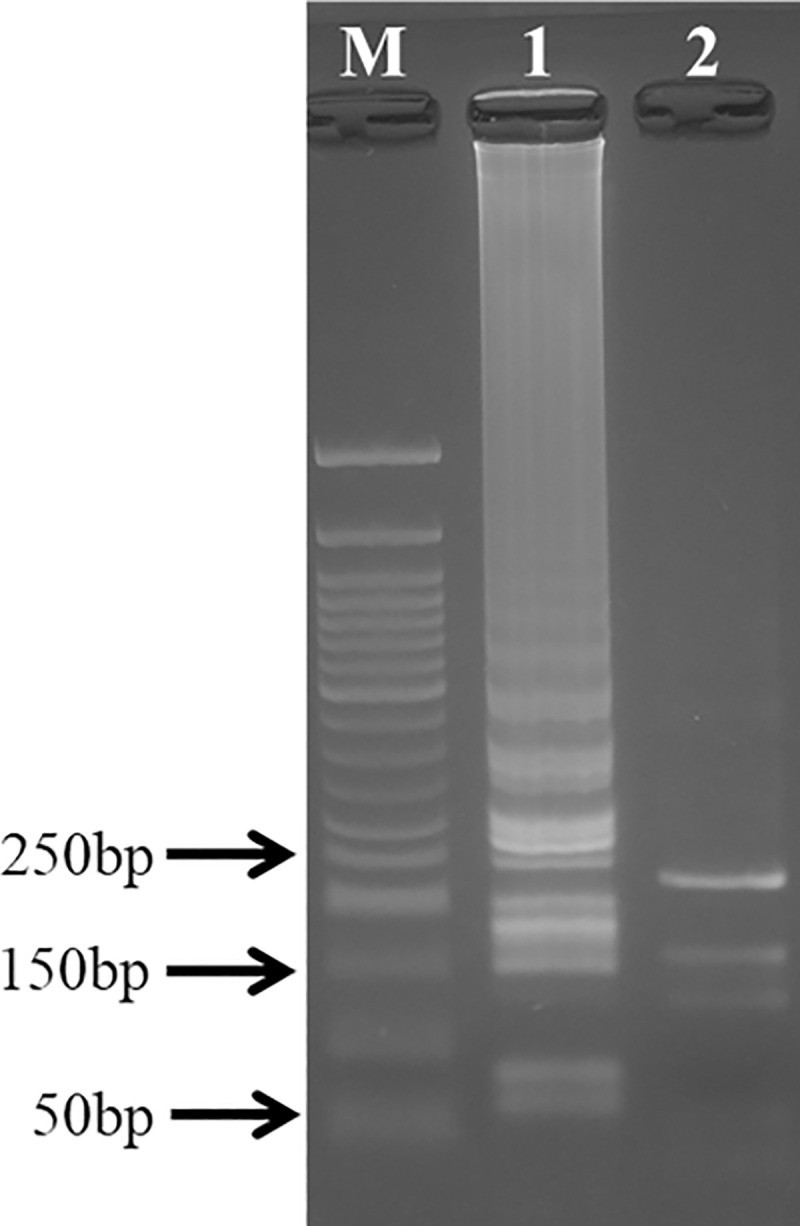
Lane M, 50bp DNA maker (New England Biolabs). Lane 1, LAMP products without the restriction enzyme. Lane 2, LAMP products digested by EcoRI. The predicted product sizes were 124bp, 169bp and 239bp.
Discussion
Bovine tuberculosis represents a potential zoonotic threat to humans in developing countries, but its control has long been neglected. There is substantial evidence suggesting that developing countries bear the highest burden of zoonotic TB due to existence of multiple risk factors maintaining the circulation of the disease in livestock [34]. In Africa a range of 0%-37.7% of all TB cases in humans are estimated to be caused by M. bovis [34]. However, detection of M. bovis is seldom performed, largely because routine TB diagnostic methods do not have the capacity to differentiate M. bovis from other MTC. Methods capable of delineating MTC species, such as PCR or culture-based methods, are time consuming, complicated, and prohibitively expensive and hence not easily adopted for widespread use. Consequently, all TB suspected cases adopt the standard M. tuberculosis treatment regimen that includes pyrazinamide, even though this approach has significant shortcomings in cases of M. bovis infection [35].
In this study, we describe the development of a LAMP-based method for specific identification of M. bovis by targeting the RD4 deletion. Thus, our newly established LAMP assay is important not only for guiding appropriate choice of antimicrobials against zoonotic TB but also for surveillance purposes and disease control. The developed LAMP method accurately identified all M. bovis isolates, while no false positive amplifications were observed with other MTC species (Tables 1 and S1). One cattle sample on Ogawa medium was heavily contaminated with other bacteria, and Pseudomonas sp. sequence was detected by 16S rRNA gene sequencing (C-43, S1 Table); however, the LAMP reaction became positive in less than 40 min in both duplicated test tubes. These results show that our established LAMP is highly specific for detecting M. bovis even in contaminated samples. Furthermore, the results show evidence for 'proof of concept' in using the RD4 deletion as a molecular signature for specific identification of M. bovis amongst other MTC species. Elsewhere, LAMP based methods have been reported for differentiating M. bovis from MTC targeting mbp70 [36] and mtp40 genes [37]. However, the specificity to detect M. bovis only is open to challenge because mbp70 is also present in other MTC species [38], while mtp40 is not present in all M. tuberculosis strains [39]. In view of this, our LAMP is reliable for the identification and differentiation of M. bovis from MTC because it targets RD4 which is the best target for this purpose as all M. bovis strains lack RD4 [15,40].
We used a variety of M. bovis and M. tuberculosis samples in our validation, encompassing M. bovis derived from different animal species, clinical samples from different countries, and M. tuberculosis strains from different lineages and a variety of spoligotypes (S1 Table). All samples gave consistent LAMP results. Moreover, our method can be performed using DNA extracted directly from cattle specimens and a variety of growth media, liquid (MGIT) and solid culture (Ogawa medium). Regardless of the sample source, the performance of our LAMP assay was the same in all cases. The ability to use simply heat-killed MGIT culture is very advantageous in this regard since the medium is now widely used in developing countries, with MGIT positive culture growth indicated within 7 to 14 days. Hence this LAMP could be incorporated with standard MGIT to confirm and speciate positive growth results, allowing diagnosis at the earliest possible time.
We also performed the established LAMP system using larger amounts of mycobacterial DNA (50pg/reaction, an equivalent to smear positive sputum+++) [41] in order to evaluate the applicability on samples with an unknown number of bacterial cells/DNA concentration. We observed no false amplification of M. tuberculosis until a reaction time of 92 minutes. Thus, the results show the ability of our established LAMP to specifically identify M. bovis. Despite the false amplification of M. tuberculosis when larger amounts of DNA were used, our LAMP reaction time could be shortened to 40 minutes to ensure specific identification of M. bovis. The established LAMP is highly sensitive, with the assay detecting as few as to 10 copies of M. bovis genomic DNA. In comparison to previous reports, a LAMP system targeting RD1 deletions for identification of M. bovis BCG required more than 200 copies of the targets for detection using a turbidimeter, and 2000 copies for detection with a visible color change [42]. In other reports, a LAMP system targeting the rim-encoding 16S rRNA-processing protein for detection of M. tuberculosis and M. bovis detected as low as 200 copies [43]. Our results therefore indicate that the newly established LAMP assay has a superior limit of detection compared to previously described systems. In addition, the LAMP can be used together with other conventional MTC identification methods, such as MGIT culture, to enhance detection of M. bovis infections. Furthermore, as well as its application in human disease, our LAMP could be employed to detect M. bovis from cattle samples after postmortem assisting in tracing back sources of infection and the implementation of appropriate control measures.
Our established LAMP can easily be integrated for use in resource limited settings due to its properties. It employs simple procedures that involve mixing the reaction reagents in a single tube before incubating at a constant temperature (66°C) for 40 min. Furthermore, the incubation of LAMP reagents doesn't require the use of expensive equipment or a standardized laboratory; a heat block or water bath is sufficient, and results can be visualized with the naked eye, eliminating the need for procedures such as gel electrophoresis and photographic imaging as is the case with PCR-based methods.
One major challenge to enzymatic-based methods is cold chain maintenance and storage of reagents in resource limited areas. To overcome this, Hayashida and others [24,44] used dried LAMP reagents, facilitating reagents' storage for an extended period without the need to maintain a cold chain. We plan to explore this option for our next study and further optimize the dry LAMP method for direct use against sputum samples and cattle post-mortem samples in a field setting. A further consideration in zoonotic TB is the emerging appreciation of the role of Mycobacterium orygis in human and bovine disease, particularly in South Asia [32,45,46]. Hence, further development of our LAMP system could allow for differential identification of M. orygis vs M. bovis, for example, by targeting the distinct RD12 deletion locus in M. orygis [47].
In conclusion, we have established a LAMP system for specific detection of M. bovis by targeting the RD4 deletion. The established LAMP showed high specificity and sensitivity, with ease and use coupled with rapid detection time. This new RD4 LAMP assay employs simple procedures and does not require expensive equipment, such as thermocyclers. Additionally, one reaction cycle of the RD4 LAMP would cost ~US$1–2, hence it is a cheaper approach as compared to other NAATs. Our future development work will focus on establishing a dry LAMP kit to facilitate transport and storage, and evaluate it on field samples.
Supporting information
(XLSX)
(TIFF)
Acknowledgments
We appreciate the Japan BCG Laboratory for providing the BCG bacterial strain, Dr. Takayuki Wada, Dr. Shiomi Yoshida and Fukuyama Zoo for providing the M. caprae sample and Miss Yukari Fukushima for her help in preparing DNA samples.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported in part by a grant from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT) for the Joint Research Program of the Research Center for Zoonosis Control, Hokkaido University (to YS), and in part by Japan Agency for Medical Research and Development (AMED) under Grant Number JP20jk0210005, JP20jm0110021, JP20wm0125008 to YS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Smith NH, Gordon S V., de la Rua-Domenech R, Clifton-Hadley RS, Hewinson RG. Bottlenecks and broomsticks: the molecular evolution of Mycobacterium bovis. Nat Rev Microbiol. Nature Publishing Group; 2006;4: 670–681. 10.1038/nrmicro1472 [DOI] [PubMed] [Google Scholar]
- 2.Kuria J K.N. Diseases Caused by Bacteria in Cattle: Tuberculosis. Bacterial Cattle Diseases. IntechOpen; 2019. 10.5772/intechopen.82051 [DOI] [Google Scholar]
- 3.Schiller I, Oesch B, Vordermeier HM, Palmer M V., Harris BN, Orloski KA, et al. Bovine Tuberculosis: A Review of Current and Emerging Diagnostic Techniques in View of their Relevance for Disease Control and Eradication. Transbound Emerg Dis. 2010; no-no. 10.1111/j.1865-1682.2010.01148.x [DOI] [PubMed] [Google Scholar]
- 4.Cousins D V. Mycobacterium bovis infection and control in domestic livestock. Rev Sci Tech. France; 2001;20: 71–85. 10.20506/rst.20.1.1263 [DOI] [PubMed] [Google Scholar]
- 5.Allix-Béguec C, Fauville-Dufaux M, Stoffels K, Ommeslag D, Walravens K, Saegerman C, et al. Importance of identifying Mycobacterium bovis as a causative agent of human tuberculosis. European Respiratory Journal. European Respiratory Society; 2018. pp. 692–694. 10.1183/09031936.00137309 [DOI] [PubMed] [Google Scholar]
- 6.Girling DJ. The role of pyrazinamide in primary chemotherapy for pulmonary tuberculosis. Tubercle. 1984;65: 1–4. 10.1016/0041-3879(84)90024-2 [DOI] [PubMed] [Google Scholar]
- 7.Papastavros T, Dolovich LR, Holbrook A, Whitehead L, Loeb M. Adverse events associated with pyrazinamide and levofloxacin in the treatment of latent multidrug-resistant tuberculosis. CMAJ. Canadian Medical Association; 2002;167: 131–6. Available: http://www.ncbi.nlm.nih.gov/pubmed/12160118 [PMC free article] [PubMed] [Google Scholar]
- 8.WHO | Roadmap for zoonotic tuberculosis. WHO. World Health Organization; 2017; [Google Scholar]
- 9.Achkar JM, Lawn SD, Moosa M-YS, Wright CA, Kasprowicz VO. Adjunctive Tests for Diagnosis of Tuberculosis: Serology, ELISPOT for Site-Specific Lymphocytes, Urinary Lipoarabinomannan, String Test, and Fine Needle Aspiration. J Infect Dis. Narnia; 2011;204: S1130–S1141. 10.1093/infdis/jir450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niemann S, Richter E, Rüsch-Gerdes S. Differentiation among members of the Mycobacterium tuberculosis complex by molecular and biochemical features: Evidence for two pyrazinamide- susceptible subtypes of M. bovis. J Clin Microbiol. American Society for Microbiology (ASM); 2000;38: 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espinosa De Los Monteros LE, Galán JC, Gutiérrez M, Samper S, García Marín JF, Martín C, et al. Allele-specific PCR method based on pncA and oxyR sequences for distinguishing Mycobacterium boris from Mycobacterium tuberculosis: Intraspecific M. bovis pncA sequence polymorphism. J Clin Microbiol. American Society for Microbiology (ASM); 1998;36: 239–242. 10.1128/JCM.36.1.239-242.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nahid P, Pai M, Hopewell PC. Advances in the diagnosis and treatment of tuberculosis. Proc Am Thorac Soc. American Thoracic Society; 2006;3: 103–10. 10.1513/pats.200511-119JH [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Case RJ, Boucher Y, Dahllöf I, Holmström C, Doolittle WF, Kjelleberg S. Use of 16S rRNA and rpoB genes as molecular markers for microbial ecology studies. Appl Environ Microbiol. American Society for Microbiology; 2007;73: 278–88. 10.1128/AEM.01177-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riojas MA, Mcgough KJ, Rider-Riojas CJ, Rastogi N, Hazbón MH. Phylogenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis. 10.1099/ijsem.0.002507 [DOI] [PubMed] [Google Scholar]
- 15.Gordon S V, Brosch R, Billault A, Garnier T, Eiglmeier K, Cole ST. Identification of variable regions in the genomes of tubercle bacilli using bacterial artificial chromosome arrays. Mol Microbiol. 1999;32: 643–55. Available: http://www.ncbi.nlm.nih.gov/pubmed/10320585 10.1046/j.1365-2958.1999.01383.x [DOI] [PubMed] [Google Scholar]
- 16.Bakshi CS, Shah DH, Verma R, Singh RK, Malik M. Rapid differentiation of Mycobacterium bovis and Mycobacterium tuberculosis based on a 12.7-kb fragment by a single tube multiplex-PCR. Vet Microbiol. 2005;109: 211–216. 10.1016/j.vetmic.2005.05.015 [DOI] [PubMed] [Google Scholar]
- 17.Halse TA, Escuyer VE, Musser KA. Evaluation of a single-tube multiplex real-time PCR for differentiation of members of the Mycobacterium tuberculosis complex in clinical specimens. J Clin Microbiol. American Society for Microbiology Journals; 2011;49: 2562–7. 10.1128/JCM.00467-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carruth L, Roess AA, Mekonnen YT, Melaku SK, Nichter M, Salman M. Zoonotic tuberculosis in Africa: challenges and ways forward. Lancet (London, England). Elsevier; 2016;388: 2460–2461. 10.1016/S0140-6736(16)32186-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Notomi T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000;28: 63e – 63. 10.1093/nar/28.12.e63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. The Use Of A Commercial Loop-Mediated Isothermal Amplification Assay (Tb-Lamp) For The Detection Of Tuberculosis. WHO Press Expert Gr Meet Rep GENEVA MAY 2013. 2013; 1–50. Available: http://www.who.int/about/licensing/copyright_form/en/index.html [Google Scholar]
- 21.Vásquez AM, Zuluaga L, Tobón A, Posada M, Vélez G, González IJ, et al. Diagnostic accuracy of loop-mediated isothermal amplification (LAMP) for screening malaria in peripheral and placental blood samples from pregnant women in Colombia. Malar J. BioMed Central; 2018;17: 262 10.1186/s12936-018-2403-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pandey BD, Poudel A, Yoda T, Tamaru A, Oda N, Fukushima Y, et al. Development of an in-house loop-mediated isothermal amplification (LAMP) assay for detection of Mycobacterium tuberculosis and evaluation in sputum samples of Nepalese patients. J Med Microbiol. 2008;57: 439–443. 10.1099/jmm.0.47499-0 [DOI] [PubMed] [Google Scholar]
- 23.Bi A, Nakajima C, Fukushima Y, Tamaru A, Sugawara I. A Rapid Loop-Mediated Isothermal Amplification Assay Targeting hspX for the Detection of Mycobacterium tuberculosis Complex. 2012; 247–251. 10.7883/yoken.65.247 [DOI] [PubMed] [Google Scholar]
- 24.Hayashida K, Kajino K, Hachaambwa L, Namangala B, Sugimoto C. Direct blood dry LAMP: a rapid, stable, and easy diagnostic tool for Human African Trypanosomiasis. PLoS Negl Trop Dis. Public Library of Science; 2015;9: e0003578 10.1371/journal.pntd.0003578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakajima C, Rahim Z, Fukushima Y, Sugawara I, van der Zanden AGM, Tamaru A, et al. Identification of Mycobacterium tuberculosis clinical isolates in Bangladesh by a species distinguishable multiplex PCR. BMC Infect Dis. 2010;10: 118 10.1186/1471-2334-10-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. American Society for Microbiology (ASM); 1997;35: 907–14. Available: http://www.ncbi.nlm.nih.gov/pubmed/9157152 10.1128/JCM.35.4.907-914.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hang’ombe MB, Munyeme M, Nakajima C, Fukushima Y, Suzuki H, Matandiko W, et al. Mycobacterium bovis infection at the interface between domestic and wild animals in Zambia. BMC Vet Res. 2012;8: 221 10.1186/1746-6148-8-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Solo ES, Nakajima C, Kaile T, Bwalya P, Mbulo G, Fukushima Y, et al. Mutations of rpoB, katG and inhA genes in multidrug-resistant Mycobacterium tuberculosis isolates from Zambia. J Glob Antimicrob Resist. Elsevier BV; 2020; 10.1016/j.jgar.2020.02.026 [DOI] [PubMed] [Google Scholar]
- 29.Suzuki Y, Katsukawa C, Inoue K, Yin Y, Tasaka H, Ueba N, et al. Mutations in rpoB gene of rifampicin resistant clinical isolates of Mycobacterium tuberculosis in Japan. Kansenshogaku Zasshi. 1995;69: 413–9. Available: http://www.ncbi.nlm.nih.gov/pubmed/7751750 10.11150/kansenshogakuzasshi1970.69.413 [DOI] [PubMed] [Google Scholar]
- 30.Tamaru A, Nakajima C, Wada T, Wang Y, Inoue M, Kawahara R, et al. Dominant Incidence of Multidrug and Extensively Drug-Resistant Specific Mycobacterium tuberculosis Clones in Osaka Prefecture, Japan. PLoS One. Public Library of Science; 2012;7: 1–7. 10.1371/journal.pone.0042505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshida S, Suga S, Ishikawa S, Mukai Y, Tsuyuguchi K, Inoue Y, et al. Mycobacterium caprae infection in captive Borneo Elephant, Japan. Emerg Infect Dis. Centers for Disease Control and Prevention (CDC); 2018;24: 1937–1940. 10.3201/eid2410.180018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thapa J, Paudel S, Sadaula A, Shah Y, Maharjan B, Kaufman GE, et al. Mycobacterium orygis-associated tuberculosis in free-ranging rhinoceros, Nepal, 2015 [Internet]. Emerging Infectious Diseases. Centers for Disease Control and Prevention (CDC); 2016. pp. 570–572. 10.3201/eid2203.151929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LAMP primer design manual. [retrieved on 5 Oct 2020]. Available: http://primerexplorer.jp/e/v4_manual/pdf/PrimerExplorerV4_Manual_3.pdf
- 34.Müller B, Dürr S, Alonso S, Hattendorf J, Laisse CJM, Parsons SDC, et al. Zoonotic Mycobacterium bovis–induced Tuberculosis in Humans. Emerg Infect Dis. 2013;19: 899–908. 10.3201/eid1906.120543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allix-Béguec C, Fauville-Dufaux M, Stoffels K, Ommeslag D, Walravens K, Saegerman C, et al. Importance of identifying Mycobacterium bovis as a causative agent of human tuberculosis. Eur Respir J. European Respiratory Society; 2010;35: 692–4. 10.1183/09031936.00137309 [DOI] [PubMed] [Google Scholar]
- 36.Zhang H, Wang Z, Cao · Xudong, Wang Z, Sheng J, Wang Y, et al. Loop-mediated isothermal amplification assay targeting the mpb70 gene for rapid differential detection of Mycobacterium bovis. Arch Microbiol. 2016;198: 905–911. 10.1007/s00203-016-1232-6 [DOI] [PubMed] [Google Scholar]
- 37.Hong M, Zha L, Fu W, Zou M, Li W, Xu D. A modified visual loop-mediated isothermal amplification method for diagnosis and differentiation of main pathogens from Mycobacterium tuberculosis complex. World J Microbiol Biotechnol. 2012;28: 523–531. 10.1007/s11274-011-0843-y [DOI] [PubMed] [Google Scholar]
- 38.Lorente-Leal V, Liandris E, Castellanos E, Bezos J, Domínguez L, de Juan L, et al. Validation of a Real-Time PCR for the Detection of Mycobacterium tuberculosis Complex Members in Bovine Tissue Samples. Front Vet Sci. Frontiers Media S.A.; 2019;6: 61 10.3389/fvets.2019.00061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weil A, Plikaytis BB, Ray Butler W, Woodley CL, Shinnick TM. The mtp40 Gene Is Not Present in All Strains of Mycobacterium tuberculosis. JOURNAL OF CLINICAL MICROBIOLOGY. 1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brosch R, Gordon S V., Marmiesse M, Brodin P, Buchrieser C, Eiglmeier K, et al. A new evolutionary scenario for the Mycobacterium tuberculosis complex. Proc Natl Acad Sci. 2002;99: 3684–3689. 10.1073/pnas.052548299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tattersfield A. Toman’s Tuberculosis. Case Detection, Treatment, and Monitoring. Questions and Answers. Second Edition. Am J Trop Med Hyg. 2005;73: 229–229. 10.4269/ajtmh.2005.73.229 [DOI] [Google Scholar]
- 42.Kouzaki Y, Maeda T, Sasaki H, Tamura S, Hamamoto T, Yuki A, et al. A simple and rapid identification method for Mycobacterium bovis BCG with loop-mediated isothermal amplification. PLoS One. 2015;10: 1–12. 10.1371/journal.pone.0133759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu R-Y, Zhang K-X, Zhao M-Q, Liu Y-H, Xu Y-Y, Ju C-M, et al. Use of visual loop-mediated isotheral amplification of rimM sequence for rapid detection of Mycobacterium tuberculosis and Mycobacterium bovis. J Microbiol Methods. Elsevier; 2009;78: 339–343. 10.1016/j.mimet.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 44.Thapa J, Maharjan B, Malla M, Fukushima Y, Poudel A, Pandey BD, et al. Direct Detection of Mycobacterium Tuberculosis in Clinical Samples by a Dry Methyl Green Loop-Mediated Isothermal Amplification (LAMP) Method. Tuberculosis (Edinb). 2019. July;117:1–6. 10.1016/j.tube.2019.05.004 [DOI] [PubMed] [Google Scholar]
- 45.Rahim Z, Thapa J, Fukushima Y, van der Zanden AGM, Gordon SV, Suzuki Y, et al. Tuberculosis Caused by Mycobacterium orygis in Dairy Cattle and Captured Monkeys in Bangladesh: a New Scenario of Tuberculosis in South Asia. Transbound Emerg Dis. 2017. December;64(6):1965–1969. 10.1111/tbed.12596 [DOI] [PubMed] [Google Scholar]
- 46.Duffy SC, Srinivasan S, Schilling MA, Stuber T, Danchuk SN, Michael JS, et al. Reconsidering Mycobacterium bovis as a proxy for zoonotic tuberculosis: a molecular epidemiological surveillance study. Lancet Microbe. 2020. June;1(2):e66–e73. 10.1016/S2666-5247(20)30038-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Ingen J, Rahim Z, Mulder A, Boeree MJ, Simeone R, Brosch R, et al. Characterization of Mycobacterium orygis as M. tuberculosis complex subspecies. Emerg Infect Dis. 2012. April;18(4):653–5. 10.3201/eid1804.110888 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(TIFF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.