Abstract
Background and aims
Potential role of health literacy in determining adherence to COVID-19 preventive behavior, pharmacological, and lifestyle management among diagnosed patients of chronic diseases during nationwide lockdown is inadequately investigated.
Methods
A cross-sectional study was conducted from May–August 2020 among diagnosed patients of chronic diseases residing in a COVID-19 hotspot of urban Jodhpur, Rajasthan, and availing health services from primary care facility. Telephonic interviews of participants were conducted to determine their health literacy using HLS-EU-Q47 questionnaire, adherence to COVID-19 preventive behaviour as per World Health Organization recommendations, and compliance to prescribed pharmacological and physical activity recommendations for chronic disease.
Results
All the 605 diagnosed patients of chronic diseases availing services from primary care facility were contacted for the study, yielding response rate of 68% with 412 agreeing to participate. Insufficient health literacy was observed for 65.8% participants. Only about half of participants had scored above median for COVID-19 awareness (55.1%) and preventive behavior (45.1%). Health literacy was observed to be significant predictor of COVID-19 awareness [aOR: 3.53 (95% CI: 1.81–6.88)]; COVID-19 preventive behavior [aOR: 2.06, 95%CI; 1.14–3.69] and compliance to pharmacological management [aOR: 3.05; 95% CI: 1.47–6.35] but not for physical activity.
Conclusion
COVID-19 awareness, preventive behavior, and compliance to pharmacological management is associated with health literacy among patients of chronic disease availing services from primary health facility. Focusing on health literacy could thus be an essential strategic intervention yielding long term benefits.
Keywords: Health literacy, COVID-19 awareness, COVID-19 preventive behavior, Chronic diseases, Adherence, Nation-wide lockdown
1. Introduction
Global crisis due to COVID-19 has demanded rapid assimilation of knowledge and significant behaviour change by community members to limit the transmission of SARS-CoV2 [1]. Health literacy is anticipated to play an essential role in understanding the specific health-related terms like at-risk groups, social distancing, or cough etiquette [[2], [3], [4]]. It implies not only knowledge of the facts but also translation of the acquired knowledge into the adoption of promotive health behaviour to improve or maintain health status, with the ability to critically analyse the background reasoning and have competency to access reliable health information [5]. Furthermore, its significance is greatly increased among chronic disease patients as they require extensive management, self-care, and repeated interactions with healthcare practitioners [6,7]. Low health literacy is associated with poor quality of life, non-adherence to management protocols, minimal or no self-care, increased health expenditure, morbidity, and mortality among chronic disease patients [[8], [9], [10], [11], [12]]. Health literacy in India is insufficiently explored, and limited literature available assessing the same [[13], [14], [15], [16]].
Patients with chronic conditions such as Diabetes, Hypertension, Cardiovascular diseases, etc., are vulnerable to acquire SARS-CoV2 and have higher mortality rates [[17], [18], [19], [20]]. The burden of patients with Diabetes and Hypertension is worrisome in India. Further, chronic disease patients face a dual challenge, not only due to the infectious disease but also due to interrupted outpatient routine care during lockdown imposed in response to pandemic [21,22]. Thus, it becomes essential to ascertain adherence to essential management recommendation among such patients.
Deficient control of SARS-CoV-2 replication and prolonged pro-inflammatory response leading to poor outcomes among T2DM patients, especially in association with older age, hypertension, and/or CVDs, is reported [23]. Li B et al., reported a 2-fold increase in the risk of severe disease or requiring intensive care unit (ICU) admission in patients with Diabetes or Hypertension [24]. Further, treatment of the original comorbidities, especially in older patients, to mitigate impact of COVID-19 infections is emphasized [25].
Assessment of baseline COVID-19 awareness and preventive behaviour is fundamental to developing tailored, specific interventions and guiding policymakers to discern any critical challenge that needs to be addressed. Thus, this study was conducted with the aim to explore the association of health literacy with COVID-19 awareness and preventive behaviour and adherence to essential treatment advice among chronic disease patients availing services from a primary health facility in one of the worst COVID-19 affected area in urban Jodhpur, Rajasthan.
2. Materials and methods
2.1. Study setting and design
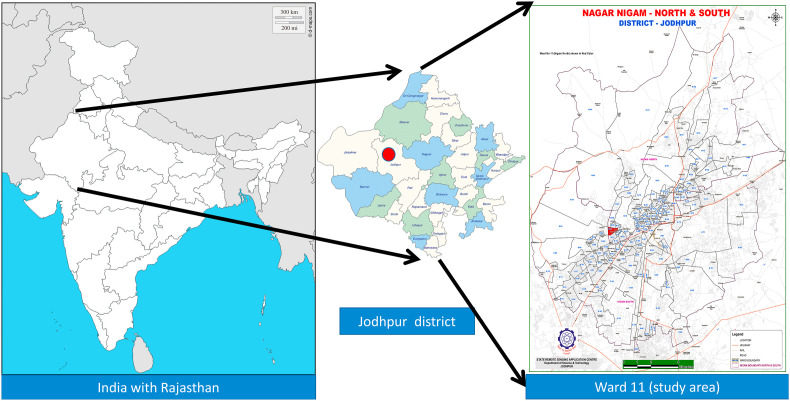
To date, India is one of the most severely affected country by COVID-19 [26]. A cross-sectional study was conducted among chronic disease patients attending Primary Health Centre in an urban area of Jodhpur, Rajasthan (hotspot area, Fig. 1 ) during the nationwide lockdown [27].
Fig. 1.
Map of India with location of study area (COVID-19 hot spot) within Jodhpur district.
Sampling frame constituted all patients with chronic diseases aged 18 years and above receiving care from Urban Primary Health Centre. Patient’s age, gender, telephone number, and diagnosis were accessed from a computerized database routinely maintained at the health facility. They were telephonically contacted for informed consent and participation. All patients were contacted for a minimum of ten times at different time intervals during the working hours on weekdays to give them an opportunity to participate in the study. In case of an invalid contact number or non-response, the participant was considered as a non-responder.
Sample size: Nearly 50% of chronic disease patients fail to adhere to their medical advices [28]. With the absolute precision of 5%, the desired sample size was estimated to be 384 for the current study.
2.2. Study tool
2.2.1. Health literacy
For the current study, European Health Literacy survey (HLS-EU-Q47) questionnaire was used, which is previously validated (Cronbach’s alpha >0.90 and item-scale convergent validity ≥0.40) among the Asian population [29]. The tool measures health literacy comprehensively in both hospital and community based settings [29,30]. The tool was translated into the local language and retranslated to English, taking the help of language experts, and discrepancies were resolved by discussion. There are 47 items in the questionnaire under three subdomains i.e., health care, disease prevention, and health promotion. Responses are recorded as “very difficult”, “quite difficult”, “quite easy”, and “very easy” [29]. Internal consistency analysis for the current study was conducted by determining Cronbach alpha and Split-half Spearman-Brown coefficient.
2.2.2. Awareness and adherence to COVID-19 preventive behavior
An interviewer-administered, semi-structured, pre-tested questionnaire was developed to assess COVID-19 awareness and preventive behaviour using a 15-item tool. Awareness was assessed for modes of transmission, symptoms, preventive behaviour, and sub-groups vulnerable to COVID-19.
COVID-19 preventive behaviour was assessed as per the WHO recommendations [31] based on an instrument measuring four domains - cough etiquette, use of face masks (either fabric or medical masks), restriction of outdoor movements, practicing hand hygiene, and adhering to social distancing. The response was recorded as “sometimes,” “always,” and “never.”
2.2.3. Adherence to pharmacological and physical activity advice
Participant’s awareness regarding the availability of essential healthcare services during the ongoing lockdown was assessed. Compliance to pharmacological and routine physical activity during the last one month of lockdown was assessed using a dichotomous question.
2.3. Scoring and operational definitions
Health literacy score calculation and grading: Final health literacy score was calculated using the formula (Mean of each item − 1) × (50/3). Respondents’ scores were categorized as “Insufficient (0–25)”, “Problematic” (26–33), “Sufficient” (34–42), and “Perfect” (43–50) [32]. Further, respondents with the category of problematic and insufficient scores were grouped under “limited health literacy,” and those with perfect or sufficient scores were grouped under “adequate health literacy” [33].
COVID-19 awareness and adherence to preventive behaviour: For COVID-19 awareness, the correct response was scored as one and incorrect as zero. Score of one was given if the participant responded “always” and zero for “sometimes” or “never” responses for adherence to COVID -19 preventive behaviour. Thus, the score ranged from zero to 15 for COVID-19 awareness and zero to 6 for adherence to preventive behaviour. Skewed distribution was observed for both kinds of score (Shapiro-Wilk <0.001). Scores above median value was taken as the cut-off for both COVID-19 awareness and recommended behaviour.
Controlled metabolic status: Last available Blood Pressure (BP) and Fasting Plasma Glucose (FPG) readings were obtained from medical records of the participants based on which they were categorized into “controlled” and “uncontrolled” status. A patient with Diabetes was considered as controlled if FPG values were <126 mg/dl as per Indian Council of Medical Research guidelines [34]. Hypertensive patients were classified based on age and BP readings using JNC VIII guidelines [35] i.e. controlled if BP < 140/90 in less than 60 years or BP < 150/90 in case of more than 60 years [35]. A patient suffering from Diabetes and Hypertension was assessed for both criteria to be included under “controlled” status.
2.4. Data analysis and statistical methods
The analysis was done using Statistical package for Social Sciences (SPSS v.23) IBM Corp. The variables were analysed using descriptive statistics to calculate frequencies, mean, median, range, and Inter Quartile Range (IQR). Bivariate analysis was done between independent variables (sociodemographic characteristics, metabolic control, and health literacy) and dependent variables (COVID-19 awareness and adherence to preventive behaviour and essential management recommendation) using chi-square, Man-Whittany, and Kruskall-Wallis test. Hierarchical regression modelling was done to control for confounders.
2.5. Ethical consideration
Institutional Ethics Committee of All India Institute of Medical Sciences, Jodhpur, provided approval for the study (Certificate reference number: AIIMS/IEC/2020–21/2001). Informed consent was taken from all respondents.
3. Results
A total of 605 patients’ details available in the database of Primary Health facility were accessed. Of these, 412 (68.1%) respondents could be telephonically contacted to administer the questionnaire. None of the participants contacted declined to respond to any portion of the questionnaire. The mean age and morbidity pattern of the responders (412) and non-responders (193) is described in Table 1 . The distribution of gender, age, morbidity profile of the chronic disease, and metabolic control assessed were significantly different for both groups. Responders include more participants aged 60 years or above; male; suffering from both Type-2 diabetes and Hypertension and uncontrolled metabolic status compared to non-responders. During the lockdown phase, some participants [40 (9.7%)] reported migrating to rural areas. At the time of data collection, 19 (4.6%) participants reported Influenza-like Illness.
Table 1.
Sociodemographic details of the study population (N = 605).
| Characteristics | Categories | Responders n = 412 | Non-responders n = 193 | p-valueb |
|---|---|---|---|---|
| Age group | 18 - <30 | 11 (2.7%) | 16 (8.3%) | 0.001 |
| 30–40 | 65 (15.8%) | 28 (14.5%) | ||
| 40–50 | 100 (24.3%) | 60 (31.1%) | ||
| 50–60 | 81 (19.7%) | 43 (22.3%) | ||
| >60 | 155 (37.6%) | 46 (23.8%) | ||
| Gender | Male | 257 (62.4%) | 100 (51.8%) | 0.014 |
| Female | 155 (37.6%) | 93 (48.2%) | ||
| Current place of residence c |
Urban | 372 (90.3%) | Urban area | |
| Rural | 40 (9.7%) | |||
| Highest level of education attainedc |
Post-graduate degree | 7 (1.7%) | Not available | |
| Bachelor’s degree completed | 34 (8.3%) | |||
| Higher secondary school completed | 43 (10.4%) | |||
| Secondary school completed | 101 (24.5%) | |||
| Less than primary school completed | 142 (34.5%) | |||
| Illiterate | 85 (20.6%) | |||
| Morbidity profile | Diabetes | 136 (33.0%) | 76 (39.4%) | 0.020 |
| Hypertension | 181 (43.9%) | 91 (47.2%) | ||
| Both | 95 (23.1%) | 26 (13.5%) | ||
| Metabolic control of the diseasea | Controlled | 187 (45.4%%) | 105 (54.4%) | 0.039 |
| Uncontrolled | 225 (54.6%%) | 88 (45.6%) |
Controlled if FBS<126 and BP < 140/90 and Uncontrolled if either Diabetes or Hypertension is uncontrolled i.e. FBS >126 or BP > 140/90.
Chi-square test.
For Current residence of all the non-responders was urban area (study area) and Highest level of education was not available for non-responders.
Health Literacy: For the HLS-EU-Q47 scale, Cronbach’s alpha was 0.958 and split-half Spearman-Brown coefficient was 0.970, depicting good internal consistency. A significantly high proportion [271 (65.8%)] of the respondents had “insufficient” level of health literacy, followed by “problematic” health literacy level [67 (16.3%)]. Mean scores and percentage distribution of responses for 47 items were calculated (Supplementary file 1). Nearly fifty percent of the study participants found it very difficult to obtain, judge, or understand health-related information pertaining to disease prevention and health promotion. Median health literacy scores using HLS-EU-Q47 was 16.9 with an Inter-Quartile Range (IQR) of 12–28 (Fig. 2 ).
Fig. 2.
Spider chart depicting distribution of health literacy categories according to the morbidity profile of the study participants
Spider chart depicting the proportion of participants having insufficient, problematic, sufficient, and perfect categories using HLS-EU-Q47 tool according to their morbidity; Diabetes Mellitus (DM), Hypertension (HTN) or both Diabetes and Hypertension (Both).
3.1. Awareness and adherence to COVID-19 preventive behaviour
All respondents had heard of COVID-19 through daily news (80.3%), friends or relatives (72.3%), social media (44.9%), and healthcare personnel (13.4%). Few [46 (11.2%)] were unaware of any modes of transmission or any symptoms [39 (9.5%)], but the majority [264 (81.2%)] were unaware of asymptomatic presentation. Approximately one-third of participants [148 (35.9%)] were unaware of susceptible population sub-groups (Table 2 ).
Table 2.
COVID-19 awareness and adherence to preventive behavior (n = 412).
| COVID-19 awareness | Aware/Unaware n (%) | Response if aware |
||
|---|---|---|---|---|
| Yes n (%) | No n (%) | |||
| Heard about COVID-19 | Aware | 412 (100) | NIL | |
| Modes of transmissiona | Aware | 366 (88.8%) | ||
| 1. Transmission by droplet infection (when an individual coughs or sneezes and another person is nearby) | 223 (60.9) | 143 (39.1) | ||
| 2. Transmission can be airborne in some situations | 67 (18.3) | 299 (81.7) | ||
| 3. Touching a contaminated surface or object | 280 (76.5) | 86 (23.5) | ||
| 4. Standing close to a possibly infected person (<1 m) | 180 (49.2) | 186 (50.8) | ||
| Various symptoms of COVID-19a | Aware | 373 (90.5) | ||
| 1. Respiratory symptoms like cough, sneeze, fever or shortness of breath | 373 (100) | NIL | ||
| 2. Diarrhea | 14 (3.8) | 359 (96.2) | ||
| 3. Asymptomatic | ||||
| 70 (18.8) | 303 (81.2) | |||
| Susceptible population sub-groupsa 1. Geriatric population 2. Patients with chronic diseases (DM, HT, CAD, CKD) 3. Both |
Aware | 264 (64.1) | ||
| 58 (21.9) | 206 (78.0) | |||
| 19 (7.2) | 245 (92.8) | |||
| 187 (70.8) | 77 (29.2) | |||
| Preventive measure against COVID-19a | Aware | 381 (92.5) | ||
| 1. By decreasing outdoor movements | 314 (82.4) | 67 (17.6) | ||
| 2. By wearing mask | 324 (85.0) | 57 (14.9) | ||
| 3. By maintaining social distance | 255 (66.9) | 126 (33.1) | ||
| 4. By performing hand washing with soap and water as frequently as possible | 291 (76.4) | 90 (23.6) | ||
| Urban primary health center is providing essential medical care (medical consultation, investigation, and medicines). | Aware | 240 (58.3) | ||
| Awareness score (median ± IQR): 9 (7–10) | ||||
| Maximum-minimum: 1-15 | ||||
| Acceptable awareness (score greater than 9): 227 (55.1%) | ||||
| Adherence to COVID-19 preventive behavior | ||||
| Alwaysn (%) | Sometimesn (%) | Never n (%) | ||
| Social distancing | 241 (60.9) | 141 (35.6) | 14 (3.5) | |
| Using face masks | 232 (58.6) | 130 (32.8) | 34 (8.6) | |
| Observing cough etiquette (Cover mouth and nose when coughing or sneezing) | 154 (38.9) | 150 (37.9) | 92 (23.2) | |
| Hand hygiene (frequently) | 302 (76.3) | 90 (22.7) | 4 (1.0) | |
| Restricted outdoor movement | 331 (83.6) | 63 (15.9) | 2 (0.5) | |
| Practice score (median ± IQR): 3 (2–5) | ||||
| Maximum-minimum: 0-6 | ||||
| Acceptable practice (score greater than 3): 186 (45.1%) | ||||
IQR: Inter-Quartile Range.
Responses have multiple answers.
Many participants [172 (41.7%)] were unaware of the availability of health care staff and medicines at the primary health care facility during the lockdown phase. Median awareness score was 9 (IQR:7–10). Participants with age <30 years [median (IQR): 9(6–10)] and with college education [median (IQR): 9(8–12)] scored higher (Supplementary file 2). About half of (55.1%) participants scored above median (>9).
Few participants [16 (3.9%)] reported nil adherence to any recommended preventive behaviours. Majority participants [331, (80.3%)] reported minimizing outdoor movements and practicing frequent hand hygiene [302 (76.3%)]. Nearly one-third participants reported poor adherence to social distancing [141 (35.6%)], use of masks [130 (32.8%)], and observing cough etiquette [92 (23.2%)] (Table 2). Median score (IQR) for preventive behaviour was calculated to be 3 (2–5). Scores were higher among patients less than 40 years and those currently residing in urban area [4 (3–6); p < 0.05]. Overall, 186 (45.1%) participants scored above median for COVID-19 preventive behaviour (Supplementary file 2).
Education of secondary level and above [{aOR: 1.86 (95% CI: 1.09–3.16)} & {aOR: 2.39; 95% CI: 1.44–3.97}] and adequate health literacy [{aOR: 3.53 (95% CI: 1.81–6.88)} & {aOR: 2.06; 95% CI:1.14–3.69}] significantly predicted both COVID-19 awareness and preventive behaviour, respectively. Urban location [aOR: 2.37; 95% CI: 1.09–5.12] of respondents significantly determined better preventive behaviour only (Table 3 ).
Table 3.
Predictors of COVID-19 awareness, adherence to COVID-19 preventive behaviour and pharmacological management, and routine physical activity (n = 412).
| Predictor variables | COVID-19 awareness (Median score above 9) |
COVID-19 preventive behavior (Median score above 3) |
Adherence to pharmacological management during lockdown |
Adherence to routine physical activity during lockdown |
||||
|---|---|---|---|---|---|---|---|---|
| ORa (95% CI) | aOR b (95% CI) | ORa (95% CI) | aORb (95% CI) | ORa (95% CI) | aORb (95% CI) | ORa (95% CI) | aOR b (95% CI) | |
| Health literacy (Adequate vs Limited) | 4.17 (2.21–7.87)c | 3.53 (1.81–6.88)c | 2.68 (1.58–4.52)c | 2.06 (1.14–3.69)c | 3.03 (1.54–5.98)c | 3.05 (1.47–6.35)c | 2.24 (1.30–3.88)c | 1.39 (0.76–2.57) |
| Education level (Secondary level or higher vs below secondary education) | 2.39 (1.46–3.92)c | 1.86 (1.09–3.16)c | 3.00 (1.88–4.80)c | 2.39 (1.44–3.97)c | 1.24 (0.75–2.03) | 0.82 (0.47–1.43) | 2.65 (1.62–4.35)c | 2.11 (1.23–3.62)c |
| Current residence (Urban vs Rural) | 0.73 (0.37–1.44) | 0.63 (0.31–1.27) | 2.69 (1.28–5.67)c | 2.37 (1.09–5.12)c | 1.55 (0.79–3.03) | 1.49 (0.74–3.00) | 0.75 (0.38–1.47) | 0.62 (0.31–1.24) |
| Gender (Male vs Female) | 1.06 (0.71–1.58) | 0.88 (0.57–1.33) | 0.96 (0.64–1.43) | 0.86 (0.56–1.31) | 1.39 (0.91–2.12) | 1.30 (0.84–2.02) | 1.75 (1.17–2.61)c | 1.59 (1.04–2.42)c |
| Metabolic control (Controlled vs uncontrolled) | 1.13 (0.76–1.68) | 1.11 (0.73–1.67) | 0.74 (0.50–1.10) | 0.71 (0.47–1.08) | 1.21 (0.79–1.84) | 1.19 (0.77–1.84) | 1.42 (0.96–2.10) | 1.48 (0.98–2.25) |
| Age (greater than 60 vs less than 60) | 0.91 (0.61–1.36) | 1.10 (0.72–1.69) | 0.81 (0.54–1.21) | 1.04 (0.67–1.59) | 1.06 (0.69–1.63) | 1.17 (0.74–1.83) | 0.84 (0.56–1.25) | 0.89 (0.58–1.36) |
| COVID-19 awareness (Median score above 9 vs below or equal to 9) | -------- | 1.26 (0.85–1.87) | 1.01 (0.66–1.55) | 1.03 (0.67–1.57) | 0.89 (0.57–1.39) | 1.27 (0.85–1.88) | 1.03 (0.67–1.57) | |
| COVID-19 preventive behavior (Median score above 3 vs below or equal to 3) | -------- | 1.58 (1.03–2.41)c | 1.43 (0.91–2.25) | 1.78 (1.19–2.64)c | 1.63 (1.06–2.49)c | |||
| Nagelkerke R Square | 0.097 | 0.113 | 0.064 | 0.964 | ||||
| Omnibus Tests | 0.000 | 0.000 | 0.014 | 0.104 | ||||
| Hosmer and Lemeshow Test | 0.427 | 0.790 | 0.896 | 0.000 | ||||
Bivariate analysis.
Hierarchial regression modelling.
p < 0.05 (significant predictors).
3.2. Adherence to medical management and routine physical activity during past one month of lockdown
One third [128 (29.9%)] participants had stopped taking medicine, and nearly half [180 (43.7%)] had stopped routine physical activity. Health literacy was significant predictor for adherence to medical management (aOR: 3.05; 95% CI: 1.47–6.35) but not for physical activity. Male gender (aOR: 1.59; 95% CI: 1.04–2.42); education status of secondary or above (aOR: 2.11; 95% CI: 1.23–3.62) and adherence to COVID-19 preventive behaviour (aOR: 1.63; 95% CI: 1.06–2.49) were significant predictors of adherence to routine physical activity (Table 3).
4. Discussion
Our study is one of the few studies highlighting the use of mobile phones in reaching out to patients of chronic diseases, especially more than 60 years of age during a nation-wide lockdown registered at a primary health facility; to assess and strengthen adherence to COVID-19 preventive behaviour, pharmacological management and routine physical activity seeking care from urban primary health care facility in Rajasthan, India. Caballero et al. have highlighted multiple challenges encountered while providing care to people living with diabetes in outpatient settings and have suggested solutions using smartphones to reconnect with patients to emphasize diet, exercise, and pharmacological therapy [36]. Our study supports this perspective and emphasizes that connecting with patients through mobile calls is an effective approach. The respondents, as compared to non-respondents, represented population sub-groups at higher risk of COVID-19 mortality comprising of male patients aged more than 60 years suffering from diabetes and hypertension and of uncontrolled metabolic status as per available records [37].
Majority of our study population had insufficient (65.8%) health literacy scores. Comparable results were obtained by Guclu et al. using HLS-EU-Q47, who reported insufficient health literacy level among 70.9% and problematic among 20.6%, patients attending the outpatient’s department at Bursa, Turkey [38]. In the Indian context, Singh et al. used the Rapid Estimate of Adult Literacy in Medicine (REALM) to determine health literacy and reported low literacy levels in a large proportion (63%) of diabetes patients [15].
Our study observed that health literacy is a significant predictor of COVID-19 awareness and preventive behaviour, previously reported by Bailey et al. [39]. Limited evidence exists from India, exploring the role of health literacy in pandemic situations influencing awareness and adherence to medical directives among patients suffering from chronic diseases. Having low health literacy implies that these individuals have difficulty comprehending health-related information holistically, affecting their health behaviour. During the pandemic time, this lacuna is accentuated as it is pivotal to adopt appropriate measures to curtail the transmission. Furthermore, it is vital to focus on health literacy even during non-pandemic times as better health literacy levels are associated with improved health status and outcomes, especially among chronic disease patients. Significant association (p < 0.01; p < 0.05) between some items of health literacy scale, HLS-COVID-Q22, derived from HLS-EU-Q, with education is reported by Okan O et al. and may explain education level as a significant predictor for adherence to COVID 19 preventive behaviour in our study [40]. Better COVID-19 preventive behaviour among urban residents is reported in other countries and is attributed to more diagnosis and testing of cases [41]. Thus in a rapidly developing pandemic, COVID 19 testing may contribute to the development and adoption of effective public health strategies [42].
Our study participants were receiving regular care at the government primary care facility before lockdown. The previously diagnosed cases of hypertension, type 2 diabetes mellitus, or both included in the current study are an important sub-group of population affected by both the COVID-19 pandemic and nationwide lockdown. Presence of uncontrolled glycemia and blood pressure in a high proportion of patients accessing regular care is reported [43,44]. A large proportion of study participants were unaware of the continuous availability of medical care at the primary health facility during the nation-wide lockdown. Poor utilization and accessibility of primary health facilities by the patient with the chronic disease during lockdown can be attributed to low health literacy level [45].
Our study participants represent the challenges suffered by patients of a small town as compared to patients with chronic diseases in a metropolitan city where 91% stated uninterrupted medicine availability [46]. Poor health literacy is a possible significant predictor for low adherence to pharmacological management as reported by other studies too [2,11]. Acute physical inactivity in our study during lockdown is an undesirable effect of COVID-19 pandemic also observed in many countries [47]. The drastic decreases in physical activity among older adults led to impaired glycaemic control, increased inflammation, reduced muscle protein synthesis, and increase fat mass. The increased plasma concentrations of inflammatory markers (IL-6) stay elevated even after returning to normal physical activity. Role of exercise, a heart-healthy diet, and an active lifestyle to achieve a healthy cardio-metabolic profile is well emphasized [48,49]. The strengths of the current study lie in determining the role of health literacy utilizing a standardized scale among the vulnerable population residing in small towns of a middle-income country, India, which is currently amongst the worst affected nation of the world.
Future research: COVID-19 pandemic is continuing in India, and technology in the form of smartphones, video-consultations, short text messaging, and mobile calls can be an effective mechanism in reaching out to patients of chronic diseases even in small towns. Training of primary care physicians and ancillary staff in providing care through this approach need to be studied and can provide valuable inputs in strengthening overall health care delivery to these patients in the coming years. This needs to be coupled with initiatives for improving health literacy for empowering communities to actively engage in their health care, identify lacunae in current health behavior, and address the deficiencies to promote their health holistically. Thus it would be worthwhile to invest in improving health literacy as a long term measure.
4.1. Limitations
Our study has the following limitations: dietary compliance, the stress factor, and access to medications during lockdown were not evaluated. This study was performed in a single urban primary health centre catering to the homogeneous population, and thus the results may not be representative of other populations. Though the social desirability bias cannot be ruled out but was minimized by conducting the interviews exhaustively without rush, and the participants were given appropriate information and time to respond. The tool used to determine the level of COVID-19 awareness and health promotive measures was pre-tested and was based on WHO guidelines, and care was taken to minimize the information bias.
5. Conclusion
Poor health literacy among our study population and its significant relation with COVID 19 preventive behaviour and adherence to pharmacological management and physical activity is noteworthy among chronic disease patients registered at the primary health care facility. The ongoing COVID 19 pandemic has emphasized the essence of electronic health records to be remotely accessed and utilized for counselling patients regarding ongoing pandemic and chronic disease management.
Declaration of competing interest
There are no conflicts of interest associated with this publication, and there has been no financial support for this publication. As corresponding author, I confirm the same. We hope you find our work suitable for publication.
Acknowledgment
We want to acknowledge the participants for their cooperation and valuable time. We want to extend our sincere gratitude to State Remote Sensing Application Centre, Department of science and technology, Jodhpur, to provide access to Jodhpur’s district map showing the study area, prepared using GIS and Remote Sensing Techniques.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dsx.2020.12.023.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Zarocostas J. How to fight an infodemic. Lancet (London, England) 2020;395:676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdel-Latif M.M.M. The enigma of health literacy and COVID-19 pandemic. Publ Health. 2020;185:95–96. doi: 10.1016/j.puhe.2020.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abel T., McQueen D. Critical health literacy and the COVID-19 crisis. Health Promot Int. 2020 doi: 10.1093/heapro/daaa040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paakkari L., Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Heal. 2020;5:e249–e250. doi: 10.1016/S2468-2667(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kickbusch I.S. Health literacy: addressing the health and education divide. Health Promot Int. 2001;16:289–297. doi: 10.1093/heapro/16.3.289. [DOI] [PubMed] [Google Scholar]
- 6.Artinian N.T., Fletcher G.F., Mozaffarian D., Kris-Etherton P., Van Horn L., Lichtenstein A.H. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the american heart association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith S.C., Benjamin E.J., Bonow R.O., Braun L.T., Creager M.A., Franklin B.A. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 8.Taylor D.M., Fraser S., Dudley C., Oniscu G.C., Tomson C., Ravanan R. Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrol Dial Transplant. 2018;33:1545–1558. doi: 10.1093/ndt/gfx293. [DOI] [PubMed] [Google Scholar]
- 9.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 10.W S., C J., A R. Relationship of preventive health practices and health literacy: a national study. Am J Health Behav. 2008;32 doi: 10.5555/AJHB.2008.32.3.227. [DOI] [PubMed] [Google Scholar]
- 11.Levy H., Janke A. Health literacy and access to care. J Health Commun. 2016;21:43–50. doi: 10.1080/10810730.2015.1131776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization . World Health Organization; 2013. Health literacy. The solid facts. [Google Scholar]
- 13.Ogorchukwu J.M., Sekaran V.C., Nair S., Ashok L. Mental health literacy among late adolescents in South India: what they know and what attitudes drive them. Indian J Psychol Med. 2016;38:234–241. doi: 10.4103/0253-7176.183092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehrotra K., Nautiyal S., Raguram A. Mental health literacy in family caregivers: a comparative analysis. Asian J Psychiatr. 2018;31:58–62. doi: 10.1016/j.ajp.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Singh S., Acharya S.D., Kamath A., Ullal S.D., Urval R.P. Health literacy status and understanding of the prescription instructions in diabetic patients. J Diabetes Res 2018. 2018 doi: 10.1155/2018/4517243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.A Gurtoo M Ap S.A.S.M.K. Level of health literacy among type 2 diabetic persons and its relation to glycemic control. J Assoc Phys India. 2019;67:59–62. [PubMed] [Google Scholar]
- 17.Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging Dis. 2020;11:668–678. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang B., Li R., Lu Z., Huang Y. Does comorbidity increase the risk of patients with covid-19: evidence from meta-analysis. Aging (N Y) 2020;12:6049–6057. doi: 10.18632/AGING.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poblador-Plou B., Carmona-Pírez J., Ioakeim-Skoufa I., Poncel-Falcó A., Bliek-Bueno K., Cano-Del Pozo M. Baseline chronic comorbidity and mortality in laboratory-confirmed COVID-19 cases: results from the PRECOVID study in Spain. Int J Environ Res Publ Health. 2020;17:1–14. doi: 10.3390/ijerph17145171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim D.W., Byeon K.H., Kim J., Cho K.D., Lee N. The correlation of comorbidities on the mortality in patients with COVID-19: an observational study based on the Korean national health insurance big data. J Kor Med Sci. 2020;35 doi: 10.3346/JKMS.2020.35.E243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Basu S. Non-communicable disease management in vulnerable patients during Covid-19. Indian J Med Ethics. 2020;103–5 doi: 10.20529/IJME.2020.041. [DOI] [PubMed] [Google Scholar]
- 22.Scott E.S., Jenkins A.J., Fulcher G.R. Challenges of diabetes management during the COVID-19 pandemic. Med J Aust. 2020;213:56–57. doi: 10.5694/mja2.50665. e1. [DOI] [PubMed] [Google Scholar]
- 23.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hussain A., Bhowmik B., do Vale Moreira N.C. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. doi: 10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organisation . 2020. Coronavirus disease (COVID-19) situation report-209 situation in numbers (by WHO region) [Google Scholar]
- 27.Official website for Jodhpur Covid19 info Jodhpur 2020. https://jodhpur.rajasthan.gov.in/content/raj/jodhpur/en/Covid19info.html#
- 28.Haskard Zolnierek K.B., Dimatteo M.R. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duong T.V., Aringazina A., Baisunova G., Nurjanah Pham T.V., Pham K.M. Measuring health literacy in Asia: validation of the HLS-EU-Q47 survey tool in six Asian countries. J Epidemiol. 2017;27:80–86. doi: 10.1016/j.je.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sørensen K., Van Den Broucke S., Pelikan J.M., Fullam J., Doyle G., Slonska Z. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q) BMC Publ Health. 2013;13 doi: 10.1186/1471-2458-13-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organisation Advice for the public. Coronavirus dis advice public 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- 32.Sørensen K., Pelikan J.M., Röthlin F., Ganahl K., Slonska Z., Doyle G. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU) Eur J Publ Health. 2015;25:1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogt D., Schaeffer D., Messer M., Berens E.M., Hurrelmann K. Health literacy in old age: results of a German cross-sectional study. Health Promot Int. 2018;33:739–747. doi: 10.1093/heapro/dax012. [DOI] [PubMed] [Google Scholar]
- 34.Indian Council of Medical Research . 2018. ICMR guidelines for management of type 2 Diabetes 2018. [Google Scholar]
- 35.Armstrong C, Senior Associate Editor A . vol. 90. 2014. (JNC 8 guidelines for the management of hypertension in adults). [PubMed] [Google Scholar]
- 36.Caballero A.E., Ceriello A., Misra A., Aschner P., McDonnell M.E., Hassanein M. COVID-19 in people living with diabetes: an international consensus. J Diabet Complicat. 2020;34:107671. doi: 10.1016/j.jdiacomp.2020.107671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martins-Filho P.R., Antunes de Souza Araújo A., Pereira L.X., Quintans-Júnior L.J., de Souza Barboza W., Cavalcante T.F. Factors associated with mortality among hospitalized patients with COVID-19: a retrospective cohort study. Am J Trop Med Hyg. 2020 doi: 10.4269/ajtmh.20-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guclu O.A., Demirci H., Ocakoglu G., Guclu Y., Uzaslan E., Karadag M. Relationship of pneumococcal and influenza vaccination frequency with health literacy in the rural population in Turkey. Vaccine. 2019;37:6617–6623. doi: 10.1016/j.vaccine.2019.09.049. [DOI] [PubMed] [Google Scholar]
- 39.Bailey S.C., Serper M., Opsasnick L., Persell S.D., O’Conor R., Curtis L.M. Changes in COVID-19 knowledge, beliefs, behaviors, and preparedness among high-risk adults from the onset to the acceleration phase of the US outbreak. J Gen Intern Med. 2020:1. doi: 10.1007/s11606-020-05980-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Okan O., Bollweg T.M., Berens E.M., Hurrelmann K., Bauer U., Schaeffer D. Coronavirus-related health literacy: a cross-sectional study in adults during the COVID-19 infodemic in Germany. Int J Environ Res Publ Health. 2020;17:1–20. doi: 10.3390/ijerph17155503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen N.P.T., Hoang T.D., Tran V.T., Vu C.T., Siewe Fodjo J.N., Colebunders R. Preventive behavior of Vietnamese people in response to the COVID-19 pandemic. PloS One. 2020;15 doi: 10.1371/journal.pone.0238830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jarrom D., Elston L., Washington J., Prettyjohns M., Cann K., Myles S. Effectiveness of tests to detect the presence of SARS-CoV-2 virus, and antibodies to SARS-CoV-2, to inform COVID-19 diagnosis: a rapid systematic review. BMJ Evidence-Based Med. 2020 doi: 10.1136/bmjebm-2020-111511. 0. bmjebm-2020-111511. [DOI] [PubMed] [Google Scholar]
- 43.Borgharkar S.S., Das S.S. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diabetes Res Care. 2019;7:654. doi: 10.1136/bmjdrc-2019-000654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Unnikrishnan R., Anjana R.M., Deepa M., Pradeepa R., Joshi S.R., Bhansali A. Glycemic control among individuals with self-reported diabetes in India - the ICMR-INDIAB study. Diabetes Technol Therapeut. 2014;16:596–603. doi: 10.1089/dia.2014.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nouhjah S., Jahanfar S. Challenges of diabetes care management in developing countries with a high incidence of COVID-19: a brief report. Diabetes Metab Syndr Clin Res Rev. 2020;14:731–732. doi: 10.1016/j.dsx.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr Clin Res Rev. 2020;14:917–920. doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martinez-Ferran M., de la Guía-Galipienso F., Sanchis-Gomar F., Pareja-Galeano H. Metabolic impacts of confinement during the COVID-19 pandemic due to modified diet and physical activity habits. Nutrients. 2020;12 doi: 10.3390/nu12061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lavie C.J., Ozemek C., Carbone S., Katzmarzyk P.T., Blair S.N. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124:799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 49.Marzetti E., Calvani R., Tosato M., Cesari M., Di Bari M., Cherubini A. Sarcopenia: an overview. Aging Clin Exp Res. 2017;29:11–17. doi: 10.1007/s40520-016-0704-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.